Amy’s Stage 4 Squamous Cell Carcinoma Lung Cancer with MET Amplification Story
Amy was diagnosed with stage 4 non-small cell squamous lung cancer. She shares the importance of finding the right doctor, her experience with hyperprogression, and switching regimens mid-treatment.
- Name: Amy G.
- Diagnosis:
- Non-small cell squamous lung cancer
- MET amplification
- Staging: Stage 4
- Initial Symptoms: Lump in the neck, felt run down
- Treatment:
- Keytruda
- Stereotactic Body Radiation Therapy (SBRT)
- Cryoablation
- Crizotinib

After [telling] my story and [hearing] everybody else’s stories, my big driving force was helping others because I remember what it felt like to be diagnosed.
- Video
- Pre-Diagnosis
- Testing
- Diagnosis
- Finding the right doctor
- Treatment
- Treatment options
- How did you feel about possibly joining a clinical trial?
- Efficacy of the Keytruda treatment
- Video
- Describe the Keytruda regimen
- What did you have to do before the Keytruda infusions?
- When did you start to feel side effects?
- What helped you manage the GI problems?
- Describe the rashes
- Severe fatigue
- Other side effects
- When did you learn about the MET amplification?
- What are bone mets (metastasis)?
- Process of radiation therapy
- Changing the course of treatment
- Biomarker testing
- Targeted therapy
- Responding to the treatment
- Follow-up plan
- Living life after a cancer diagnosis
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Video

Pre-Diagnosis
Tell us a little about yourself
I grew up in the Philadelphia-Delaware-New Jersey area. For most of my life, I actually worked in oil refineries. I was pretty much everything — secretary right up to machinist.
I really enjoy riding my bike. My current job now is walking dogs and housesitting for people… Believe it or not, that’s a really lucrative business.
What were your first symptoms?
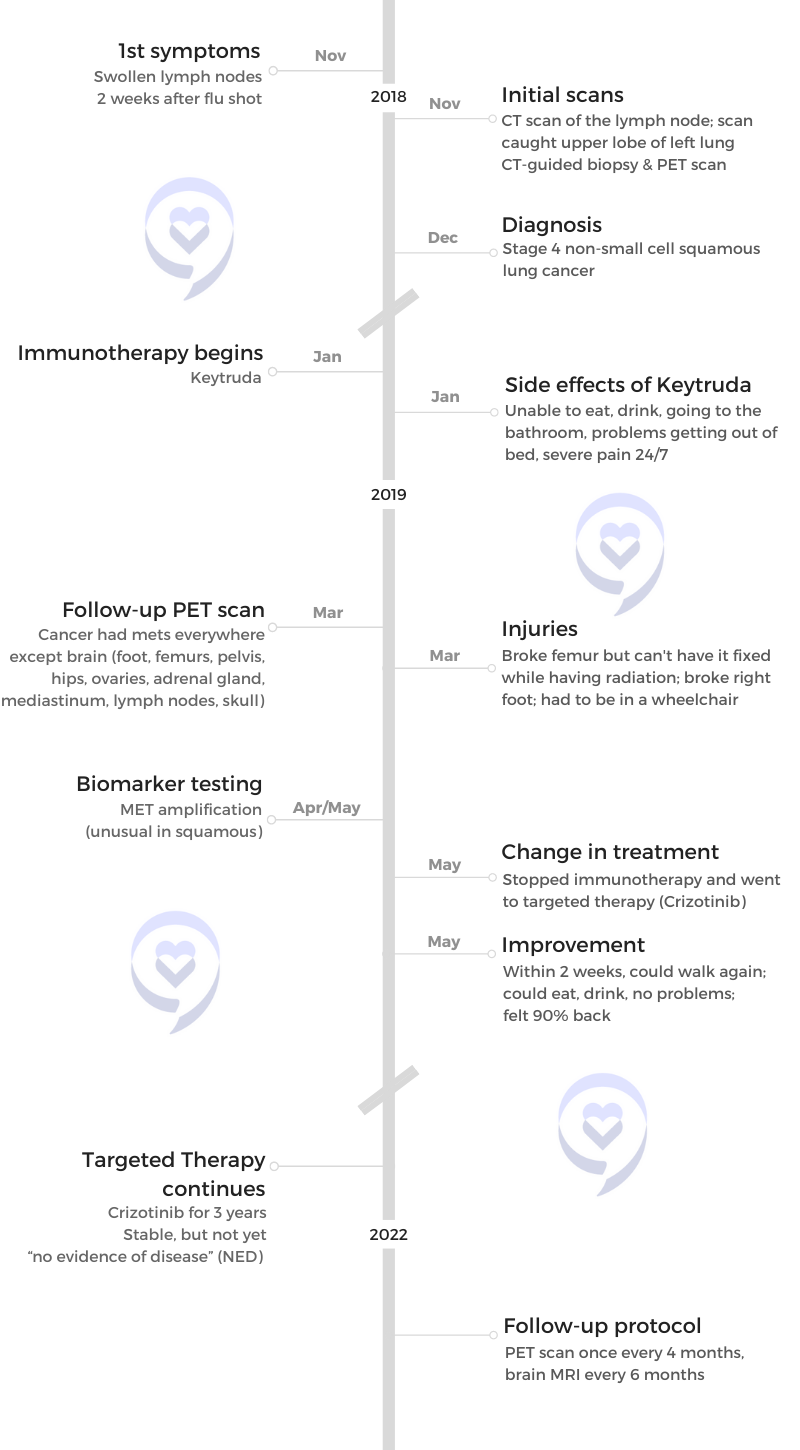
Back in November of 2018, I had a flu shot and [it was] no big deal. I’ve never had a problem with a flu shot before.
In two weeks, a lump had come up on my neck in a strange spot. I knew it was a lymph node. I just assumed that it was from the flu shot. Didn’t think it was anything more than that.
I felt a little run down, but nothing big. For about a month, it had stayed there, so I had decided I’d better go call my primary care doctor.
For some reason, I just knew. I knew it was lung cancer. I just felt it. All I could hope is that it was an earlier stage.
What did the primary care doctor say?
She originally took a blood test just to see if there was anything that would show up… The blood test only showed a small increase in my calcium; didn’t think much of it.
She decided that I needed to get a CAT scan done on my lymph node. During that time, [the scan] had caught the top of my lung, my right lung, and had shown that there was a spot there.
Testing
What’s going through your mind during the tests?
I was incredibly nervous. For some reason, I just knew. I knew it was lung cancer. I just felt it.
I had no other issues. I had always known that lung cancer doesn’t really show any symptoms until it’s almost too late.
All I could hope is that it was an earlier stage.
What were the next steps?
The next step after that was I had to have a biopsy. I had a CT-guided biopsy of my lymph node, which at that point showed that it was lung cancer, squamous lung cancer. We didn’t have it staged at this point.
After that, they sent me for a PET scan, which showed that I had it in other areas.
All I wanted to do was figure out a plan to get it going.
Dealing with the wait for results (“scanxiety”)
I’ve been kind of lucky. My doctors have had a really fast turnaround. The CT-guided biopsy took maybe 20 minutes at the most. It was awkward. I was worried.
I had results within about 5 hours. But during that time, I still knew that it was cancer.
All I wanted to do was figure out a plan to get it going.
Diagnosis
Getting the diagnosis
It actually was on my birthday in December of 2018. I was driving somewhere and my doctor had called me and said, “We have your results.” And she said, “Are you with someone or are you at home?” Right there, I [knew].
My life has been so good up to this point. All of a sudden, just one little thing turned out to be pretty major.

I said, “Since you’ve kind of let it off that way,” I said, “Just tell me now, I’m at a stoplight.” At that point, she had told me I had stage 4 non-small cell squamous lung cancer.
I had turned around and called my husband because he was at work. I’m in tears because at this point, “Oh, now it’s real. It’s really real.”
In my mind, I’m thinking, “My life has been so good up to this point. I have everything. I have my husband. I have a house. I have a dog. Everything is going great.”
All of a sudden, just one little thing turned out to be pretty major.
How did you break the news to your family?
I just told [my husband] outright on the phone. I said, “I have lung cancer.” The next thing I know, he hung up and came home. He couldn’t handle it as much as I couldn’t handle it.
I knew I had to tell my parents. My parents were the second group of people I had to tell. I didn’t want to tell my mom first.
My dad has gone through so many medical issues that I figured he’d be easier to talk to about it. I called him up on the phone. We talked for a good half hour about it. I didn’t have plans on what I’m going to be doing but he just kept saying, “It’s going to be okay.”
At this point, ‘Oh, now it’s real. It’s really real.’
Getting a second opinion
It basically was, “We have an oncologist that you can go to to discuss this.” I went to this oncologist and, funny enough, I didn’t like his bedside manner, so I decided to get a second opinion.
The second opinion basically was to get a new oncologist. I ended up going all the way to a new medical group. It’s kind of a community, but more midland. I ended up going to a pretty old university teaching hospital afterward.
I found a better oncologist who again told me the same thing he did. There was no change.
Finding the right doctor
You definitely have to have someone who not just treats you as a patient, but more can be a friend, I want to say? Somebody you can tell everything to because you’re going to have to throughout your cancer journey. You have to definitely have a doctor that you jive with.
You want to be able to ask questions. With the first oncologist, I didn’t feel like I could ask questions. It was more like, “This is what you’re going to do and you’re going to like it.” And I didn’t really want that.
[I went to the] University of Penn [and saw] a hematologist with a specialty [in] lung cancer. He’s not specifically for lung cancer, but his specialty is lung cancer.
Open lines of communication
They make it so easy to get ahold of them. It can be at 3:00 in the morning and they’ll still answer you.
[My doctor, Dr. John Kosteva,] texts me and I can text him, [but] not very often. We also do emails and we have our patient portal where it goes directly to them immediately.
Importance of access to information and knowledge
You definitely have to self-advocate. I know there [are] smaller cancer centers out there in the world where you’re not close to a university hospital conglomerate. What I would say is do take the time to go to one, even if you have to travel, but also bring the information back to your smaller cancer center so that they know that that can be done.
Treatment
Treatment options
The first oncologist had basically told me, “We’re going to do Keytruda immunotherapy. That’s what we’re going to do and we’re going to start next week.” That was basically it, which I liked. I thought, “Oh, that’s nice.”
His personality didn’t work for me. It’s almost like he had seen so many people with cancer [that] it was more of a dollar thing than it was a feeling thing.
At this time, we did not know that it was MET amplification. At this point, we only knew that it was stage 4 non-small cell squamous. He said, “The gold standard is Keytruda. Just Keytruda, nothing else. However, there is a clinical trial,” so I had to make the choice of whether I wanted to do Keytruda or the clinical trial.
How did you feel about possibly joining a clinical trial?
My fear was being new to the cancer world. I had worried [about the] clinical trial being new and not really much known about it. Whereas Keytruda had some data behind it, so I knew the side effects.
She had explained to me the better choice would be to go with what’s already known, to try that out first, and that there’s always a clinical trial further down the line.
You’ll never know whether a drug works or not unless you try it. I figured at that point, that right there was my biggest thing, was you’re not going to know how it works until you try it.
My doctor had handed me the paperwork: one for Keytruda [and] one for the clinical trial. The clinical trial was actually a lot thicker than the Keytruda one.
The side effects that were for Keytruda were your normal digestive issues, rashes… [there were] some funny ones in there.
As it turned out, I ended up having hyperprogression, which is also a side effect [that] had happened to me.
Efficacy of the Keytruda treatment
I had heard about [Keytruda] because six months before, they had the ads on TV. It kind of pushed my thought that, “Wow, these people are doing really good. That’s going to be me. It just has to be me.”
The way they explain it is that a lot of people do very well on Keytruda. I don’t remember the same exact numbers, but it was high. It was high enough for me to say definitely. Try it for that.
Video

Describe the Keytruda regimen
Keytruda was done by infusion. Every month, I would go into the cancer center and they would just infuse me with Keytruda. It took half an hour. It wasn’t long at all.
Right after the Keytruda, I would get a shot of Xgeva, which is a bone strengthener because, at this point, we had found out that I was starting to get bone mets so he didn’t want me to break any bones. The Xgeva was important as well.
What did you have to do before the Keytruda infusions?
Usually what they would do is they would do the labs to make sure that your liver and your kidney and everything is working like [they’re] supposed to [work]. Then I would see my doctor and after that, I would go to have my infusion done.
When did you start to feel side effects?
The first time I had the first infusion, I had a panic attack when I got home. I’m kind of funny when it comes to drugs [where] you don’t know what to expect, so I tend to worry about it and it caused my own side effects.
I had a panic attack the first time and then about three days afterward is when the GI problems would start. The rashes started about a month afterward.
What helped you manage the GI problems?
When I first started having the GI problems, I had texted [my doctor] and they have a nurse navigator there who pretty much will answer all the questions. They prescribed me several different types of nausea meds [as well as] several different diarrhea medications along with anything I could get off the counter. Basically, they would throw everything at it and use what worked.
The nausea medication worked fairly well, but I noticed that I also had a funny taste in my mouth. I ended up going and getting something called Tummydrops, which are peppermint hard candies, and [they] worked very well to get rid of the nausea.
It was funny because my mom had come up from Florida, so she was trying to take care of me. She would always want to feed me and I wanted nothing to do with eating anything. I’ll take a popsicle and that’s it.
I had this sugar rush for a while because all I could eat was ice cream popsicles. That’s the only thing my stomach could handle.
[That lasted] the whole time I was on Keytruda.
Describe the rashes
I had a rash on my chest and a little bit on my legs. They itched real bad. I ended up using Aquaphor, which worked well. I also had steroids, in case I needed to take that. I never really did because it never got that bad.
They would break open. Almost blistery type. [It was] more of a nuisance.
It never went away. It always stayed there until I stopped Keytruda. Once I stopped that, it went away.
Severe fatigue
[There was also] severe fatigue. But I couldn’t figure out if that was from the drug or from me not eating correctly. I wasn’t sure what it was.
My doctors were on top of everything. All the medication they thought I might have to have was already ready for me.
Other side effects
Another side effect I had — that I honestly don’t know if it was because of my age — it seemed that Keytruda stopped my period. I now had a weakened urinary tract, so I would pee. I would always have to wear diapers just so I didn’t do that.
The only other side effect I had, which was helped by something called Silvadene, was I did get burned. I did have [burnt areas] in my groin area. But the doctor previously had prescribed me Silvadene because they knew that might happen.
The good thing about my doctors is they were on top of everything. All the medication they thought I might have to have was already ready for me.
When did you learn about the MET amplification?
That happened on my last infusion of Keytruda. The doctor had decided to take some blood to do the biomarker testing to see if I had any.
The strange thing, he had told me, is that there usually [aren’t] a lot of people with biomarkers that have squamous lung cancer. I didn’t think anything was going to come back. It took a couple of weeks to get it back.
Back then, I think it was a 6- to 8-week wait till you found out. And that’s when I found out that I had MET amplification and I couldn’t have been happier.
What are bone mets (metastasis)?
[Bone mets] basically means the cancer is in your bones. It’s eating it. It’s the best way to explain it. They can break very [easily].
[I had] extreme pain. No amount of opioids or anything could help that pain. We tried. Nothing worked. The opioids did help to let me sleep more so I could avoid the pain sleeping but you still had that pain constant.
It is [really tough], especially where I had them. I had them in my femur. I started off with a cane, then I went to a walker, and then I ended up in a wheelchair. It was bad [for a] period of about a month and a half.
Side effects of Xgeva
Not that I noticed. The only thing was a pain in your arm… and it was pretty bad. It wasn’t your normal [when you’re given] a shot [and] it hurts. No, it was bad in the arm. But other than that, no side effects that I could tell.
If you have pain and you’re a cancer patient, get the opioids.
Opioids for cancer pain
On top of that, I was taking the opioids for my own metastasis. I was taking something called Xtampza, which is a long-acting oxycodone. I was taking oxycodone for breakthrough and I was also taking Ativan to help. There was a lot.
I had asked my doctor, especially about the opioids. He said in most cases, a lot of cases, cancer patients, especially stage 4, do not get addicted to opioids.
If you have pain and you’re a cancer patient, get the opioids. Don’t be worried about getting addicted. I never did and I was taking them 24 hours a day. I had no issue.
As for taking any other drug, it kind of comes with cancer. You have to try it and just know that there are doctors and medications that can help you get over that hump.
Video
Process of radiation therapy
The radiation therapy was about a month.
It was during the time I was on Keytruda, about [midpoint]. At the time, I had started getting a met in my femur. We didn’t know how bad it was, but the radiation was done on my hips and my femur at that time.
It was an easy process if you want to say. They build a mold around your hips so that you won’t move. There was no pain associated with the actual radiation itself [but] because of the bone met in my femur, the pain was incredible but had nothing to do with radiation.
[The radiation session] was every three days. [Each session lasted] about half an hour. It took me more time to put on a gown because I could hardly move. I was in a wheelchair. I couldn’t take my clothes off. My mom had to help me.
My doctor decided that Keytruda wasn’t working. We have to try something else.
Changing the course of treatment
What drove the decision to take you off Keytruda?
I was on it for three months and the catalyst was my third-month PET scan, which showed I had it everywhere. Besides my lymph nodes, I had it in my shoulder, I had it in my adrenal glands, my ovaries, my ribs, my fingers, my hips, my femurs, and one foot.
At that point, he decided that Keytruda wasn’t working. We have to try something else.
Dealing with the news emotionally and mentally
It was hard. Just based on how I felt physically, I thought that April of 2019 was my last day or last month on Earth. I felt so bad.
When the doctor told me that, I thought, “Well, that’s it. I might as well get everything in order. Do what I want to.”
Just tell me how long I have. That’s all you thought about. Constantly, 24 hours a day.
I had slipped into a severe depression. I had asked my primary care doctor to put me on antidepressants.
In the meantime, I was still on Ativan because that helped with my anxiety. They switched that over to something called BuSpar, which helps my anxiety as well.
It was not only physically did I think April was my last month. Mentally, I wanted it to be my last month. I was not only just in that amount of pain, it was the whole, “How long do I have?” Tell me that. Just tell me how long I have. That’s all you thought about. Constantly, 24 hours a day.

The antidepressants definitely helped to pick me back up and make me more hopeful.
I couldn’t sleep, even though I was forced to sleep. You didn’t really sleep well. There was no relaxing. I would go to the grocery store and say, “What’s the point of doing this? Why, why, why? There’s no point.” Even everyday things just seemed pointless.
The antidepressants definitely helped to pick me back up and make me more hopeful.
Was there anything else that helped with the depression?
The biggest thing that helped was Facebook. I found a bunch of lung cancer groups and there were people that had been through it. Same thing as I’ve been going through.
Over time, after I told my story and heard everybody else’s stories, my big driving force was helping others because I remember what it felt like to be diagnosed. To put it out there, to help other people get through that, and know that they have a chance really, really made my life more worthwhile.
I did nothing but sleep all day. Everything hurt.
Biomarker testing
How did you deal with the scanxiety?
I grew up with a mother who always told me that you can’t worry about things [where] you don’t know is going wrong. It’s only going to hurt you more than anything. I’ve always tried to live by that.
I don’t really have anxiety but waiting for the biomarkers was a little testing because, at this point, I had lost so much weight. I was down 40 pounds.
I did nothing but sleep all day. Everything hurt. I had a rash covering my chest, so I really needed to get off Keytruda.
Getting the biomarker results from the doctor
[My doctor] said, “It’s rare that squamous has a biomarker, but you have it. And the good news is that there is a drug that works for it.” I was so excited and I’m like, “Oh okay, how long do I have to sit in a chair?” He’s like, “No, it’s a pill. You take a pill, a pill twice a day,” and I’m like, “Oh, this is great!”
Then I said, “Okay, well, what’s the side effects?” He started explaining to me and I’m like, “All right, they’re not that bad. It seems like the Keytruda ones were worse.” I thought, “All right, I’ll try it.”
[The] fact that it’s a pill now just thrilled me to death because now I didn’t have to travel back and forth and worry about all that. I could take it at home. Best thing ever.
Targeted therapy
Difference in quality of life with the pill
When you tell people about it, they’re like, “That’s not possible.” Yeah, it is. Yeah, I take a pill. People that are new to lung cancer don’t know that there are pills that you can take to help keep it at bay.
Importance of biomarker testing
[Ask those questions], absolutely. I’m still trying to learn at what stage they will do biomarker testing because I think they don’t really want to do it on the stage one, stage two. Three and four, more than likely they will do it.
I’m hoping that they start doing that earlier because it makes more sense. But that’s out of my hands at this point.
Side effects of Crizotinib
The first week, I was put on 500 mg — one pill in the morning and one pill in the evening. I started having very bad GI issues again and I’m thinking, “Oh, here we go.”
My doctor got the smart idea. “Let’s cut you in half.” I said, “Okay,” so I only take one pill a day.
The only side effect I had, and I don’t know how to explain this, is if I went from dark to light, I would have like a trail. I could see the door going sideways for a little more than it should. I don’t know how to explain that. It was strange but I thought, “Oh, this is all I have to deal with. I can do this.” It only happens sometimes.
It does cause visual disturbances. They don’t really explain that so much. You could lose your eyesight, which I didn’t have that problem with, so I just had those trails.
It lasted for about a year.
[I told my doctor] and he said it was normal for Xalkori or Crizotinib. If it got worse or it became where I was starting to lose my eyesight, then we would have had to do something different.
I did [check in with an optometrist] because I had to get my eyes checked anyway. In the meantime, I told them about trails and that it was probably a side effect of my drug. They didn’t see anything in my eyes to say, “Okay, you’re going to lose your eyesight.” There was nothing there.
GI issues with Crizotinib
It was mostly vomiting and some diarrhea, but it ended up being diarrhea for like a day. Then it was constipation for days on end.
I tried everything — and I mean everything — to get rid of the constipation, which was harder than stopping the diarrhea.
[I tried] everything in the store. I tried prunes. I tried prune juice. I used to have milk intolerance or lactose intolerance, so I would drink massive amounts of milk, eat a lot of ice cream, thinking that’ll loosen it up. No, nothing, did nothing at all.
If you’ve ever seen raccoons when they have their babies, they tend to rub their stomachs, lick their stomachs. I was actually pushing on my stomach to get it moving, which worked but not easily.
The GI issues went away immediately along with all the other things.
SBRT and cryoablation
SBRT is stereotactic body radiation, which means you get stronger radiation to a smaller spot instead of the whole area. I had five SBRT sessions on my lung to shrink [the tumor], but we wanted to kill it. Who knows? It might be dead. It may not.
As for the cryoablation, that is interesting. You go into a bit of a twilight. It’s like three needles or so. They go in and they freeze the tumor on your adrenal gland.
It only hurt for a second, but when I banged on the table, the nurse knew so she upped my twilight a little more. I couldn’t talk. For some reason, the words wouldn’t come out, so I just thought I’ll bang on the table. So if you ever do encounter that, bang on the table.
I had no pain afterwards. There was no recovery time or anything to it.
The SBRT was done five sessions one time so it was over five days. Then the cryoablation was done once and that was a one-shot deal.
Responding to the treatment
In April of 2019, I thought I was gone. The first week of Crizotinib, it was a little rough. The second week, all of a sudden, I felt like a new woman. I had no pain, no lumps anywhere, and just felt like I did before I had cancer. I knew, at that point, that the Crizotinib was starting to work.
It’s such a great feeling to know that it worked that fast and even my doctor really couldn’t believe it. It doesn’t seem possible. But the fact that I could feel it. It wasn’t just my brain saying, “Oh, you feel better because you’re taking [medication]…” like a placebo effect. It wasn’t that at all. I knew I physically felt better. I mentally felt better. I knew. It was a good drug.
I could walk again. I was out of the wheelchair. [I could] eat and drink [with] no problem.
I felt like a new woman. I had no pain, no lumps anywhere, and just felt like I did before I had cancer. I knew, at that point, that the Crizotinib was starting to work.

Feeling somewhat like yourself again
You have the hope. You’re thinking, “Wow, I physically feel like that or mentally feel like that. I can live like this. I can go about my everyday life and enjoy things again.”
I just kept calling it the miracle drug. Even my family, my family called it. They’re like, “Ame, you were stuck.”
I could not walk up the stairs to take a shower, so I hadn’t taken a shower for almost six months. I didn’t sleep in my bed. I slept on the recliner downstairs and only slept lying on my back because [of] my femur.
Everything was broken at the time. [I] had all the issues. But it’s [a] miracle drug.
I keep going and asking [my doctor] if I’m boring… He said I’m the fastest turnaround he’s ever seen.
Follow-up plan
Follow up with PET scans
[I have a PET scan] once every four months now. Back then, it was once every three months for a PET scan and then once every six months for a brain scan, for an MRI.
The PET scan, after being on Crizotinib for three months, came back and the doctor was like, “Look at this!” He showed me on the screen and he said, “This is what you look like before. Look what you look like now! This is gone. This is gone.”
I was just thrilled. I was like, “Oh, I knew it.” I said, “The way I felt physically, I knew it had to have been doing something.”
I’m mad that [my body] didn’t let me know before I had it, so I knew ahead of time to push my doctor more about the symptoms. When I think back now, the pain in my shoulder a year before I got diagnosed probably was a symptom of lung cancer [but I] didn’t know it.
Right now, I believe [they’ll be doing the brain MRI] indefinitely. The PET scans are now [every] four months. I did go up once and that’s indefinitely as well.
I’m stable. It hasn’t grown and that’s all I want to know.
Stable but not yet NED (no evidence of disease)
At this point, I still have a light up in my lung and a light up on my adrenal gland. But again, the doctor said that could be dead tissue or the radiation may still be working and we just don’t know. I’m stable. It hasn’t grown and that’s all I want to know.
I continue on Crizotinib until either it stops working or becomes toxic. Right now, I’m stable and I’m happy to say that’s what I am and I hope it continues to work. We’re on three years of stable, so that’s a great thing.
The Facebook page [of lung cancer groups], you tend to get attached to some people and you think, “Oh, they were diagnosed the same time I was.” Then you realize that they passed and you just don’t understand how they did when they had the same exact cancer as you. So to think that I’m alive is wonderful but sad in that effect.
I know [my doctor] talks to his tumor board regarding me. I don’t know how often. I’m assuming every time I have a PET scan, he’s like, “Well, she’s still boring.” We’re hoping — knocking on wood now.
Crizotinib’s been around for a long time. That was one of the first targeted therapies they had come around with, I believe it was maybe 2013 it came out. Could be wrong on that date, but it’s still been around for a very long time. But the squamous with a MET amplification is a shocker.
Never give up and always hold on to that hope.

Living life after a cancer diagnosis
You definitely have to enjoy every day; actually, every second. Even the bad stuff, you still need to enjoy it because it may not be there for long.
Also try not to be nervous about your scans. It’s not going to help anything at all and may actually make things worse. If you’re really, really upset and your anxiety is through the roof, definitely call your primary care doctor to have help with that.
Never give up and always hold on to that hope. If you don’t like an answer a doctor gives you, try another one. Get a second opinion. Get a third opinion. You have time. You just have to find the right doctor.
Just hang on to hope.

Inspired by Amy's story?
Share your story, too!
Non-Small Cell Lung Cancer Stories
Maggie M., Non-Small Cell Lung Cancer, EGFR+, MET Amplification & Overexpression, Stage 4 (Metastatic)
Symptoms: Ocular migraines (kaleidoscope vision), partial blood clot (DVT) in the leg, vision and balance problems, minor chest pain
Treatments: Targeted therapy (tyrosine kinase inhibitors or TKIs), radiation therapy (stereotactic body radiotherapy or SBRT), clinical trials, chemotherapy (combined platinum-based regimen)
Clara C., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Pelvic pain and discomfort, bladder issues related to pelvic tumors, incontinence, pain in the lower back and hip
Treatments: Chemotherapy, immunotherapy, radiation therapy, targeted therapy (lorlatinib)
Shira B., Lung Cancer, EGFR+, Stage 1B
Symptoms: None per se; discovered during a preventative full-body MRI
Treatment: Surgery (thoracotomy)
Phil P., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptoms: Persistent cough, nasal drip, shortness of breath, inability to speak in full sentences
Treatments: Chemotherapy, targeted therapy, radiation therapy, next-generation ROS1 inhibitor (clinical trial)
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy