Brittany’s Stage 4B Squamous Cell Metastatic Cervical Cancer Story
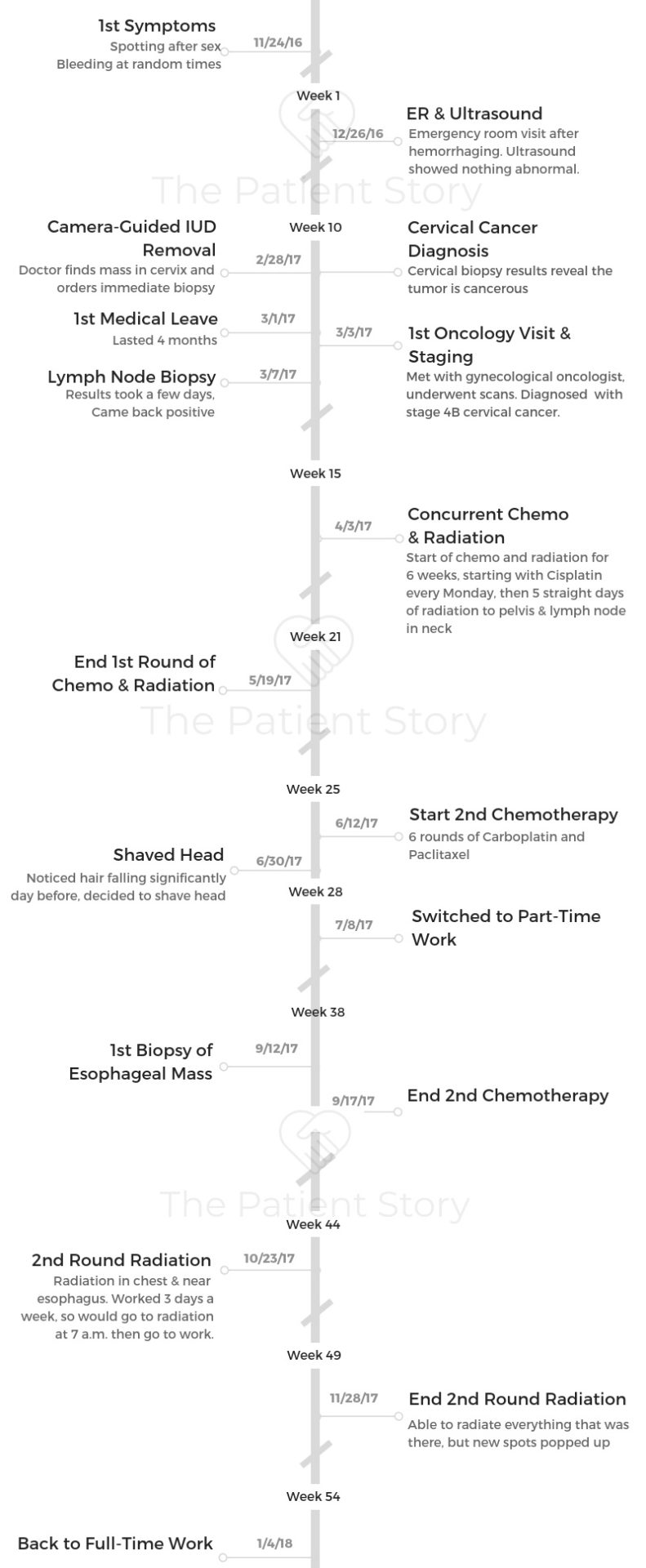
Brittany shares her stage 4B metastatic cervical cancer story, diagnosed at just 30 years old. She detailed her first round of chemotherapy and radiation, second round of chemo and radiation, undergoing immunotherapy, and targeted therapy.
In her in-depth story, Brittany also highlights the issues that were most important to her to navigate: losing her hair, dealing with no real standard of care, how to be a self-advocate, and the impact on her marriage.

You’re doing great. Keep it up. I just look back at all of the doubt that I had every step of the way. I think every day that you live with cancer, you’re a cancer survivor.
Every time you wake up and decide to have a good day and get through what you need to get through, you’re doing amazing.
Brittany W.
- Name: Brittany W.
- Diagnosis:
- Cervical cancer
- Squamous cell carcinoma
- Stage 4B
- Age at Diagnosis: 30
- 1st Symptoms:
- Spotting after sex
- More spontaneous bleeding
- How Diagnosis Happened:
- Hemorrhaging led to emergency room stay
- Ultrasound didn’t detect anything at first
- Brittany pushed to have IUD removed
- During camera-guided removal surgery, doctor spotted massive tumor
- Biopsy revealed cancer
- Tests and Scans Pre-Treatment:
- Ultrasound
- Biopsy of pelvic mass
- PET/CT scan
- Fine needle aspiration (for staging)
- Treatment:
- Concurrent chemotherapy (cisplatin) and radiation
- 2nd round of chemotherapy
- Carboplatin and paclitaxel (Taxol)
- 6 rounds
- 2nd round of radiation
- Focus area: chest and near esophagus
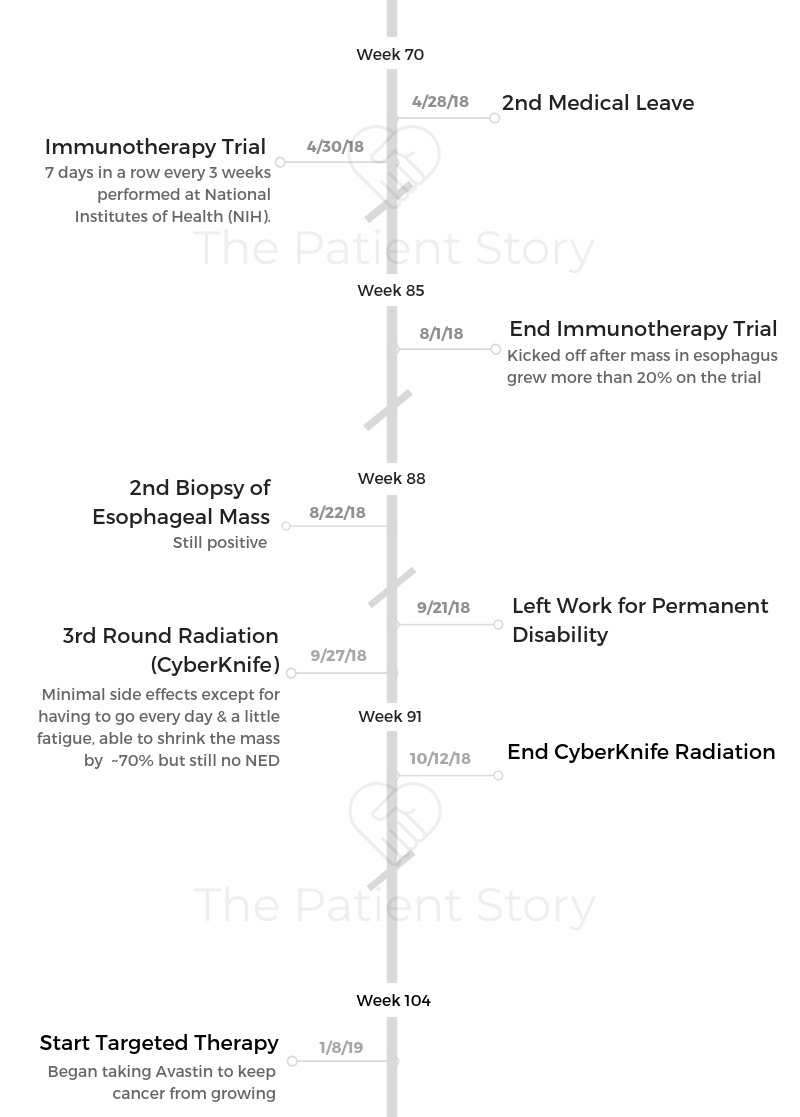
- Immunotherapy
- National Institutes of Health trial
- Ended when one mass grew more than 20% during trial
- Targeted therapy
- Avastin for indefinite period
- Goal: to keep cancerous tumors from growing
- Diagnosis
- Tests & Staging
- Treatment Decisions
- Chemotherapy & Radiation
- 2nd Round of Chemo & Radiation
- Describe the 2nd round of chemotherapy
- Describe each cycle of that chemotherapy
- What were the 2nd chemotherapy side effects?
- Describe the 2nd round of radiation
- What were the 2nd radiation side effects?
- You underwent no surgery
- What was the result after this second round of treatment?
- Describe the moment you realized you still weren’t at "no evidence of disease” (NED)
- Immunotherapy
- CyberKnife Radiation
- Targeted Therapy
- Dealing with no standard of care
- Hair Loss
- Financial Support
- Emotional & Mental Care
- What helped most with the emotional and mental stress?
- How do you approach thinking about life and your future?
- What kind of outside support was most helpful?
- Did you and your spouse have different styles in approaching treatment?
- How did the diagnosis impact your relationship?
- What’s your message to those dealing with the same or any cancer diagnosis?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
It started off with a little bit of spotting or bleeding after sex. I remember it very clearly the first time it happened because it was Thanksgiving morning, and I was with my husband.
I was totally freaked out. I put it on the back burner because it was Thanksgiving. I chalked it up to having an IUD.
I made a lot of different rationalizations in my head.
A few weeks later, I ended up going to get a pap smear, and I was bleeding. I wasn’t supposed to have my period. It was my first time seeing that gynecologist. She reprimanded me, “You know you can’t come when you’re on your period.” I told her I wasn’t.
One thing led to another, and I was telling her about this. She said, “Okay, you know it is probably your IUD. I can’t see it right now, so I’m assuming that maybe it’s shifted or something, and that’s what’s causing this.”
Cut to a few weeks later, I was asked to make an appointment for an ultrasound. My insurance was saying, “We can only do it 6 weeks out.” I was waiting for an ultrasound, and then on Christmas Eve with my whole family around, my in-laws and my parents, I started hemorrhaging.
That really scared me, but I didn’t want to say anything because it was Christmas. I had my whole family here, and in a way I guess I was being a little willfully ignorant about the whole thing.
The next day, I ended up in the emergency room because it had happened again overnight. I spent the day after Christmas in the emergency room. I was there for 10 hours.
They did an ultrasound, but they told me they couldn’t see anything. They didn’t know what was wrong with me. They put me on birth control, saying I had something called “irregular bleeding” or something. But I knew something was off. I kept pushing to get the IUD out.

What led to the diagnosis?
Finally, I went to have the IUD surgically removed with a camera. The woman who did that procedure happened to be the specialist in gynecological biopsies.
As soon as they put the camera in my cervix, they saw a huge, massive tumor, and she was able to biopsy it right that second. They actually had another doctor come back to the hospital to confirm that it was a cancer diagnosis.
I woke up from thinking I was having a quick IUD removal to seeing my husband and asking him what happened, if they had got it out.
He told me no. Right at that moment, I just knew something was really wrong.
That night they told me I was anemic because I had been hemorrhaging so much. “You have to be in the hospital. You need a blood transfusion. This is definitely a cancerous tumor, and you need to start seeking treatment right away.”
After that, I went and met with the gynecological oncologist, and they did all of the scans. At that point, they diagnosed me with stage 4 cervical cancer.
You had to deal with misdiagnosis
To make matters even worse, when I had gotten the pap smear, it had come back for HPV. My doctor had referred me to get a colposcopy.
They cut some tissue and test it from your cervix, but they wouldn’t do the colposcopy because they said I was bleeding. They said, “We have to get the IUD out before we can do the colposcopy, because that’s what’s causing your bleeding.” But really it wasn’t at all.
They had been putting off actually doing the test that could’ve diagnosed the cancer. It was a really challenging time.
I have several women I know from the cervical cancer community who have had very similar experiences.
Describe the first biopsy
The biopsy wasn’t done until the end of February, actually. They had put me on this birth control and said, “You just have some irregular bleeding.” I was like, “Okay, whatever.”
I had gone to get the IUD out at another appointment. I’m not sure how familiar you are with IUDs, but generally a gynecologist can just pull it out and be done with it.
For whatever reason, they kept scheduling this appointment to get it out, and then they couldn’t see it. They couldn’t figure out why they couldn’t see it. Turns out it was because there was obviously a massive tumor in the way.
But they just kept saying that the IUD had shifted. It took me until the end of February of that year to actually get the proper appointment and get the diagnosis, even after I had gone to the emergency room.
Describe the 2 months before your diagnosis
There was more bleeding, more hemorrhaging. I remember being at World Market and having to run out because I was just hemorrhaging.
I was starting to develop really intense lower back and hip pain on my left side. I had been working out constantly, and I just thought that’s what it was from.
Again, I don’t know if I was at the time fully convinced of that, but wanting to think that. I was feeling progressively, progressively worse, to the point when I finally did get my diagnosis, I was almost relieved. Not relieved, but I just felt like this all made sense now.


How did you process the preliminary diagnosis?
My husband actually broke the news to me about the cancer. He had been informed by the doctor, who did the biopsy before I even woke up, that they found something and they were pretty sure it was cancer.
My husband was the one that told me. The doctor had asked him not to say anything to me until she was able to confirm or come back in the room.
When I asked him if it had worked and what was wrong, he said he just couldn’t lie to me or say anything. So he just spilled it.
‘They found something, and they think it’s cancer.’
I was just completely overcome with all different types of emotion. Like I said, relief. But of course, just utter, utter sadness and fear.
It’s kind of weird. I don’t know if this is something you would share with everybody, but I’ve always felt like in my life, I’ve always been waiting for the other shoe to drop or something.
When my doctor told me that, sitting in that hospital room, something clicked, and everything made sense in a way, even though it was absolutely terrifying and the scariest moment of my life.
»MORE: Reacting to a Cancer Diagnosis
How did you break the news of the diagnosis to your loved ones?
I was with my husband. I remember not being able to call and tell my mom. I asked my husband to do that. They admitted me to the hospital that night because I was so badly in need of a blood transfusion.
I broke the news to my family and friends. It was hard. For my parents, my husband is the one who originally told them of the diagnosis. I called my best friend, who’s really more like a sister to me, honestly. I’ve known her since I was 8. I told her.
At that time, I said I assumed it would be an early stage of cancer. I just thought, “Okay, I have this, and we’re going to get through this.” I remember I was more concerned about their feelings and telling them these things than I was about myself at that time.
When I had to tell my parents about the staging, that was hands down the hardest thing, having to tell them that I was stage 4B. That night I think I had a crazy, large glass of just gin to get through it.
I just remember saying, ‘It’s really not good, you guys. I’m going to do the best I can, but it’s really not good.’
My husband thankfully has been an amazing caretaker in all of this and has done all of the research and everything. He was able to research more of the details.
I found having to tell other people to be literally the hardest thing about this. I find it so hard to have to share with my loved ones.
»MORE: Breaking the news of a diagnosis to loved ones
Tests & Staging
What were the tests, scans, and biopsies that you had to undergo?
- Ultrasound
- Pelvic mass biopsy
- PET/CT scan
- Fine needle aspiration
When I went to the emergency room, I underwent an ultrasound. I don’t know why that didn’t pick up anything, but apparently it didn’t. After that, I had the original biopsy of the mass in my pelvis.
Then I had a full PET/CT scan, which showed that it had spread to lymph nodes and my abdominal area. Then also it spread to a lymph node in my neck. I had to have what is called a fine needle aspiration, which is basically a biopsy that they do.
They stick a needle in a lymph node if it’s surfaced, if it’s close enough to your skin. That did come back and confirm that the lymph node in my neck was positive for cancer. That’s how we ended up getting not only a stage 4, but a stage 4B diagnosis. That’s the absolute worst one you can get.
That literally all happened within 3 days, so I was going, going, going, constantly doing things to get the diagnosis.
There were doctor appointments every day. Then that Friday, when I knew I had all weekend and I got the final diagnosis, that’s why I collapsed a little. All the tests were done; all of that was done. It was just those words. Then you go home and somehow try to continue your life.
The only question I could get out was, “Can I still do yoga?” I do a lot of yoga now, but at that time, I don’t know why I asked that. I thought it would make me seem healthier or something. I just remember how dumb I felt after I said that.

Describe the pelvic mass biopsy
It didn’t hurt at all. I was put completely under general anesthesia. It was supposed to be a quick in-and-out procedure. Basically they put you under. and you go home that same day.
No issues. It wasn’t painful. Because they had found me to be so anemic, that’s where all the complications had come in.
The biopsy was a couple of hours because they basically weren’t going in to biopsy it. They had to scramble and get everything together while I was on the table.
Describe the PET/CT scan
I had never done one before. I’m someone who suffers from anxiety, so I remember being really, really scared about going into the machine. I’d always heard that people with anxiety or people that are afraid of close quarters don’t do well.
I was more scared about flipping out and having a panic attack than I was about anything that would come up in the results.
Honestly, it wasn’t as scary as I made it out to be. They did pretty heavily sedate me at that point, but that’s okay.
If there’s a message there, it’s okay to ask for Xanax if you’re scared of the imaging machines, or just if you’re scared about getting them.
I had to be in the machine at that time for about 15 or 20 minutes. I’d never had a scan like that before, where you’re fully immersed in a machine that’s completely surrounding you for that long. I never had one like that.
Describe the fine needle aspiration
The fine needle aspiration biopsy also wasn’t painful, but just very scary. That one, you’re under local anesthesia, and you can tell someone’s basically digging around inside your neck.
It’s just very uncomfortable, but also very quick. The fine needle aspiration was maybe 10 minutes total.
How long did it take to get staging?
Staging only took a few days. We worked really, really quickly. That night when I was in the hospital, I had emailed my work and said, “Look, I’m not going to be in for probably a week. I have some crazy health stuff going on.”
Within a couple of days, we had gotten the staging. I went into the hospital on a Tuesday, and it was that Friday actually when I got my official diagnosis.
Do you remember the moment you got the staging?
After scans and everything, when I was told it was actually stage 4, I lost my thought of, “I can get through this. I can do anything.” I really just fell apart for a few days at that point.
They had prescribed to me some sort of narcotic pain pill for all of the pain I was having in my back. They told me on a Friday, and I totally felt medicated for that entire weekend.
My parents were down, and I just look at myself in photos from that time or even a little bit before that. I just see how gaunt and drawn I looked. I didn’t have any blood, so I distinctly remember just sitting in the little exam room with my back up against the wall with my husband.
The doctor told me it was stage 4. “We’re going to give you the best that we’ve got, but we really don’t know how much good it will do.”
At that point was when I was really like, “Holy shit. I don’t know if I can do this.”
Treatment Decisions
Did you get a second opinion?
I did decide to get a second opinion, because I knew you have to be your own advocate.
I’m lucky enough, living in the Washington, D.C., area and having the insurance that I have because my husband’s active-duty military. I was easily able to get the referral for a second opinion and go to Johns Hopkins.
I saw a really great gynecological oncologist there who was a woman, which for some reason made me feel better. Up until recently, every single one of my doctors had been male. I was able to meet with her, and she said, “I know your doctor at that hospital you’re going to. I think this is the absolute best course of action.”
Let’s be honest, at stage 4B, there’s not a ton of options there. If you can, you undergo radiation and chemotherapy, and those are really your only options. Just hope that they knock out as much of it as possible.
But I still thought it was important to see another doctor and ask the questions because I wouldn’t have been able to forgive myself if I had left something on the table.
»MORE: How to be a self-advocate as a patient
How did you decide where to get treatment?
I didn’t really have any options there because my husband’s active-duty military, so we have to go to military medical facilities. I ended up with this team of doctors because that was my only option, unless I had gone to Johns Hopkins for the second opinion and they said, “Absolutely not. We would do things completely differently.”
Then I could have left to go somewhere else. I ended up getting treatment at Walter Reed, where I’m still getting treatment, just because of how our insurance system works.
Is the hospital you’re at now a smaller hospital or larger medical center?
I would characterize it as pretty small because you have to be either active-duty or retired military to go there. I don’t know how many people that they treat, to be honest. I would say it’s probably a smaller hospital. It’s not MD Anderson or the Mayo Clinic by any stretch of the imagination.
What have been the pros and the cons to the hospital size?
We’ll start with the cons. Even though my team is amazing and they work with the best of the best, I feel like I have to really advocate for myself because they are a smaller hospital. Especially being a military hospital, dealing with the gynecologic cancer.
I’ve had to do my own research [to] see what clinical trials are offered around at different places. It just helped to be on top of that for myself. I think at some of the larger hospitals, there are more resources there, as far as that goes.
The pros are definitely that I feel really comfortable there because I know my doctors really know who I am individually. I have what’s called a nurse navigator. I know a lot of places do this, but any time I feel any weird ache or pain, feel like I need a prescription, or feel like I need a test or something, I can just text her. She always gets back to me within an hour.
I just love being able to have that. It’s a big asset to me. When I was at a bigger center, if I had any questions, I’d have to submit a question through a form. “Then we’ll email you back.” There are a lot more levels of bureaucracy there.
Describe getting the port put in
I got the port put in a couple days after my diagnosis, before I even had a second opinion. They said they needed to move and no matter what kind of treatment I did, I would probably need some sort of infusion, so I got the port put in.
The procedure was fairly easy. They put you under local anesthesia. You basically don’t feel any pain, but it’s uncomfortable, and there’s some tugging.
They put you in what I think is called a twilight sleep, so while you’re not necessarily completely zonked out, you’re not really aware of what’s going on. It’s a pretty quick procedure, maybe 30 minutes.
How was recovering from port surgery?
What I was not expecting was how painful the recovery was, or maybe I had just been so jilted by that point, I didn’t care. I had made plans to hang out with my friends that night of getting the port placed, and I was in so much pain just from the whole procedure that I couldn’t even think straight.
I remember I ended up leaving, going home, and just taking the pain pills they gave me and going to sleep for the rest of the weekend, because this was also on a Friday.
I was a little surprised by that. People are always like, “I’m getting my port line placed,” and everyone’s like, “Oh, it’s no big deal, blah blah blah. You’re fine.”
I always want to be that one detractor who says, “Not to scare you, but just so you know, it can be a little painful afterwards. Just don’t plan anything. Take the time to recover.” All of that.
That was something, but I obviously recovered in a couple of days. People tell me I’m really lucky because the scar isn’t very pronounced, so that’s good.

Chemotherapy & Radiation
Describe the first round of concurrent chemo and radiation
The original treatment, my first treatment I had was a combination of chemotherapy and radiation. The chemotherapy was intended to boost the effects of the radiation.
I did that for about 6 weeks, where I would get cisplatin every Monday. Then I would do a full 5 straight days of radiation to my pelvis and to the lymph node in my neck.
For about 6 weeks, I did cisplatin every Monday, which was through an infusion, like regular chemotherapy. The intention of that chemotherapy was just to boost the effects of the radiation therapy.
I went every day, every Monday through Friday, for 6 weeks to radiation every day to have radiation to my pelvis and to the lymph node in my neck.
What were the treatment side effects?
I believe it was about 2 hours every Monday. Right after that, I would go into radiation. I didn’t really have any side effects directly from that cisplatin chemotherapy.
It generally doesn’t give you a lot of side effects. They also had me on a great deal of steroids and anti-nausea to combat any of the side effects.
I would say some of the side effects of the steroids, as I think anybody who’s had chemotherapy knows, almost seem worse. I’d rather just be nauseous than deal with some of the steroid side effects. I just never could sleep. I always felt out. I just didn’t feel right.

But from the radiation, it started off on an upward swing. I started to feel better because it was working, and the pain in the neck was going away. Let’s say that’s the first 2.5 weeks of the 6 weeks.
Then it starts to go downhill a little bit, where it’s like you’re no longer getting all of that excitement from the good effects of it, and you’re starting to get more tired and more nauseous. I remember I went to lift a box with clothes in it, and I almost passed out. I was so weak and so tired.
What helped with those radiation side effects?
During that time, I had to have 3 or 4 blood transfusions because I was already fairly anemic from all of the hemorrhaging. A lot of your red blood cells are made in your pelvis, so if you’re radiating your pelvis within an inch of its life, your body can’t make blood cells.
There were several times when I would get lab work done, come home, and have them be like, “You need to come back. Your red blood cells are so low. I don’t even know how you’re functioning.”
That was definitely a lesson to self-advocate because I just assumed that that’s what it felt like to have cancer. I didn’t think, “Oh, there’s something wrong.”
It’s a side effect of something, and so that was a really good lesson for me to learn that you don’t have to feel terrible.
»MORE: Cancer patients share their treatment side effects

Describe the blood transfusions
It’s like a chemo infusion, except there are no side effects. You just sit there over the course of a couple of hours, and they slowly provide you with red blood cells or white blood cells or just blood, whatever it is that you need.
When they would have to do emergency transfusions, I would have to go stay overnight. They basically wake you up every hour to check your blood pressure, and you stay overnight. Then you could go home if your cell counts are where they should be.
What were the steroid side effects?
For the steroids, it was [during] the summer. I remember I went on a beach trip again because I was like, “I won’t be different with my girlfriends.” I didn’t know why at the time, but I felt like a massive beast. I hated the way I looked in a bathing suit, and I just couldn’t understand it. I wondered how I gained all of this weight?”
I had lost a lot of weight from the radiation. It makes you lose weight sometimes, and I couldn’t understand it. Not until even maybe 6 months ago did I realize, “Oh, that was the steroids making me feel that way and act that way.”
I was really emotional all the time. I just chalked it up to my body and all of that. I didn’t realize that it was probably from the steroids.

I guess another thing that came out of this is learning you don’t have to keep pushing. There were many things that I would do when I was so anemic that I had to come in and have an emergency blood transfusion are insane to me.
I think I went jogging one day, and I was just like, ‘Oh, I mean, I guess this is how it feels to jog with cancer.’ I had no idea what I was doing to myself for a while, and because I also just refused to give in.
No matter how bad I was feeling or whatever, I refused to just allow myself to be sick, and that was a lesson I had to learn as well.
Did the radiation side effects get better?
You start to feel better from radiation helping where your tumors are. My back pain went away, and it’s really good. Then on radiation, you just start to get so fatigued, so I had blood transfusions.
Also, because where they were radiating on my neck was so close to the skin, I got terrible burns all down my neck. My friends were like, “Just use aloe vera, like real aloe vera from the leaf. That’s all you need.”
I was putting that on, and it wasn’t getting better. Finally, I got the burn cream from my radiation oncology nurse, prescription, and within a few days, the burns were completely gone it seemed. I suffered for no reason.
2nd Round of Chemo & Radiation
Describe the 2nd round of chemotherapy
It was 6 rounds of carboplatin and paclitaxel. That’s when I had more of your traditional chemotherapy regimen. We had great luck with the radiation. Basically apart from completely curing me, it did as best it could.
However, as it’s getting all of the spots that were originally there, new spots were kind of popping up because radiation is a local treatment, whereas chemotherapy is kind of systemic, meant to get everything.
I did a round of chemotherapy to try to get anything that was left behind or anything that might’ve popped up while I was doing radiation.
Unfortunately, after 6 rounds of that kind of traditional chemotherapy, I still had a couple spots left, so that’s when I went into another round of radiation.
Describe each cycle of that chemotherapy
It was every 3 weeks. I would go on Mondays, and that infusion was about 5 hours. I would get there early in the morning. They would do sulfates and just kind of fluids and stuff, and then do the infusion over 4 hours, I believe.
What were the 2nd chemotherapy side effects?
For chemotherapy, the side effects hit me really hard, really quickly on the first round. I was tired all the time. I was nauseous. I don’t know. I never felt like I was going to throw up, but I just constantly felt like things were spinning. I had really bad bone pain, which is awful, like pain that stretches out in the bones.
That was really bad the first time I got it. I think it took me about 4 or 5 days, maybe even 6, to get over those side effects. My husband said every time I got the chemo, you could just see the color draining out of my face and my skin turning yellow over the 4 hours.
That kind of cycle continued every infusion but got better. By the end of it, my recovery time was maybe 2 days instead of 6 days, but I still experienced the same kind of side effects every time I would get a cycle of it. Then, also, it did make my hair fall out.
Honestly, I’m very lucky. I say all the time that I take to the medications and the treatments very well. I’m very lucky in that, so they can push them as much as possible without having to worry about me having really negative side effects.
What I was saying about everything can be good news, to me that’s one of those things that was good news for me. Even though maybe the treatments aren’t always working 100% like we’d like them to, they’re not necessarily making me super sick and really robbing me of a lot of my life, so I feel very grateful. I’m very happy for that.
Describe the 2nd round of radiation
After those 6 cycles of chemo, we found that everything that was originally cancerous had gone away. However, a couple new spots had popped up in lymph nodes in my lungs.
At that point, they said, “We can start to look at the clinical trials. We don’t think chemotherapy is good for you because obviously it allowed these other spots to pop up while you were on it. We can do radiation on the spots that are there and hope nothing else pops up, or we can start looking for clinical trials.”
I elected to do radiation again at that time. It was over Thanksgiving. Again, I had radiation in my chest and near my esophagus. I actually worked during that time. I worked 3 days a week, so I would go to radiation at like 7 a.m. and then go straight to work.
What were the 2nd radiation side effects?
Same kind of side effects. My biggest side effect there [was] since it was near my esophagus, it became kind of challenging to eat just because there was scar tissue building up.
It was right over Thanksgiving, too, but luckily I stuck through it. I kept being able to eat, thinking we’re going to have to put in a feeding tube, which I inevitably did have to have at a different point. It was like, “No, I’m not doing that. I’ll be fine. I’ll eat mashed potatoes. I’m not doing that.” I was able to get through it.

You underwent no surgery
No, I’ve never had surgery as an option. When I was first diagnosed, it’s like the cancer was so rampant that to remove it just didn’t really make any sense because they would’ve had to take out so many lymph nodes and things.
To this day, we’ve never really discussed [surgery]. Well, we have discussed maybe surgically removing a mass that I had in my esophagus a couple months ago, but it was in a very precarious place, so to remove it surgically was a very high-risk surgery.
What was the result after this second round of treatment?
Unfortunately, during that time, new spots popped up. We were able to radiate everything that was there, but new spots popped up, and that’s when I started on a clinical trial.
Describe the moment you realized you still weren’t at “no evidence of disease” (NED)
That was hard for me. That was a hard day because we all talk about the anxiety or whatever. That was a time the anxiety was the worst because it was either, “There’s no evidence of disease and come back in 3 months,” or, “There is evidence of disease, and we’re starting to run out of our options.”
It was really hard to hear that we didn’t get the news that we wanted to get.
I was working. I was back at work and in the middle of a huge conference where I was speaking at, and I had to leave early to go get my scan results. It was like, “Either I’m going to be really happy at the end of this day or really, really sad.”
It turns out that I was really sad. I definitely didn’t go to work the next day, and I just kind of took that afternoon and the next day to just be sad and process.
I almost tear up thinking about it now, but after that day, I was like, “Okay, what’s next? Let’s look at clinical trials.” Then we started exploring them.
Immunotherapy
What do you remember of your conversation with your oncologist considering new options?
They were like, “We need to maybe explore something.”
There were 2 different trials they wanted me to go up for. The one was basically they used your cancer cells to grow some sort of vaccine. I don’t know very well or don’t remember very well all of the details because I had so many of these conversations, but I wasn’t eligible for that one because for whatever reason, my cancer didn’t have the correct marker.
Then I ended up doing an immunotherapy trial, which was a little bit less specific for cervical cancer, but I was still eligible for it.
Describe the immunotherapy trial
I was on that from about May to July. I was excited to pursue clinical trials because I do think cancer treatments are constantly, constantly improving and evolving and getting better.
Not only was I excited for my own medical benefit, but there is something that feels really good about being able to participate in maybe creating a treatment for others.
Also, it wasn’t a hard treatment. There really weren’t any side effects. It was basically an injection. I would have to go for 7 days in a row again, every 3 weeks.

What were the results of the immunotherapy trial?
Unfortunately, it didn’t work for me. It was not successful. Basically, while I was on this immunotherapy trial — and this is at the National Institutes of Health over the summer — there was a mass again in my esophagus that started to grow. If you have more than 20% growth on this trial, you can’t be on the trial.
Also, because the mass was in my esophagus, everyone was really concerned that it was going to start obstructing my ability to eat and swallow, which it eventually did. I hate to use the term “kicked me off,” but I was kicked off the trial, and I went back to my regular oncology team to try to figure out what we were going to do now about the mass in my throat.
What were the next steps?
At that point, they said, “We’re going to biopsy you, and then we’re going to come up with a treatment plan.” My head of gynecological oncology team had transitioned out, so a new doctor was coming in.
For those of us who have had to go through lots of different types of treatments, I was just over it at that point, so I took a little bit of a break.
We did the biopsy. I wasn’t having any specific symptoms at that point, so my doctors were like, “Let’s chill and think about this for a little bit.” I went to a music festival.
I needed a break from all of this because I couldn’t think straight anymore. Again, now we were running out of even more options, right?
»MORE: Read more patient experiences with immunotherapy
What happened when the symptoms returned?
That was all well and good. I had my few weeks off, but when the symptoms did start coming from the esophagus mass, they came on really, really quickly.
I ended up in the emergency room, not being able to swallow any food. That’s when I had to have the feeding tube placed, which again, I was entirely against. But it was so bad, they were really afraid I would aspirate or something, so they basically forced me into getting the feeding tube.
Because I was in the hospital then, the conversation was very different. My team was working really hard to figure out what we were going to do because I’d already had radiation to that area. At a certain point, you can only be radiated so many times in the same area.
This was kind of the scariest time for me of this whole thing because when I ended up having to go the emergency room, I thought, “I might not ever leave the hospital at this point. If there’s nothing they can do, this might be where I start just getting sicker and sicker.”
At that same time, I was very solution-oriented, wanting to start looking at treatments. I was in the hospital. I really wanted to do radiation to that area, and they were able to do something called CyberKnife treatment.
CyberKnife Radiation
Describe the CyberKnife radiation
I had thought that because I had been so successful under radiation before, that just to shrink the mass enough so that I could eat normally and get rid of the feeding tube. At that point, that was like, “This is all I want to do. Let’s just focus on that.” We were able to do that.
Luckily, my radiation oncologist is amazing. He told me he’s given me the most radiation dosage he’s ever given anyone, which I appreciate him for. I was like, “This is what I want to do. Do it. I’ll be fine. I’ll make it through. I’ll do what I need to do, but I need you to go hard and get rid of this thing ’cause I need to be able to eat.”
We did the radiation, over 2 weeks of CyberKnife therapy.
What were the CyberKnife side effects?
Honestly, the side effects were minimal except for just having to go every day and a little fatigue, but really they were minimal.
What were the CyberKnife results?
We were able to shrink the mass by about 70%.
Now I could eat. I’m good. I can do all of that stuff. Basically, where I am now is on the other half of that treatment. After the radiation, I wasn’t symptomatic, so I felt like I had a little bit of time.
I wanted to explore clinical trials because I didn’t want to commit to palliative therapy at that point. I really still wanted to be no evidence of disease and still see if the right opportunity arose.
Targeted Therapy
What options did you consider at this point?
I talked to Mayo Clinic. I talked to MD Anderson. I did a lot of research about other clinical trials and other types of chemotherapy, but ultimately, there was really nothing for me that was better than just doing the palliative chemotherapy at this point.
There was one clinical trial that used a certain type of immunotherapy that I was eligible for, but it was a big ask physically and mentally, and I just didn’t think it was the best option for me at the time.
It was really hard to say no because you want to just always go hard. I’d rather be alive than have hair. Also, at a certain point, part of being your own advocate is you can’t just let people push you into something because it’s available.
You have to really weigh the cost-benefit analysis to yourself. Through all of that, that’s when I had my most recent scan, which actually showed up better than my oncologist was expecting.
You decided to go on targeted therapy (Avastin)
Now I’m on Avastin, which is considered palliative. My last scan was at the end of December. My second dose or my second round of this is on Wednesday. I just had my labs and my meeting with my doctors this morning.
How often are you taking Avastin?
It’s every 3 weeks, so every Wednesday I take it.
»MORE: Read more patient experiences with Avastin
Dealing with no standard of care
How do you deal with the lack of standard of care for the disease?
I guess I just kind of feel like this is my way of life now. Because of how advanced my diagnosis was, I never really went into it thinking that I would have the traditional story of you do the chemo, then you’re cancer-free, and then you go on to be a survivor.
I’ve always kind of taken issue with how we describe a survivor. It was also like #LifeAfterCancer. When you’re going through this, maybe you’ll never be done being treated, and that’s a blessing.
Every treatment that I go through is a blessing because it’s keeping me alive that much longer. Who knows what clinical trial they will come up with in a month that might be great for me?
I don’t have to put my life on hold until I don’t have cancer anymore. I have life with cancer. I treat it like a chronic disease, like people that live with all different types of diseases that constantly have to get treatments, dialysis, things like that.
I look at it in that way. It might always be a part of my life. I didn’t put my life on hold to battle cancer. Battling cancer is going to be a consistent part of my life.
Even if one day I’m in remission, it’s still going to be a consistent part of my life, and that’s okay. That’s okay. It doesn’t stop me from doing anything I want to do. In fact, it’s brought some opportunities to me that I might not have had before, so I think that’s important to remember.
New perspectives on life
[It brings] opportunities for perspective. I’m currently not working because I’m lucky enough to have a good disability insurance, but I never would have this time to myself to think about what I do.
And absolutely perspective. I don’t know, but I’d rather live 5 years with the perspective I have now than forever with the perspective I had before my diagnosis.
I feel like it sounds selfish in a way because I know that my friends and family suffer a lot, but I’m really much happier with life now. It’s true. When you find out life is fleeting, it does change your perspective.
You feel gratitude
I hope that does come through because I am very grateful for the things that I do have that make this easier on me.
There are people that if someone else had the same diagnosis as me, I could’ve been much different because I’m just so lucky to have a lot of resources and a lot of people around me.
Be a self-advocate
Absolutely. Not just in terms of diagnosis, but in terms of all of your treatment. If there’s one thing I learned, you have to be your own advocate, as much as we know that our doctors are there for us and want to take care of us, and whoever else in our community that’s helping with our treatment.
You have to stand up for yourself [and] make sure that things are being done properly and how you want them to be done. I don’t blame this entirely on my doctors, because like I had said, I was being a little willfully ignorant about the whole thing.
If I hadn’t kept pushing and pushing, who knows how much longer I would’ve gone without a diagnosis?
»MORE: How to be a self-advocate as a patient
Hair Loss
Describe the hair loss
It was hard for me. Losing my hair was really, really hard for me. I was a little surprised by my reaction because I joke all the time, “I’m incredibly vain and insecure. I love my own reflection. I’d rather be bald than dead,” or whatever.
It was the first time throughout the entire process that I didn’t feel like myself.
When you look in the mirror, you don’t see yourself anymore when you don’t have eyebrows [and] you don’t have hair, no matter how good the wig is. When you look at yourself, you still don’t see you.
That was really hard for me. I remember I knew when my hair was going to start falling out, and I just tucked it up like a messy bun for about 8 days. I didn’t wash it. I didn’t touch it.
Then the night of my best friend’s 29th birthday, I wanted to wash my hair. I wanted to shower; I couldn’t go out like this. I basically just pulled my bun off my head. It was just all hair in my hands. I was like, “Oh, my goodness.”
That was the first night I ever wore a wig out in public. I hated wearing wigs, but I did it. I tried to see the positive side to it. You can definitely wear easier with a wig than your own hair.
I had this hairstylist friend of mine just shave it because I felt like that was going to be easier than waiting to watch it fall out.
»MORE: Patients describe dealing with hair loss during cancer treatment
How did it feel after shaving your head?


After I had my head shaved, I met up with a friend for lunch. I went out without a wig on or a scarf on with just my shaved head. I was okay with it. The problem, though, is having a shaved head than having no hair at all, once even that stubble starts to go away, you really feel like an alien. Once I lost my eyebrows, that was really, really, hard.
I’m still struggling with my hair growing back. It’s at a place where I finally look at mirror and feel like I look like myself. Finally. It’s been 18 months since my hair started growing back. It’s taught me a lot about vanity, what a person can endure, how little it matters how our hair looks [or] how perfect our eyebrows are.
It taught me a lot about my relationship — the fact that my husband never looked at me differently once. That meant a lot. That definitely meant a lot.
What helped most with the hair loss?
Losing your hair sucks, and it’s hard, but it’s a great plan to experiment with looks that you never in a million years would ever do. When my hair was shorter and just growing out, I dyed it platinum blonde. I loved it.
I have crazy chemo curls, but I just tried to focus on the side that’s either different things that I never would have done in the past and I get to play around with my style for. That’s something to take away from it.
Financial Support
How was dealing with finances?
As far as that goes, super, super lucky that I’ve had great insurance and great support. My husband is in the military, so obviously he has a very stable job and a very generous leave package. I’m very lucky in that regard.
I was about 30 when I was diagnosed, and I’d finally gotten the job that I have dreamed of. I got to travel. I finally felt that I was really coming into my own professionally, which is something that was important to me. I worked on and off.
Luckily, my company was great to me and let me take long leaves of absence for when I needed to or let me come back and work part-time when I wanted to or work full-time when I wanted to.
Could you work during treatment?
Ultimately in April, when I needed to start the clinical trial, I decided to kind of give up work. It was really hard for me, but again I looked at it like it’s not forever.
Right now, I need to be in the business of getting better.
I’m lucky enough to have resources to devote myself 100% to that cause and not have the added stressors of competing. I owe that to myself. Not only do I owe that to myself; I owe that to all of the people that love me.
A lot of times I feel I’m perfectly fine, and tomorrow I’m going to spend my day going to yoga, to lunch, [and] living like I would never expect to be able to live. I look at that as like I need to be doing that right now so that my body can feel itself as best as possible.
It’s okay. You don’t have to do it all. If you can take a step back from your company, then you are more than entitled to do that.
»MORE: Patients talk about working during cancer treatment
Emotional & Mental Care
What helped most with the emotional and mental stress?
I don’t know. I feel like it sounds cliché where you just kinda take it day by day and revel in the small victories. Again, it goes back to me just being grateful that I have the insurance that I have.
I’m grateful that I don’t have a lot of terrible side effects. Grateful that the lymph node that is positive for cancer. It’s just to the right of whatever organs that it could bother.
I just try to focus on the positive of what’s happening around me. I don’t know where I heard this, but growing up I always had this slogan: ‘There’s always someone that’s done a lot more with a lot less. ‘
I just remind myself all the time that even though it’s bad, it could be worse.
Also, I treat my illness like my job in that when I’m dealing with my cancer, getting treatment, or I’m not feeling it because something or another, that’s like my work time. That’s what I do then. It doesn’t define who I am as a person at all.
How do you approach thinking about life and your future?
It’s something that I struggled with. I’d love to have a baby. I know I can’t have my own baby, but I’d love to have children. I don’t know if that’s ever going to happen for me because I don’t know what my disease will be like for day to day.
The thought about struggling with your mortality is so hard. I’ve gotten the worst diagnosis.
Remain resilient. I will even say just fight hard. If you do what you’re supposed to do, things will fall in line however they are supposed to fall in line. You’re not going to survive and you’re not going to beat this thing by feeling sorry for yourself or ignoring it.
If you let the idea that stage 4B or whatever diagnosis, if you let that destroy who you are before it kills you, it’s already done what it came to do. I just feel like, ‘Well, I feel good.’ I want to take advantage of every opportunity that I have.

The other thing is we’re 2 years from my diagnosis. Honestly, I could have had pretty much like 6 months, and I’m better than I was when I started off.
You never know what treatment is going to come up. You never know what new thing will happen, so just keep plugging away at it. I guess that’s all. That’s a very heavy topic for me to think about.
What kind of outside support was most helpful?
I love to cook and so does my husband, and so I definitely think it’s the meal thing for a while.
So many people were constantly asking, ‘What can we do?’ It almost becomes another thing to manage as part of your illness.
I guess I’m really lucky because my best friend — she’s also named Brittany, not to get confused. She called herself the VIP or the VP of “Brittany’s Cancer Corporation.”
Basically, she did all requests for what can we do. You can sign up to bring the meal 2 days a week or something. We did that for a while. I like to cook. That’s like one of the things that I can do to relieve my tension.
I will say, just being willing to come over and sit with me and hang out, drink wine on my couch, and not make me feel guilty for always having to have things at my house felt so good.
Because you want to hang out, but especially when you’re actively going through certain types of treatment like radiation and chemo, you never know when you’re going to hit the wall and be like, “I’m done.” The last thing you want is to be out in some bar in DC and have to Uber home and all that.
It was really nice that for a good 8 months, my friends just formed a cocoon around me. We were going to do stuff, but only on my terms. It really helps.
»MORE: What kind of support cancer patients say helped the most
Did you and your spouse have different styles in approaching treatment?
Yeah, for sure, which is good in a way. My husband is an army guy. He sees a problem, [and] he thinks, “Assess, analyze, problem, solution.”
I’m very emotional. I like to not necessarily deal with things very well. He just jumps right in.
This is also something that I think caregivers and friends can do for the patient. Whenever I had a question about one of the medicines I was taking or how effective things are, that can be a really dicey. The last thing you want to have to look up is how effective is this type of chemotherapy, because honestly the results won’t make you feel good.
It was really nice that I could always go to my husband or my best friend. “This has been hurting me,” or something, and they would actually do the research for me and kind of help [and] be honest with me. I didn’t end up having to fall into this terrible information overload about everything cancer-related. That really meant a lot to me. That’s something a lot of caretakers can do.

How did the diagnosis impact your relationship?
I would say it’s impacted our marriage in mostly good ways. I’ll be frank. I have cervical cancer. I’ve had a lot of radiations to my pelvis. It’s certainly impacted our sex life. I just think honestly you’re not feeling particularly attractive and beautiful.
No matter what your partner says to you about how wrong you are, [it’s] very challenging to get that out of your head.
I definitely had to regain confidence in myself as my husband’s sexual partner. That’s a challenge, and I’ll say that’s something I’m definitely still working on, which is okay.
Again, I feel very lucky because I don’t know that we would ever be as close as we are if — well, we were always very close. I never saw any issues, but I never imagine that you can be as close to someone as I am now with my husband because of what we’ve gone through.
Just conversations that we’ve been forced to have or just seeing him rise to the occasion every time. It really makes you grateful for someone. Same with my friends and family, but my husband definitely the number-one caregiver for me, so he deserves all of the credit.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
What’s your message to those dealing with the same or any cancer diagnosis?
You’re doing great. Keep it up.
I just look back at all of the doubt that I had every step of the way. I think every day that you live with cancer, you’re a cancer survivor.
We’re cancer survivors no matter what we do. Every time you take a step in the right direction, every time you wake up and decide to have a good day and get through what you need to get through, you’re doing amazing.
It’s like that Kim Kardashian gif where her mom’s like, “You’re doing amazing, sweetie.” I would tell that to myself, and I would tell that to every cancer patient. You’re doing amazing. Don’t give up on yourself.

Inspired by Brittany's story?
Share your story, too!
Cervical (Squamous) Cancer Stories
Mila L., Squamous Cell Cervical Cancer, Stage 1B1
Symptoms: Abnormal lump in cervix area, bleeding after sex
Treatments: Chemotherapy (cisplatin), radiation, adjuvant chemotherapy (carboplatin & paclitaxel
...
Marissa N., Squamous Cell Cervical Cancer, Stage 3B
Symptom: Excessive and prolonged vaginal bleeding
Treatments: Chemotherapy (cisplatin), radiation, brachytherapy
...
Brittany W., Squamous Cell Cervical Cancer, Stage 4B
Symptoms: Spotting after sex, eventual significant bleeding at random
Treatment: Chemotherapy (cisplatin) concurrent with radiation, 6 rounds adjuvant chemo, 2nd round radiation, immunotherapy trial, targeted therapy
...
Kate R., Squamous Cell Carcinoma of Unknown Primary Origin, Stage 3C
Symptoms: Intermittent spotting during or after sex, unpredictable menstrual cycle, abdominal pain particularly under the rib cage
Treatments: Chemotherapy (cisplatin & paclitaxel), immunotherapy (Keytruda), surgery (total abdominal hysterectomy with bilateral salpingo-oophorectomy & omentectomy)
...
Chrystal M., Squamous Cell Cervical Cancer with PALB2 Mutation, Stage 3C
Symptoms: Pain during intimacy, irregular menstrual periods, abnormal bleeding (sometimes heavy), severe exhaustion, pain in left leg and groin area (deep vein thrombosis), lump in left armpit
Treatments: Surgery (installation of inferior vena cava filter), radiation therapy (brachytherapy), chemotherapy
...




