Margaret’s Stage 2 IDC & DCIS Breast Cancer Story
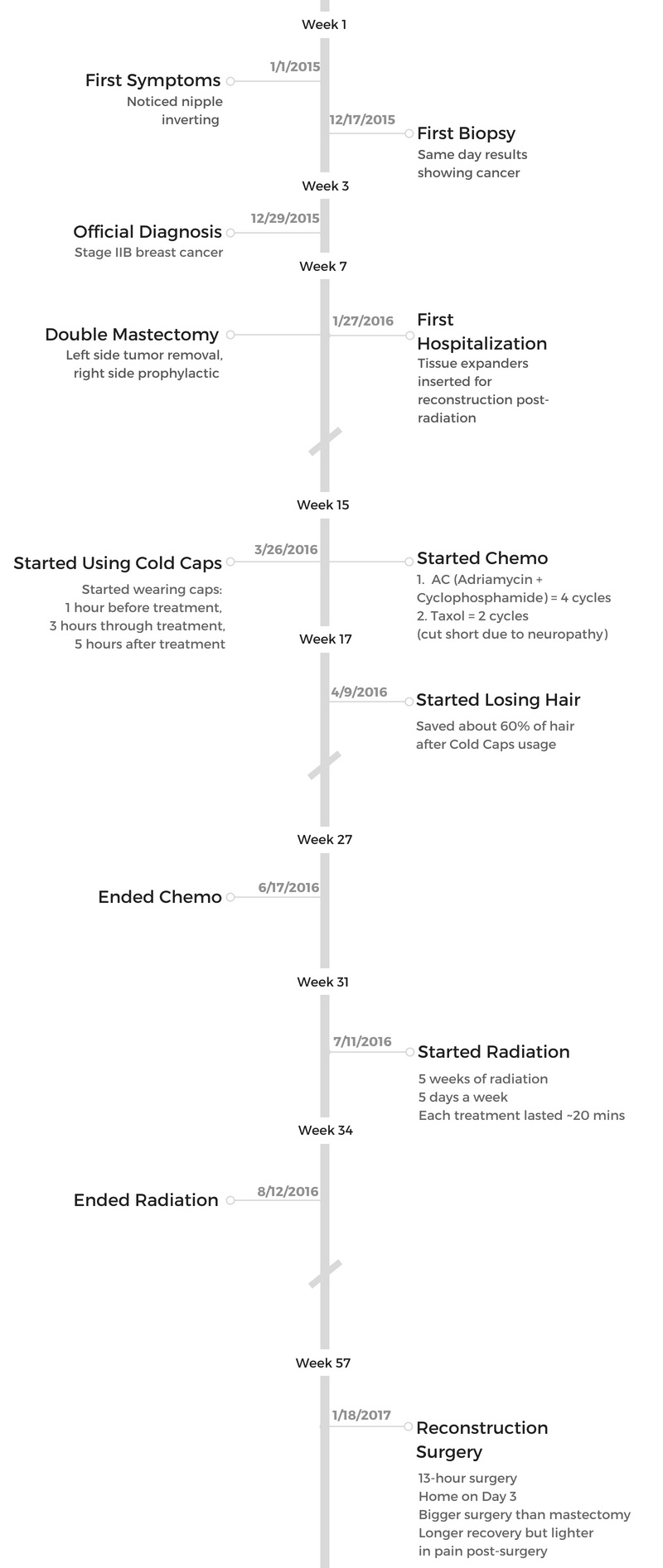
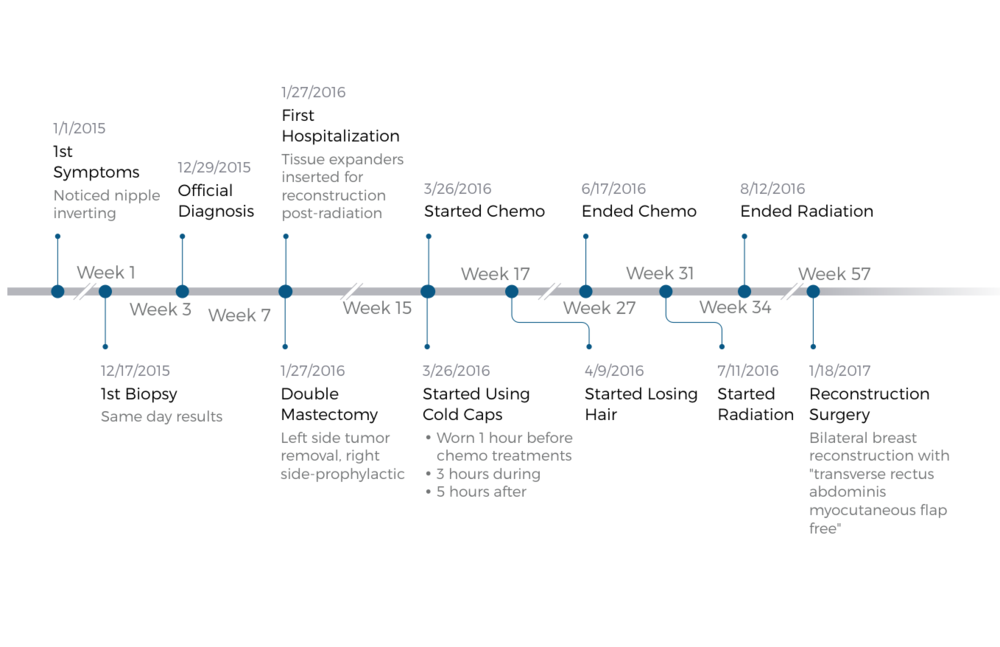
Margaret shares her stage 2 breast cancer story, both IDC and DCIS, after experiencing pain in her left breast and noticing an inverted nipple. She describes going through treatment, including a double mastectomy, chemotherapy, and radiation.
In her story, Margaret also highlights managing hair loss, using cold caps, using integrative medicine, and guidance for other patients dealing with cancer.

- Name: Margaret A.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- Ductal carcinoma in situ (DCIS)
- There were 2 tumors that merged into a bigger one.
- There may have been Paget’s disease involved.
- Staging: 2
- 1st Symptoms:
- Pain in left breast
- Left nipple inverting
- Treatment:
- Double mastectomy: removing all breast tissue
- Chemotherapy: AC-T for 6 weeks
- AC (Adriamycin & cyclophosphamide): 4 weeks
- T (Taxol): 2 weeks (cut 2 weeks early)
- Radiation
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
For those of you who may have just received the same news I received, with a lot of questions and a lot of emotions, I just want to say that there is the other side.
I made through it. A lot of others have.
Margaret A.
Diagnosis & Surgery
How did you get diagnosed?
I didn’t feel much at all. I did feel a little pain, but it was really just a physical change that really kind of made me wonder what was going on. I went in for the mammogram, and they brought me right back the next day for the biopsy.
Describe when the doctor broke the news of cancer
They had me wait. Within a half hour, I was called in to see the doctor. He was the one who told me. That was probably the worst experience I had.
It was very cold and non-emotional, just, “Here you are, this is what you have, and you can go talk to the oncologist more.”
It was shocking because it was the first time I was told, and it came from someone who was just not very emotional or compassionate.
I came home just not really knowing what this all meant, and that fear of the unknown was very scary.
Then my primary care doctor [was] calling me and explaining what it was further. But she actually painted a very rosy picture and said, “Oh, you know, you’ll just get treatment, and you should be done in 3 months. By spring break, you’ll be able to travel with your kids.” So that was the impression I was under.
Learning the recovery timeline
When I actually went to see the surgeon, the oncology surgeon I saw first, she explained to me exactly what was going on and what needed to be done. I realized I may not be done by spring break.
She scheduled me for surgery for January to do the double mastectomy, so I did that. I was home within a day and a half.
That was also rather shocking how they send you home so quickly. I appreciate that it did happen quickly, so within a month, I was ready to go in for my mastectomy. I did that in late January.
Surgeries and Decisions
How did you decide between a lumpectomy and mastectomy?
The many questions and many decisions you have to make, and you’re also going in to get the scans and so forth. I had a scan done, and they saw a little speck on the right side. They didn’t know what it was, so I had the choice of doing just the left.
Then I was in between stage 2, so originally they said I could do a lumpectomy. The location was right behind my nipple, so I had to lose my nipple anyway.
Then the question was, ‘Do you want a lumpectomy or a full mastectomy? Do you want one, or do you want to do a prophylactic on the right?’
Having to go through all those decisions was hard for me. Then the whole genetic testing thing came in, so it was just a lot being rapid-fire.
Everything comes very quickly right at you, and it was hard to sort through all that. I did feel very overwhelmed at times.
I think the difference is just how much tissue they take out. For a lumpectomy, they go into where the tumor is, and they take some amount around it. It’s much easier in that sense.
The mastectomy, they go in and take all the tissue out of your breast. I chose to do both.
Why did you choose a double mastectomy?
The right side would have to be continued to be monitored, and the monitoring itself would be challenging. You’d have to go into a CT scan.
I’m somewhat claustrophobic, so being in there for 20 minutes was really hard. Having to do that over and over did not sound like fun, so I thought, “Let’s just do it then.”
Then [the] plastic surgeon also comes in. They’re kind of tandem. He had explained that it would be easier to do reconstruction and be more symmetrical if I did both. That was another reason I chose to do that.
Describe the mastectomy process
It was a surgery. I went in at 5 a.m. to get prepped — general anesthesia. You’re under the whole time. They put you to sleep, but I just remember I was really scared. I was just really, really scared of what this was going to be like and the pain I would feel afterwards.
Then there was also a question of what would I lose in terms of reconstruction. I knew I was going to lose my left nipple, but I wasn’t sure if I could save my right nipple or not. There was some back and forth before the surgery.
Turns out I was able to save my right nipple. You go in, there’s a whole team there, and they prep you. You get the line in for the anesthesia. They put you to sleep, so I don’t really know what happened. It was in the morning we went in. I came out about 6 or 7 p.m.
I remember waking up and just suddenly feeling excruciating pain. They pumped up the drugs to alleviate that. Then I stayed overnight, and they were monitoring me pretty frequently. They would give me pain medication, but it was very restrictive in that it had to be every 4 hours.
By the end, around 3.5 hours in, the pain would start coming, but the nurse wouldn’t give me the pain medicine until I hit 4 hours. That last 30 minutes was just awful.
Then the next morning came around, and the doctor came by. I had both the oncology surgeon who took out the tissue, and then right in there with her is the plastic surgeon who put in the tissue expanders. It happens altogether. They came in the morning, checked me out, and said I was fine to go.
I remember being scared and not ready to go home. I asked them to let me stay a little longer. They said I would heal better at home, so they were really urging me. It really hurt.
I didn’t feel confident that I could take care of myself, even with my husband helping me, so just was really scared to go home. Once I got home, I realized it is a lot easier to recover because you don’t have a lot of the other distractions going on.
The mastectomy was the hardest part of this whole treatment. Even reconstruction was actually a bigger surgery but actually easier to do.
Choosing reconstructive surgery
After the mastectomy, I was flat. I did have options, and I could’ve chosen not to do reconstruction. It was about, for me, looking and feeling complete. I just didn’t feel that. I felt like there was something that I lost, and so for me I just wanted to gain it back.
I actually wasn’t able to do reconstruction until I finished all of my treatment, so it was the chemo and then radiation. Then a while after that, I had to wait. It was a full year until I was able to go in to do the reconstructive surgery.
They put in tissue expanders before the surgery
They’re like these plastic cups that are flat, and they insert them into your chest area into the cavities. Gradually, they expand like balloons [and] put fluid into them. Each time was 100 cc, so [it depends] on how big you want to be.
I think I had to go to 650 or 700 cc, so every 2 to 3 weeks I’d go in and have these expansions. When they did the first fluid insertion, it just hurts because you have very tight tissue, and you’re trying to loosen it up. That was pretty painful.
They cut under, they take out your breast tissue, [and] they insert these plastic-y balloons inside under your muscle. Then they have a metal piece, and the nurse would use a magnetic detector. There’s a little port, hole in there, and she’d find it with the magnetic detector, insert the line in, and pump the fluid in.
There’s 1 on each side. Of course, I chose to do the more complicated reconstructive surgery. The option is to do implants, so they’re silicon implants, or what I chose to do was called the flap. They take tissue from my stomach and use that to build up my breast.
What was the reconstructive surgery like?
It was a 13-hour surgery. I went in around 7 a.m., and I came out about the same time. It was 3 days in the hospital. You’ve lost skin. It’s tissue, so you’re crunched over because you can’t actually stand up straight.
The first day or 2, I couldn’t get out of bed. The first night, they want to make sure the vessels reattach, so they put this warm inflatable heating pad over you. You have to sleep with that all night.
The nurses come in to check with ultrasound every half hour or so to make sure all the vessels are attaching. It was a major surgery. I was told 6 to 8 weeks to recover.
I got home day 3, and we had to try to figure out sleep and how to get in and out of bed. It was really hard to move with this huge cut. We had rented one of those recliners at first, but it was so uncomfortable to sleep there, so I just slept in bed.
Whenever I had to get up, my husband had to help me get out of the bed because just the movements were extremely painful. The pain meds were good, so thank goodness for them. It was a much bigger surgery, I’d say, than the mastectomy even.
It took longer to heal, but the pain after was much less. It probably was the pain medication. Maybe it was also because it was inserting instead of taking out. Although it was a longer recovery process, it was lighter in terms of pain.
Why did you choose flap surgery over implants?
They were saying with the silicon it would have been a 2- to 3-week recovery. I just philosophically have an issue with any kind of foreign things in my body so I try not to take pain meds or aspirin if I don’t have to, so I think it might have been psychological.
I just knew I couldn’t do the silicon because I knew it wasn’t me. I just needed to feel complete and be assured that it was all me. Everybody’s different, and I totally respect everybody’s decision on this, but that was just my choice.
Unfortunately, one of the other issues is my other friend didn’t do this, although she had the option. When I asked her why, it’s because she’s a very slender, slim person, and she just didn’t have enough tissue [in her stomach area].
Even my plastic surgeon had said, “Don’t try to lose too much weight.” You need to keep the tissue to be able to have enough to build the breast sizes that I wanted. I got to eat more [and] eat whatever I wanted to eat. That was nice!
Chemotherapy and Side Effects
How did you decide to pursue chemo?
There was an issue of whether my tumor, which was a slow-growing tumor, if chemo would be effective with it. My oncologist [and I] went back and forth. She did an onco-typing test, so they delved even deeper into the type of tumor it is.
They have these charts, and if you’re from 1 to 20, you’re very unlikely. There’s mid-range and high-range. I was number 18, and so I was on the borderline of whether chemo would be effective or not.
She just recommended that I do that. I think that was originally why my primary care doctor thought I’d be done by spring break. She didn’t think I’d have to go through the full treatment.
That’s something that I think that may be different from what I’ve talked to my friends about. Depending on where you go for your care, their diagnosis, their suggestion, [and] treatment suggestions are different.
I went to Stanford, and my own analysis is that they pretty much want you to go through everything. They want to make sure all the i’s are dotted and t’s are crossed. It’s just to be double sure, extra sure, [that] they will recommend you go through the full treatment.
What chemo did you undergo?
The chemo I underwent was AC-T.
What were the chemo side effects?
They’d start me with anti-nausea medications. That would be for about a half hour or so. Then an hour later, they’d start the AC (Adriamycin, cyclophosphamide) which wasn’t very long, maybe 2 hours.
I didn’t really feel a whole lot during the treatment. The AC was actually fine. Most people actually say that’s the harder one, and I did not feel many side effects. I really think I was lucky that the AC didn’t hit me that hard.
It’s just this feeling of fuzziness in your head that you have and the queasiness in the stomach. That and then some fatigue, so just not feeling like I really wanted to get out of bed and do much was how I felt.
But the Taxol really affected me. That one was the one that was supposed to be easier according to all of my friends and what I read on the online chats. I threw up, and I think it was when I started the Taxol.
Within a day or 2 after the treatment day, I just started feeling this pain, mostly in my knees, in my joints, and in my feet. I couldn’t stand up out of bed. I had to hold onto things to walk, and it was this excruciating pain.
I remember just being in bed and trying to take pain meds. I was on oxycodone, which was the best for me, but that wouldn’t take the pain away. I got really bad neuropathy. I remember after the first round, I couldn’t stand up. I just curled up in a ball just in pain.
I called my oncologist, went in, and talked with her about it. She suggested reducing the dose, so we tried again at 25% less dosage. It was a little better, but not good enough for me to be able to go about my daily routine.
After the second round, I went back, and the doctor had said the chemo is minimal in terms of effectiveness. The type of tumor I had was really receptive to the hormone therapy that I would get later, so the few percentage points I might gain from the chemo wasn’t worth the risk of the long-term nerve damage.
We decided to end it after 2 rounds.
»MORE: Cancer patients share their treatment side effects

How did you do at home after chemo?
The first couple of days, I remember feeling pretty good. I would even go work out to keep up my exercise during treatments. But then during day 2 or 3, [I had a] little bit of nausea.
They give you anti-nausea medications that I took. I remember just mostly being in bed those 2 days. I was also working part-time during this time, so I timed it. I was able to time it, so I’d have the 5 days they say you won’t feel well off, and then I’d go into work on day 6 or 7.
The second week, you feel pretty good, pretty back to normal. Then you start again. It was usually about 5 days where I felt stomach queasiness. I remember not feeling like eating much.
The only thing I really enjoyed eating was potatoes at the time, so I ate a lot of potatoes, which probably didn’t help. I heard during chemo you lose weight, and that was the one thing I was looking forward to. It didn’t happen. I think I might have even gained weight.
Just feeling a little bit of nausea during that time and fatigue, of course.
I just remember at my work there’s a staircase to get to the office, and just during the chemo treatment barely being able to walk those last few steps. That was actually my way of measuring how things changed. As I was recovering, I could tell it was getting better because those stairs were getting easier to climb.
More: Working during cancer treatment →
How was radiation after chemo?
I went into radiation, which was 5 weeks, every day for 20 to 30 minutes. That started a couple weeks later in July, and I finished my last round on August 12th.
Hair Loss After Chemotherapy
Describe the hair loss
Then just facing the possibility that I might have to go out in public with some bald spots. I guess through that process, I realized how tied in your look is to your confidence, unfortunately, but that’s the reality of it. People do judge you to a certain extent by the way you look.
You feel better about yourself when you look better, for most people. It was definitely that for me. That was a revelation to realize how important my hair was.
»MORE: Dealing with hair loss during cancer treatment
Processing the hair loss
I didn’t realize how important my hair was until the idea of losing it all was in front of me. I really didn’t think it was going to be a big deal, but it was.
Part of it for me, too, was that I really felt I needed to be quiet about my condition as I was thinking of running for elected office again. As a woman having been in elected office, I’ve experienced the double standards, the stereotypes, and I knew that if I revealed what was going on, there would be folks who’d try to use that against me.
That was part of my thought process. I wasn’t hiding it. I definitely told my close friends, but I didn’t want to publicize it.
I remember during the second week, after the first round of chemo, just losing a clump of it. I was supposed to go out to a concert, actually, and just about to lose it. I was like, ‘What am I going to do? How am I going to cover this?’
You used cold caps. What are they?
I had learned somewhere along the way about these frozen caps that you can rent out and wear during chemo treatments. It’s supposed to save your hair.
I looked into these Penguin Cold Caps, and you get these liquid and plastic-y velcro bowl caps. The night before, my husband would go to the grocery store [and] get 80 pounds of dry ice. You get 8 of these caps, put them in the ice, and freeze them overnight down to -48 degrees.
You wear the caps before treatment, during treatment, and after treatment. You have to change them out every 30 minutes to keep it at that temperature.
My husband came with me to the treatments, and he would be working. We had the timer going. He would have to try and thaw it out a bit to soften it up so it would wrap around my head completely. It would be about 8 or 9 hours that I would wear these caps.
Actually, the hardest part of my chemo treatment was the cold caps. By the end, by the last cap, I was just wiped out. It’s like a brain freeze that entire time and a headache. That was probably the most painful part. With the AC [chemo] I’d come home, [and] I’d have the caps on for another 4 or 5 hours.
Did the cold caps save your hair?
I did lose some hair. I saved about 60%.
Would you recommend the cold caps?
I definitely would recommend it as an option to look into. I know things have advanced a lot since even I did them. There was very little information. There was basically 1 company in the country at that time that had these cold caps.
They are expensive, about $1,500 to rent. It is quite an effort, so you definitely need to have someone to come in, support you, and do the changing every 30 minutes.
They have to knead it, so it’s a lot of work. It is pretty excruciating. [In] the beginning, it’s just cold. Then your brain gets numb, so you don’t really feel it. But that numbness [turned into a headache].
It is hard, but in hindsight, I’m glad I did it. I saved some of my hair, and I think my hair has grown out more quickly than others because I had some hair that was saved.
I think it really is a personal decision based on how important it is, frankly if you have the support to help you get through it, and just how much pain [and] coldness you can handle. You just have to weigh all that.
I think it’s worth looking at. I have recommended it to my friends to at least try it out. You can try it for a couple sessions and decide it’s just too much or not.
If the cost isn’t too inhibitive, I’d recommend it. Insurance didn’t cover it for me, so that’s another thing to consider. I’ve heard some hospitals — I think Stanford, too — is supporting it. When I did it, we had to bring in these coolers with ice caps in them, roll them in, and roll them out.
They have these little machines that I guess keep them cool. You can plug them in. I know UCSF had that when I was doing it, and Stanford, I heard, just started supporting it. At least they’re making it easier for you, so definitely worth looking into.
Life Outside Treatment
How was the medical staff?
I really felt like you get to know them, and they get to know you. It was from the parking valet to the nurses to all the staff there that check in people. The doctors really get to know you, so I felt they really cared.
I remember when I finished radiation just feeling kind of sad that I wasn’t going to see these people anymore, and it was an interesting feeling.
They just became a part of my life, and it was a little bit of sadness and a hole in me because these folks that were so integral to my life for so long, for that amount of time, weren’t going to be around.
That was probably the most positive surprising experience or feeling I got from all of this.
You also used integrative medicine
They suggested integrative medicine. Stanford has an integrative medicine department, so I started that. That did help, and I still go now. It’s been a real positive source of treatment throughout the cancer treatments. Now I think it’s helpful for my daily health.
Neuropathy is something that can last for a long time, and it comes and goes. Even after I started the Taxol, I had it. My fingers and my toes would tingle.
That’s when I went to acupuncture, and over time it got better. Even now I go. Sometimes when I’m tired, I feel a little bit of tingling, but it has definitely subsided over time. There was instant relief from the pain when I went, so I thought, “Yeah, this is a good thing.”
Just from my past, I did a martial art. The whole idea of Qi and the flow of energy and what acupuncture does to help with that flow really makes sense to me. I definitely embrace that Eastern medicine philosophy.
I think it’s great we have both Eastern and Western medicine coming together.
What was the biggest surprise?
Everything was.
It was obviously new, and there was definitely this unknown factor. Just not knowing is something is hard for me. I like to have my life planned out.
There are so many variables, and so I couldn’t plan out my year’s treatment. From the very beginning, when my primary doctor said, “You’ll be done in March or April,” then having to actually go through more like 13 months to be complete was probably the biggest surprise. Just the fact that it took a long time and way longer than I expected.
What got you through the tougher times?
I have 2 daughters — they’re 16 and 13 — and I realized I needed to still be there for them. There was no question for me. It was like, “I have to get through this.”
‘I can’t leave my husband with the girls. They’re not ready to not have a mom, and I’m not ready to leave them.’ That’s what kept me going, and that’s how I tried to stay focused on that.
There are those go back-and-forth, up-and-down roller coasters, but that was my target or my focus. That’s what kept me going through all this.
You just have to believe. You have to have faith and believe that you’re going to get through it. The odds are so high — the numbers out there for recovery and for being cured — that it was very assuring. That’s what I tried to focus on to get through the whole process.

What’s your advice to others in your shoes?
I think it’s very helpful to have a support network. It’s amazing that one of the biggest discoveries was once I started sharing it, it seemed like everybody I talked to either knew somebody or had gone through it themselves.
There’s a lot of information online. I was told, “Don’t read it,” but for someone like me, I needed to know what to expect.
But there’s so many different experiences. Everybody goes through it in their own way, so I think it’s helpful to get a range of what some of the symptoms might be or the side effects and whatnot.
I think it was helpful to know what was possible, but also know that I wasn’t going to track exactly like anybody else. As long as I wasn’t a super outlier of what I read was possible, it was reassuring to me.
I was very fortunate to have a friend who’d gone through almost the same exact experience, including the cold caps, a couple years prior. She really guided me through this process.
I hope that there are folks like that for everybody who might go through this, but this website is also a way, I hope, for folks like us who’ve gone through it to share and try to make it at least be able to share the information so folks know what to expect. For me, that gave me more assurance.
Having that relationship with your doctor is very important. Being assertive and asking all the questions you need to ask is really, really important.
I know there are times when you might feel the doctor’s busy and they’re trying to get you in and out, but be sure to really advocate for yourself and get the questions you have answered. You’ll have more peace of mind.
Mental and emotional health
I really believe that your mental [and] spiritual state affects your physical state. Once the doctor told me I would be cured, that switched my attitude. I think that has helped me to get through this process more smoothly than if it hadn’t been that way. I think peace of mind is really, really important.
Try to stay positive. I’m amazed and grateful that medicine is advancing so much, and I really now believe there is a cure for most cancers. That’s something positive to look towards.
Also, let yourself feel the emotions you’re going to feel through this, because it is a journey. It’s hard to describe, frankly, until you get through it.
I had no idea. I didn’t know anything about cancer before this. It is hard to describe to others, but I hope I do my best to be able to describe it, share it, and make it a little easier for someone else.

Inspired by Margaret's story?
Share your story, too!
Combination Type Stories
Symptom: Sunken in nipple of right breast
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Symptom: Lump in right breast
Treatments: Lumpectomy, double subcutaneous mastectomy, hormone therapy (tamoxifen)
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
LaShae R., IDC & DCIS, Stage 2B, ER+
Symptoms: Lump in breast, pain
Treatments: Chemotherapy (Taxotere and cyclophosphamide), proton radiation
Dee D., Metastatic Breast Cancer, IDC & DCIS, ER+
Symptoms: Inability to produce milk on the left breast while breastfeeding, breast pain (palpable and radiating to the back), lumps in the breast and armpit
Treatments: Chemotherapy (AC-T), surgery (bilateral mastectomy & axillary lymph node clearance), radiotherapy, hormone therapy (Zoladex/goserelin), aromatase inhibitor (letrozole), targeted therapy (Kisqali/ribociclib)
Cat L., IDC & DCIS, Stage 2B, ER+
Symptom: Pain in left breast radiating from lump
Treatments: Bilateral mastectomy, chemotherapy, hormone therapy (tamoxifen)





