Kelly’s Stage 3C Triple-Negative Breast Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Kelly was diagnosed with stage 3C triple-negative breast cancer at 33.
She regularly did breast self-exams when one day, she noticed a golf ball-sized lump on her left breast near the armpit. In that instant, she broke down and just knew that this was breast cancer.
She shares how she became a staunch advocate for herself to the point where she started treatment without an oncologist because she knew that the doctor she had then wasn’t the right one for her.
She also shares the importance of open lines of communication with your medical team, especially when she was experiencing serious mental side effects from tamoxifen.
A year after her diagnosis, she founded TNBC Thrivers on Instagram, an online community that seeks to bring together women with a similar diagnosis.
In addition to Kelly’s narrative, The Patient Story offers a diverse collection of breast cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
TW // Suicidal ideation
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Kelly T.
- Diagnosis:
- Triple-negative breast cancer (TNBC)
- Staging:
- 3C
- Initial Symptoms:
- Golf ball-sized lump in the left breast
- Treatment:
- Chemotherapy: doxorubicin, cyclophosphamide, paclitaxel, carboplatin, capecitabine
- Surgery: nipple-sparing, skin-sparing double mastectomy
- Radiation
- Hormone therapy: tamoxifen


Introduction
I’m a stage 3 triple-negative breast cancer survivor.
I am a content creator and founder of TNBC Thrivers on Instagram. I’m also the chat host for the Triple Negative Breast Cancer Foundation.
Besides all that, I’m a wife and a cat mama of two. I work in finance. I love travel, fashion, and makeup. That’s me in a nutshell.
Pre-diagnosis
Initial symptoms
I saw doctors regularly. I always did my breast self-exams. I checked my breasts every time I was in the shower and never felt anything.
One day, I folded my arms and noticed something that wasn’t there before. It was huge. It felt like a golf ball on my left breast. I checked the right one thinking, Do I have anything like that going over there? I immediately broke down and cried. I thought, This is breast cancer. I know this is breast cancer.
Ironically, I volunteered a lot with my local breast cancer organization in October. As soon as I felt that lump, I thought, I help women that deal with this. I think I’m about to become one of them.
No one in my family had breast cancer. They’ve had cancer but not breast. I didn’t test positive for any gene mutation. I was 33 years old. No one knows why I got this.
Getting an initial appointment
I immediately called my gynecologist. I had to wait a little bit to get in with her. She’s fantastic. She has been the backbone of finding my cancer doctors throughout my treatment.
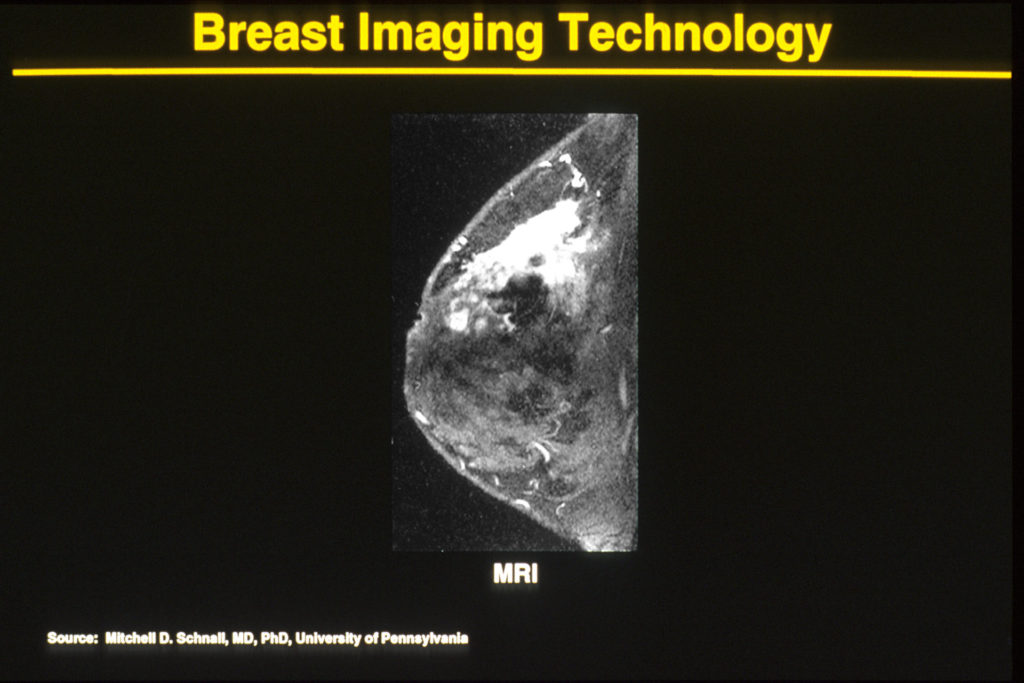
She looked at me and said, “You’re young. You’re 33. It could be nothing, it could be something,” so she sent me for a mammogram and an ultrasound. That took another few weeks to get in.


When I had the mammogram, as soon as they began, they knew it wasn’t good. They said, “The doctor doesn’t like what he’s looking at. We need to do the photos again.”
I never had a mammogram before. I’m trying to keep it together so badly and trying not to cry because the first thing I want to do is cry. As soon as they said that, I just let it all out. I know this isn’t good and it’s not good.
We did the imaging again then I went across the hall for the ultrasound. They took images on the screen. I grabbed my phone, took photos, and thought, There’s something here. There’s something not good here.
The doctor came back in and said, “We want to do a biopsy immediately.” The biopsy happened in a day or two, but the biopsy results took a whole week, which is a very long time. You think, No news is good news, right? But it was the worst possible news.
Diagnosis
Getting the biopsy results
I had a kidney stone at the time and I fully believed that my body wasn’t going to get rid of that kidney stone until I found out I had breast cancer.
I was working and had to leave because I was in so much pain. I said, “I need to go to the doctor. I need to go to the hospital because I need to know where this kidney stone is.”
They took me in and scanned me. It was the day I was supposed to get my phone call. They wheeled me out of the room to get my scan and I came back to see a missed phone call from my gynecologist. She sounded happy. She said, “Hey, Kelly, it’s so-and-so. Give me a callback.” I said, “All right, awesome.”
She called and said, “You have breast cancer and you need to find a breast surgeon immediately.” It was like whoa.
The doctor came in and said, “This kidney stone is so, so close to your bladder but also, we see a mass on your left breast.” I said, “Screw the kidney stone. I got breast cancer.”
I worked with the American Cancer Society every October for the yearly walk. Being in finance, I worked in the finance tent. We organized the deposits and all the donations that they would get. I thought, People get breast cancer all the time and they’re totally fine.


She had to knock me down a little bit and said, “You need a breast surgeon immediately. Time is ticking. I hope you don’t mind. I already made an appointment for you with the breast surgeon at the hospital here.” I was so honored. How could I mind?
First of all, when I got the news, I was all by myself in a hospital bed. It was such a breath of fresh air. My mom didn’t know what to do. This is so foreign to us. We don’t know the first thing about breast cancer.
Learning about the triple-negative diagnosis
I met with my breast surgeon and she told me about the oncologist that I would be meeting with, who is the head oncologist at the hospital. She called him up and found out he was on vacation. She said, “We have no time to waste. You’re at least stage 3. You need to see his partner.”
I thought I caught this early. As soon as I felt it, we did something about it and it was already stage three.
I went with my husband to see his partner. We did the tumor marker test and it came back elevated. I got a 75 on that, which meant there was breast cancer present in the blood.
We sat down with this gentleman and he said I had something called triple-negative breast cancer, what my treatment plan would be, and that I would need chemotherapy, surgery, and radiation guaranteed.
He turned and looked at me and said, “Kelly, people die from what you have.” I talk about that all the time and it shakes me so much every single time. Five years later, it’s still so hard to say out loud.
I thought, No, I’m 33 years old. My life is just beginning. I just got married at 27 years old. I’m thriving in my career and doing big things. I can’t. I can’t die. I said to him, “You’re not going to let me die.” He looked at me and said, “I’ll do my best.”
I’m not angry at him. Sometimes when things don’t work out, they actually do work out. You can’t appreciate the sweet without the sour.


Changing oncologists at the start of treatment
The day before my first chemotherapy with this oncologist, I fired him. I was the career woman I was, very in control, even though I was so scared and so nervous and had no idea what was about to go through. This is not the doctor for me so I fired him before my first chemotherapy and got the doctor I was always supposed to have.
I feel like my current oncologist was always supposed to be a part of my story and he’s just absolutely phenomenal. I fully believe that I would not be here without him and I wouldn’t appreciate him as much if I didn’t go through what I went through. I cannot wait for the day that I get to see the first oncologist and say I’m still here.
Anytime I had an issue, I would reach out to my breast surgeon. My breast surgeon is a tiny lady, but you don’t mess with her. She will come for you, especially when it comes to her patients.
The first oncologist messed up a bunch of stuff. He wasn’t returning phone calls. I had no idea when chemotherapy was starting. The quantities of the pre-meds that I got from the pharmacy before I started chemo were all messed up. I said, “All right, enough’s enough. This is my life here.”
I reached out to my nurse navigator, who was side by side with her, and said, “Give me Cohen. Give me the doctor I was supposed to have.”
I knew this guy was something special. If you’re an elder millennial like me, back in the 2000s, there was a show called The O.C. Who was the best character on The O.C.? Seth Cohen because he was the funniest.


My husband and I loved The O.C. I don’t even think my oncologist knows this story. We found out I’m going to be with an oncologist by the name of Dr. Seth Cohen. We immediately looked at each other and I said, “I’m gonna be okay. We’re gonna be okay.” That was our big, funny aha moment with that.
I Googled his name and found stories of him successfully treating patients with aggressive cancers and those who didn’t think that they were going to make it and they’re still here. You say his name in the hospital and people start to shake. I thought, I don’t know who this doctor is, but I need him. He was supposed to be mine and I’m going to ensure that he is mine.
Treatment
Chemotherapy
We had two separate treatment plans. The first oncologist was only going to give me eight chemotherapy sessions considering my aggressive stage of cancer. Looking back on it now, I don’t know if I’d be sitting here if I stayed with that doctor. With his plan, I was only supposed to get four AC (doxorubicin and cyclophosphamide) and four Taxol (paclitaxel) then do surgery and radiation.
I did that first chemo without an oncologist. A lot of people don’t know that my first oncologist came to my first appointment and confronted me about firing him, which speaks to his own professional character. I’ll never forget it.
I went with my husband. The first day of chemo is such a long day. Your nurse comes in and explains everything that you need to know about chemotherapy.
As soon as she left to get the chemo, the oncologist walked in and said, “I hear that you’re going to whoever.” I said, “Are you seriously confronting a cancer patient on the day of their first chemotherapy?” He left and the nurse walked in. She looked like she saw a ghost.
She said, “I’ve been a nurse for 25 years. He was standing outside of the room listening to us the whole time. I’ve never experienced anything like that in my life.”


The following week, I finally met my new oncologist, Dr. Cohen. He busted through the door and said, “I heard you’re starting trouble in here.” I thought, This guy is awesome.
He said, “I reviewed your plan. It’s good, but mine’s better. With the initial plan, you may get a home run, but I’m going to knock it out of the park.”
His plan was to do four AC, eight Taxol, and four carboplatin. Back in 2018, not a lot of patients that weren’t BRCA were doing carboplatin. But considering it was already stage 3C, he said, “Carboplatin is a metallic chemotherapy and it can be very hard on the body. But you’re 33 and I think you can take it. If you’re my sister, this is exactly how I would treat you.”
Side effects of chemotherapy
We did AC first. Nowadays, they save it for the end.
My first round went very well. I didn’t have any side effects. I said, “I am superwoman, I can do this thing.”
As for the second and third, that was a totally different story. I was extremely nauseous that I didn’t want to do it anymore. I didn’t want to leave my house. My friend would pick me up and drive me around just to go driving. You have car sickness the whole time.
I tried everything. When you’re so desperate for something, you’ll try anything. Even the pre-meds that they give you to help with nausea didn’t do anything.
I said to my oncologist, “It’s bad. I don’t even know if I can continue going on.” He said, “No, you’re going to hang with me. We’re going to get through this and we’re going to figure this out together.”
I actually helped him come up with a way to help me. I was on Decadron (dexamethasone), Zofran (ondansetron), and Ativan (lorazepam). I would take them and would still be nauseous, but he would have me take them in a certain order.
I had this idea. “What if I took them all at the same time?” He said, “They won’t counteract so nothing bad will happen.” We put our heads together and that was the secret sauce.

I was on a lot of steroids. If you look at old photos of me, I do not look the way I look today. My oncologist lovingly said it would make my head the size of a football field but that was about it. I gained 13 lbs during chemotherapy because of the steroids. I also went on a health journey.
You’re fighting cancer. You get diagnosed with what they’re saying is the worst breast cancer to get. You have in the back of your mind the doctor who said, “People die from what you have,” so weight gain is the least of your worries. I just don’t want to be nauseous. Let’s get through this and, hopefully, this all works.

Surgery
Preparing for surgery
I was so anxious about having surgery. It was my first surgery ever. I never had a stitch, never needed anything. Going through treatment and surgery was the part that stressed me out the most.
I literally waited two weeks before surgery to tell my breast surgeon what surgery I wanted to do, even though when we first met, it was a double mastectomy, hands down.
You are the CEO of your body so it’s still your decision on what you want to do. There might be a high recommendation for a certain type of surgery.
I was so nervous that I was starting to make a decision based on fear of what surgery was going to feel like vs. choosing a surgery that would benefit me in fighting cancer. I went back and forth between a lumpectomy, which seems less invasive, and a double mastectomy. I knew the decision I had to make. Sometimes you have to make decisions and do it scared.
Nipple-sparing, skin-sparing double mastectomy
My breast surgeon specialized in nipple-sparing mastectomy. It wasn’t that I sought after that because I’m fighting cancer, nipples or no nipples. Most breast cancer patients lose their nipples because sometimes the tumor is very close to it. Mine was in the armpit area.
If the doctors can save them, they will. I highly recommend saving yours if you can do it because it helps a lot with recognizing your body after surgery and having self-love again. They save the skin, too. I know a lot of times they cut the skin. My incisions are underneath my breast.
I was mentally prepared. I’m still going to identify with my own body. I’m just going to have more scars on my chest.
My surgery took a long time, about seven hours because I had my plastic surgeon in there as well. He put in expanders. I had under-the-muscle surgery so he helped me start the reconstruction part of the surgery.


Discussing with your surgeon
I would say definitely get opinions. There’s a lot about breast reconstruction and surgeries that I didn’t know.
A lot of times when you’re in that space, the information goes in one ear and out the other. With any kind of appointment that you have, I highly recommend always having somebody with you.
I had no idea there were different options: under-the-muscle surgery, over-the-muscle surgery, you keep your nipples, you lose them. There’s never a good time to have cancer, but I’m so glad I had cancer during social media because I learned so much about so many different surgery types that I didn’t even know.
I don’t know anything about breast cancer nor did anyone in my family or friends. Luckily, I had the best options laid out for me, but that’s not always the case. Everything worked out in the best possible way for me.
Some doctors are going to recommend procedures that they want to do; maybe not necessarily procedures you want to do. I scream that a million times on social media, especially when it comes to breast reconstruction. Sometimes it’s really hard to pick what breast reconstruction you want. Do you want to use your natural tissue? Do you want to use breast implants? There are complications with both.
I met with a plastic surgeon in the middle of chemo. She spent five minutes with me and said, “You need radiation. I would never give you breast implants. In fact, if it was up to me, I would talk you out of getting radiation for that reason.”
Another situation where I was so scared about having surgery, but I was very firm in having the comfort of being with a doctor that I completely trusted. You’re rebuilding my body. I knew that plastic surgeon wasn’t meant for me.
I go back to my breast surgeon and tell her. She said, “All right. I’m very close with this one plastic surgeon. Let me give him a call.” She called him and said, “I can get you in tomorrow at 8:30 in the morning.”
He is by far one of the best doctors on my team. I’m very, very blessed to have so many amazing doctors. He’s just phenomenal. Again, sometimes when things don’t work out, they actually work out. Sometimes you have to go through the bitter doctors to appreciate the sweet doctors.


Recovery from a double mastectomy
Recovery was the worst, but if I had to do it over again, I wouldn’t have changed a thing.
A lot of patients do over-the-muscle surgery now. I think it’s easier for both the surgeon and the patient.
When you do under-the-muscle surgery, they cut muscles and take a tissue expander, which is basically like a deflated implant, and put it underneath. You need to heal from the incisions and have them remove the tissue and if there is a tumor left. I slept in a recliner for a month and a half.
Radiation
I healed from the double mastectomy and then went on to the plastic surgeon. I met with him weekly and he would do fills where they fill saline in. I was doing I think 60 cc a week, which is actually pretty low. You can do more, but they can be uncomfortable.
Meanwhile, my oncologist asked, “Are you at radiation? What’s going on?” I said, “I’m getting my fills. We cut the cancer out, right? I’m fine now.” He said, “No, we’re not fine now.”
Ironically, my plastic surgeon and radiation oncologist fought at my first radiation appointment. My plastic surgeon said, “I get her next.” My radiation oncologist said, “No, she’s a cancer patient. I get her next.”
I had to get my medical oncologist on the phone and he said, “Kelly, you’re going to radiation.” We got all the fills in, got fully expanded, and then did radiation. I did 28 rounds, which is about a month and a half.


Side effects of radiation
Radiation was interesting. Some people say this is the easy part. With chemotherapy, you’re very nauseous, you have to shave your head, you don’t feel well, and all that. Surgery is physical because you’re being opened up. Radiation is like a bad sunburn, which is how they explain it to you.
I would say radiation is more mental than physical, although it is physical. As you go on and your skin gets red and you start to burn a little bit, it does feel like a sunburn.
There were times when I was lying on the table, crying, and I can’t tell you why. I was just sad. I’d be in the changing room, putting my regular clothes on, and I would just sit there for five minutes and cry. It was such an emotional part of the treatment.
I know they say that depression and anxiety is a side effect of cancer treatment. I don’t know if they know what exactly causes it, but you just feel overwhelmingly emotional and have sadness and it’s almost like you don’t know why.
It wasn’t like that all the time. You would get spurts and it would eventually subside.
Radiation is tricky. Breast implant surgery, especially having what they call delayed breast reconstruction, could change. It all depends on how well you go through radiation.
I made it my absolute mission to research what I needed to do for my skin to ensure that I could have the surgery that I wanted. I read a lot about different creams.
My radiation department highly recommended Aquaphor. Aquaphor is greasy and could stain your shirt so get a loose-fitting shirt that you don’t care about. I would put Aquaphor three times a day: after treatment, once I got home, and once before bed. I continued even when I finished treatment.
Occasionally, I would have appointments with my plastic surgeon to see how the skin is looking. I did very well. My skin got red, but it never peeled or broke open.

Scans post-treatment
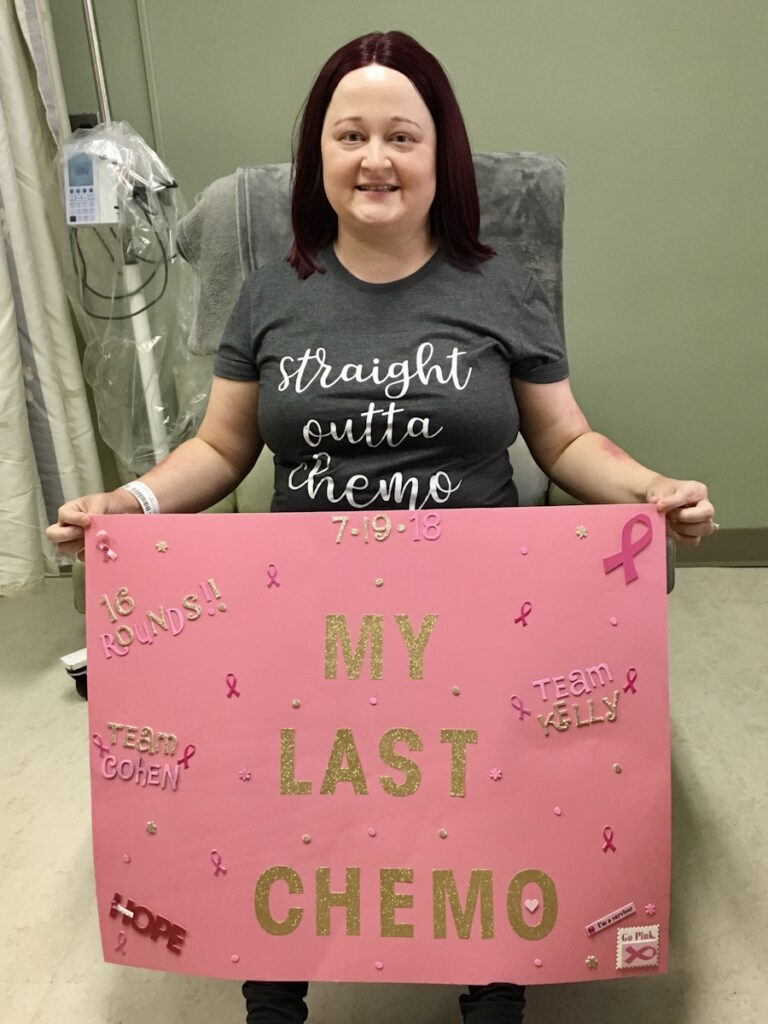
I did six months of 16 neoadjuvant chemotherapy. My breast surgeon ordered a breast MRI once the chemo was done. They looked at the breast tissue and the lymph nodes to see if I got a complete response or not.
At my last chemo, I said to my oncologist, “I’m going to go for this scan, but I need you to give me the results.” He has a very calming aura and I said, “If it’s the worst scan ever, I know I could take that news from you so much better than her. If you give me the news, I can prepare for her.”
My breast surgeon is very serious. She will give it to you straight. Some people like that. Some people like to get told what they need to be told and it is what it is and this is what we’re dealing with.
I’m a more sugar-coated kind of person. I’ve got this aggressive, rare, high-recurrence cancer. I needed a softer approach and that’s my oncologist.
When I first met with him, I asked, “What stage am I?” He said, “You’re at least stage three, but it doesn’t matter because we’re getting rid of it.” I said, “Yes!” If you follow me on Instagram, he’ll pop up on a post every once in a while because he gave me comfort and sugar-coated the stuff that I needed to know and didn’t tell me things that I didn’t need to know.
Getting the results of the breast MRI
After the scan, I met with my oncologist. He put his arm up to give me a high five and said, “We did it. It’s a complete response.” It’s so amazing. I’m crying. I said, “Oh, I got this thing, Let’s go see my breast surgeon.”
I went to my breast surgeon. She looked at the paper and said, “Hmm, we’ll see what surgery says.” I thought, You should be happy. It’s a complete response. That’s what we wanted. That’s the overall goal here.
She was right. She’s never been wrong. I honestly wish that she would look into my eyes and tell me how the rest of my life is going to pan out because whatever this woman has said to me has been completely on the money.

I had the surgery and there is no tumor left. However, there’s cancer in my lymph nodes. Two of eight of my lymph nodes came back positive. But here’s the kicker: it wasn’t triple-negative. It was low-grade, estrogen-positive. I said, “How does that work? Because I was zero on everything.” I had a cancer mutation.
Cancer in the lymph nodes
Cancer is really smart. When you’re getting chemotherapy, it’s dying. It doesn’t want to die. It wants to thrive. It could change its DNA so it could survive. When you’re triple-negative, you get triple-negative drugs so my body started to grow estrogen and the cancer was able to survive and it was already in my lymph nodes at that point.
This only happens to 3% of people. I always hit those low targets for some reason. I felt completely defeated.
After meeting with my breast surgeon, I met with my oncologist and the very chipper, positive-outlook oncologist sat in the office, put his head in his hands, and just sat there.
My mom was with me and I said, “This is terrifying because he’s scared. If he’s scared, then I should be scared.” He looked up at me and said, “Did they explain what this is? Do you know what this is?” I said, “Yes, it’s cancer and it’s estrogen cancer now and I can’t cry anymore. I cried already. I’m done. What are we going to do? What’s the plan?”
The good part was estrogen is very slow-growing versus triple-negative, which is very aggressive growing. By the time they found it, it was still considered low-grade estrogen cancer. Out of the whole cancer cell, only 20% of it was estrogen cancer. The rest of it wasn’t cancer at all.
Hormone therapy & chemotherapy treatment
I was put on tamoxifen and then I started Xeloda (capecitabine). Xeloda is oral chemotherapy. I did that for eight cycles, which is six months.


Side effects of Xeloda
He knows I read everything. He asked, “What are the side effects of Xeloda?” I said, “Hand and foot syndrome.” He said, “You may get diarrhea, too.”
I started Xeloda and within 30 minutes, my stomach hurt. For whatever reason, my body’s very quick to react.
Side effects of tamoxifen
Tamoxifen made me want to unalive myself. I was crazy depressed and emotional. I had very strange thoughts. After three days, we were on the same page and I was able to stop taking it.
When I started tamoxifen, all of a sudden, I started feeling sad and depressed.
When I started radiation, I wanted to lose weight. I was overweight at diagnosis and then gained another 13 lbs, which technically gave me an obese BMI.
I was reading so much about TNBC and came across a statistic that said overweight women have a poorer prognosis. I said, “Absolutely not.”
Being a career woman, you put your health last. This time, I’m going to put myself first and put my health first. I’m going to lose this weight. I’m in the middle of my health journey.
I’m feeling depressed from tamoxifen. I thought, Let me go exercise. Let me get some endorphins released. It was weird because it was like I was mentally me and knowledgeable enough to know what I was experiencing wasn’t normal.
I was getting bad thoughts in my head and thought, Wait a second. That doesn’t sound like me. Why would think that? Why would that pop into my head?


There’s a reservoir by me and I would walk around it. As I was walking around, I was hysterically crying. I called my oncologist and said, “I can’t do this. I can’t take this anymore.” He said, “Let’s give it another day. It’s still very early.” I said, “Okay.”
I got in my car and started driving home. I don’t have any hills or cliffs near me, but I had this thought of driving off a cliff. I said, “No, no, no, no, no, no, no, no, absolutely not.”
I texted him when I got home and said, “I’m getting these very weird thoughts and visions in my head.” He said, “This is not worth the quality of life. I’m not stressing over this over 1% of cancer that you may or may not have.”
It was so low-grade. My oncologist said, “What if they messed up at the lab? What if it was never estrogen? I still think you’re 100% TNBC,” so we just banked on it wasn’t worth even talking about ever again.
I took my last Xeloda in July 2019 and I’ve been cancer-free ever since.
Follow-up protocol
With surveillance, my oncologist does tumor markers, which I know is a whole can of worms in the cancer community. Most oncologists don’t do tumor markers. Mine does. Whenever I share about it, people say, “Why is your doctor doing it and not mine?” I don’t know, that’s just what mine does.
Tumor markers are one of those things that can be unreliable and I think that’s why a lot of oncologists don’t use them, but they’ve always been reliable in my case.
I get CA27-29 where anything over 38.6 is considered high and could be potential cancer. I got a 75 when I was diagnosed. When I initially finished radiation and started Xeloda, I would be in his office every three weeks and we would check the tumor markers. I had scans only if I had symptoms and if there was any kind of issue.


Two-year mark
The two-year mark for triple-negative is a doozy. Everyone talks about the five-year mark and the five-year mark is very important, but the two- to three-year mark is when you are most likely to recur as a triple-negative.
Two years later, I started coughing. I thought, Nope, I’m not going to go there. I’m not going to jump to any conclusions. It started getting worse. I’m in the shower and can’t breathe. I thought, It’s back. It’s in my lungs. TNBC is most likely to recur in your lungs or your brain first before it goes anywhere else.
I went to see my oncologist. The tumor markers were normal so he sent me for a chest X-ray. Having the position that he does at the hospital, he can find out scans very fast. I hadn’t even gotten to my car yet and he texted me and said, “X-ray is clear.”
I said, “You know I don’t make things up. I can’t breathe.” He ordered me a chest CT. He got the results of the scan and called me. He’s not the kind of doctor to call. He said, “I need to review this with your radiation oncologist, but I don’t think it’s cancer.”
There were spots on my left lung and there was a nodule, but we were putting all of our money on the tumor markers that everything was fine. I was prescribed steroids to help with the coughing and it did help. It forces you to stop coughing.
They described my lungs as mucky. They couldn’t really see through the left lung. They were going to wait some time and a re-scan was highly recommended. In fact, the notes from the hospital said, “We don’t think this is cancer, but we don’t think this is not not cancer.”
I re-scanned in a month or so and the lung cleared up. The spots were still there. I have my radiation oncologist on the phone and he said, “This looks like this is what radiation did. You had left-side breast cancer. A lot of times, unfortunately, with left-side breast cancer, your lungs can be affected by therapy. Not cancer and this is how it is.”
A few months later, I was out exercising and I started coughing again. I do very well with being positive and being, “I’m a survivor and cancer is in the back mirror.” I started coughing and it took me back to that place again. I texted him and said, “I’m coughing again.”
We scanned and my radiation oncologist ironically got the results on October 1st and I thought, Great. Breast Cancer Awareness Month. This is when we’re going to find out.
The scan’s totally fine and I get a diagnosis of radiation fibrosis. They saw the spots on the lung again and said, “This is as good as your lung going to look.” It’s something that comes along later on.


When I get these coughing episodes, I get put on steroids. Fast forward to today, I have a pulmonologist and I have to do lung exercises with her. I’m on Symbicort (budesonide/formoterol fumarate dihydrate), a prescription inhaler that has steroids in it.
It’s funny because radiation was the one that they said was so easy, but radiation is the one that gives you some of the longest side effects and hardest side effects. Radiation is the gift that keeps on giving.
Every time I cough, of course, they have to investigate. I know air quality can make me cough. Depending on where I go, my doctor told me to wear a mask. I’m more susceptible to lung illnesses. On one of my birthdays, we went to a rooftop bar, had a great time, and came home from the weekend with an upper respiratory infection.
Starting an online community
I desperately looked for survival stories and I realized that I might need to go out and find these people. Again, going back to that first oncologist when he said, “Kelly, people die from what you have.” I’m going to find the people that are thriving with what I have and living many years.
Let’s be honest. A lot of times, you see bad stories or you’ll see recurrence. A lot of people that go through cancer and get through cancer leave the community and that’s totally okay because you got to do what’s right for you. But when you are always looking at these bad stories, you’re going to think no one makes it out.
I like to say that I was the first one to coin TNBC thriver as a thing. I created it in 2019, a year after my diagnosis. I said, “I’m going to find these people.” I would search hashtags and slide into people’s DMs and say, “Hey, can I share your post? Can you write something for me?” That’s how I started it.


I also started sharing other breast cancers to get eyes on them and say, “Hey, I know you’re not TNBC, but you have an amazing cancer story. I would love to share it.” It became this beautiful community that I can’t even believe that it has become what it is.
People ask, “How do you find the people to share?” I don’t put a call to action. I basically go through posts on my personal Instagram and TNBC Thrivers and anytime someone says, “I’m a five-year survivor,” I reach out to them.
I have so desperately wanted to be a community leader. I sat down with many cancer organizations, young breast cancer organizations, and there wasn’t ever a spot for me. There was never a seat. I was told that I didn’t have a place there and that hurts.
Words of advice
There’s one message that I like to say and it’s something my mother told me: their story is not your story.
When I was diagnosed in 2018, there was nothing on social media where you saw uplifting stories. You had to find them. You had to aggressively search for triple-negative breast cancer and find people.
I remember going on the Internet very, very early in my diagnosis. It’s terrifying. You have TNBC and we have the highest recurrence and the lowest survival. In my heart, I thought, There’s got to be somebody thriving with this. I found stories of someone doing well. Six months later, they weren’t here. Same story over and over and over again.
I would call my mom in a panic, “Mom, I saw this person and now they’re not here. Then I found this other person and they’re not here.” She said, “A few things: you don’t know them, you don’t know their treatment, and their story is not your story.”


I’ve clung on to that so much. It’s so easy to be on the Internet and think, Oh, well, that person has the same type of cancer that I do and their cancer came back so that must mean my cancer is going to come back.
I remember being in year three and someone said, “Oh, my cancer came back in year three,” and I immediately thought, This could be the year for me. That is so not the case.
An oncologist that I’m very connected to said to me, “We know statistics on Google are off. They’re just off. But also what you have to remember is there are so many more medications nowadays that the statistics do not reflect those numbers.”
When I was going through chemo, they were talking about Keytruda (pembrolizumab) being in trial. Keytruda was only available for lung cancer and then for stage 4 TNBC. Now, if you have stages 2 to 3, you’re going to get Keytruda. Keytruda is helping a lot of people. Then you have a drug called Lynparza (olaparib) that wasn’t out before and that’s for people with the BRCA mutation.
There are so many ins and outs with cancer. Cancer is so complex we could not possibly be a carbon copy of each other.
Their story is not your story.

Inspired by Kelly's story?
Share your story, too!
More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy
Nicole F., DCIS, Stage 1
Symptom: Appearance of a lump in the right breast
Treatments: Surgery (lumpectomy), chemotherapy, cold caps, radiation therapy, hormone therapy (tamoxifen)
Erica C., DCIS, Stage 0
Symptoms: Indeterminate calcifications found on a routine mammogram
Treatment: Double mastectomy
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
Alison R., Partially Differentiated DCIS, Stage 4 Metastatic
Symptom: Lump in underarm/breast
Treatments: Chemotherapy, surgery, radiation, targeted therapy
Symptom: Sunken in nipple of right breast
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Symptom: Lump in right breast
Treatments: Lumpectomy, double subcutaneous mastectomy, hormone therapy (tamoxifen)
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
LaShae R., IDC & DCIS, Stage 2B, ER+
Symptoms: Lump in breast, pain
Treatments: Chemotherapy (Taxotere and cyclophosphamide), proton radiation
Dee D., Metastatic Breast Cancer, IDC & DCIS, ER+
Symptoms: Inability to produce milk on the left breast while breastfeeding, breast pain (palpable and radiating to the back), lumps in the breast and armpit
Treatments: Chemotherapy (AC-T), surgery (bilateral mastectomy & axillary lymph node clearance), radiotherapy, hormone therapy (Zoladex/goserelin), aromatase inhibitor (letrozole), targeted therapy (Kisqali/ribociclib)
Cat L., IDC & DCIS, Stage 2B, ER+
Symptom: Pain in left breast radiating from lump
Treatments: Bilateral mastectomy, chemotherapy, hormone therapy (tamoxifen)