Mila’s Stage 1B1 Squamous Cell Cervical Cancer Story

Mila shares her stage 1B1 squamous cell cervical cancer story, detailing how she underwent a radical trachelectomy (surgery), chemotherapy, radiation, and adjuvant chemo.
In her story, Mila also highlights navigating life after her cervical cancer diagnosis, including managing through hair loss with cold caps, how she approached fertility preservation, and the importance of patient self-advocacy.
- Name: Mila L.
- Diagnosis:
- Cervical cancer
- Stage 1B1
- Age at Diagnosis: 29
- 1st Symptoms:
- Abnormal lump in cervix area
- Bleeding after sex
- Tests for Diagnosis:
- Routine pap smear came back with irregular results with squamous cell carcinoma
- Treatment:
- Surgery: radical trachelectomy
- Chemotherapy: cisplatin
- Radiation
- Adjuvant chemotherapy:
- Carboplatin + paclitaxel (Taxol)
- Fertility Preservation:
- Underwent IVF during 6-week treatment break
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
You can get through it. It’s going to be hard. You’re going to need support, but there will be a day when you look back on that time and it will be far in your rearview mirror.
You’ll go on with your life, and it will strengthen the person that you are.
Mila L.
Diagnosis
How did you get diagnosed?
About 2 months before I was diagnosed, I started feeling this little lump. It turned out to be inside my cervix. I didn’t really know what it was. It wasn’t really painful or anything; it was just kind of there.
About a month before my diagnosis, I started bleeding after sex every time, which I later found out is a big indication of cancer.
The way I was diagnosed was just from a routine pap smear. It came back with irregular results with squamous cell carcinoma. I already knew I had had human papillomavirus (HPV), so I wasn’t really worried about it, but then they told me to go get a colposcopy, where I would then get a biopsy.
The biopsy is how they found that it was cancer.

What were you feeling when you were diagnosed?
The first feeling was shock. I was sitting there, and the doctor was my obstetrician (OB) who had told me. She was sitting next to me talking, showing me what it potentially looked like, and describing next steps. I was sitting there, staring at the ground.
I couldn’t really look at her. I couldn’t look my boyfriend in the face because I knew if I looked up, I would just start bawling. For me, I was really focused on the ground so I wouldn’t start crying.
Once we got in the car, I remember I still didn’t cry because I didn’t want to believe it. I didn’t want to believe I had cancer.
I didn’t want to say the word ‘cancer.’ I probably couldn’t say the word ‘cancer’ for probably a good 2 to 3 weeks after. I honestly couldn’t bring myself to say the word, let alone acknowledge that it was something that I had.
The first time I cried was that night when I was going to bed. I actually didn’t cry too much during that whole process.
Luckily for me, it wasn’t terminal cancer, and they caught it early enough. I think I knew that I wasn’t in real danger of dying. It was just going to be something that was going to upend my life for a while, and probably some lasting effects from it.
I had a really great support system in my boyfriend at the time, who used to be in the Army, so I think he’s used to dealing with these kinds of things and being strong.
He didn’t show any of that concern and was very steel-faced about it, which helped me be strong. I didn’t feel like I needed to be strong for him, so that was a huge help for me. My default is to kind of go inwards and shut down to that outside.
»MORE: Patients share how they processed a cancer diagnosis
Why was the diagnosis delayed?
It actually ended up being a longer timeline because I put it off. The pap smear I got was in June. Then the results came back fairly quickly from that, and they told me to get a colposcopy. I actually ended up putting that off for a couple months because I had a trip planned to the Bahamas.
I had just started a new job. It was something I wasn’t really prioritizing. Because I already knew I had HPV when I was 19, I just thought it was something related but not a big deal.
When I went to go get my colposcopy, it was probably in the beginning of August. I had a follow-up appointment set up with my doctor to come in about a week later to get my results later and talk. She actually ended up calling me a couple of days after that initial appointment and asking me to come in, which raised a little bit of a red flag but not too much.
I thought maybe I had an infection or something. Then when I came in, I actually brought my boyfriend at the time with me to the appointment because she had asked me to bring someone with me, which also for some reason at the time didn’t set off that big of a red flag but should have. That’s when she told me. From the colposcopy to the diagnosis, it was really only a couple of days.
What is a colposcopy?
It was a really quick biopsy. I actually didn’t even know she was going to do a biopsy, which was probably good that she didn’t tell me. I didn’t realize or really know what a colposcopy was.
I just went to get it because that was what I was told that I needed to get. She told me kind of as she was doing it that she was doing it. It was fairly painful. I think it was just a snip or with tweezers or something that she took a piece of tumor itself.
What was the cancer stage?
It was stage 1B1 when I initially got staged and diagnosed. The interesting thing about cervical cancer is that once I got my surgery and they took a biopsy of some lymph nodes, they found it had metastasized to my lymph nodes.
But the staging for cervical cancer for some reason doesn’t change, even if it’s already metastasized. My staging stayed at 1B1, where I think with other cancers it would have changed.

Describe the radical trachelectomy
Because of the staging that I had, I had something called a radical trachelectomy, which is where they take just the piece of the cervix. I think it was 2 inches or so.
Luckily, my doctor was trained in doing that type of surgery. He also did it laparoscopically [and] was trained on the Da Vinci (robotic surgery) machine. I was able to not have to have a hysterectomy.
What was the next step after surgery?
After I had the radical trachelectomy surgery, if my lymph nodes had come back clean, that would have been the end of it. I was actually sitting in my oncologist’s office when he got the results because they hadn’t come in yet, so he called the lab to find out the results.
I found out the same time as him that it had metastasized to 2 of the 6 or 8 lymph nodes that he had tested. Immediately in that office, [as] we were sitting there, he called a colleague of his who was a radiology oncologist to get me set up with an appointment with him. We laid out a plan for my chemo and radiation regimen.
Could a pap smear have caught it early?
The guidelines are essentially that you should only have to get a pap smear once every 3 years. According to my OB, she really doesn’t agree with that. I obviously don’t agree with that as well.
In my case, I had gone for a pap smear. I had irregular results from the time I was 19, so I was getting pap smears every single year. The results were coming back irregular. Then one year I had results that were regular, which I’ve now learned you can have even if you have a high-risk HPV strain.
Because my results were regular that previous year, when I went in to get it the next year, the doctor that I went into at the time told me that I didn’t need one and that I shouldn’t come back for another one for 3 years.
The next time that I came back to get a pap smear was that June of 2015 that I was diagnosed. My obstetrician that diagnosed me said it looked like it was a very slow-growing tumor that had developed probably over 3 years or so. It could have easily been prevented.
Treatment Plan
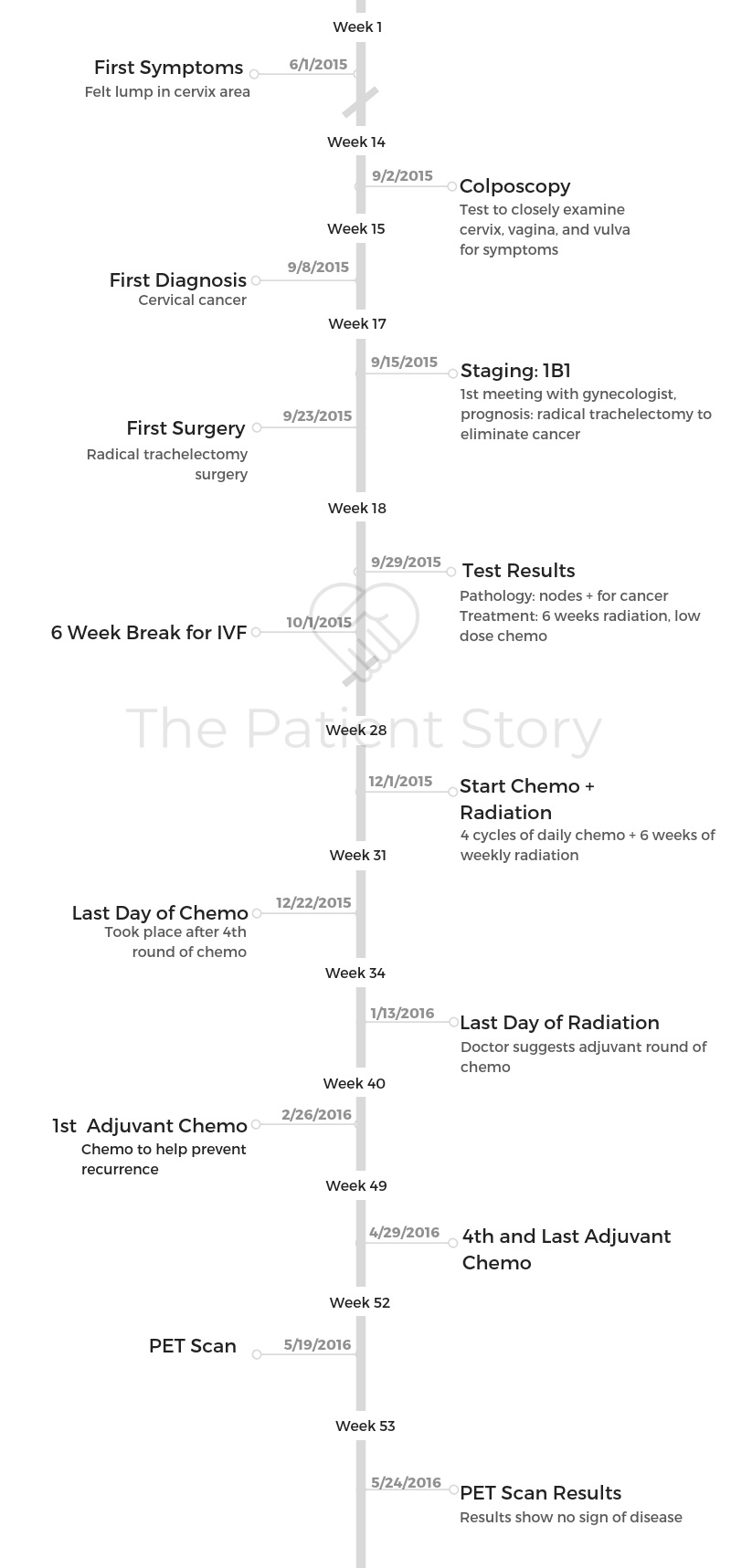
Timeline of diagnosis and treatment
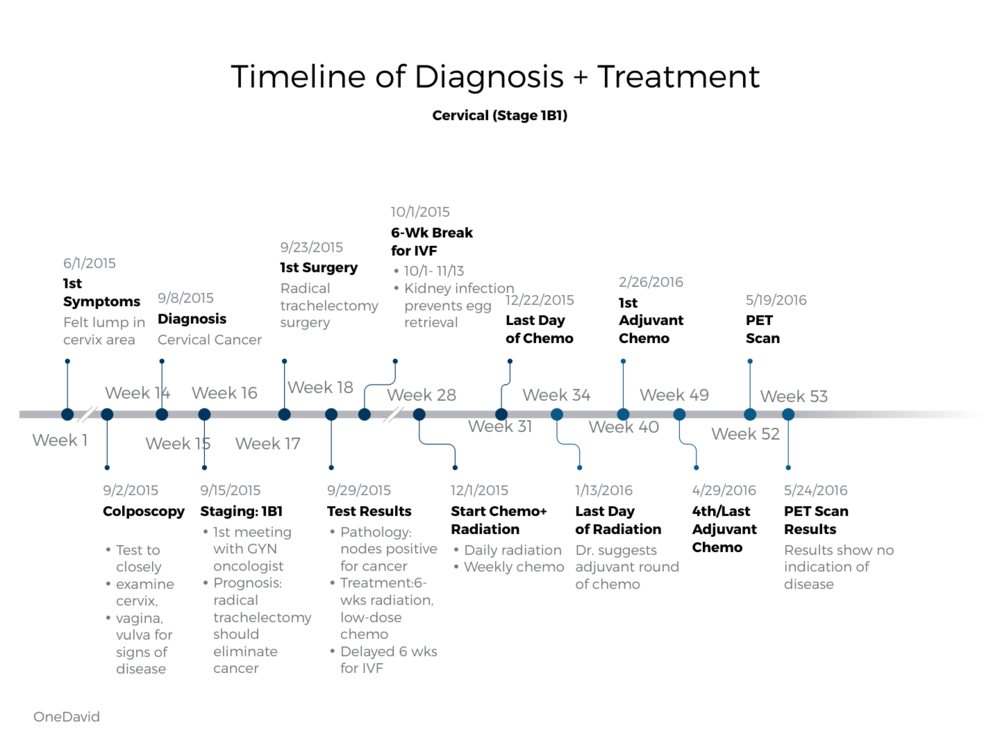
What was your treatment plan?
- Concurrent chemoradiation: chemo + radiation given at the same time
- Adjuvant chemotherapy: chemo given to prevent recurrence
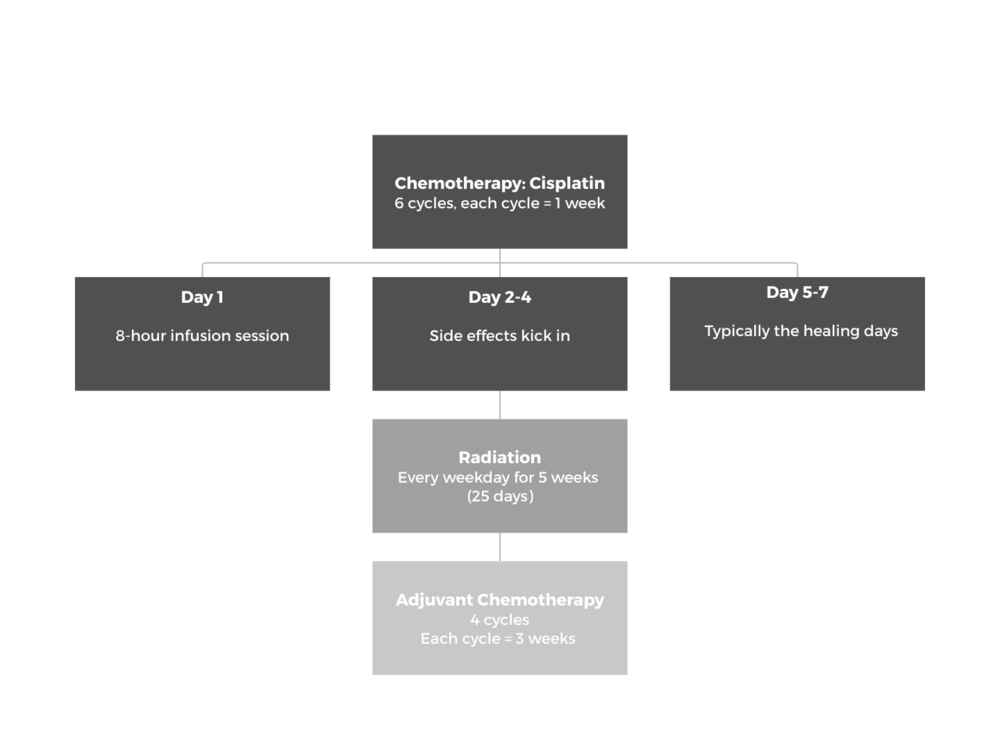
- Chemotherapy: cisplatin
- 6 cycles, each cycle = 1 week
- Cut down to 4 cycles because of neuropathy
- Day 1: one 8-hour infusion session
- Day 2-4: bad side effects
- Nausea
- Neuropathy
- Loss of taste
- Sensitive to smell
- Day 5-7: typically the healing days
- 6 cycles, each cycle = 1 week
- Radiation
- Every weekday for 25 days
- 5 weeks, no weekends
- Adjuvant chemotherapy: carboplatin + paclitaxel (Taxol)
- 4 cycles, each cycle = 3 weeks
- Used cold caps to save hair
- Chemotherapy: cisplatin
Radiation Therapy
Describe the radiation schedule
I would go in the mornings to radiation. Prior to that, I had to get fitted for it. They had to measure me. For the lasers to go into the same place every time, they actually gave me 3 little dot tattoos that are great souvenirs for me on my pelvis going forward. It’s funny. I joke I have 3 tattoos!
I got measured. Then I’d go in every morning [and] wait for my turn for the radiation. Then I would lay down on this machine that did the radiation. It was in a tube. I was in a tube, but for me it was just my pelvis. My head didn’t have to be there, but it was halfway on my body.
The process took about 10 minutes. It didn’t hurt. It was totally fine. You just kind of lay there in this loud machine. Then you go on your way when you’re done, so it’s not that intense itself, not that scary.
Did you feel the radiation?
The radiation itself, I didn’t necessarily feel it. My skin was a lot more prone to lesions. It was really sensitive. I didn’t feel the sunburn necessarily that you would feel with other types of radiation, but [my skin] was really kind of brittle.
If I would get a scratch or something, it wouldn’t go away. I would have to put lotion on it. Also for me, because it was pelvic radiation, I couldn’t really have sex. It was a pretty painful process.
Were there any side effects with radiation?
I was really sedentary essentially during that time and sitting a lot. In my pelvic area on my back, the skin was where I would get a lot of lesions, and it would get really itchy.
In the beginning, I would be scratching it, not realizing it was from the radiation. I would get these scabs that wouldn’t go away.
The combination of chemo and radiation was supposed to make you sick or constipated, and that was definitely an issue that I had. Combined with the nausea from chemo and everything, I found the best thing was actually just drinking prune juice versus all of the different medications they would give you.
»MORE: Read other patient experiences with radiation therapy

You had to go to physical therapy after radiation
I started seeing a pelvic physical therapist, which was recommended to me by my radiation oncologist. I’m very happy that I did. He talked to me about what could happen if I didn’t. If you don’t do certain exercises or stretch a muscle, radiation really shrinks things and makes things constrict. Same thing goes with your vagina.
With cervical cancer, with pelvic radiation, if you don’t stretch it out or dilate it regularly, there is a chance that your vagina could shrink down to really small. I think 2 inches, he said, maybe smaller, and there are certain exercises I have to do.
Because I had surgery and radiation, in that area I had a lot of scar tissue. The muscles were really constricted, and there was a ton of trauma done to that area. If you think about what happens [and] what you do when there’s trauma, you just tense up.
I had a wonderful physical therapist, and she did different exercises with me. She helped me stretch out and showed me how to do it on my own.
She used an electronic stimulation machine because I would get constant really sharp pains in my pelvic region all the time. She would do electronic stimulation, and then they’d go away for a while. That would really help ease the pain.
She was telling me how to do different stretches. Not only in your pelvic region, but let’s say your groin muscles for your legs. I’m less flexible now than I was before the radiation because those muscles are constricted and tougher. For me to be as flexible or to do those things, my muscles get sore quicker now than they did in the past.
Physical Therapy Recovery
How long did physical therapy last?
I did physical therapy for the first 2 or 3 months. It wasn’t just for that area. I have scars in different areas, and she showed me how to massage those scars so they didn’t get that rippling that you see bad scars get. They’re smooth and fade with time. We did some of that.
She showed me how to do those exercises. Once she showed me how to do all those things and I had improved, it didn’t make as much sense to go to her. I did it for the first couple of months, and then I could just do it on my own.
In this last appointment, I learned that apparently the dilation needs to happen ongoing in perpetuity for the rest of your life — unless you are having regular sex — to stretch your vagina out.
In the beginning, I’m pretty sure I was told it was only for the first year or so that you had to do it. Turns out it’s for your whole life that you need to maintain.
Can you describe the therapy and stimulation?
The electronic stimulation wasn’t a pleasurable stimulation kind of thing. It was different parts, including on my inner thigh and around my pelvis. The way she explained to me why I was having these really sharp pains is there are different types of nerves and nervous systems, and there’d be certain type of nerves that were firing.
That’s why I was having these really sharp pains. The electronic stimulation would confuse the nervous system. It would fire different ones, or it would engage different nerves that would help that one nerve system that was firing to not fire.
That’s why when we did the stimulation, it would last for a couple days. That would be helpful. I think that it’s for anybody that’s gone through radiation in your pelvis, because the radiation makes your vaginal canal constrict.
There are these dilators that vary in size. They look like these cone shapes, and they go into each other like little nesting dolls. There’s a little handle and a little cone shape. They vary in size. In the beginning, when you first finish radiation, you probably start with the smallest size. You use it to stretch the muscles, because it is a muscle.
You’d use maybe a smaller one to stretch in different directions to get the knots out of the muscles there and make them more pliable. Then you really just lay there with the larger one inside for a few minutes every day. Supposedly, that helps the canal not constrict.
I think ideally it’s supposed to happen every day. I will admit I am really bad about this, and I probably do it once a week. I think for myself, personally, I found that that’s just fine. I think that it would probably vary, depending on each person.
Chemotherapy and Side Effects
Describe the first chemotherapy cycle
The first chemo was pretty straightforward and simple. I would walk in. They would hook me up, give me steroids, and go through different IV bags.
Because they were giving me steroids on my chemo days, I actually felt fine other than the fact that I was sitting there with an IV for 8 hours that day. I’d come into the chemo center, sit in a chair, and just have this IV drip for 8 hours that day.
For that first round of chemo, I got a PICC line, which was honestly more annoying than anything else because you just have this plastic tube sticking out of your arm for a couple months while you’re getting chemo. That plastic tube has a catheter basically inside, so it doesn’t necessarily have to go through the veins in your arms.
You can’t really shower. It’s really uncomfortable to sleep. You have to go into get them cleaned. In the beginning, it’s fairly painful while it’s healing, and you have this hole in your arm with this tube sticking out of it. I didn’t love it.
What were the side effects from chemotherapy?
For those chemo sessions, I still was still working, so I would actually be on my laptop working on those days. I had a few client fires that I had to put out, which was really funny because I was on these phone calls and on my laptop answering these emails during these sessions. Otherwise, I felt totally fine.

In the days afterwards is when I would start feeling really bad, when the steroids would wear off. Not even the day after — because I would still have a little bit of steroids in the system — but after the chemo, the second, third, and fourth days were the worst.
The first chemo I underwent was called cisplatin. It was fairly neurotoxic. I was actually supposed to go through 6 sessions, but I ended up going through only 4 because I started to get ringing in my ears.
That was a neuropathy that my doctor was saying if that doesn’t go away, you could actually lose hearing. We lowered the number of chemo sessions, luckily.
Describe the side effect cycle
The day that I would feel the best in that time frame was the day right before chemo. It’s kind of a wave; you feel okay on the day of chemo, and then it kind of goes downhill from there.
Day 4 was the worst day. Then right when you’re feeling better day 5 and day 6, then comes around day 7, and you’re getting chemo again.
It would really hit days 2, 3, [and] 4. I would be really tired, really extremely nauseous, [and] very sensitive to smells. I actually couldn’t taste anything, so I lost my sense of taste. My sense of smell was really heightened. Even the smell of coffee or smell of cologne — I usually love the smell of cologne — would make me really, really sick.
I couldn’t eat anything, and I lost a lot of weight. The only thing that I really could eat were carrots and celery, maybe dry toast. My one saving grace — I still love these [and] even when I see them now, reminds me of this time in a happy way — [was] those blueberry breakfast crackers. Those, carrots, and celery were the only things I could eat. I ate a lot of those during that time.
»MORE: Cancer patients share their treatment side effects
Did you take medication to help the side effects?
I tried taking anti-nausea medication. There’s one called Ondansetron, and they gave me another one. Those honestly did not work for me at all.
To be honest, the absolute only thing that worked for me were weed edibles. Not even smoking or vaping; those would not work quite enough. As soon as I would eat an edible and it would kick in, I felt totally fine and was able to eat. The other effect of it is that I was really high.
I would usually take them in the evenings to help me go to sleep because I don’t love the high from edibles. Some people might. That weed was honestly the only thing that made me feel normal.
Describe the adjuvant chemotherapy
Carboplatin + paclitaxel (Taxol)
The second chemo was better in terms of the pain itself. I didn’t feel any sort of pain. They would give me these steroids I’d take before and after.
I’d actually go into the office during my non-chemo days and be functional, working. I was able to eat. I didn’t feel sick at all. It just felt like normal. Except for the days I had chemo, I felt totally normal.
The days that I did have chemo for me were a little bit harder because that was the round of chemo that I did cold caps. To do those, you’re basically giving yourself a little “brain freeze.”

Hair Loss
Describe the hair loss
For me, being able to keep my hair was extremely important because I didn’t want people knowing that I had cancer without me telling them. I wanted control of that information. When I was first diagnosed, I couldn’t even say the word ‘cancer,’ let alone tell people that I had cancer. So for me it was really important to be able to be the narrator of my story.
I still lost my eyebrows, and I still lost my eyelashes but being able to keep my hair… I think that having your hair is a signal of health. Whenever you see people that don’t have hair, you might think either they’re balding or they’re going through cancer.
I really just didn’t want to be a statistic for someone or a representation of something that they’re thinking.
I had instances, like when I went to a bar or somewhere, where I would actually tell people I had cancer. Their initial response was, “But you look healthy.”
Anybody who knows me or knew me during that time knows that you absolutely don’t say that to someone who’s going through something. I don’t know how others would feel about it, but for me it really enraged me because you’re basically invalidating what I’m telling you I’m feeling by saying that outwardly I’m not representing what that looks like to you.
So for me, hair was really important because I didn’t want to look like what somebody though sickness was.
I’m generally a pretty private person when I’m going through something. I’m happy to talk about it once I’m through it and help other people, but when I’m going through something, I don’t want to be a victim. I want to control that. That was a way for me to do that.
You used cold caps to save your hair
I found cold caps because I was searching online for ways to keep your hair through chemo, or how people have done it. It was the only thing that I found that helped you keep your hair. It really was.
Describe the cold caps
The second you put on this cold cap, which is a temperature of -32 Celsius because you keep it in dry ice, you just can’t function. I wasn’t really able to work during those sessions of chemo. You just lay there for 8 hours. It’s different depending on the type of chemo that you’re getting, but you have to wear them basically the entire day, even after your chemo’s over.

You have to change them every 30 minutes. The second you kind of get okay with what’s on your head, it’s time to renew that coldness, and you get another brain freeze.
How do you get cold caps?
It is fairly expensive. I think for the 3 months that I did it, I think it was something around maybe $5,000 completely out of pocket. You can’t even buy them in the U.S. because they’re not approved. You have to rent them from a distributor that owns them. Then you pay a monthly rental fee.
Once you’re done with them, you send them back. I don’t remember what the rental fee is. Something like $1,000, plus shipping fees, everything else, and paying for the dry ice. If you don’t have somebody who can help you, you can hire caregivers that sit with you during your chemo days and change out your cold caps every 30 minutes.
Once I brought up cold caps to [my doctor], he mentioned he had another patient, an older woman, that had gone through a similar process. Luckily, she was open to it. He connected me to her. She was a huge help to me because there were a lot of things you need to buy, like coolers. You need to buy gloves that won’t burn the person or you working with the dry ice. You need to buy a temperature gun and know how to put felt on your forehead and ears so they don’t burn.
It’s a process to figure out how to do it. You want to do it right because if you don’t, then you’re paying all this money and have all this effort, and you still lose your hair.




»MORE: Dealing with hair loss during cancer treatment
Cold caps don’t guarantee they’ll save your hair
Absolutely. My doctor was very open. My doctor didn’t even advocate for it. He was just matter-of-fact about it saying it doesn’t necessarily guarantee anything.
It could keep about 50% of your hair or so. Luckily for me, I would say it was about 70 to 75%. You can definitely tell around my forehead that my hairline receded a bit.
I had a couple of spots up on my head that were a little bit balding, but nothing that I couldn’t cover up with some black eye shadow and my hair.
I did lose my eyebrows, so I’d have to draw them in. I also lost my eyelashes, but I think that if I met someone on the street and they didn’t know, it was passable for them not to know.
Support
Who brought up the issue of fertility preservation?
I brought up the question of fertility. My doctor didn’t bring it up. I brought it up because it was something that I knew would affect my fertility. Luckily, my cancer wasn’t as aggressive, so I was able to put off starting my chemo and radiation regimen for the 4-week cycle of IVF to go through that process.
He also put me in touch with a colleague of his that was a really great IVF doctor as well, so my gynecological oncologist was really great and instrumental in rallying other doctors and referring me to the IVF and radiation oncologist.
I would say that the doctor’s goal is to kill the cancer. Their main concern is not your quality of life or necessarily what happens after they’ve done their job of killing the cancer and keeping you alive. That’s their goal. They’re people, too, so they are aware and they’ll sympathize, but it’s on you to be your own advocate.
»MORE: How to be a self-advocate as a patient
If having children is something that’s important to you, really research the options that you have and bring it up, because they’re not necessarily going to bring it up.
For example, with my radiation oncologist, he was very open and upfront with me about the fact that after radiation, I would likely not be able to carry my own child.
That was the aspect of fertility that he brought up, not anything about IVF or surrogacy. Being able to do your own kind of research in that, bringing it up with the doctors, and asking them to maybe postpone treatment if possible to go through an expedited round of IVF are really important.
»MORE: Read a patient’s detailed IVF journal
There are organizations out there that help cancer patients with the monetary aspect of it because it also isn’t covered by insurance, and it’s really expensive. Walgreens, for example, has the Heart Beat program. Livestrong has a really great program where they help cancer patients going through IVF. There are organizations out there that know and are advocates and help monetarily.
»MORE: Cancer organizations and nonprofits
Did you work through treatment?
I worked from home. Luckily, I had an amazing manager, and my work was so understanding about it. Don’t get me wrong, even when I worked, I wasn’t working to my full capacity. There was a lot of laying around in bed and watching a lot of TV because I couldn’t really concentrate as much or do anything else.
Then there was a fair amount of the chemo brain aspect of things, where you can’t concentrate. I couldn’t think of the words that I wanted to use. That was really, for me, very frustrating because I had always prided myself on having a large vocabulary.
I work with people and have clients, and so being able to express myself the way that I wanted to was always something that I was good at. That was kind of taken away from me in that time. Very frustrating.
»MORE: Working during cancer treatment
How was life after treatment?
I would say that life kind of went back to normal in that I was just working. I was fatigued. [It] lasted a while from what I can remember. [I was] going to regular doctor’s appointments, so still going into the hospital and going to see my doctor to get checked that everything looked fine.

How was dealing with insurance for treatment?
One thing that I found to be interesting and a little bit difficult was the fact that there wasn’t really anybody to help with the financial aspect of things.
For me, the thing that compounded it was my work. They were switching insurance providers at the time that I was going through this, so I unfortunately had to get through my deductible twice.
There isn’t really anyone I found to guide or help you through that financial process. It’s really inefficient.
Let’s say you have a doctor visit and get labs done. You’ll get multiple bills from multiple different providers — from the doctor, from the lab, maybe from someone else — for that same visit. Unless you’re really keeping track and call them, it’s really confusing.
The process that I found that worked the best for me to make sense of this was calling my insurance when I had all these bills in front of me with the reference numbers. [I was] keeping track of the dates in a spreadsheet of the appointments I had and what was done in those appointments. I could reference back to those [when] calling my insurance provider and seeing what they paid out and what wasn’t paid out.

Talking to them, I realized that a lot of times providers might give the wrong reference number. They might say something, or they might try to bill something that’s different.
It’s not a fluid process; it’s not automatic. There are people behind the process, so there’s tons of human error that happens that affects you in potentially the thousands of dollars.
Unless you call 2 or 3 times to different places and figure out where the error might be, why something was billed the way that it was, you’re just going to be stuck paying those thousands of dollars, which could have been maybe a hundred dollars or something else. It adds up. All those mistakes add up on your end.
What’s your advice for dealing with payments?
I learned from a friend that had surgery before and had gone through this. He said to get set up on a payment plan so you don’t have to pay everything right away.
Because it’s a medical bill, they can’t charge you interest on those payments. You can easily pay $100 down a month or whatever you can. They’re willing to work with you.
If you can prove a monetary hardship, there’s a chance they will lower that bill for you. You just have to ask. Knowing you can ask for that type of thing is really important.
How to be your own advocate
I absolutely stand behind being your own advocate in multiple ways. Going to the doctor and getting a second opinion in the very beginning. Doing your research before going into the appointment. Maybe your doctor has one avenue of treatment.
You looked up something else that might be a little more experimental that you want to try. They’re maybe a little more conservative, so they didn’t bring it up.
You absolutely need to take ownership and do your own research so that you’re prepared when you come into the office, into those appointments, and you can actively participate in your treatment plan. Secondly, really being your own advocate in saying if something doesn’t feel right, bringing that up and not letting it go.
For example, if you don’t feel right and if you go in the hospital, doctors have a certain playbook. They know to look for certain symptoms. They know to look for certain conditions and parameters, but outside of that, they don’t think too much outside the box. You might be an edge case.

Unless you advocate for yourself in your voice, your situation could get worse. That’s absolutely important.
When it comes to the monetary aspect of things, being your own advocate and going to the hospital or the doctor’s office or the lab, it’s in their best interest to get paid in some way. For you to even ask for some sort of reduction in your bill based on you paying it, they might be open to that.
Probably the best way to do that would be to say that if you’re able to reduce the bill this certain amount, I will pay it all right now. That’s the best course that I found to getting that done. I would say just be an active participant in your treatment and also the payment.
»MORE: How to be a self-advocate as a patient
Mila’s Message
I’m Mila, and I am a cervical cancer survivor. The message I want to get out there is you can get through it. It’s going to be hard. You’re going to need support, but there will be a day when you look back on that time, and it will be far in your rearview mirror.
You’ll go on with your life, and it will strengthen the person that you are. It will help you see life for what it is and not stress nearly as much about the everyday little minutiae, because the good news is you’re alive and you don’t have cancer.

Inspired by Mila's story?
Share your story, too!
Cervical Cancer (Squamous) Stories
Mila L., Squamous Cell Cervical Cancer, Stage 1B1
Symptoms: Abnormal lump in cervix area, bleeding after sex
Treatments: Chemotherapy (cisplatin), radiation, adjuvant chemotherapy (carboplatin & paclitaxel
...
Marissa N., Squamous Cell Cervical Cancer, Stage 3B
Symptom: Excessive and prolonged vaginal bleeding
Treatments: Chemotherapy (cisplatin), radiation, brachytherapy
...
Brittany W., Squamous Cell Cervical Cancer, Stage 4B
Symptoms: Spotting after sex, eventual significant bleeding at random
Treatment: Chemotherapy (cisplatin) concurrent with radiation, 6 rounds adjuvant chemo, 2nd round radiation, immunotherapy trial, targeted therapy
...
Kate R., Squamous Cell Carcinoma of Unknown Primary Origin, Stage 3C
Symptoms: Intermittent spotting during or after sex, unpredictable menstrual cycle, abdominal pain particularly under the rib cage
Treatments: Chemotherapy (cisplatin & paclitaxel), immunotherapy (Keytruda), surgery (total abdominal hysterectomy with bilateral salpingo-oophorectomy & omentectomy)
...
Chrystal M., Squamous Cell Cervical Cancer with PALB2 Mutation, Stage 3C
Symptoms: Pain during intimacy, irregular menstrual periods, abnormal bleeding (sometimes heavy), severe exhaustion, pain in left leg and groin area (deep vein thrombosis), lump in left armpit
Treatments: Surgery (installation of inferior vena cava filter), radiation therapy (brachytherapy), chemotherapy
...



