Joanna’s Stage 3 Rectal Cancer Story
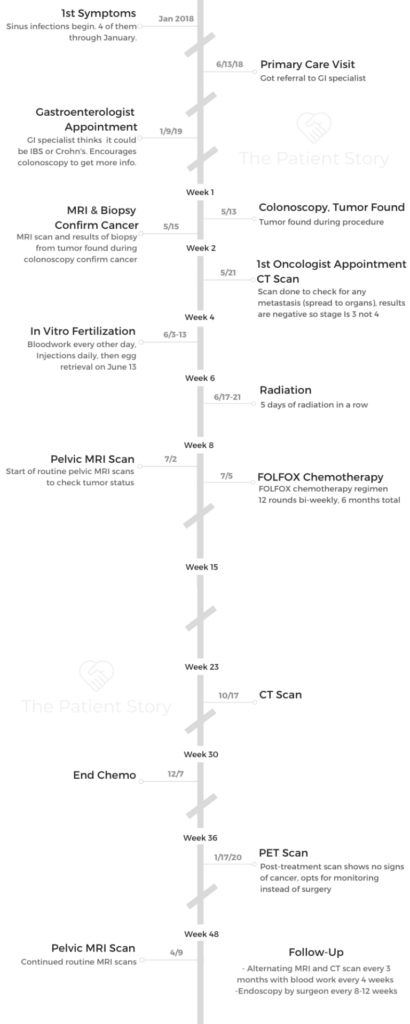
Joanna shares her stage 3 rectal cancer story, which start with fertility preservation before she underwent radiation therapy and chemotherapy.
In her story below, Joanna shares the issues she had to navigate after her rectal cancer diagnosis, including how she got through in vitro fertilization (IVF), managing through changes to her hair, tending to her mental health, and transitioning to survivorship.
- Name: Joanna H.
- Diagnosis: Rectal adenocarcinoma
- Staging: 3
- 1st Symptoms:
- Rectal bleeding
- Bloating
- Stomach aches, eventually after every single meal
- Treatment:
- Fertility treatments
- Successful egg retrieval surgery
- Radiation
- 5 days of radiation treatment (in a row)
- Side effects: GI symptoms, bladder issues
- Chemotherapy
- FOLFOX
- 12 rounds biweekly
- 6 months total
- Fertility treatments

- First Symptoms and Colonoscopy
- Dealing with a Cancer Diagnosis
- Cancer Treatment Decisions
- Next steps after the diagnosis
- What happened before getting an MRI?
- How do you stay still during the scan?
- How do you decide where to go for cancer treatment?
- Meeting your medical team
- Impact of radiation on fertility
- Advice for others on preserving fertility
- What goes on during IVF?
- What are the IVF side effects?
- Getting help paying for IVF
- Radiation and Side Effects
- FOLFOX Chemotherapy and Side Effects
- Post-Treatment Monitoring
- Quality of Life
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
It’s like a seesaw in a way. I feel really strong some days. Some days I don’t. I think it’s being okay with that.
Allow yourself to give yourself some grace that it’s going to be a bit of a roller coaster the first couple years, but to be okay with that. I’m allowing myself that because it is traumatic to go through cancer.
Joanna H.
First Symptoms and Colonoscopy
Describe the first symptoms
From the get-go, I started to experience blood in my stool. It started a little bit here and there and got progressively worse over the course of a year and a half until I was diagnosed. I also started to experience stomach aches and bloating. I really wasn’t able to identify it until I actually got into the GI doctor.
I would eat just about anything. It started out usually triggered by dairy products. Then by the time I was diagnosed, just about anything gave me a stomach ache and/or that really uncomfortable bloating feeling for a couple of days.
What made you go to the doctor?
It got to the point where I was actually almost unable to eat anything.

If I had something to do that day, a meeting at work and/or I had to teach a fitness class, I would restrict what I would eat so much because I knew that if I ate, I wouldn’t feel good.
By having that something to do, I would just avoid doing it — eating — so I could go about living my life, which really isn’t living your life. It was pretty terrible. It got to the point where even eating salads would give me that really uncomfortable bloating feeling.
Problems scheduling appointments
I contacted my gynecologist first. I’d lived in St. Louis for almost a decade and had the same gynecologist for years, so I talked to her first about it. She gave me the referral to the GI. Unfortunately, it took me almost 6 or 7 months just to get into the GI doctor.
That was just scheduling issues. That’s really what it was. They couldn’t get me in until 6 or 7 months later. I decided to stay within that same hospital system.
I experienced an inability to access health care. It’s hard to make appointments with certain specialty groups.
Advice to others in getting treatment
I was pretty lucky. I teach at a local cycling place, and several of my regular riders or members actually worked at one of the hospital systems that I was trying to access and get a GI appointment.
One of them worked in the president’s office, so I was lucky enough to just share my story and my difficulty with having to get into an appointment.
That morning I woke up at 4:30 a.m. and felt terrible. I had a terrible stomach ache and had to teach a 5:30 a.m. class, so I relayed this to him after my class. He basically took the matter into his own hands. I was able to get in even sooner than the January appointment.
I still had to wait 6 or 7 months. I was actually going to have to wait almost 9 months to get in. It sounds like there’s no way, that’s impossible, but that actually is what happens.
What’s really unfortunate is that with COVID, it’s going to be even longer. It’s actually a real issue in certain health care systems.
Describe the GI appointment
I finally got into the GI doctor. She was wonderful. At first, it was the same thing: it was IBS, potentially Crohn’s. She was the first one that told me maybe I had Crohn’s disease because I had relayed to her, “I’ve cut out gluten, dairy. What do I do? I don’t know what else to do right now.” She said, “You most likely have Crohn’s disease. Let’s get in and see through a colonoscopy.”
She wasn’t sure if insurance would cover it. I pushed for it and said, “Regardless, if they don’t, I’d like to have this colonoscopy to see what is going on.” I’ll be honest, not once in this entire journey from about January 2018 until May 2019 was the word “cancer” ever discussed.
It just never crossed anyone’s minds that I would have cancer.
I went in and had the colonoscopy, and that’s when they discovered that I had a large tumor in my rectum.
It took a while to get a colonoscopy
I was supposed to have a colonoscopy in March, and then I ended up having something happen with work. Once again, not thinking I have cancer, so I had to reschedule.
The next appointment I was able to get was that May 13th appointment. Kind of wild. I look back and think, “What I would do to have gotten it done in March.” But it just is how it happened. There was another 2-month wait or so to get the colonoscopy.
How did you prepare for a colonoscopy?
I don’t mind the prep, I’ll be honest. I had read every article or blog about it. Everything was so negative about it, so I had a negative attitude about it.
I’ve since had another colonoscopy. I have preps; I have CT scans. I think just having an open mind about it is that it’s 24 hours of your life, and a colonoscopy will allow you to have real answers if you’re having that severe GI problems. This is the way to go to rule out anything.
For the prep, it really wasn’t terrible. I feel it wasn’t that awful. I’m sure the majority of people feel it’s absolutely terrible, but just have an open mind when you’re going through it.
Every prep’s a little different, but the ones that I’ve had is a thicker liquid. You put water with the liquid. You drink it. I did 2 different preps. I think they were 8 hours apart from each other.
Essentially, it’s clearing out your system so that they can go in and do the procedure for the colonoscopy. You’re not allowed to eat for 24 hours before you have the colonoscopy.
You could have broth. There’s certain jello you can have. Make sure to google the colors you can not have (I believe it’s red, purple, blue), so stay away from certain jello.
Just be prepared. Make sure you ask the questions when you talk to your nurse practitioner, who’s going to call you a couple days before. They are very strict on what you can and cannot do.
What happens during a colonoscopy?
They put you under. I know my first colonoscopy was not long at all. They immediately found a tumor. Then my second one I’ve had post-chemo treatment, that one was a little bit longer, 15-ish minutes.
It’s a very quick routine procedure and really nothing to be too nervous or scared about in my opinion.
Dealing with a Cancer Diagnosis
How did the gastroenterologist tell you about the tumor?
She said, ‘We found a tumor. We are not sure whether or not it’s cancerous.’
I initially did not cry. I was in shock for a couple of hours. I think what’s so scary about that diagnosis piece is that they diagnose you and say, “We found a tumor. It could be cancerous.”
Then you start to ask questions because that’s what you do as a human. They really can’t answer anything because their specialty starts, and another specialty begins.
I’m an attorney, so I understand that from a legal perspective, they don’t want to say anything that could potentially harm them and their medical license.
But I think from the patient perspective, it’s really difficult because you do have all these questions. I think that’s what makes cancer so difficult in the beginning. You have all these questions, and then there’s more waiting… to get to the oncologist, to see the radiologist.
That was what was hardest for me in the beginning. Once I found out I likely had cancer, I couldn’t ask questions for almost 10 days.
»MORE: Patients share how they processed a cancer diagnosis
Dealing with a cancer diagnosis
I truly believe people enter your life for certain reasons. Sometimes we don’t immediately see it, but life kind of unfolds, and you’re able to understand those relationships.
I had met a woman in February who became instantly a best friend of mine. She had lost her mother to colon cancer when she was 19, so about 15 years prior. When I met her in February of 2019, she had just lost her best friend to stage 4 colon cancer. She was actually with me.
My husband is a corporate attorney. Again, we thought nothing was wrong with me in terms of cancer. He dropped me off at my colonoscopy and was going to meet me back at home that evening.
She picked me up from the colonoscopy and was actually there when I woke up. The doctor told us together. Once again, it was a newer relationship, but we instantly bonded. I just feel so lucky to have someone who was so experienced not only with cancer, but my specific cancer.
I really relied on individuals right away who had cancer. I almost immediately got involved in the cancer community. I have a dear friend and mentor who’s very well known nationally and internationally with the community for colorectal cancer. I met with her almost immediately.
Building those relationships and asking those important questions before I even met with my oncologist was a huge way in which I gained back control at a time when you feel almost hopeless. You feel you have no control.
Advice on handling a cancer diagnosis
One in particular in terms of colorectal cancer — I know immediately, and I know if someone watches this, they are immediately going to resonate with this. When I was pretty sure, after they told me they thought it was cancer, I went home and Googled it. I had almost every symptom. I was textbook rectal cancer.
My husband and I were pretty sure I had cancer. It was just a matter of whether it was stage 3 or stage 4. Something that I almost became borderline obsessed with was, “What am I going to look like pre-cancer, during cancer, and post-cancer?” Something a lot of colorectal patients have to deal with is an ostomy or ileostomy bag.
You never know what direction your cancer’s going to take. My best advice I received from a dear friend was, ‘You need to focus on the here and now, right now.’ Here and now, at that moment, was finding the right oncologist to see. It was not having sleepless nights worried about a surgery that might never take place.

That is something I know got me through cancer. I think receiving that advice from several people who went through this already was just huge, because we don’t know. If it’s going to happen, it’s potential. It might not happen.
For me, asking that question of, “What can I expect?” The answer was really awesome. It was, “You can expect X, Y, Z with chemo, but everyone’s journey is different. Don’t compare your journey with someone else’s, especially in the beginning.”
Focus one day at a time. I know that sounds so cliché, but it really forces you with cancer to do that. I can’t worry about something in 9 months. I have to worry about today and what I can do to receive the most information to be the most informed cancer patient.
»MORE: Read different experiences of a cancer diagnosis and treatment

The importance of find your cancer community
I always heard it when I went to law school: “Don’t reinvent the wheel.” Make sure in practice and in law school that you’re constantly reaching out to mentors. I think there’s so much value in having people around you that have gone through maybe not the same situation, but they’ve lived, so they’re wise.
When it comes to cancer, don’t reinvent the wheel.
I think the first thing a lot of people should do is reach out to their local hospital and find if there’s a community of cancer patients. Who’s the best doctor?
You’re probably not going to be able to find that answer via Google, but you’re going to be able to find it in relationships or meeting with people who’ve already gone down that path. Then you’re getting real-life testimonials from people who’ve had that doctor.
That’s how I found my doctor. I called almost every person I knew that had some connection to the cancer center here in St. Louis. It made a world of difference, because he was exactly the doctor I needed based on what people had told me [about] his demeanor and what to expect from him.
From the get-go, people should be really advocating for themselves by forming relationships with people in the cancer community.
»MORE: Join other patients and caregivers on The Patient Story social media community
Cancer Treatment Decisions
Next steps after the diagnosis
I had an MRI with that same health care system that diagnosed me. The MRI and biopsy confirmed that I did have cancer. It was not benign; it was cancerous. After that, I went to my oncologist in the cancer center at a different hospital system.
I remember everything was so scary in the beginning.

They weren’t able to get me in right away. I had to wait maybe 2 days. For me, that felt like forever. I had to go to an appointment. My MRI was at 6:15 in the morning. They made a special time slot to get me in. I just remember it was so scary.
It was almost like Caleb, my husband, and I couldn’t even think straight. We couldn’t even find the MRI area. We couldn’t think about what we were doing.
I remember that technician was wonderful. He explained everything to me once he found out that I was new to this. That really confirmed that I did have cancer, like I said.
That was scary. I thought to myself, “Okay, I have cancer.” But then it almost gets worse in a way, because you have to do a CT to confirm it’s not stage 4. Then you get staged.
There’s a lot of check-ins that I think people who haven’t gone through cancer don’t realize exist.
What happened before getting an MRI?
For the MRI, you have to have a contrast. It takes roughly 30 to 45 minutes. Some people have a hard time with the contrast. I am one of them; I get extremely nauseous from the contrast.
Most people thought, “It’s nothing.” You just have to sit very still, so if you have any type of back issue, it might not be the most pleasant experience for you. You have to sit still.
How do you stay still during the scan?
I request headphones with music, and I would recommend very deep breathing, almost meditative breathing, when you do it. Especially in the beginning phases of a diagnosis, there’s something about going into these procedures and scans that you’re anxious, scared.
Not only do you have to go through a lot of steps, but you then have to wait for the news. I would say anything you can do to make the experience — I won’t say “enjoyable,” but get through it. I would request music.
I would say to take a deep breath. I know that sounds like, ‘How can you do it at that moment?’ But that’s my best advice. It’s something I tell myself every time I go to the hospital, which is almost every month now.

How do you decide where to go for cancer treatment?
I went to a different hospital system. Immediately, my husband and I Googled cancer centers. Luckily, I had worked at this hospital system in the pediatric side years prior, so I knew that Siteman Cancer Center was one of the top cancer centers in the country.
In terms of finding my doctor, when I saw him, that was from word of mouth. We contacted as many friends as we knew that had [been] in and out of cancer. We asked, “Who do we go for colorectal cancer in St. Louis?” By the luck of God, we received the same person’s name over and over.
Just to us, that was a sign of that’s where we need to go and who we need to see. Once we found that insurance was going to cover it, that I was in-network, it was an easy decision. I switched health care systems, and I was able to get into him about 8 days later.
Meeting your medical team
They didn’t know what stage I was, so I had to do a CT in the morning. Then we met him (oncologist), as well as the radiation oncologist and surgeon.
Something I think a lot of people should be aware of is that, especially when it’s dealing with advanced cancers, you are going to meet the entire team. That was new to us. We had no idea.
After I had my CT scan, I met the radiation oncologist. I didn’t know I’d be meeting him that day until I got there.
In that same meeting, the surgeon was sitting with us as well. We talked to them for about an hour and a half. They exited, and then my oncology team came in. My doctor, my nurse practitioner, and my nurse coordinator — the whole team.
We were there, between the CT scan and finally leaving, close to 6 hours.

Impact of radiation on fertility
That was really scary because of a couple things they told me that, again, we didn’t think about. I was told I would for sure have to go through radiation and because of the radiation, I would not be able to likely have children.
If I was able to get pregnant, I would likely not be able to carry them full term. That’s something as a young adult female, you have to be aware of that.
The better equipped you can go into a meeting like that, the more emotionally stable you might remain. That was really difficult for us because we hadn’t thought of it.
Advice for others on preserving fertility
If I could give one piece of advice, I would say to really push your doctor on that. Once again, it’s not part of their specialty. It’s not that they don’t care about that, but they are so focused on getting you to be cancer-free to continue to live that it’s not top of their mind. I’m so glad I pushed my doctor on that and was able to go through IVF.
»MORE: Fertility preservation and cancer treatment
What goes on during IVF?
My oncologist was not against me going through fertility, but I almost had a full obstruction in my rectum, so he wanted to start radiation the next week. I was able to find a fertility doctor. He said, “If you can find one soon, start the process of IVF. I’d like to see you back in 3 weeks.”
Luckily, through word of mouth, I was able to find an incredible human who’s a fertility doctor. I was able to get in the next day, so I started IVF (June 3). How my fertility doctor did it, which I’m assuming is pretty normal and pretty regular across all organizations, is they start a group of women together for their egg retrieval. I started June 3rd and had egg retrieval June 13th.
It involves a lot of blood work, a lot of visits, a lot of injections. But all in all, I thought the process of 10 days for me was very quick. I would expect somewhere from 2 to 4 (shots) depending on the day, so more shots toward the end. Several different drugs.
What are the IVF side effects?
The main side effect I experienced was just an imbalance in my hormones. I really didn’t feel like myself in terms of hormonally functioning like I normally do. I felt pretty emotional. Very, very common side effects.

[There were] 10 days worth of shots, and then I went in for the procedure. You’re not fully out. You’re aware of what’s going on, to a degree. I remember the procedure being about 20 minutes. You’re in; you’re out. Unfortunately, I developed ovarian hyperstimulation syndrome (OHSS). I was pretty bloated and pretty out of it for a week or 2 while my ovaries settled down.
The reason that was the case is that they shot me with a little bit more hormones because I started radiation 4 days later. They wanted to make sure that they were successful. It was a high-risk case. If you have that tight timeline, just make sure that you’re well versed and well educated on what can happen during IVF, because there is a risk of that syndrome happening.
I thought overall it was a really good experience. I’m very thankful I was able to go through that.
»MORE: Read a patient’s detailed IVF journal
Getting help paying for IVF
If you are diagnosed with cancer, advocate for yourself when you call a fertility clinic. A lot of fertility clinics offer what they call “rescue retrieval,” so a portion of your bill will be comped — essentially their gift to you — as well as some storage fees that go along with that.
Radiation and Side Effects
The cancer treatment plan
The CT scan was in place to determine if I was stage 4, meaning the cancer had metastasized to another organ. That was confirmed that it had not. We got that confirmation about a day later.
That’s when they really mapped out a plan for me. It’s amazing how quickly they work once you’re actually in an appointment. I was told 5 days of radiation. We will not do surgery until chemotherapy is over. That is different by hospital system.
How do you prepare for radiation?
Our hospital system does surgery post-chemotherapy. Then I was told I would do 12 rounds, 6 months of chemo, as long as my body allowed me to keep the chemotherapy going. Then I would do surgery. I was told I was 100% a surgical candidate. I would have surgery after chemotherapy.
What I learned from talking to other individuals who’d gone through colorectal cancer throughout the country, every hospital system will do it a little bit differently. Siteman Cancer Center followed a 5-day approach of 5 days of radiation.

Before you even go through radiation, you have about a 2-hour appointment where they make a mold of your body so that the radiation can go into a localized area. The beam is positioned to go into the side if you’re getting radiation into your colorectal area.
Essentially, be prepared for about a 2-hour appointment with some technicians to create that mold. I think that’s pretty similar to a lot of cancers.
I was petrified for radiation. It doesn’t hurt when it’s happening. Some individuals burn from their radiation. I did not because I had a very short 5-day protocol. I was probably on the beam for less than 5 minutes every day. I went every day at 8 a.m. for 5 days.
What happens during the radiation procedure?
I know Siteman Cancer Center has 3 proton beams they use for radiation. I had to go to the basement. You check in. Usually there’s a bit of a wait involved, 10 to 15 minutes. They call you back. You can only go by yourself. I couldn’t have my husband come with me.
They have 3 technicians there. They are very diligent about what they do. They will have you lie down on what looks like a CT scan board. They will position you.
Most of the time you’re in radiation, they are lining up the proton beam to where it needs to go in order to be most effective (i.e. hit the tumor). I would say that’s what takes the most time.
My best advice, especially on your first day, is it goes back to that deep breathing, because you have to be extremely still.
Super still while they’re doing radiation. The actual radiation going into your body is a couple minutes. All in all, it’s a pretty short experience, and you will not normally experience any side effects for days, weeks, or even a month after.

What helped you get through radiation?
Another thing that really helped me is when I got there, I was really distraught that day. I couldn’t believe this is where I was at in my life. Something I feel really lucky for is I know the cancer center does an amazing job at hiring amazing people in the front desk, their technicians.
They asked, “How can we ease your worries right now?” I asked for music. “Can you play music while I go through radiation?” And they did. It was another nice little touch that I felt like I was their only patient that day.
Don’t be afraid to ask for things, because a lot of these individuals go into this work because they want to help people, especially people in compromised situations such as cancer patients.
»MORE: Read other patient experiences with radiation therapy
Radiation side effects
For a colorectal cancer patient, I’d expect you to experience issues with your bladder and otherwise GI system. I experienced pretty significant GI symptoms, as well as bladder issues. The radiation hit my bladder and obviously the whole GI area.
That was pretty tough, I’ll be honest. I’m a very, very social human. Radiation side effects hit about a week after my last appointment. For about 2.5 weeks, I experienced side effects, which I was told was going to happen. We were prepared for that to happen.
Everybody’s different. I would have extreme stomach aches. Urgency or frequency — it would just come out of nowhere that you’d have to use the restroom. If I could put it into a number, I’d probably say 8 to 12 times is how much you’d have to use the restroom any given day.
Working from home
I was at home more. I worked from home when I could. I really advocated for myself. I made sure my employer understood that I’m going to have a difficult time the next few weeks, so I really need you to work with me.
He was more than willing to help me out in that situation, and I could work from home as much as I possibly needed to.

My life kind of slowed down, but that’s what I needed to do to get through that. Then one day, they just stopped, and you move onto the next thing, which is chemotherapy.
»MORE: Working during cancer treatment
Routine pelvic MRI scans
With the pelvic MRI, my oncologist wanted to determine if the tumor was shrinking, which luckily even after the first 4 rounds of chemo, it was shrinking. He stuck with the pelvic MRIs twice, 2 rounds of that, before he then went onto a CT scan.
The pelvic MRI was just similar to the one I initially had to determine how big it was in my pelvic area, in my rectum. That takes about 45 to 60 minutes in order to have that scan.
How long did it take to get scan results?
It’s relatively pretty fast. I usually get a call the next day. If a holiday falls in there, it messes things up. Normally, once you’re an established patient, they like to call you — at least my oncologist does — usually the next day.
»MORE: Dealing with scanxiety and waiting for results
Advice on scheduling scans
With my CT scans, I like to go in the morning because I don’t have any nausea associated with it. With the MRI, I like to do it in the evening because I have such extreme nausea with it that I like to go home and just have no plans for the day.
If you’re affected by that contrast dye, you’ll know right away. It’s pretty rare, I’ve been told, but it’s something I struggled with.

FOLFOX Chemotherapy and Side Effects
Getting a port before chemo
I had my port placed about 2 weeks before chemotherapy. They told me I could have my port placed a day before chemotherapy. I personally would not recommend that for most people.
Because I had such terrible problems with my food intake, I had lost so much weight. I was very thin when I started chemotherapy. Port placement was very difficult for me. I think for a lot of patients, it can be, and some people aren’t affected at all by it.
I was actually bedridden for about 3 days. I couldn’t lift my chest. I couldn’t lift my arm up. It actually hurt to walk. I would say have your port placed at least a week before chemo so your body can heal and accept that foreign object before you then go through chemotherapy.
What is FOLFOX chemotherapy like?
The chemo I was on is called FOLFOX. Very standard for colorectal cancer patients, as well as a couple other cancers. This chemotherapy, as is the case of most, is cumulative.
They didn’t tell me, ‘You’ll for sure do 12 rounds.’ They said, ‘We’ll hope for 12 rounds in order to completely shrink or have your tumor disappear, then kill off as many cancer cells as we possibly can.’
For me, the regimen is 6 months unless your body just can’t take it anymore. A common side effect is that your body more or less begins to shut down a little bit during the end — the 10th, 11th, or 12th round.
What are the chemo infusions like (outpatient)?
I would normally go to chemo for morning appointments. You would go in, go to the blood clinic area, have your blood drawn. Usually, you’ll have a port.
Chemotherapy lasted about 2 hours for pre-meds, including anti-nausea. They did a lot of different medications to kickstart your body before the chemo went in.
Then I would do a 2-hour infusion with my chemotherapy. They’ll do that to watch you to ensure you don’t have any adverse effects. Then after the 4.5 hours, they send you home with a chemo pump. You will have that with you for about 48 hours.
What’s it like using a chemo pump?
Your pump tells you everything. It’ll show you how many units left you have of chemo, and so you know exactly when it’s going to go off. By your third, fourth, fifth rounds, you know what’s going to happen. It’ll beep for you to tell you that it’s empty.
Something I did is I became comfortable changing my wardrobe a little bit. For me, in the first 6 to 7 rounds, I felt okay on chemo. I was definitely dehydrated, but I was able to go about and do things, run errands with it. I was able to live a pretty normal life with the pump. I definitely felt tired; I lacked energy. I did things on it.
What I would do is there’s a certain company that I bought a lot of clothes from that just made it very, very easy to access my port. I wore a lot of tank tops that were not high neck. That made me feel more like myself because I was able to wear clothes that I liked.
I know that sounds trivial, and maybe someone can’t relate to that, but I think if you can do as many things as you did before, you’re going to feel a little more normal, because our life isn’t normal when you’re going through cancer.
That made me feel good about myself, maintaining the way I looked.
Hiding the chemo pump
The biggest thing I did to make sure I maintained a “normal” life was that I bought this adorable little backpack, cute little designer bag, and I would put my chemo pump in the bag. I was able to walk around St. Louis, and no one knew I was on chemo. I was able to do a lot of things, even though I had that attached to me for 48 hours!

Tip on handling chemo: hydration and getting fluids
It’s so important. That’s something I really harp on is find ways in which you can drink water while you’re on chemo.
That was a struggle I had until the sixth round, when I realized how important it was. Then it was a game changer for me in terms of energy and recovery once I was unclipped (from chemo bag).
Something we were told from the get-go by a patient who’s now a survivor — she told me it was almost impossible for her to have enough fluids during chemotherapy. What she would do, and what I did as well, is when my chemo pump would go off, we would go into the cancer care clinic. Most hospitals have this; it’s essentially a clinic open on the weekends.
What we would do is go to the cancer care clinic. They would give me a bag of saline, so I’d have a whole bag of fluids. Then I’d have the nurse take the needle out of my port.
A couple reasons we did that. I just couldn’t get enough water during chemo. I was very nauseous. I didn’t feel like drinking water.
We just wanted my port to stay in the best shape it could to eliminate infections. A registered nurse or nurse practitioner accessed and de-accessed my port.
I would recommend that for people. Go the extra mile. Get the fluids. Then have a nurse take it out to confirm it’s not swollen or that there’s an infection. The cancer care clinic had all nurses in it, and I believe all of the individuals who accessed my port were nurses (RNs).

FOLFOX chemo side effects and what helped fight them
I lacked a lot of energy for the most part. I was nauseous a lot. Make sure you talk to your doctors about it if you’re experiencing nausea. There are ways around it.
After the 48 hours (of chemo), just tired. If I could shed any light on that, I think it’s just about taking yourself where you’re at. Not where you want to be, but where you’re at. That was really hard for me in the beginning, because I wanted to work out the next day once chemo was over. I started realizing that my body was fighting a battle. While it did that, I mentally had to allow myself to slow down.
Side effects were hard: nausea, fatigue, just slowness. I felt very slow with a lot of things I did. Towards the end of chemo, I finally accepted that. But it took me a little bit of time, which I’m sure most young adult cancer patients can relate to, especially if you’re really active and wanting to live your life.
I did not have dryness on my hands or feet. I did have a throat sore issue during round 6. I was just really thankful that I asked a lot of questions and was told that it was a very common side effect.
I made sure to have the magic mouthwash with me before it even happened. I had those resources available when I did start to experience those side effects.
I think my biggest side effect that I still experience today was neuropathy. Especially for colorectal cancer patients, that is the most common side effect. You almost can’t get away from it. You’re going to experience it at some point. That is something that I still experience, but it’s gotten better. It gets better.
During those 48 hours, the neuropathy was pretty bad. My neuropathy in my feet was like muscle spasms and muscle cramping. That had to do with the neuropathy and the dehydration. Dehydration causes the muscle cramps that a lot of cancer patients experience.
Hair thinning
I used to have extremely thick hair! So much that I used to actually thin my hair out every 6 weeks. I would make comments like, “I wish my hair was thinner. It’s so unbelievably thick.” Pre-cancer, I would say that.
With my chemo, I didn’t lose all my hair. It just thinned out, so I lost all my thickness.
I don’t think you realize how traumatic that is until you go through it. I’ve had some people tell me, “Well, at least you didn’t lose it all.” I think it’s a little insensitive because until you’ve gone through it and you’re washing your hair, your hair’s falling out in clumps, you don’t realize how much of that is your identity. As a female, I think it’s so difficult to lose it.
»MORE: Dealing with hair loss during cancer treatment
That was pretty hard for me. I’ll be honest, it’s still hard for me. I’ve had to cut my hair because it was so thin at the ends. That hasn’t gone away.
I’m still trying to accept the human I see when I look in the mirror because she’s different than she was a little over a year ago. I do think that’s part of cancer — accepting yourself where you’re at, not where you want to be.
Losing your hair — I hope everyone watching this gives themself some grace. It’s traumatic. You’re not being dramatic; it is a traumatic situation.
Holistic approach
When I got diagnosed, one of my biggest pieces was not fully regaining control, but finding ways in which I could feel like I was taking every step that I could towards being cancer free. Something in particular was I definitely lived a more holistic, homeopathic life.
My doctor approved me to take 18 vitamins and antioxidants. Several of those vitamins and antioxidants definitely helped with my neuropathy. They’re known for that. I think I was able to recover from my fatigue so much faster because I was pumping my body full of antioxidants.
I personally believe that what we give our bodies can be beneficial or detrimental.
I definitely think during chemo treatment, it’s best to fuel your body with foods that it needs. Whenever someone calls me after they’ve been diagnosed and they asked what I did, how my body reacted so well to chemo, I do share that. I think it was my plant-based diet [and] also the vitamins and antioxidants that I take.
I’m a huge proponent of that. I know it worked. Being healthy during chemo and cancer treatment, I think it helps.

Post-Treatment Monitoring
Results after chemotherapy
My tumor had completely disappeared. There was no sign of it in my rectum, and my CEA levels had gone back down to a normal range.
Deciding against surgery
When I met my surgeon, he said to be prepared to have surgery. [Because of] where my tumor was and how large it was, he said, “You’re 100% a surgery candidate. You will have surgery.”
I was determined after my PET scan after chemotherapy that I was actually a candidate for a non-operative approach. What that entails is for the next 5 years, I’m very closely monitored with blood work, CT scans, PET scans, and scopes.
I actually have not had surgery, and I’m part of a very small group of people that fall into that category. I feel really lucky that chemo worked so well in my situation.
It’s definitely a riskier path. I fully, fully recognize that, but I don’t think there’s an easy path with this. I could have had surgery to remove my rectum, and the likelihood of cancer coming back is very slim.
Right now I’m in my first year, about 6 months out from chemo. The likelihood of it coming back is about 40%, which is why I’m so closely monitored. Colonoscopies, scopes, scans, and blood work will hopefully find the cancer if it does come back and find it fast!

Weighing your options
Where my tumor was, the affected area, they would have to remove the entire rectum, and I would be 100% ostomy bag. That would be it for sure. My husband and I decided that everything looks good right now.
We know it’s a riskier path to take, but I know I will be a compliant patient. I will never miss an appointment, a blood work. I committed to this, going to my doctor quite often.
Let’s take this path, and if it comes back, then I will have the surgery. For me, it was tough. I didn’t know what to do.
I thought a lot about it. Because I am so compliant, because I want to be an advocate in my own health care, my oncologist thought it was a good path for me to take, and we would reconvene every 4 to 6 weeks and determine from there. Once again, taking it day by day.
Describe your monitoring protocol
(For 5 years.) At that point, I’m considered cancer-free. Then it starts with 6-month colonoscopies and then yearly colonoscopies, so it’s for quite a while.
But the extra work, for me, is worth it. I’d be remiss if I told you that I’m not scared to have an ostomy. I am. I think it definitely changes your life. Not forever, but it’s a life-altering surgery.
When something like that is about to happen to you, you need to think about all the avenues before you go down and have such an invasive surgery. You go down that path. I think we have done our due diligence, and we feel comfortable with our decision.
You have to also get endoscopies. What are those?
They call it a light colonoscopy, so you’re not put under. It’s actually just an outpatient procedure, but the procedure sounds scary. It’s not.
I had it a week or 2 ago. I was in the doctor’s office for maybe 15 minutes, so essentially it’s a scope that they insert into your rectum. It ensures the tumor has not regrown so that there’s no tumor growth. In my case, re-growth.
I’ll be honest, I get nervous every time I go to the surgeon. Like I said, it’s a short procedure. You’re in; you’re out.
Quality of Life
How do you deal with the uncertainty?
It’s like a seesaw in a way. I feel really strong some days. Some days I don’t. I think it’s being okay with that.
I’ll be honest, from January after I was told I was a non-operative patient until my 1-year in May, I was so strong about it. I thought to myself, [and] I told people out loud, “If it comes back, it comes back. We’ll deal with it.”
Then May hit, and my 1-year was pretty traumatic. I had this rush of fear for 2 or 3 weeks, and now I don’t.
I don’t think you just wake up, and you’re okay with it. It’s really scary, but I think you allow yourself to feel it, but not allow it to consume everything you do. I think that’s the difference.
I meet some people who it’s almost like they’re so negative — “It’s not if it’s going to come back, it’s when.” I don’t live my life like that. I pray it doesn’t, but I know that it could. Then again, it could not. It might never come back.

Just allowing yourself to give yourself some grace that it’s going to be a bit of a roller coaster the first couple years, but to be okay with that. I’m allowing myself that, because it is traumatic to go through cancer.
But I think there’s a point to where it’s super healthy, and then it’s a healthy level of concern. I like to watch myself on that. Am I obsessing over it? Or am I just a concerned human who’s worried about their cancer coming back? I like to keep myself in check.

Survivorship
I tell my husband this a lot. I tell people this a lot. I feel like my battle started after I rang the bell.
I’ll touch on that. I felt like I had so much support. I teach at this cycle bar here, and they started a group called Jo’s Army. They had headbands and special cycle bar rides for me.
I had so much support that it was almost overwhelming. It really helped me [and] kept me alive during chemo. Then I rang the bell, and it’s almost like most people forgot that cancer is still really, really relevant in my life.
For me, where I struggled in January, February, and March was I didn’t give myself any grace. I was really hard on myself because I wanted my life to go back to where it was. That just isn’t life. It’s going to take time.
Menopause and fertility
Something I want a lot of women to be aware of is you’re probably going to go through temporary or permanent menopause. There’s no way around it sometimes. It sucks. It’s terrible.
I’m currently going through temporary menopause. I wish I would have asked more questions about that. I felt like after chemo, they kind of let me out into the world. My life was supposed to pick up where it left off, and it just doesn’t work like that. Some essential things I’ve done is joined a group of gals on Instagram. We talk about what life after cancer is. We are all colorectal cancer survivors.
Tending to mental health
I have a grief and loss counselor I talk to on a weekly basis, because I think I am still grieving what was my life pre-cancer. It pops up in really small ways. I think where I’m at 6 months later is that I’m just trying to accept myself for who I am.
I don’t think I need to be “Joanna, cancer patient,” but right now it’s a huge piece of who I am, so I think accepting myself for all the things that carry with it post-cancer.
I hope people recognize it’s not just a year journey. It’s going to be a lifelong journey. Your life just looks a little bit different than everybody else’s without cancer. That’s okay. That comparison factor has to go away.
I think those are the things post-cancer I’d love to relay to people. The hardship of it doesn’t stop. That’s something I didn’t really realize was going to happen.

Inspired by Joanna's story?
Share your story, too!
Rectal Cancer Stories
Sarah G., Rectal Cancer, Stage 2A
Symptom: Minor and inconsistent rectal bleeding
Treatments: Surgery (low anterior resection or LAR), chemotherapy (FOLFOX)
Kalei M., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Presence of mucus and tissue-like substance and blood in stool, stomach cramping
Treatment: Radiation therapy, chemotherapy, surgeries (two lung resections)
Jessica A., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Changes in bowel movements, blood in stool, abdominal pain, back pain, difficulty sitting comfortably, constipation, feeling of incomplete evacuation (as if some stool remained after bowel movements), mucus-like stool consistency, bloating
Treatment: Immunotherapy under a clinical trial
Shiva S., Rectal Cancer, T2, and Renal Cancer, T3
Symptoms: Pressure and urgency of bowels, back pain
Treatments: Chemoradiation (for rectal cancer), surgery (ileostomy, combined bowel and kidney surgery), immunotherapy (for kidney cancer)
Jeanine B., Rectal Cancer, Stage 3 (T3bN0M0)
Symptoms: Long history of bleeding that was blamed on hemorrhoids, pain in the tailbone, urgent need to use the restroom, unusually narrow stools, presence of mucus in stools, fatigue
Treatments: Chemotherapy, radiation therapy
Devon B., Rectal Cancer, Stage 4
Symptoms: Pain when trying to move bowels, increased frequency of bowel movements alternating with periods of constipation, passing mucus instead of feces, narrow stools
Treatments: Surgery (ostomy surgery), radiation therapy, chemotherapy







One reply on “Joanna’s Stage 3 Rectal Cancer Story”
Your story was very inspiring to me Joanna. Diagnosed with stage 2 rectal last month. Cancer center setting me up for chemo & radiation stated it is treatable, surgeon from Indianapolis called me this evening and stated 50% remission rate which was terrible news. Your story was inspiring to me, I am going to ignore the Indy surgeon call and go with your story. Matt