Stephanie’s Stage 3 Colon Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

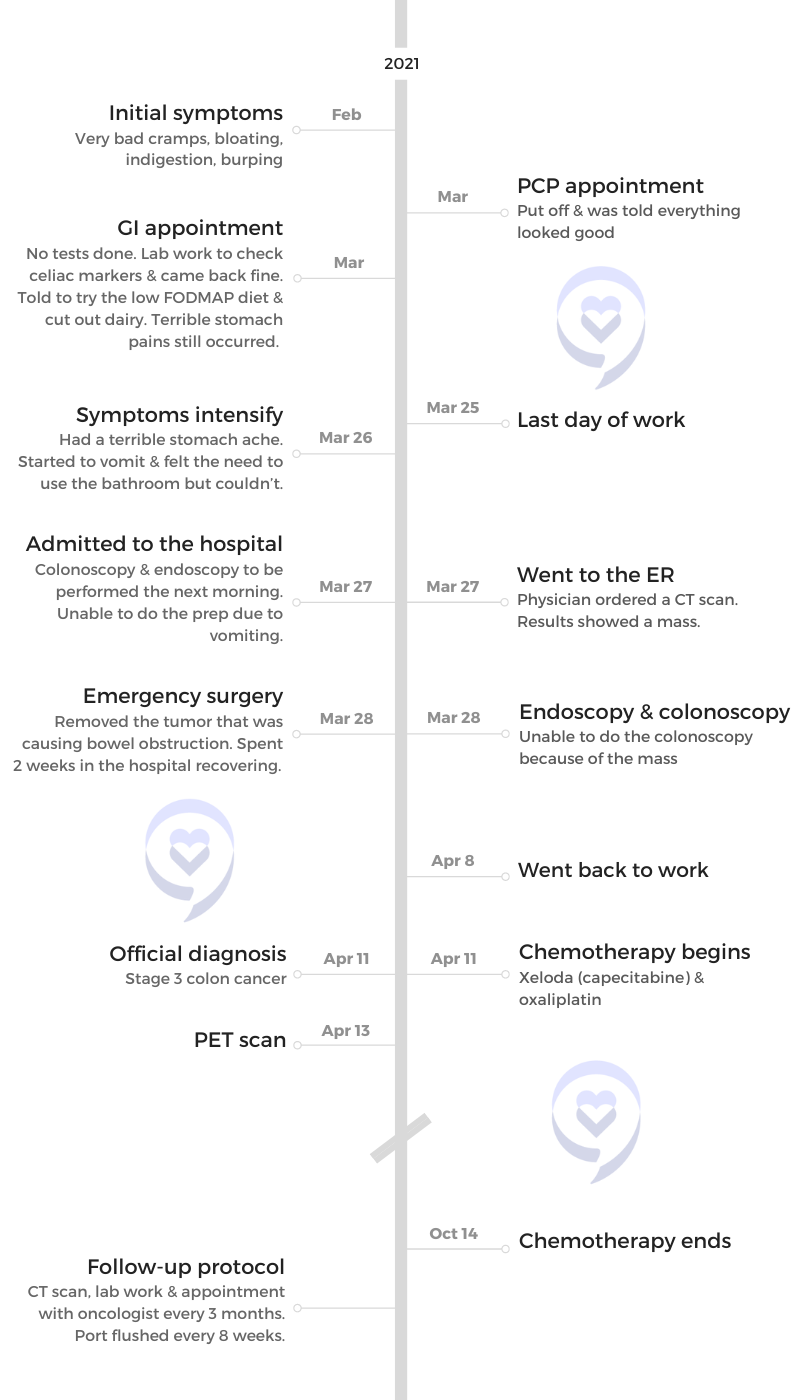
Stephanie was diagnosed with stage 3 colon cancer when she was 32. A mom to a 15-year-old son, she shares her journey from pre-diagnosis to recovery.
Before the diagnosis, she experienced stomachaches, bloating, fatigue, and low energy. Despite seeking medical help, doctors brushed off her symptoms. Various attempts to address the issues, including dietary changes and birth control, proved unsuccessful.
Her symptoms worsened and eventually led to an emergency room visit. A CT scan revealed a mass, leading to a hospital admission. Unable to perform a colonoscopy due to the obstruction caused by the tumor, the surgical oncologist recommended immediate surgery. Steph feared the worst, but the surgery went well, and she avoided having a colostomy bag.
The official diagnosis of stage 3 colon cancer came after a PET scan, revealing no spread beyond the colon. She underwent chemotherapy, surprisingly experiencing minimal side effects. She underwent regular monitoring, including periodic lab tests and CT scans. Despite insurance hurdles, a PET scan confirmed her cancer was in remission.
Engaging in activities and maintaining connections with friends was crucial for her mental health throughout the journey. Dealing with anxiety post-treatment, she emphasized the importance of self-advocacy, trusting one’s intuition, and having a positive mindset.
In addition to Stephanie’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Stephanie K.
- Diagnosis:
- Colon cancer
- Staging:
- 3
- Initial Symptoms:
- Very bad cramps
- Bloating
- Indigestion
- Burping
- Treatment:
- Surgery
- Chemotherapy: CAPOX (capecitabine and oxaliplatin)

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I felt that something was wrong. There was no blood so I never thought of colon cancer.
Introduction
I’m 33 years old. I’m a nanny and I work occasionally as a server in restaurants.
I have a 15-year-old son. He’s a sophomore in high school.
Before I was diagnosed, I went to the gym. I like to lift. I had a bunch of gym friends and we lifted a lot of weights.





Pre-diagnosis
Initial Symptoms
I was getting stomachaches and felt very bloated. I was tired and didn’t have much energy. I felt that something was wrong.
There was no blood so I never thought of colon cancer. I had bowel movements but felt bloated and had terrible pains that would come and go pretty much every day.
I went to the doctor and said, “I’m getting these terrible stomach pains. I feel like something’s not right.” They said, “You’re active, you’re healthy, and your labs look good,” but I always had low iron so they said, “Maybe change something with your diet and see if that takes away the cramps and the bloating.”
I was driving myself crazy. I would eat a lot of broccoli and look up online, “Does broccoli cause bloating and stomach pains?” I started thinking, Am I crazy? Because I would go to the doctor and he’d say everything’s good.
One weekend, I was out to lunch and couldn’t even stomach a bite because that’s how bad my stomach was hurting.
Gynecology Appointment
I went to the gynecologist. I wasn’t on birth control, but she said, “Maybe due to your heavy menstrual cycles, the birth control will help lessen the cramps and all the things that come with your menstrual cycle, like tiredness and headaches.” She said it could make the flow lighter. We went the whole route of doing birth control to see if that would help, but nothing seemed to help.
One weekend, I was out to lunch and couldn’t even stomach a bite because that’s how bad my stomach was hurting. I couldn’t eat. I knew something was wrong. I said, “I need to go home and lie down.”
I had that feeling like I was going to throw up. I called my mom and she said, “Maybe you caught a stomach bug. Take some Pepto-Bismol,” so I did that.
The next morning, the pain was still there. It was pretty bad and I knew. I called my mom and said, “I should go to the ER.”





Emergency Room Visit
She dropped me off at the ER. When they were checking me in, I said, “I’m getting terrible stomach pains. I’m sick.” COVID is going on so they said, “Maybe you have COVID. We’ll do a COVID test.” Negative for COVID.
The physician said, “I’m going to order a CT scan to see what’s going on in your abdomen.” We got the CT scan and he came back and said, “We found a mass in your stomach area so we’re going to have to admit you.”
I’m 32. I was thinking of the worst-case scenario. I’m scared. I called my mom and said, “They found something in the CAT scan. They’re going to admit me to the hospital. You have to come down.”
My mom came down. When they took me into a room, the nurse said, “We’re going to have a gastro doctor come down and check you out.” He came down and said, “We can’t tell you what it is until we go inside and do a colonoscopy.”
I called my mom and said, ‘They found something in the CAT scan. They’re going to admit me to the hospital. You have to come down.’
Preparing for a Colonoscopy
They tried to prep me for the colonoscopy. All night, I couldn’t drink. It was coming back up. I was very nauseous. They tried every nausea medicine, but nothing was working. The nurse said, “I’m going to call the physician on call and see what he suggests.”
He must have gotten in touch with the gastro doctor and they took me as the next case first thing in the morning. I had an endoscopy and was supposed to have a colonoscopy. All I remember is being wheeled down.

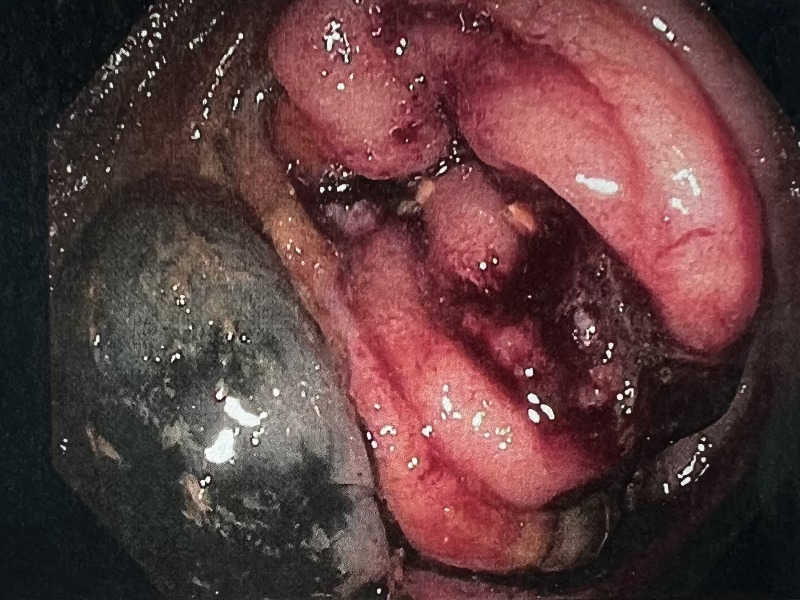
Finding a Mass
When I woke up, there were a ton of doctors around. They couldn’t do the colonoscopy because the tumor was causing an obstruction. They couldn’t get through.
They said, “We found a mass. It’s probably cancer. We’re going to have to get a surgical oncologist in to see you.” They took me back up to my room and when the surgical oncologist came in, he said to my mom, “If this was my daughter, I would do surgery now.”



Surgery
They wheeled me down to the OR. He explained, “You could have a colostomy bag when you wake up. We don’t know until we get in there.” I’m scared. I’ve never had major surgery. I was thinking, Cancer. Chemo. I’m going to lose my hair.
I don’t remember anything, but when I woke up, the first thing I looked for in recovery was if I had a colostomy bag. Thankfully, I didn’t. The surgery went well.
I had an idea of what a colostomy bag was, but no other information like what it would make me feel like or what I would have to do if I woke up and I had one.
I had no time to process anything because everything happened so fast. It put things in perspective. I knew that something wasn’t right in those two years when my stomach was hurting, but the doctors kept on saying, “Oh, you’re young,” and then it turned into a horror story.

I don’t remember anything, but when I woke up, the first thing I looked for in recovery was if I had a colostomy bag.
Recovering from Surgery
When I woke up in the recovery room, the doctor wasn’t there but my parents were. They took me up to the oncology floor until I could heal. The doctors came in, but they couldn’t tell me until the results came back from pathology.
My mind is in a million places. I have cancer. Did it spread? Am I going to live? Everything comes crashing.




Diagnosis
Getting the Official Diagnosis
Once I was discharged from the hospital, I had a follow-up appointment with the surgical oncologist.
Both my parents came to that appointment. He said stage 3 or 4 because the CT scan picked up a spot on my liver and lung and he wouldn’t know exactly until I had the PET scan.
The PET scan results showed that it was just in my colon. It did not spread.
After the surgical oncologist, I went to see the general oncologist and he went over my treatment plan, the pathology results, and all that.
Breaking the News to the Family
I honestly didn’t know what to say because I was probably as scared as my son was and I didn’t want to show that to him. My parents, my two older sisters, and my brother reassured him that things would be okay. I’m sick, but I’m on the path to get better.
Treatment
Discussing the Treatment Plan
Both my parents came with me. I remember being so nervous and scared to death. I was thinking, I’m going to have to get a port and get chemo. I’m going to lose my hair. I didn’t know the side effects or how it was going to feel.
I remember him telling my parents the cancer had gone into some of the lymph nodes. They cut them out during surgery, but I will have to do chemo to make sure. I would do a chemo regimen of oxaliplatin and Xeloda (capecitabine).
I got a port placed in my chest. Once every two weeks, I would go in for a chemo infusion. Every day for two weeks, I would take two chemo pills — one in the morning and one in the evening.

It was very hard for me to relax because I wanted to keep on living life as normal as possible. That’s what helped me the most.

Side Effects of Chemotherapy
My side effects were very minimal. My oncologist was very surprised.
I had a little bit of hair thinning. I had neuropathy in my fingers and feet. I had a ton of cold sensitivity. After I would get the chemo infusion, for about a week, I couldn’t have cold water. Everything had to be at room temperature.
I was very tired. I would get nauseous. I took a lot of nausea pills from the oncologist.
Managing the Side Effects
I’m very outgoing. I love to socialize so it was very hard for me to relax because I wanted to keep on living life as normal as possible. That’s what helped me the most.
This is sad to say, but I was the youngest patient getting chemo. Everyone else was probably 50 and older. I’m coming in, this young girl, and I still have my hair while a lot of these patients are sick.
I tried to be very positive. I would bring in little note cards and hand them out to patients. I brought in a lot of word searches and positivity coloring books because they helped take my mind off of everything else that going on. There are also these little crafts that I would buy. They’re little sticky coloring pages and you put the gem to the number and they make very beautiful pictures.
I also bring music. Anything to distract you and keep you occupied.





Follow-up Monitoring
When I was going through chemo, I usually went in the morning. Every morning, they would draw my blood, check my cancer markers and all that, and make sure I was on the road to recovery.
If I had low iron or if they saw a red flag within my labs, they would check with the oncologist. I had iron transfusions a few times. If I needed potassium or sodium, they would give that to me. I didn’t have any scans until after my chemotherapy ended.
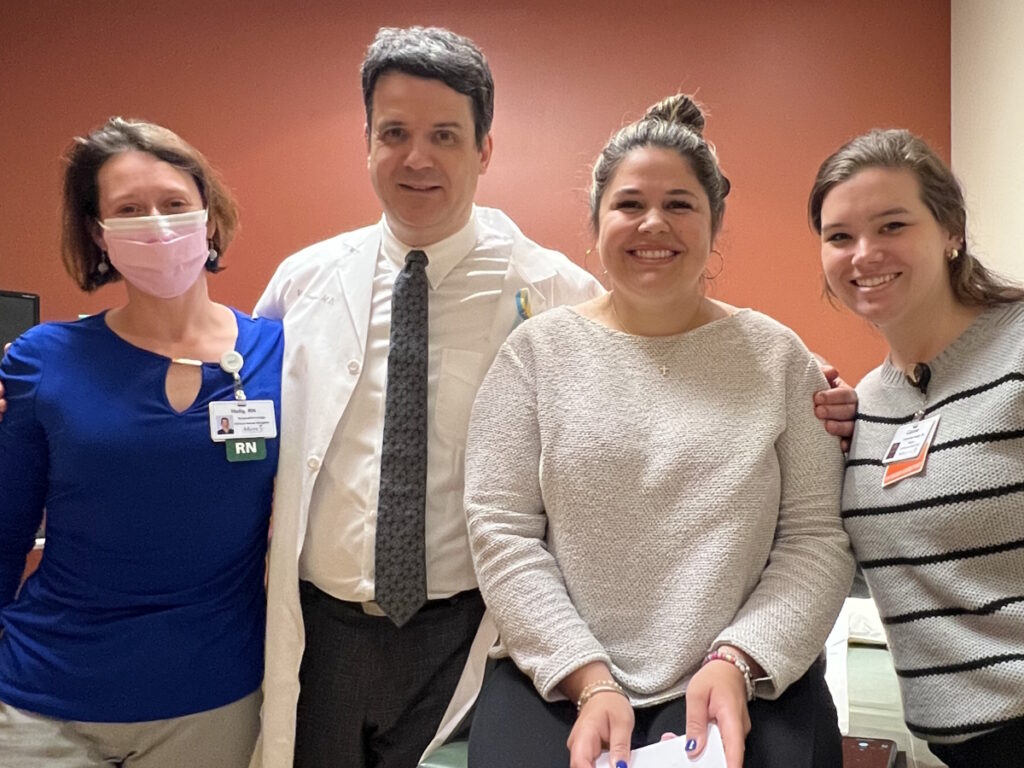
After my treatment, my insurance kept denying a PET scan. I couldn’t have a PET scan so I had a CT scan. I didn’t know any of the results until I saw the doctor. I followed up with the doctor and he said, “Things look great. Your cancer is in remission.”
But I wanted to get a PET scan because it scans your whole body and it would help me sleep better so I pushed for that. He said, “I don’t think you need it. Labs look good. The CAT scan looked good.”
After my treatment, my insurance kept denying a PET scan… But I wanted to get a PET scan because it scans your whole body and it would help me sleep better so I pushed for that.
I said, “I really want to get a PET scan,” to ease my mind. The nurse navigator was able to contact insurance and get authorization so I was able to get a PET scan.
I still have the spot on my liver and lung, but it did not grow in size so they’re not very concerned, but they’ll continue to monitor. Every three months, I go in for a CT scan and lab work. Every eight weeks, I get my port flushed.
My last scan was in October 2023. The scans came back clear and the doctor says my cancer is in remission.

Dealing with Scanxiety
Since my diagnosis, my anxiety is pretty bad. Every little ache and pain, I think, Oh, is something wrong? The oncologist told me that’s normal.
I try not to think too much about it, but if I have a test coming up, I do take anxiety medicine prescribed by the oncologist to help put me at ease so I’m not too stressed out.
The oncologist reassured me. At my last oncology appointment, he said, “Your cancer is in remission.” I thought, Then what? What if I feel a pain? But he said, “You’re going to get stomach aches. You’re going to get the stomach flu. Try to not think worst-case scenario every time you feel something.”



Words of Advice
Trust your intuition. When you feel as though something isn’t right and you need further help, you need to advocate for yourself. “I’m not going to leave this doctor’s office until you do a test.” I would hate for someone to end up in my shoes, but I didn’t know then.
I was going to the doctor and at one point, I felt like I was crazy. My friends and I would have plans to go out to dinner and I would cancel because my stomach was hurting. I didn’t want to be the girl who has terrible stomach aches all the time. I thought it was social anxiety. It was driving me insane.
What I’ve learned through my experience is to advocate for yourself when your intuition is telling you something’s not right. Fight to get your voice heard.
I knew something was not right. Unfortunately, I’m young. I was 32 at the time of my diagnosis. How often do you hear of a 32-year-old female getting diagnosed with stage 3 colon cancer?

Advocate for yourself when your intuition is telling you something’s not right. Fight to get your voice heard.

Colonoscopies aren’t necessary until you’re a certain age and that I think should be changed because I’m proof. Stomach pains for two years and the doctors said I was fine because I was young, but I knew within me that something was not right.
You have to be positive. Cancer is a scary diagnosis and your world can come crashing down. Think positively and try to keep pushing forward. You’re going to have bad days, but take those bad days and turn them into good days.
Go for a walk. Get outside. Try to stay involved in activities. Hang out with friends. My friends called to check in and sent text messages, asking if I needed anything.
Do things to keep your mind off of what’s happening, even though it’s so hard to do. That was my saving grace.



Inspired by Stephanie's story?
Share your story, too!
More Colon Cancer Stories
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy
Heather C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Severe bloating, indigestion, vomiting, rectal bleeding
Treatments: Chemotherapy, surgery (liver transplant, upcoming)
Nicole S., Colon Cancer, Stage 3
Symptoms: Dull lower abdominal pain that sharpened and was focused on the lower left side, appearance of dark blood in stool, difficulty retaining food due to near-complete blockage of sigmoid colon
Treatments: Surgery (colectomy), chemotherapy






One reply on “Stephanie’s Stage 3 Colon Cancer Story”
Abdominal Cancer Day is an annual observance dedicated to raising awareness about cancers affecting the abdominal region. This global initiative aims to educate the public about risk factors, symptoms, and prevention strategies while advocating for early detection and improved treatment options for abdominal cancers, including those affecting the stomach, liver, pancreas, and colorectal area.