Erica’s Stage 0 DCIS Breast Cancer Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

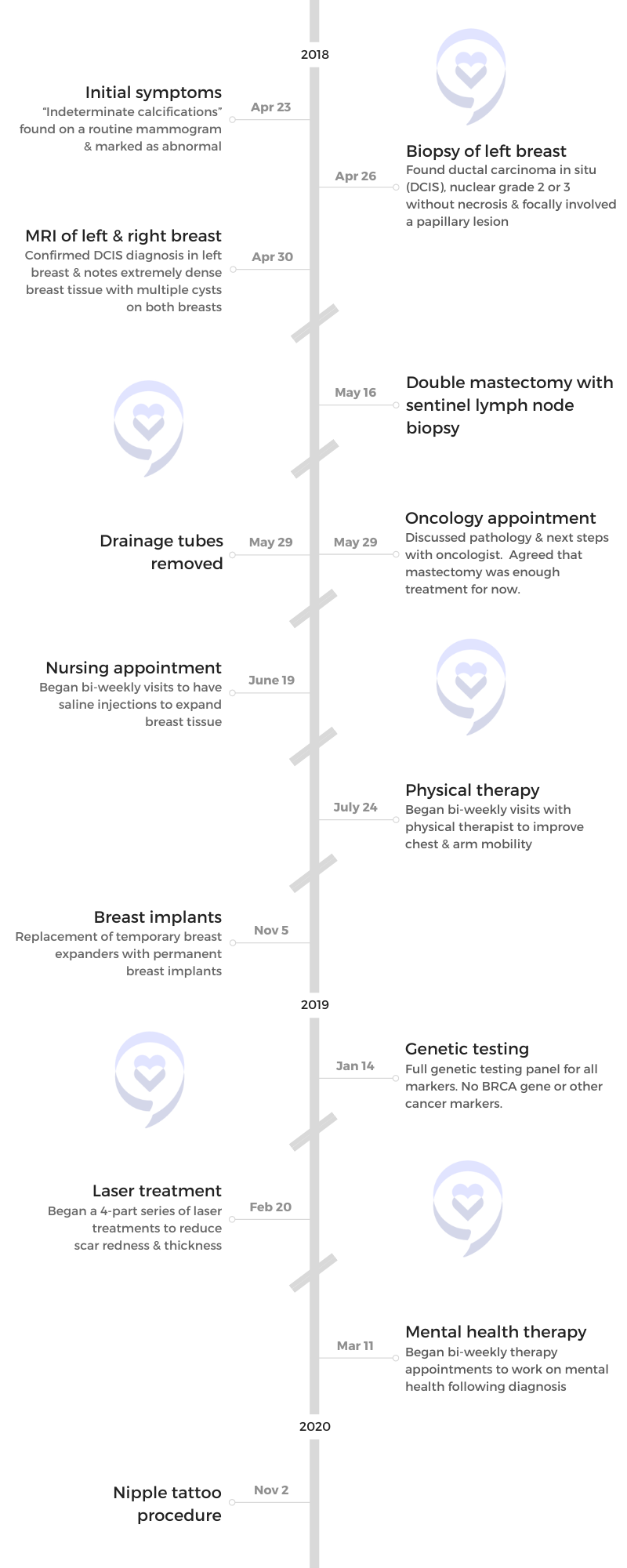
Erica, who lost her mother to breast cancer over 20 years ago, shares her stage 0 DCIS breast cancer journey. After a decade of concerning mammograms and due to her mother’s history, she remained vigilant despite negative BRCA results. Following her biopsy diagnosis, she was overwhelmed by the treatment choices but ultimately opted for a double mastectomy to minimize recurrence risk.
Choosing to undergo a double mastectomy including nipple removal provided Erica with confidence and a cancer-free peace of mind. She subsequently underwent reconstructive surgery and as she embraced her new body, she was more excited about having no fear of recurrence.
She completed her transformation with a 3D nipple tattoo from a specialized artist, providing closure to her journey. Leading a nonprofit for kids with cancer, Erica supports other women and caregivers, emphasizing the importance of trusting oneself and the process when navigating cancer treatment decisions.
- Name: Erica C.
- Diagnosis:
- Breast Cancer
- Ductal Carcinoma In Situ (DCIS)
- Staging:
- 0
- Initial Symptom:
- Indeterminate calcifications found on a routine mammogram
- Treatment:
- Double mastectomy
While cancer is a club you never want to join, once you’re in, there are some silver linings, like the people you meet and the life perspective that you get, and those are true gifts.

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I had increasing scans over the years, but I’d never had a biopsy and that was when I thought this was going to get a little bit more serious.
Introduction
I live in Minneapolis, Minnesota. I’m a breast cancer survivor. I lead a nonprofit that helps children with cancer and their families. I’m also a cancer orphan because I lost my mother to breast cancer over 20 years ago. These multiple perspectives on cancer make me incredibly interested in other people’s journeys and sharing my journey to help other women who come after me.


Pre-diagnosis
I was diagnosed in 2018 and it came after about a solid 10 years of “scary mammograms.” Because my mother died of breast cancer, I was on high alert. I met with tons of doctors who said I have the same risk as any other human in the population. I underwent genetic testing and I wasn’t BRCA positive, but I still didn’t feel good about my health journey given my mother’s unfortunate diagnosis and death.
Over the years, I’ve had mammograms, ultrasounds, and MRIs. They would always see something a little bit scary, ask me to come back for a higher level of screening, and then say it’s fine. It built up this anxiety over the years because they started to see some abnormal things, particularly calcifications, which are potentially early signs of breast cancer.
It got to the point where I thought, When are we going to take this a little bit more seriously? I was getting routine mammograms every six months and one time, they said, “Let’s have a biopsy.” I had increasing scans over the years, but I’d never had a biopsy and that was when I thought this was going to get a little bit more serious.
While stage zero sounds great, it still requires a fair amount of intervention and a fair amount of choice.
Diagnosis
Looking back, I’m not sure if I was surprised by the diagnosis or if I felt like, “Finally.” After the biopsy, I received the diagnosis that it was DCIS, which is ductal carcinoma in situ. It’s an early-stage breast cancer. Many people can say that’s a good kind of cancer, but there’s no such thing as a good kind of cancer.
While stage zero sounds great, it still requires a fair amount of intervention and a fair amount of choice. Being presented with all those choices became the most overwhelming part because it was starting to come at me like a fire hose.


Treatment Decision Making
The choices that I had to make ranged from doing nothing to a double mastectomy and everything in between. I was given the choice of a lumpectomy to remove the part of my breast that showed early-stage breast cancer. I was also given the choice of hormone therapy. I was given a choice of radiation, even the choice of some chemotherapy. It all ranged amongst a spectrum.
My mother’s journey had been a painful one because hers also started as early-stage breast cancer. At the time, doctors said it wasn’t a big deal. As you know by the results, it became a big deal. She relapsed four times over her journey and it came back bigger, stronger, and more invasive every time.
I had all these choices of less aggressive treatment, but I wanted a double mastectomy because I didn’t want this to come back.
For me, it became this choice of how to rewrite the story. How do I advocate for myself in a way that maybe my mom didn’t? Maybe she didn’t have the right information at the time.
I felt more confident facing all these choices and because of what I’d seen with my mom, I went straight to a double mastectomy. I got a lot of eyebrows raised. I had all these choices of less aggressive treatment, but I wanted a double mastectomy because I didn’t want this to come back.
I had all the statistics and all the advice, but within about a week, I became pretty firm in my decision to choose a double mastectomy. People questioned me, but it was the best decision I ever made.


Double Mastectomy
A double mastectomy is a pretty radical choice. Once you choose a double mastectomy, they remove your breast tissue. A choice that you get to make is whether you want to also remove your nipples or if want to try to keep them through a nipple-sparing surgery.
For me, this was a fear-based choice. If I was going to do such an invasive surgery to essentially remove two near-lifetime body parts, I wasn’t going to leave anything to chance, so I chose to have my nipples removed as well.
I chose to go under the chest muscles, which is more painful but ensures the longer-term security of the implants.
Reconstructive Surgery
The other choice I had was whether or not I was going to have reconstructive surgery. I can buck the stereotype and say I don’t need breasts. I’ve already had children and was done breastfeeding. But I chose to have reconstructive surgery.
At the time, it was a very extensive surgery. It’s done in two parts, which is what I didn’t realize at first. I was in surgery for 8 to 10 hours. The first four were simply removing my breasts. I had a breast surgeon who was going to take out everything and some lymph nodes to test. Then the breast surgeon handed me off to a reconstructive plastic surgeon.
To me, plastic surgery sounded vain and unnecessary, but I had to get comfortable with having a breast plastic surgeon come in. For the next four hours, that surgeon cut into my muscles. I could have gone over my chest muscles, but I chose to go under the chest muscles, which is more painful but ensures the longer-term security of the implants.
My surgeon said, “It sounds like you’re all in and that you’re confident. This is going to be more painful, but you will have a better outcome with the implants. They’re not going to move around. They’re going to be secured into your chest. Trust me.” For somebody who I’ve just met to say, “Trust me,” is quite possibly the greatest leap of faith.

At the end of that surgery, not only did he cut underneath my chest muscles, but he essentially put two deflated balloons under my chest muscles and then sewed me up.
After that eight-hour surgery, my job was to heal and make the choice of what I wanted my breasts to look like afterward because, over time, he would fill those balloons with saline to expand my chest. If you’ve ever had dental braces, that’s the kind of soreness and pain you feel when they’re expanding your chest over time. It’s a wild ride and it was painful.
I didn’t realize how much I used my chest. When you raise your hand, that’s your chest muscle moving. I couldn’t touch my nose so when my nose itched, I had to have someone else scratch my nose for me. It was scary and painful, but I still stand by it being the best choice I ever made. I healed and have full mobility now. I can work out, do push-ups, and everything.
They look great. I can wear a bikini and you would never know.
Post-Mastectomy
Right after surgery, you start flat-chested with what looks like Frankenstein stitches. They are not pretty. What’s interesting is that every week, when I would go to the nurse or the doctor, they would say, “Oh, this is going to look amazing. I could see it.”
These sort of deflated balloons come with what seems to be a metal top that’s placed under my skin. Every week, they would put a magnet on my chest to find where that metal piece was and that’s where they would pierce my skin and inflate the balloon with saline a little bit at a time. This took about three months. It’s quite painful to stretch your skin and your muscles at the same time when this massive scar is healing.
As they’re slowly inflating these balloons with saline, I start to see what’s happening and start to see them look real. I’m still wearing loose tops and tops that zip up because I don’t have full mobility of my chest, but I was starting to feel normal again.
They were hard massaging my scars, which I couldn’t even believe. There are also certain oils you can apply. I even had a laser procedure done to reduce some of the scars. I ended up with this really beautiful chest—just without nipples.

I had to have another surgery, which was supposed to be easy but there’s no such thing as easy in this journey. They had to take out the temporary balloons and put in a permanent implant. They also did a fat graft by taking fat out of my belly and putting it around the implant so they looked natural. I walked out of the second surgery looking like someone attacked my breasts and my abs. Liposuction was so painful. I couldn’t even breathe. It’s not easy, but it was so worth it.
I wear the exact same bathing suit that I wore pre-surgery. I wear the exact same tight dresses. But here’s the kicker: I don’t have to wear a bra. My implants don’t move so I get to wear backless dresses with nothing. I get to wear fancy dresses that I wore before and not have that feeling at the end of the night when my bra is too tight and I can’t wait to take it off. They look great. I can wear a bikini and you would never know.
The biggest reason I’m so excited about this is because I have no fear. I have no fear of reoccurrence. The mental game that I had to go through to get here was hard. You heard about the physical pain. The procedures were challenging, but my mind is cancer-free and that is the most beautiful thing. I don’t worry about reocurrence. I can’t get breast cancer. I don’t have to get mammograms. I don’t worry about it and that to me is the greatest gift.
Between a lumpectomy and mastectomy, I’m confident in saying a double mastectomy.
I did get mental health therapy at the request of my breast plastic surgeon. He said, “You look great, but I’ve been around the block. I encourage you to get some therapy.” I’m a proud person and said I didn’t need it. I needed it. I absolutely needed it.
In the beginning, I had a fear of relapse. My therapist and I talked through some ways and some strategies to get around that. My body is cancer-free, my mind is cancer-free, and that is the greatest choice I made.
If I had had a lumpectomy, I’d be subject to continual mammograms and we all know that those are anxiety-inducing. I’d be subject to hormone therapy. I’d be on high watch. It would not be worth it.
A lot of people who are newly diagnosed reach out and ask what they should do between a lumpectomy and mastectomy, and I’m confident in saying a double mastectomy.


Lumpectomy vs. Mastectomy
A lumpectomy is a minimally invasive surgery where they take out the area that has the cancer and the surrounding tissue. It’s “easier,” although I’ve heard lumpectomies are still not easy.
A lumpectomy can be done outpatient, but depending on the diagnosis, there is typically some follow-up. For quite some time, you have to come in every day to have it taken care of.
With mastectomy, they remove the entire breast. Depending on whether or not that cancer has spread outside the breast, there could be chemotherapy as well.
You might need to have radiation to make sure they got everything and radiation can be painful. There’s also hormone therapy, which involves taking some drugs to make sure that some of your hormones are not feeding the cancer.
It was unclear whether or not I was going to get sensation back in my breasts and to be able to feel the pain of the needles of a tattoo was relieving.
Getting a Nipple Tattoo
I read an article about a tattoo artist who specialized in nipple tattoos. It was a beautiful article about how much compassion he had for breast cancer survivors so that’s where he dedicated his career.
I originally wasn’t going to see him because I’d have to fly across the country. It seemed to be a big hurdle and I was going to have it done at my plastic surgeon’s office where a nurse practitioner said she could do it. I kept hemming and hawing about it and I realized that I wasn’t ready for the journey to end because the last step of the entire journey was the nipple tattoo. I decided to get some mental health therapy first because I didn’t think the journey was over for me mentally.
On the day of my appointment, I canceled with the nurse practitioner. When I talked to my therapist, she said, “It sounds like this is a big thing for you. Tell me more about it.” I told her I had the dream about getting this fancy tattoo artist to do it for me. She said, “Well, then you go do that,” and so I did. It was the celebratory closure for me.


I drove up there and there was no fanfare. I was alone going to a tattoo parlor in a strip mall outside of Baltimore. I’ve never had a tattoo. I was afraid of needles and pain but here I am, about to get a tattoo, which was quite ironic.
Part of reconstructive surgery is that you lose sensation. I couldn’t feel my breasts. As I was sitting with the tattoo artist, he said, “You probably won’t feel a lot of this because you’re still in the reconstructive phase and your nerves are still healing.” Sure enough, it was painful. It was unclear whether or not I was going to get sensation back in my breasts and to be able to feel the pain of the needles of a tattoo was relieving.
The tattoo artist approached the process quite clinically. He looked at my breasts and said, “Okay, I think I’m going to do this. I think I’m going to do this.” He didn’t ask my opinion. He just asked, “You want 3D? You want it to look real?” I said, “Yes, I do,” and he went to town. Twenty minutes later, I put my shirt back on and it was over. It was truly over then.
My mission to support other women and caregivers because of the many gifts that I have been given by other cancer patients.
Life’s Mission
Cancer changed my life. I lead an organization that helps kids with cancer and their families, but that journey started when I was right out of college and didn’t have a lot of purpose. I didn’t love my first job and volunteered at a sleep-away summer camp for kids with cancer. I took a week off of work and would be the mom to these kids, whether they were seven-year-olds or teenagers. Those were some of the most life-changing experiences I have ever had.
When I was diagnosed, I realized it’s what I’m supposed to be doing. Not only is it my career now, but it is my mission to support other women and caregivers because of the many gifts that I have been given by other cancer patients.
I spent a lot of time with my mom in the hospital where I met other cancer patients. While cancer is a club you never want to join, once you’re in, there are some silver linings, like the people you meet and the life perspective that you get, and those are true gifts.


Words of Advice
Trust the process and trust yourself. No one better than yourself knows what’s right for you. While I recommend having a mastectomy or someone may have said something, ultimately, trust yourself and trust the process. That will get you through.

Inspired by Erica's story?
Share your story, too!
More DCIS Breast Cancer Stories
Nicole F., DCIS, Stage 1
Symptom: Appearance of a lump in the right breast
Treatments: Surgery (lumpectomy), chemotherapy, cold caps, radiation therapy, hormone therapy (tamoxifen)
Erica C., DCIS, Stage 0
Symptoms: Indeterminate calcifications found on a routine mammogram
Treatment: Double mastectomy
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
Alison R., Partially Differentiated DCIS, Stage 4 Metastatic
Symptom: Lump in underarm/breast
Treatments: Chemotherapy, surgery, radiation, targeted therapy


