Ashley’s Stage 4 ROS1+ Non-Small Cell Lung Cancer Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

Ashley, a mother of 2 young children, shares her journey with stage 4 lung cancer. Initially experiencing a persistent cough post-COVID, Ashley also began to experience shortness of breath and sharp pains that led her to seek help at a hospital. While the first hospital misdiagnosed her ailment as pneumonia, a second hospital found a life-threatening pulmonary embolism. Further tests confirmed stage 4 adenocarcinoma (non-small cell lung cancer). Ashley and her husband, Jason, deeply felt the impact of her diagnosis, particularly given past family losses to cancer.
Determined to seek comprehensive care, Ashley pursued a second opinion from MD Anderson. There, she learned about her ROS1 biomarker, which allowed her to undergo targeted therapy. This approach has been successful, putting her in remission.
Ashley sought refuge in her faith and combines traditional treatment with holistic methods, emphasizing the importance of integrating both to support her immune system. She has taken proactive steps to improve her well-being, including leaving her full-time job to focus on her health and spend more time with her family.
Ashley underscores the significance of self-advocacy in her treatment, highlighting instances where she challenged medical advice and conducted her own research. Through therapy and a positive mindset, she combats the mental health challenges associated with her illness. Ashley advises others to maintain hope, advocate for themselves, and support their emotional and physical health integratively. Her story emphasizes the importance of seeking answers and living fully despite her prognosis, as she cherishes her time with loved ones and continues making memories.
- Name:
- Ashley S.
- Diagnosis:
- Lung Cancer
- Staging:
- Stage 4
- Symptoms:
- Cough that lasted for months
- Sharp pain in right abdomen and shoulder area
- Treatment:
- Targeted therapy

We would like to thank The White Ribbon Project for its partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Thank you to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.
I’m such a data-driven, logical, realistic person.
But cancer has taught me that I have to live in the space where optimism and hope are.
Introduction
Hi, I’m Ashley. I was diagnosed at 35 years old with stage 4 lung cancer, adenocarcinoma, non-small cell with the genetic mutation of ROS1.
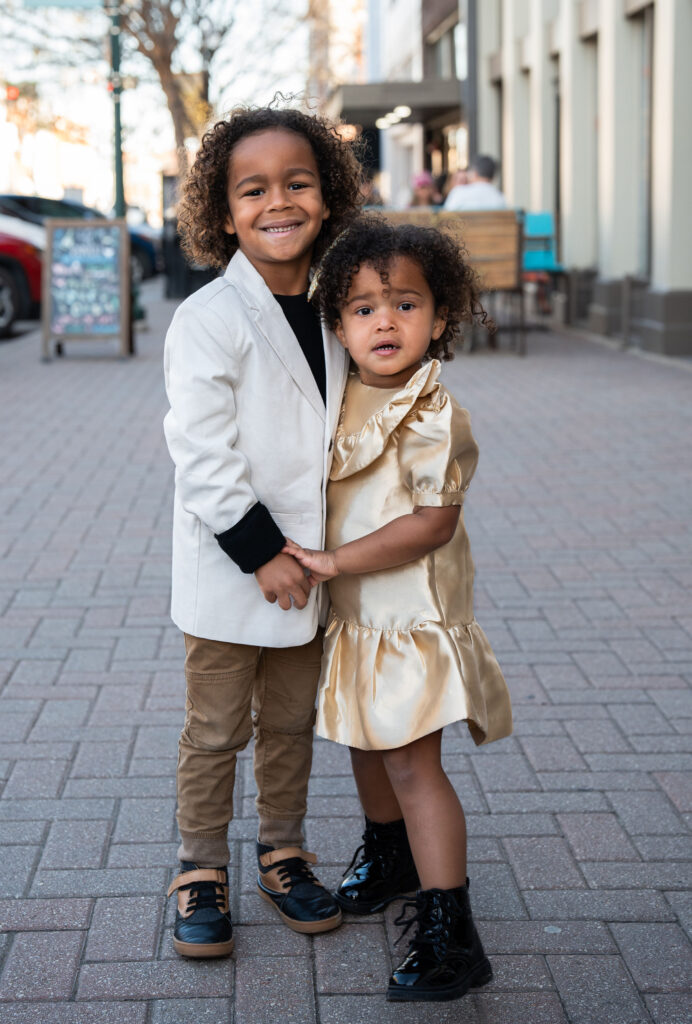
I am a mom of 2, a little boy and girl who were 5 and 2 respectively when I fell ill. I love being outside, going on nature trails and hiking.
Also, we have a pool in our backyard and swimming laps for exercise is definitely a hobby and something I was doing a lot leading up to my diagnosis.
I was also working out with a personal trainer and lifting weights, all up until the day my initial symptoms started.


Pre-diagnosis
Initial symptoms
Before all this began, I struggled with a persistent cough that lasted for maybe 8 or 9 months.
I’d had COVID in January, and by September I was still coughing. On a daily basis, it would start out mild, but would worsen as the day progressed, and then I would be hacking by bedtime. But I wouldn’t allow it to interrupt my day; I would still be going 100mph as a mom.
I saw a doctor in May, and he chalked it up to allergies. I just kept getting my daily stuff done because it wasn’t so disruptive anyway.
Later on in the year, my husband Jason and I were working out with a personal trainer, and I was weightlifting, deadlifting heavy weights. We started HIIT workouts, high intensity interval training.
One morning, we were swimming laps in our backyard pool to the point that we were trying to huff and puff. And I noticed that I really couldn’t be underwater for a very long time.
I went on about my day and began work by 2:00 p.m. that day. I started having a sharp pain in my right abdominal area, the rib cage area. I powered through and ignored it.
That evening we were hosting a small group, so we had roughly like 20 or so people over, and were in the middle of a meal when I started having another bout of sharp pain in my right abdomen again and my right shoulder area too.
I thought, man, was it something I ate? Could it be gallstones? It’s unbearable, just a lot of pain. But I decided I would get to it after everybody left. The group laid hands on me and prayed over me, and we went about our night after they went home.
The next day, the pain got even more intense. I couldn’t walk from my bed to the bathroom without hunching over in agony. So we decided it was time to head to the ER.
We went in, and they did a workup. And they found that I had a lung full of fluid. They told me I had pneumonia and sent me home with literally 12 prescriptions, like muscle relaxer, pain relievers and inhaler and everything you could think of for pneumonia.
That weekend, I spent in my room away from my kids because I didn’t want them to catch anything from me. And that evening, my lips started to turn blue. And at this point I was having trouble breathing, but at no point did I think that it had anything to do with my lungs — I just thought that the pain was so intense that it was affecting my breathing.
First hospital admission
Jason rushed me to a hospital where I got admitted this time. They took my blood oxygen level using a pulse oximeter and the reading was 70 or so, which was unbelievably low.
I had them retest me 3 times, with the same result each time. They rushed to provide me with supplemental oxygen, and I ended up staying at that hospital for 4 days.
At that hospital they conducted a workup and scans, including a CT scan with contrast. And that’s when the 6-letter word entered the conversation.
They said they had seen lesions on my spine, and said that they could be either calcium deposits or cancer. And since I wasn’t anywhere near 60 years old, calcium deposits were unlikely.

They did 2 biopsies — the first one was around the sternum and completely missed the area. I could feel it, feel the drill, feel everything. They were nervous about proceeding because they could hit my heart if I moved.
So the next day they drained the fluid from my right lung and conducted a second biopsy, for which they completely put me under. It was in a whole different location this time. And then they started working on getting my oxygen back.
So it was a bit of a jarring hospitalization for me. I was thankful to have been supported by my family and my church during my stay.
After 4 days, I was ready to be discharged me and to be sent home with oxygen. But they spoke with me and said that since cancer has entered the conversation, they recommended that I transfer to a second hospital, in Dallas.
You have to lead your treatment process in your journey.
You can feel like you’re just a number, given the number of patients doctors have to see.
But of course you’re more than just a number.

Second hospital admission
The second hospital was 45 minutes away by car, and my husband took me there right after I was discharged. We got in pretty quickly and told them what the first hospital had said — that we needed to have a PET scan double-time.
Lo and behold, this second hospital discovered that I had a really large pulmonary embolism, caused by a huge blood clot in my lung, which the first hospital had missed completely.
So only by the grace of God did I manage to survive. I’ll never forget the expression on the faces of the doctors.
They immediately put me on a blood thinner, and I had some great specialized care courtesy of amazing nurses and specialists like physical therapists. But cancer continued to be the main topic of conversation at this hospital.
I had to undergo scans that required me to be wrapped up like a mummy. I was terrified and claustrophobic, but I just had to go in that machine. I just had to talk to the Lord and try to be courageous, and also focused on scripture and thought about my kids.
I ended up spending 8 days in that Dallas hospital.
Non-Small Cell Lung Cancer Diagnosis
While I was in Dallas, the results had come back from the tests the first hospital had run.
They were positive for adenocarcinoma.


Reaction to the diagnosis
Initially, during those 12 really long, jarring, shocking days before my diagnosis, we just kept holding on to the hope that I didn’t have cancer. We kept praying and hoping that they really were just calcium deposits or just something else, something benign. But all the signs were always pointing towards cancer.
And so the moment that the doctor came in and confirmed it was cancer, I completely lost it. I bawled my eyes out and shook uncontrollably. It felt so, so unbelievable. And what’s worse, it wasn’t just cancer, it was lung cancer.
Because the doctor had told me that since I was a nonsmoker, if I did have cancer, it would probably be breast cancer. So I was so taken aback that it was cancer. It was lung cancer. It was stage 4 non-small cell lung cancer. It was inoperable. It was terminal. And he told me that some people in my situation would live, say, 5 to 10 years.
So a tremendous amount of fear rushed over me, and I was shaken. But I clung to my faith and knew that the ultimate physician is the one who has the final say.
As for my husband, he’s a bit of an introvert, and processes things very differently from me. I think he did a lot of his grieving outside the room. He wanted to remain strong and steady and full of faith and constant. He’s already lost his dad and brother — the latter to cancer, just in 2020, and in the low 40s, so I think there’s some PTSD there. And I think he kind of shut down.
So quite apart from me, he sat in his chair and didn’t express too much emotion. And that’s been in character with how he’s been grieving, like when the kids are asleep, we’ll lie down and sometimes cry together.
You may have big decisions to make really fast, and to do that — and to advocate for yourself — you need to be prepared.
Second opinion
I decided to get a second opinion with MD Anderson, based on their reputation.
While I still do have an open file at the Dallas hospital and can get treatment from them if I need to, the quarterback of my care team, the decision maker, would be MD Anderson.

MD Anderson had a lot to teach me. For instance, I had already heard that a particular drug I was about to take, if I were to respond well to that treatment, would work for a couple of years.
But then I learned from talking to MD Anderson that the cancer was likely to come back, that I might grow resistant to the drug in a couple of years. I didn’t know that coming into that appointment.

ROS1 and biomarker testing
I also have the ROS1 biomarker.
The topic of me possibly having a biomarker was brought up at my first appointment. Ever since then, I was really hoping that I had a genetic mutation, because I don’t want to do traditional chemotherapy at all.
So I was very happy to learn that I do have the ROS1 biomarker. And my having it has informed my treatment.
So I’ve been undergoing a targeted therapy. I’m taking a TKI drug and it’s been working really well.
Treatment, remission, and further steps
Targeted therapy for non-small cell lung cancer
I’m now in remission thanks to my first-line treatment.
Every single night, I take my TKI drug. I’ll be on it for the rest of my life.
I can’t actually handle a full dose — I didn’t even start out on the full dose, I began with three-fourths of a dose — and now I’m just taking half a dose every time.
My medicine is heavy on my kidneys and my liver, which makes it imperative that I get them to be in tiptop health.


Holistic approach
My total approach, though, is actually more integrative and holistic. I augment the solution MD Anderson has given me with solutions from integrative doctors.
I had actually quit my job so I could spend more time with my family, my kids. But another big reason I did that was also to free myself up to do things that are going to help my immune system. A lot of holistic care and integrative treatment.
I don’t think it’s all Western or all traditional medicine that helps. I believe it’s a blend of both, like you take the best of both worlds. And so I do seek out the opinions and inputs of both oncologists and experts in integrative medicine.
When your mortality is on the table and you see so many people across the board struggling with and passing away from cancers like this [ non-small cell lung cancer ], it’s like you want to throw a hundred things at the disease and not just 1. If I were to depend on MD Anderson alone, that would just be like placing all my eggs in only 1 basket. And so I would rather have multiple experts weighing in.
I think the integrative world does great at looking into root causes. They say that cancer isn’t just this tumor that appears 1 day and out of nowhere; it’s something that has been building in one’s body for maybe a decade, for example. And it’s like a perfect storm, like glucose in the body, the diet, the microbiome, the immune system, and so on.
And so I do things like taking IVs of sodium bicarbonate — which is alkaline and helps make my body alkaline too, so that cancer cannot survive in it. I think my whole mentality as far as integrative medicine goes is that I create an environment within me that cancer is unable to return to.
I went to an integrative cancer center in California for 6 weeks through Thanksgiving and Christmas last year. I entered with my oxygen tank in tow. I left without it.
Self-advocacy
Sometimes, these approaches I go for and experts I consult clash and don’t agree with each other, or with me. And, moreover, sometimes they miss things. And this is where I have to be my own advocate and discern and ask God which direction I should go.
I’ve already mentioned earlier that the first hospital I went to completely missed my pulmonary embolism, and that’s no less than life-threatening. I also have a run-in with a particular doctor to share.
So I did a blood panel and checked out my B12 levels, which were way off the charts at over 2,000. The doctor just shrugged it off, saying that it was water-soluble and thus not worth looking into. He said, it’s probably from your diet. So I paused drinking this plant-based protein shake I’d been taking, and it had no effect on the super high B12 levels.

So I self-advocate. For every doctor’s appointment I go to, I craft bullet points and an agenda to help guide our discussion. And sometimes I’ll send this agenda ahead of time and tell the doctor, hi, I’d like us to address these concerns and I want you to know ahead of time what we’ll be discussing.
You have to lead your treatment process in your journey. You can feel like you’re just a number, given the number of patients doctors have to see. But of course you’re more than just a number.
Do your research, learn from other people. At the start I was like, it’s a full time job to learn everything. But that’s how I know what kind of questions to ask. You may have big decisions to make really fast, and to do that — and to advocate for yourself — you need to be prepared.
So I’m living life.
I’m doing all the things and making all the memories.

Improving mental health
I’ve also found that there are steps one can and should take to improve one’s mental health.
After my non-small cell lung cancer diagnosis, I literally was walking in depression. I was literally preparing to die. For the first year or so, I experienced so many days and nights where I thought about dying a lot. I would just see my husband and our 2 kids continuing life. My mind would even go to events like my daughter’s future wedding taking place without me, or my funeral with my family grieving.
But I couldn’t succumb to that.
Some people in cancer groups online, for example, are preparing to die and doing things like writing their kids books so that they’ll read them in the future and get to know or remember their parents.
Sure, I’d want to write a book of my own down the line. But I’d like to do it from the standpoint of being NED.
And so I think that a lot of therapy has been necessary.
Living life
So I’m living life. I’m doing all the things and making all the memories.
I’m literally not saying no to anything, just trying to do all the fun things I can with my husband and kids.
We’re having a whole lot of fun.


Advice for others
Place your trust and have hope
The first piece of advice I would like to offer is definitely to have hope. And for me, this is based in faith.
My faith is everything to me. My experience has taught me that placing my trust in God and something bigger than myself is crucial.
I’m such a data-driven, logical, realistic person. But cancer has taught me that I have to live in the space where optimism and hope are.
Think positively and act like you’re healed
Positive thinking is massive. It may seem silly to some, but from all the research I’ve done, I’ve found that there’s so much truth to it.
It’s like our brain is telling our body what to do.
So act like a healed person. Keep living your life like you’re healed.


Advocate for yourself
I’ve said this already earlier — it’s so important to advocate for yourself, and to do so you must prepare properly.
Don’t just trust one doctor. Go get a second opinion, seek the help and inputs of other experts. Get as many eyes on the glass as you can. Especially if you have other people like kids who love you and depend on you.
And if their opinions and advice clash, seek guidance to resolve it. But build your own knowledge base too.
Support yourself both physically and emotionally
I think it’s also crucial to support yourself integratively, holistically, as you’re going through this. And emotional work is extremely important.
I’ve learned in the integrative space that emotional work matters just as much as physical work does. And not only dealing with the emotions you’re managing at present, but also with any emotional backstory, like childhood traumas, that might have contributed to your situation at present.
I’ve heard from more than one integrative provider that deals with cancer patients and has been doing so for decades. The ones who don’t survive are the ones who aren’t doing the emotional work.

Get to the root cause
If you experience a suspicious symptom just like I did with my cough, don’t shrug it off. Investigate it and get to the root cause.
I didn’t have allergies year-round — so why was I having a cough for 9 months?
I didn’t want to take time away from my work and family to do so, and besides, I thought, my cough was livable. It wasn’t really interrupting my daily life. But look at how things developed.
My cough was in itself a small thing, but it was persistent. It wasn’t allergies. It wasn’t long COVID. It wasn’t pneumonia. It was a sign that I had stage 4 non-small cell lung cancer.
Special thanks again to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.

Inspired by Ashley's story?
Share your story, too!
More Stories with The White Ribbon Project
Luna O., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptom: None involving the lungs; severe abdominal pain
Treatments: Chemotherapy, targeted therapy
Calvin M., Lung Cancer, Stage 1
Symptoms: Frequent illness (monthly cycles of sickness), breathing difficulties
Treatment: Surgery (pneumonectomy)
Jill F., Non-Small Cell Lung Cancer with EGFR Exon 19 Deletion, Stage 1A
Symptom: Nodule found during periodic scan
Treatments: Surgery, targeted therapy, radiation
Additional Lung Cancer Stories
Ashley C., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Fatigue, breathlessness, persistent back pain, multiple rounds of bronchitis
Treatments: Chemotherapy, targeted therapy
...
Loryn F., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Extreme fatigue, persistent back pain, chest pain, joint pain in the feet, hips, legs, shoulders, and elbows
Treatments: Chemotherapy, radiation therapy (foot and elbow to help with mobility), antibody-drug conjugate
...
Clara C., Lung Cancer, MSH6, Stage 4 (Metastatic)
Symptoms: Pelvic pain, joint and bone pain, breast lump, extreme lightheadedness and dizziness, vomiting, fainting spells, swollen lymph node in the neck, neuropathy, headaches, unexplained weight loss, severe anemia
Treatments: Radiation therapy to the brain, chemotherapy, immunotherapy
...
Wyatt D., Non-Small Cell Lung Cancer, KRAS+, Stage 4 (Metastatic)
Symptoms: Intense migraines, vision loss, muscle cramping in the hands, fainting
Treatments: Chemotherapy, immunotherapy
...
Ashley V., Non-Small Cell Lung Cancer, Stage 4 (Metastatic)
Symptoms: Trouble swallowing, shortness of breath, fatigue, loss of appetite, chest pain, swelling in her body
Treatments: Surgery (removal of lung), chemotherapy, immunotherapy, radiation
...
Leah P., Non-Small Cell Lung Cancer, EGFR 19del, Stage 4 (Metastatic)
Symptoms: Persistent dry cough, shortness of breath, heaviness in the chest, coughing up blood, weight loss, right rib pain, right shoulder pain
Treatments: Targeted therapy, chemotherapy, radiation (SBRT)
...









