Margo’s Plasmacytoid Bladder Cancer Story

Margo never expected to develop bladder cancer, let alone two versions at the same time.
When Margo noticed something was off, she visited her OB/GYN, then a urologist and urologist oncologist. If she hadn’t advocated for herself, she would not have gone to MD Anderson and discovered a second diagnosis of plasmacytoid, a rare and often deadly form of bladder cancer.
Margo underwent intense chemotherapy and a radical cystectomy to save her life. Margo shares her story of dealing with loss and isolation during treatment, finding humor and the sliver linings in life, and writing a book about her incredible journey.
- Name: Margo W.
- 1st Symptoms:
- Blood in urine
- Diagnosis (DX):
- Stage 1 bladder cancer
- Plasmacytoid
- Tests for DX:
- Cystoscopy
- TURBT
- Treatment:
- Chemotherapy
- Methotrexate, vinblastine, doxorubicin and cisplatin
- Radical cystectomy
- Chemotherapy
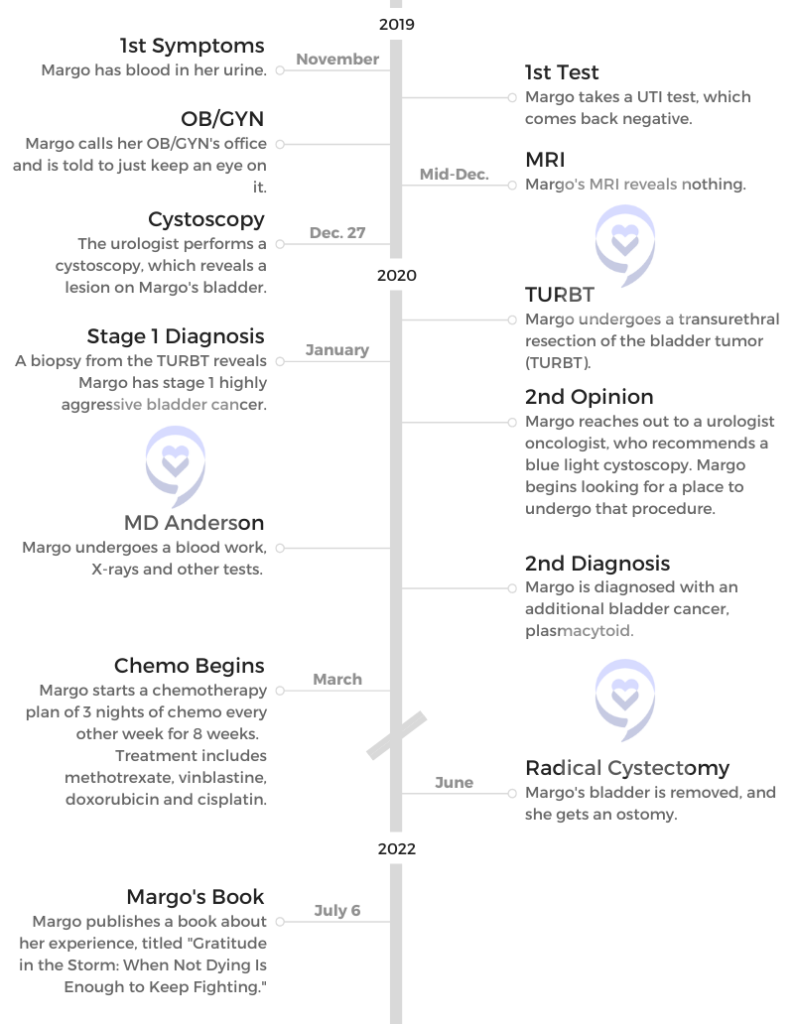
- 1st Symptoms and Self-Advocacy
- Introduction
- Cystoscopy and TURBT
- In mid-December, you find a urologist. What happened at the appointment?
- Did you know you were going to have a cystoscopy before the appointment?
- What was the cystoscopy like?
- Did you have localized anesthesia or a painkiller?
- Results of the cystoscopy
- Transurethral resection of the bladder tumor (TURBT)
- Managing scanxiety while waiting for results
- How did you find out the results?
- How were you feeling?
- Breaking the News to Loved Ones
- Getting a Second Opinion
- Second Diagnosis
- Treatment
- Chemotherapy
- What was the plan going forward?
- The chemo plan was methotrexate, vinblastine, doxorubicin and cisplatin. What were the major side effects, and what helped with them?
- What was it about that moment in particular where you felt this eruption of all this emotion?
- Giving yourself grace to grieve
- Undergoing chemo during the pandemic
- How were you able to manage the extra isolation?
- Radical Cystectomy
- Undergoing a radical cystectomy (removal of the bladder) for 7-8 hours
- Finding the silver linings
- What were your options after the radical cystectomy?
- Anxiety surrounding the neobladder
- What guidance do you have for someone getting a radical cystectomy?
- Changing perspective
- Talking to others who have been through it
- Hair Loss
- Reflections
- Normalizing the conversation about sexual health effects
- Physical effects of treatment
- Emotional effects of treatment
- What other losses did you experience around this time?
- Losing your mom
- Taking time to celebrate remission
- Experiencing more loss
- Getting through so much loss
- You filmed a video as Wonder Woman. What did that mean to you?
- Margo’s book “Gratitude in the Storm: When Not Dying Is Enough to Keep Fighting"
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Symptoms and Self-Advocacy
Introduction
Tell us about yourself
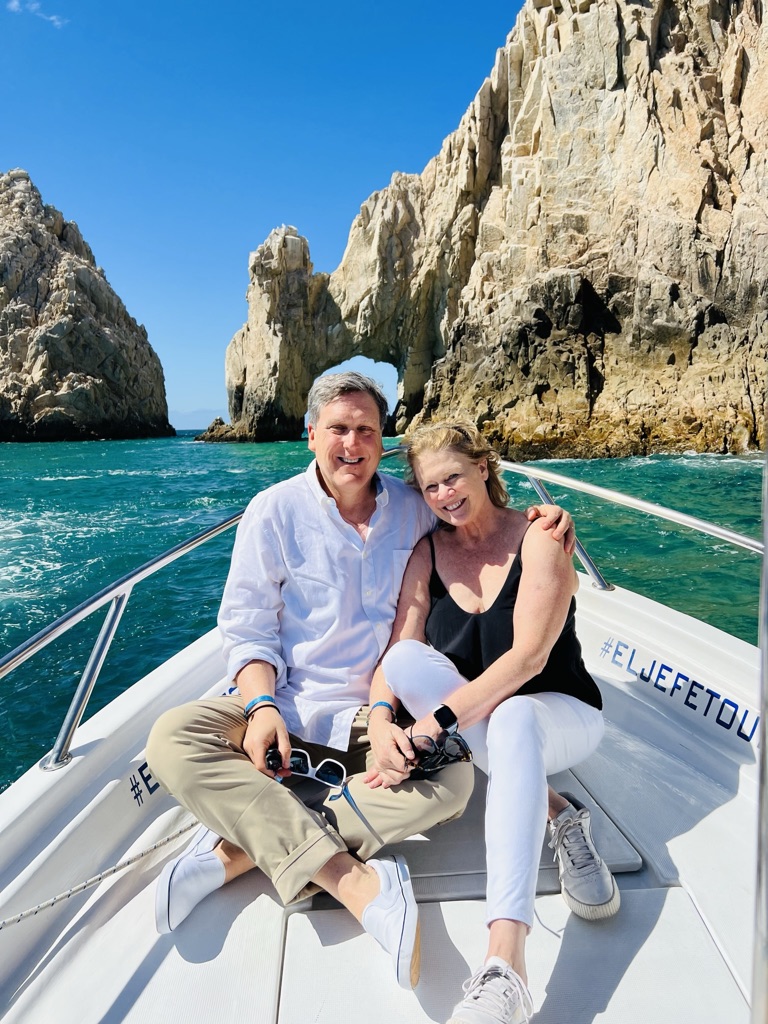
I am a seize-the-day, make-the-most-of-life, passion-for-life kind of a gal, and I pretty much always have been. For example, we go on family dive trips. I got my children certified to dive when they were 13, the earliest age that you could do it. We like to travel. We love our dogs. We love spending time together. I’m married to a great guy and I consider myself very fortunate.
You noticed something wasn’t right in November 2019. What happened?
I think one of the things that is very common for cancer patients is that we don’t feel anything. Nothing’s up. We don’t have any pain symptoms or discomfort or anything like that. It was the same for me, except for that one day late in November, I noticed that my urine was the color of rosé, like a deep rosé.

I thought, “Well, that’s not right.” I’m old enough that menstruation could not have anything to do with it, but women are often kind of swept under the rug when it comes to things like that. At any rate, it stopped. The afternoon was clear. Then the next morning, it happened again. A little bit of blood in the urine. Then I never had it again. That’s the only symptom I had.
I consulted Dr. Google, which is both a good and a bad thing. I immediately went to a lab and did a UTI test. Now you can get them over the counter, which is awesome. I was on extra alert and a little concerned.
I have developed over the years a way of saying to myself, “I don’t have that information. If it is worst-case scenario, I will have plenty of time to stress and worry and fret over it. If it’s not worst-case scenario, why put myself through that in the meantime?” I tried very hard to hang on to that. The lab called and said, “Great news, it’s not a UTI.” I was like, “No, that is not great news. UTI would be so much better.”

OB-GYN appointment
I called the OB-GYN. I treat her very much like my GP. A lot of us do, I think, especially if your GP retires, and you’re like, “Yeah, she knows me. We had babies together.” I called the nurses there, got a hold of one of them, and I told her what had happened. She said, “Well, let’s just keep an eye on it.”
I thought to myself, “Nope, I’m not doing that, because nothing good happens from waiting.” What’s the worst thing that happens if I go right away to a urologist and find out that it is nothing? I don’t know what it could have been that was nothing, but it might have been.
What am I? I’m not a doctor, so I don’t know. That information can only help me. Waiting cannot at all help me. That would absolutely make things worse, especially given that it was actually something nefarious.
I immediately started looking for a urologist, and for one that I could get in to see pretty quickly. It was 2 weeks out, so I made the appointment with the urologist, who had a good reputation.
How did you research and make decisions?
First, I call my friends. I say, “Do we have a urologist in the stable of providers?” We do the same thing with shoes. “I need silver platform shoes for a dance. Does anybody have one?” Nobody had a urologist. I did do some research and looked for health grades and a couple other things like that, and I did what I could for due diligence. He had a good reputation, and everybody seemed to love him.
Cystoscopy and TURBT
In mid-December, you find a urologist. What happened at the appointment?
I don’t know the outcome, and I’m doing the discovery. I’m getting the answers. It’s very scary. We could very easily go to DEFCON 5. What good is that going to do? I can’t operate at my best abilities to make decisions and continue self-care and advocating for myself if I’m just freaked out.
I kept doing that, but it’s beginning to take more effort at this point. But I did that, and we went in. That was early mid-December. A little nervous, not too bad. Went in, did the cystoscopy, and I actually could see it. You could look over on the monitor and see this little soft cauliflower wafting. It looks kind of pretty.
Did you know you were going to have a cystoscopy before the appointment?
Actually, I just collapsed 2 appointments together. I went into the first appointment with the urologist. He said, “Yes, we should do some looking around. Go get an MRI, and let’s meet back here for an appointment.” The MRI had showed nothing.

I actually tried to cancel the cystoscopy because I was like, “Since there’s nothing on the MRI, I guess we can go ahead and say that it’s all fine.” They were like, “Sometimes it doesn’t show everything.” Then we ended up with a cystoscopy. That was after Christmas. That was actually a day before my birthday, on the 27th.
What was the cystoscopy like?
What I will tell you is that men complain about this a lot more than women do. It’s a little more complicated. There’s more acreage that has to be covered with a man, but they’re basically slipping a tiny tube with a camera through your urethra to head on into the bladder and have a look-see around. That’s being shown on a screen. It might have an easier term than that, but that’s what’s happening.
Did you have localized anesthesia or a painkiller?
They said it’s not necessary. I said, “Well, maybe for you. Can I please have a Xanax at least? Or I’m going to have 2 margaritas before I come in here. Either one.” They gave me a Xanax.
Your urethra is one of the several areas that is designed to be a one-way street. It is not comfortable. It was worth the discussion. If you’re a doctor and you’re doing 20 of these a day or something, it’s nothing to you, but it’s not nothing to the patients.
Results of the cystoscopy
[The doctor] said, “Oh, yeah, that’s a lesion.” That was his less scary word for a tumor. I learned that that’s what he meant when I had coffee with a good friend of mine who shares the same birthday as me the next day. I said, “Oh, I’m not really worried about it because he said it was just a lesion.”
She said, “Yeah, that’s a nice word for a tumor.” She’s a doctor. I thought, and then I said, “Yeah, but at that point, I’m still feeling pretty positive because it could be a tumor. It could still be benign. Those happen as well.” The next step was to schedule the transurethral resection of the bladder tumor.
Transurethral resection of the bladder tumor (TURBT)
They again go in through the urethra and use whatever tools that they use to remove tumors. I imagine there’s cutting things involved. Then they send that off for biopsy to find out what’s going on with it.
Managing scanxiety while waiting for results
I focused on that I still had my kids at home and family to enjoy and everything else I could think of. I also had work, so I just focused on everything else that I could think of. Again, I’m flexing that muscle more and more and strengthening it to be able to put it off and say, “I’ll wait till I have more information before I freak out or get concerned.” I also discontinued Googling all this stuff at that point, which is what I advise.
»MORE: Patients describe dealing with scanxiety and waiting for results
How did you find out the results?
6 days later, I still had a catheter, which is just no fun. You’re carrying a bag around. 6 days later, I was in the office. They remove the catheter, and they go, “Okay, so you have stage 1 highly aggressive bladder cancer.” That’s staggering.
I thought I had a contract with cancer. I will do the lifestyle things over here, and you leave me alone. I thought that I had made that arrangement. Cancer didn’t sign that contract, so it was void.
Then he drew a crude picture, just like a basic picture of, “Here’s a bladder; here’s the ureters.” He said, “Here’s what’s going on. Stage 1 means it’s only in the bladder. It hasn’t crept through to some of the other layers — 2, 3, 4 and so on. The good news about that is that we can treat this with BCG.” I don’t remember what that stands for, but it’s related to what they use to treat tuberculosis.
Immunotherapy in this case would be inconvenient, not very pleasant. Again, it’s going through the urethra to deliver immunotherapy to the bladder. At this point, I’m just thinking, “Ugh, okay, so now I’ve got to do this every 6 weeks. Then I’ve got to have another cystoscopy, so I’ve got to do this for the next 2 years.” I’m making peace with that. That’s what’s happening in that doctor visit.

How were you feeling?
I think this is probably the case for a lot of us. You’re thinking, “This cannot be. This doesn’t make any sense to me. Nothing about this makes sense to me. This couldn’t be more out of the blue.” Zero kind of cancer runs in my family. Lots of other stuff, but just not that.
Smokers are associated with many kinds of cancer, and actually, bladder cancer is one of the things. So I’m like, “It’s not that.” Because in the meantime, I had done research on causes, trying to understand how we got here? I gave up sodas. I eat clean. I drink a lot of water. I exercise. I do all those things.
I thought I had a contract with cancer. I will do the lifestyle things over here, and you leave me alone. I thought that I had made that arrangement. Cancer didn’t sign that contract, so it was void, and you just never know. I’m told by doctors that sometimes you can figure it out, and sometimes you can’t. Sometimes it’s just random, which is 100% unsatisfying.
All of that’s going on in your head at one time. How did this happen? How can this be true? Come on, universe, higher being. I have enough character. I feel like now I am hogging the character. Somebody else wants to have a shot at going through something difficult. I’d been through a lot already in life. That’s what I thought. Really, another thing that’s really hard? All of that was going on through my head at the time, and it’s frightening.
»MORE: Patients share how they processed a cancer diagnosis

Breaking the News to Loved Ones
How did you break the news to the rest of the family?
My hubby was with me the whole time for all of that, which was really great. His name is Coleman, and he’s unbelievable. I think that caregivers have a whole different set of needs than patients. They go through all of it with us, just not the physical part of it. They can’t lean on us as patients to be there for them, so they definitely need to have resources and support.
It was wonderful that he was able to be that support for me. With me, I could squeeze his hand as tight as I needed to, and he could handle that. Then we just looked at each other like, “Okay, well, we’re going to get through this somehow, some way. We don’t need to know all of the ways and the details and what comes. We don’t need to know all those things. We just know we’re going to get through this.”
Talking to your kids about cancer
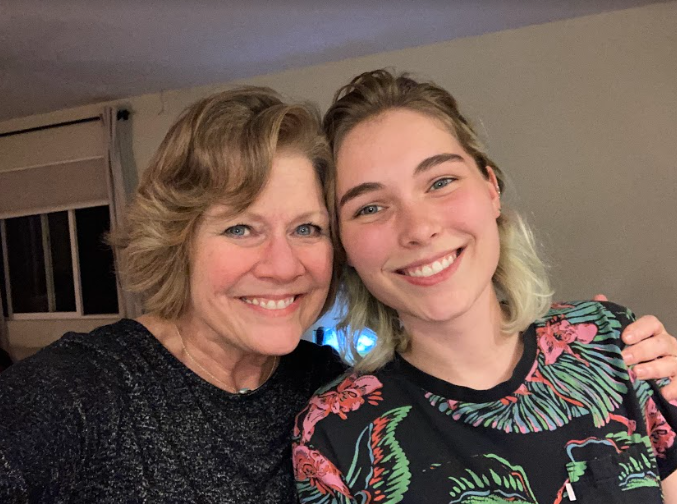
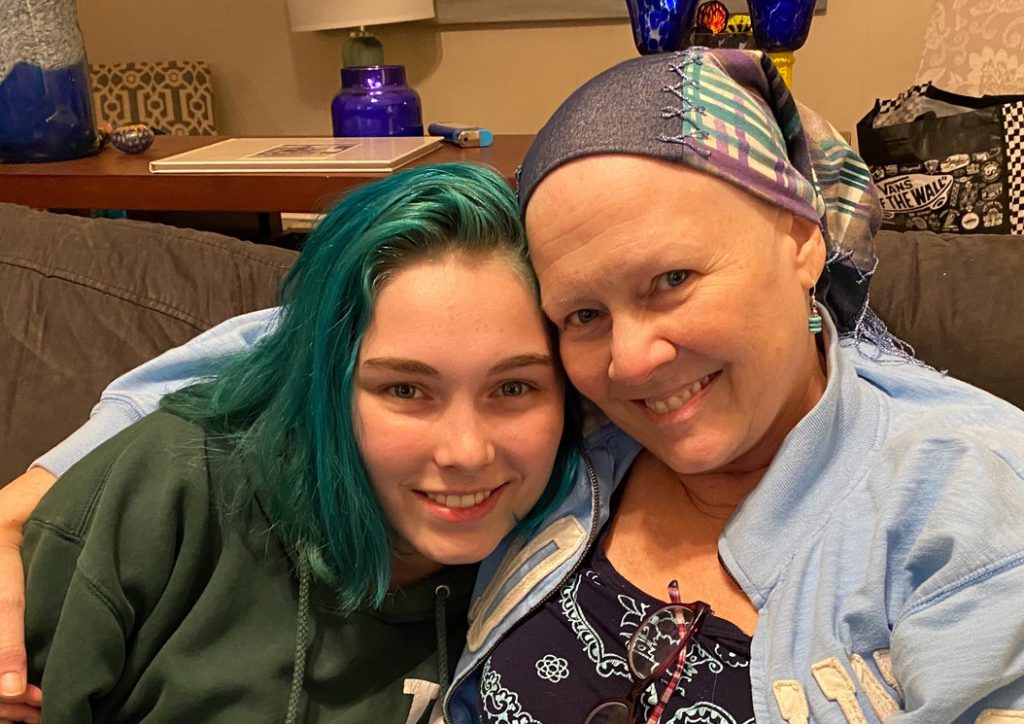
My kids at this point are 19 and 21. They’re adults. One’s in town. One is not in town. This is not news you like to break over the phone to people.
Part of what made this hard for me telling my kids is that I’m their only living parent. When they were in middle school, their father died. I was not married to him at the time, but he died. There wasn’t a reason that he should have died, but he did. He basically died from alcoholism. He drank himself to death.


That was a terrible experience for me to have to come home and tell them that their father had died. Not only was I thinking I don’t want to worry them because I am their only parent. Even though they’re 19 and 21, they still need parents and family. That was the biggest concern I had. How do I make sure that I explain this to them in a way that doesn’t feel as scary and life-threatening and doesn’t freak them out?
I don’t want to mince words either. I don’t want to mislead them. I don’t want to sugarcoat it. Kind of choosing the right way to communicate with each of them. Now, at this point, that’s all I know about my cancer. I’m still thinking it’s garden variety, essentially, and this is going to be really inconvenient. That’s what I understood at that point.

Is there anything you learned in terms of guidance for other people on how to navigate that?
Yes, there is. I learned that the best way to do this, at least for me and definitely for them, is to go right to it and to say, “Reed, we just got home from the doctor, and it does turn out that this is cancer. It is stage 1, and here’s what we’re going to do about it.”
Right to the point. Don’t go heavy into details. In this case, I just said, “Here’s the therapy.” They’re grown, so they can understand it, but that’s not the point of the conversation. Then follow it up right away with, “And we’re going to get through this.”
Getting a Second Opinion
Why did you get a second opinion?
Actually, it’s my job. I sell health insurance policies for self-employed people, like realtors. I had learned a lot about what most policies do and don’t include. Second opinion is really, really important. I’d learned that the data shows the number of misdiagnoses is really high. I didn’t know how high. For cancer, it’s actually 70%. That’s what my oncologist told me.
I said, “How many of the cases you see are wrong, or it’s an incomplete diagnosis?” They all said 70% in separate appointments. I knew to take advantage of a second opinion service, which I did. The second opinion service was an oncologist urologist.
Back up for a second. I went to see a urologist. At this point, what do I know? Do I know that there’s a urologist oncologist in the world? I know nothing of this world. I don’t know that I should be seeing an oncologist urologist. Who tells you that? Not your urologist.
There’s a lot of this seeking information, gathering it real time while you’re experiencing it, trying to process it, trying to hold it together and figuring out what’s the best path forward. It, as you know, is a mind-numbing experience. It’s a soul-numbing experience.
Without this experience, you may not have known to ask for a second opinion
I may not have. I’d kind of like to think I would, but I can’t say for a fact that I would. You don’t know what you don’t know. If you are aware and then you choose to not get that information, that’s on you. But if you don’t even know, it’s tough to say, “Oh, I should have gone and done that.” I’m really glad I did go get that second opinion from a specialist, who was a urologist oncologist.
Seeing the urologist oncologist
He said, “About 20 or 30% of the time” — this was his number — “stage 1 bladder cancer is actually stage 2 bladder cancer. Completely different treatment regimen. I want you to go get a blue light cystoscopy.”
I thought, “Oh, that sounds almost fun.” The blue light picks up on cancer cells that aren’t visible to the naked eye. Okay, that sounds like a good thing to do. I hung up the phone. Actually, it was a virtual visit.
Then I called my urologist office, and he said, “Oh, I don’t have the equipment to do that. It’s a good test. I believe in it, and one day we’ll all use it. But right now, nobody in Austin does it.”
Going to MD Anderson
I did my own research. I live in Austin, Texas. MD Anderson is right down the road in Houston, 3 hours away. I’m aware of them and their reputation, and I thought, “Well, I’m stage 1, garden variety bladder cancer. I don’t need to go to MD Anderson.” Why did I think that? I have no idea. That’s kind of the bias that you have — it’s not that serious. I so wanted to cling to that.

At any rate, when the second MD recommended the blue light, I couldn’t find one here. I had to start doing research, and I found that there were 3 places nearby. One was San Antonio, and 2 were in Houston. What I did — and I think this is really smart — is always ask the people who know more than you do and ideally who know the most of any one thing.
What did I do? I sent those names to the urologist oncologist, who was the specialist in my second opinion. I said, “What do you think of these?” He goes, “I can vouch for these 2 cases. I’m just saying, don’t go to the one in San Antonio.” He didn’t vouch for that one.

Then I basically figured out how you open up records and let hospitals see your records and start the process. You don’t know how any of that works, and so you’re figuring that out as you go. How do you get an appointment? I went through the process of getting the documents in my records and everything to them.
Within days, appointments started showing up on my calendar. MD Anderson — you’re going to have a blood test; you’re going to have all these different things. I thought, “Okay, I guess I’m going to MD Anderson.” They’re one of the best. They’re rated the top all the time. I felt confident about that and good that I’d found one that was highly [recommended]. I was, at this point, still hopeful that this was just mainly super inconvenient and uncomfortable.
Seeing Dr. Ashish Kamat
He’s a superhero. He’s amazing. I had an occasion to see him at a bladder cancer event recently, where I was one of the 3 patients that shared their stories. We just hugged. I had sent him the first chapter of my book and said, “I don’t know if you feel like saying anything.”
The second kind is lethal. It is very rare, it’s fatal, and it always comes back. We have to do everything. If we do everything, we throw the kitchen sink at it, we can save your life.
Dr. Ashish Kamat
I didn’t know if he was going to read this email or not. He replied back through one of his assistants. “Here’s what I think.” He said these glowing, wonderful things. 2 years to the month later, he told me in person at this event, “I want the whole book, and I want it signed by you.” Okay, I’ll do that for you.
Second Diagnosis
Receiving an additional diagnosis
[Seeing him] would save my life. I did a bunch of breathing exercises while we sat in the room waiting for him to come in. I’d done blood work and X-rays and things, but I’m still thinking that he’s going to go, “Yep, we need to do immunotherapy.” But I also know there’s a chance that it could be something else.
It takes forever. There’s so much waiting. The good news about all that waiting is not that you’re waiting with your thoughts to yourself, but it is that when it’s your turn, they’re there for you. I used all of my best coping skills to get through the [waiting]. It felt like an hour. It probably was 30 minutes. Breathing in and out, and just trying to stay calm.
When he came in and talked to us, he got right to the point. He said, “We’re not going to do a blue light cystoscopy tomorrow, or at all. Because looking at your slides, at the images from your biopsy, you have not 1, but 2 forms of cancer in your bladder.”

I’m thinking, “Yet another thing I had no idea was possible.” What’s the limit? How many is the most you can have in one place? 2? He said, “The first kind that you already know about will respond to BCG. The second kind is lethal. It is very rare, it’s fatal, and it always comes back. We have to do everything. If we do everything, we throw the kitchen sink at it, we can save your life.”
Processing the plasmacytoid diagnosis
That is the hardest thing I’ve ever had to hear. You don’t even know how to react when that’s what you hear. Save my life? I’m fine. Look at me. I’m healthy. I don’t feel anything.
He went on to explain that this second form is a plasmacytoid, and it does sinister things like cloak itself and make itself look like bladder cells to the other bladder cells. That’s very sneaky. That is one of the reasons it’s so hard to treat.
Throwing the kitchen sink at it in this case was 4 kinds of chemo every other week for 8 weeks, followed by a radical cystectomy. That is the removal of the bladder and usually some other things along the way.

What were you feeling?
It was indescribable. It felt like my throat, my stomach, all just dropped. I thought, “I’m going to black out.” I really thought I was going to just pass out. My husband’s with me, thank goodness, and so I held his hand. He listened for both of us, which is great because in some ways, I did black out.
No one knows us like we do. I think it’s really important to listen to our instincts, to listen to our gut.
Margo W.
I was conscious, but I don’t recall the conversation after that. My husband will say, “Remember when he said blah, blah, blah, and you said yada, yada, yada?” And I’m like, “No, I don’t. I don’t remember that.” I don’t. I remember the part I just shared with you, and really nothing after that.
It’s impossible [to process in the moment]. I agree with using the phone to record. I found that later on that was very useful, and they were always really open to it. You can’t necessarily process everything. You’re like, “I’m sitting up, right? I’m looking at you. Not on the floor, so that’s good. That’s all I got. That’s all I can deliver right now.”
The importance of self-advocacy and getting additional opinions
As individuals who need to have access to health care, the best thing we can do is advocate for ourselves all along the way. That doesn’t mean yelling and screaming and saying, “Get somebody in here.”
I think we almost have a passive acceptance and total trust of anybody in a white coat. Doctors are amazing, and I have huge respect for them and nurses and everybody who does all that work. But they don’t know each of us individually, and no one knows us like we do. I think it’s really important to listen to our instincts, to listen to our gut.
I joked it was my spidey sense. [It] was like, “Oh, this doesn’t feel right.” Listening to that and then just keep getting information. Don’t accept no answers when you can get answers. Then always go to the very best that you can get your hands on, because they’ve seen the most cases.
»MORE: How to be a self-advocate as a patient
Seeing a specialist
Dr. Kamat asked me, “Who were you seeing in Austin?” Austin has almost 2 million people. It’s not a little podunk town. This doctor had a good reputation, but when I said his name, he goes, “I don’t know him.” I thought, “Well, that’s bad, if you haven’t heard of him.” I don’t know how big the world of urologists is, but he wasn’t a urologist oncologist. He doesn’t see as many cases as they do.
You want that. You want literal volume. Let’s take a look at what the Austin doctor and Austin pathologist had versus MD Anderson doctors and MD Anderson pathologists. They had the same images, same exact data. It was really important to get the best eyes on it. They already knew before I got there what the diagnosis was and what they were going to need to tell me.

They knew that because they see so many more. This is so rare. It’s like 1%, 2% of bladder cancer patients, but they see 4 or 5 of them a month. Which is just so many, relatively speaking, and there are very few survivors of plasmacytoid. They don’t often get to save their lives, because it’s also asymptomatic.
Sneaky, asymptomatic, and 100% fatal and recurring. If you don’t know you have it, by the time you do, you typically don’t have much time left. I can thank the first kind for giving me the flowy tumor that there was to see to take me to the doctor, and then thank of myself for continuing to advocate and go to the best doctors I could find.

Don’t worry about hurting doctors’ feelings
Don’t rest if there’s something I’m thinking needs to be addressed or seen. That’s just so important for all of us. We can advocate for ourselves without offending doctors. This is something I want to mention. I feel like it’s really common that we don’t want to hurt their feelings. Some people will say, “Well, shame on you for worrying about hurting their feelings.”
Well, maybe you don’t care about other people’s feelings, but I do. This is a real thing for a lot of people. I did take into account my doctor’s feelings. I did feel like I was being disloyal to get a second opinion. It didn’t change my behavior. It didn’t change that I did go get that second opinion, and in fact, saved my life. But it is a real thing that people go through.
Let me shine a light on that and say that’s pretty common. You can feel a little bit like you’re being disloyal to your doctor, and they’re going to have their feelings hurt or be offended. Just acknowledge you might feel that way if you have to go get the second opinion, and that’s okay. Do it anyway.
Many doctors say, “It’s your prerogative, and you go do what’s best for you.”
That’s actually what my doctor said. It was a good thing. I would have done it anyway. That just would have been more uncomfortable. Probably most of them will say that. It’s important to not have an expectation that we’re not going to feel that.
We’re thinking, “I’ve got a diagnosis.” The next thing needs to be to get a second, maybe a third opinion. If you feel this reticence or concern about how you’re going to leave the doctor feeling, that’s okay. Do it anyway.
Treatment
Chemotherapy
What was the plan going forward?
The plan going forward was to start radical chemo. It was 4 kinds of chemo. It required a 3-night stay in the hospital to have all of that chemo. I didn’t get a port. Sometimes that’s what you get, but I had a PICC line instead. I don’t know why. It was fine. It doesn’t matter. That’s the least of the concerns.
It’s like going to college when you go to a place like MD Anderson. You have all these classes. You don’t know where they are or where this lab is. Where is that [department]? Okay, go get a CT scan there. But I could go get it there, too. You just have to pay attention and ask for help along the way.
That meant checking in the following week to MD Anderson on, I think, the 12th of March. My husband could come with me for that. Anyway, we knew that I would have 3 nights of chemo every other week for 8 weeks, followed by a 6-week break, and then a radical mastectomy in June.
The chemo plan was methotrexate, vinblastine, doxorubicin and cisplatin. What were the major side effects, and what helped with them?
They are so great at handing you resources. I got a book this thick with what to expect when you’re having chemo. You read through it, and you go, “What, my fingernails could fall out? My hair is absolutely going to fall out, and there’s nothing we can do?”
I’m a gal who has always had long hair, and I associated with me and part of my femininity — right, wrong or indifferent. Having it just taken away all of a sudden… Most of us don’t welcome that. When I see teenage girls shaving their heads for no reason, I’m like, “Don’t do it.”
At any rate, it was so overwhelming to read all those potential side effects. I couldn’t really handle it. Most of that didn’t sink in. I remember sitting there with the oncologist March 2nd, that day that we got the news that this was big and bad, and we had to do everything. Another oncologist said we need to do [methotrexate, vinblastine, doxorubicin and cisplatin].

It’s a common MVAC, I think, for bladder cancer. It’s different. She’s telling me all these things. Tears are rolling down my face. I couldn’t process it, yet you can’t say, “Hold on a minute. I need to go collect myself.” This is what they do. They need to see patients.
Fortunately, I had my husband with me for that appointment. We just got through. We got through learning about what the chemo was going to do. I didn’t really know what I was in for.
What was it about that moment in particular where you felt this eruption of all this emotion?
Wow, that’s a great question. I don’t know if I can answer it. My immediate response was that was just the icing on the cake. To hear her talking about the chemo treatment and the hair loss, and maybe the fingernails are going to fall out. Just the stream of all these things, because that’s when we dug into what the treatment was going to look like.
Self-care isn’t selfish.
Margo W.
Dr. Kamat laid out the strategy. Now we’re into the tacticals of what it’s going to look like. I compartmentalize pretty well, and that’s handy. I know that it’s really important to not compartmentalize so much that you don’t deal with stuff. Part of it was that.
Some of it s because I’ve been compartmentalizing, and now the greatest fear was in fact what was happening. Then the gates unloaded. If it is really terrible news, I will have time to grieve and be angry and sort through it and process it. That’s what I started doing right then and there.
Giving yourself grace to grieve
I don’t want it to seem like I was able to actively make that choice. By that time, I was just so overwhelmed I could no longer keep it at bay. Self-care is not something we heard about until, for me, like the last 5 years. It was selfish and indulgent if I did hear about it.
Self-care isn’t selfish. Listening to our instincts, listening to what our needs are — whether they are medical, whether they are emotional, all of the needs — is really important. Allowing ourselves to process all this stuff is really key. It’s going to look the way it’s going to look.
I think one thing we know, a lot of us know anyway, is that grief is very personal. It looks different for everybody. Because it looked like this for me doesn’t mean that’s going to be somebody else’s path, even if they have the same exact diagnosis. Whatever the path is is fine. There’s zero judgment on what it should or shouldn’t look like. We need no more “shoulds.”

Undergoing chemo during the pandemic
The first chemo treatment was in early March. That’s the last time anybody could come into the hospital with me, because we were in full quarantine after that. Every day, the nurses and providers were wearing more stuff, more masks, more plastic, all of that. It was just changing.
I don’t know if anybody remembers. It’s hard to go back to that. The president was talking about it, and they were trying to figure it out. That was the last time he came into the hospital with me. Every single other time — there were 3 other rounds of chemo for 3 nights, and then the surgery — he had to drop me at the door and leave.

That’s really not fun at all, because when you have the 4 kinds of chemo, they get progressively more uncomfortable. The first one, you’re like, “That’s fine.” The second one, you’re like, “Oh, I have a headache.” Then you start feeling just like living hell, and your face is puffy, and you look and feel terrible, and that’s hard.
You have to leave when it’s your turn to leave, even after that fourth round of chemo — which, by the way, they call the red devil, and they were wearing literal hazmat suits to handle it. I thought, “Okay, you’re wearing a hazmat suit to handle it, and then you’re dripping it right into my veins. This definitely feels like poisoning me within an inch of my life.” [That] is essentially what chemo is.
How were you able to manage the extra isolation?
I have a few things to be grateful for. First of all, my husband and I both were working remotely already, so there was no change there. Literally no change there. I had the love and support of my husband. I had the love and support of 2 amazing kids.
Then I had the love and support of my extended family, who were here to do what they could, like leaving food at the door. This is how we did it during quarantine. You couldn’t come in and heat it up. People would just take a whole cooler and drop it off.
I just would accept the help. Accepting the love and support from the people whose love and support I had was essential. We had dogs, and so lots of loving on the dogs. There would be a time after at least a week that I would start to feel like maybe I could take a little walk around the neighborhood. I would do that if at all possible, and try to do as many normal things as I could think of to do.
Radical Cystectomy
Undergoing a radical cystectomy (removal of the bladder) for 7-8 hours
Well, it is figure-changing. Again, an unwelcome result. Not happy about that. I’d already been concerned about my waistline, but it’s vanity weight. It’s 10 or 15 pounds that I’d rather not have. For health reasons, it wasn’t an issue.
Now, I knew that I was going to have a forever-changed body. I chose the ostomy bag solution. Think of an oblong, elliptical-shaped Ziploc stuck to your belly 100% of the time. That’s pretty much what you got going on. They’ve done some things to make it a little more comfortable. There’s little fabric; it’s not just plastic on your skin. But not fun.
Nobody wants to have this at all, although I will say — and here’s me doing my little humor thing. I will say that when I was hiking in the Appalachian Mountains with my family, I could tell [I] needed to empty the bag. I stood up like a guy in the woods. It was so cool. I was like, “This is great.” That’s the only good thing that came from it.

Finding the silver linings
Sometimes it’s so slim. It’s helpful, and looking for, “What do I have to be grateful for?” is a big part of how I have gotten through difficult times in the past. I called it the grateful game way back in the 90s, when I’d be like, “Okay, I feel like hell. I’m so depressed and frustrated. What can I think about that’s positive? What can I feel grateful for?”
That’s a baseline, the core framework for how I navigate through the tough times. Also core to how I do that is to embrace what’s actually happening. I don’t try to stuff it, pretend like it’s not happening or “should” it somehow.
What were your options after the radical cystectomy?
The options presented to me were I could have a neobladder, or I could have the ostomy, so that’s 2. When we were with Dr. Kamat in that first meeting and he explained those to me, I said, “What about a pig bladder? Come on, we’ve got lots of different organs we can borrow from animals. Surely those would work.”
He said, “No, those don’t work.” I said, “Okay, can you 3D print one?” Can we not use technology here? Of course, we’re not ready. We don’t have 3D printed full bladders, and maybe one day we will. Once I exhausted all the other ideas, I had to accept that these were my 2 options.
I said, “Well, tell me about the neobladder.” It’s pretty tempting to think of. Basically what they do is take a part of your intestine — I don’t recall which one — and they make a new bladder out of it, which is pretty fancy. It’s not shaped the right way, so it’s pretty creative.
It doesn’t have muscles, so you have to train it. But if it doesn’t have muscles, how do you train it? Leaking is a common problem. He said, “It can take a year to train it.” I thought, “Oof.” He seemed to think that the ostomy was the better path as well, so I took that.
Anxiety surrounding the neobladder
This is an embarrassing problem to deal with. Nobody wants to have issues with any kind of fluids or matter that our body gets rid of. We don’t want to deal with that. It’s inherently embarrassing, so adding to that embarrassment. It might be a year before you can get it to work.
Well, I can’t stay at home and not live my life. I have jobs and things to do. Those question marks definitely weighed in on that. When [the practical side of me is] deciding something big like that, the emotional side of me says, “Hey, I have an opinion about this.”
The [practical] side says, “That’s great. We’re going to hear about that later. That’s valid. We thank you for that, but we’re going to just make a practical decision here. We’ll talk about how you feel later.” It’s kind of how I ended up managing making that decision.
What guidance do you have for someone getting a radical cystectomy?
First of all, I think it’s personal. However other people are experiencing it is fine. I’m doing my path. You do you. I’ll do me. I think having conversations with other people who’ve gone through similar things.
For example, I know there’s women on Tik Tok who show off their ostomy bags, and good for them. I’m not going to do that. Do not look for me to do that on Tik Tok. It’s not happening. Good for them, and I like that they’re doing what they feel comfortable. Or maybe they’re pushing themselves, and they don’t feel comfortable.
It doesn’t have to look a certain way for any one of us. For me, I have what I call a love/hate relationship with my ostomy. I would like to be less disdainful. Last night, we were watching a show. I have very sensitive skin, and it’s got adhesive on it all the time. Sometimes it’s very raw, and it itches.
I can’t not have anything on it, because here’s what happens: what they do is take a little part of your intestine. They create a little conduit. They reroute the ureters to connect from your kidneys to this little tube instead of to the bladder. Then the tube just gets rid of the urine, and it goes straight into the back.
I can’t control that. I can’t just take it off for a while and walk around. You can’t. It’s not an option. I get very frustrated when that happens. I try to be kind to myself, and that’s how I feel. When I’m feeling up and good, I’m grateful.

Changing perspective
The night before the surgery, I had a lot of feelings. I looked at my body, and I thought, “I’m never going to look down and see this again. It’s going to look totally different.” That made me sad.
My brother said, “Well, think of it as getting rid of a body part that’s no longer serving you. This is your metamorphosis.” I thought, “Oh, that sounds a lot better than what I’m imagining, so I’ll go with that.”

Talking to others who have been through it
I think talking to people who’ve been through it [helps]. There are support groups on Facebook. The hospitals do a lot of things now. I couldn’t tap into any of the support because it was all shut down for quarantine, so I don’t know how good it is. I wasn’t able to use it.
Tap into all the things that are useful and have conversations with people. Some people you’ll connect with, and others you won’t. I wanted to talk to a woman who had been through what I’d been through. I was scared. I didn’t know what was going to be left. I didn’t know a lot of things. I talked to a woman who had had the radical cystectomy 10 years before.
I said, “Kind of a tough subject, but sexually, how were you after this thing?” She goes, “Well, I wasn’t interested in sex, and my partner wasn’t that excited about that.” I thought, “No, that is not what I want to hear.”
I’d been married to my husband for 5 whole years at that point. We’d just found each other finally, so I wasn’t ready to go to, “Octogenarian, we don’t have intimacy anymore.” I was not prepared for that. Fortunately, that doesn’t have to be the answer.
There may be some other things going on with her besides that, but that’s the problem with talking to people. Sometimes you hear things that upset you, or you think, “I don’t know if I can live with that.”
Just keep talking to other people, and keep going back to your doctors and asking them what’s physiologically going to be intact or not intact to understand. Allowing ourselves to be assertive and ask those questions, even if they’re a little uncomfortable, is well worth it. It’s our lives.
Hair Loss
Dealing with hair loss
I guess one of the things that’s good to know is what you can and can’t control. I couldn’t control that it was going to come out or when. By the way, it’s day 14, so that’s what I learned. That is when my hair follicles started hurting.
I likened it to when you have your hair in a bun or in a ponytail for a really long time, then you take it down. It’s like the follicles go, “Oh no!” Only it felt like that a lot of the time, and clumps are falling out, so it’s different. I felt nothing the first week, hair-wise. But on day 14, when we were checking back in, a whole bunch came out.
My daughter was at home. Her hair was, I think, purple at the time. [Knowing that it was going to come out,] I said, “Hey, let’s just make it whatever. What’s the wildest color? It’s all going away anyway, so let’s just go be wild.”

I have a professional job. I can’t have pink hair most days, but I thought, “Why not? Why not?” She dyed my hair bright pink. We had kind of fun doing it. It was a way for us to enjoy doing a little fun mother-daughter activity.
The reason that we were doing it wasn’t fun. I think there was a really therapeutic thing going on. [For me, it was] accepting her help, even if it’s just this light little color happening. For her, it was understanding what it’s like for me to go through this. She’s seen her mom always have long hair, and now all of a sudden, we’re going to have to cut it off, which we did days later.
She helped me with that. I said, “If it’s not too much for you, will you help me cut it all off and shave it down?” She said, “I’d be honored.” We went outside, put the iPhone up on the fence, and let it run. Fast-forward, because that’s a slow process. I still have a hard time watching that today because it’s just such a shift. We would love to say the hair doesn’t matter that much, but it does.
»MORE: Patients describe dealing with hair loss during cancer treatment
What comes up for you when you’re watching that video?
Part of who we are is how we look. We could comment on whether that should or shouldn’t be, maybe especially even more so for women. You see part of yourself that you expect to see and you define yourself as, “Okay, I am a tall woman with blonde hair that is long, and I can wear it in a braid or ponytail.”
Then you see that it is gone. Now I’ve got to figure out a new way to look at myself, but I feel like part of me and my sense of self. That’s a blow, even though I know intellectually it’s just hair. What does it matter? Everybody loves me. Who still loves me? Who’s important? Nothing about that has changed.
I get both how unimportant it seems, and yet I felt that it was very much a loss at the time. Also, I’m a woman in my 50s, and we’re doing everything we can to try to look as nice as we can and keep the gray and the wrinkles and all that at bay. A bald head is not a good way to do that.
It’s rough. I think it was the emotions of seeing that happening and seeing the hair coming off. It’s a very literal vision of me losing part of myself. I was able to learn down the road how to keep myself intact as a result. But at that moment, that’s not how I felt.

Your brother had the longest hair at one point
I never imagined this day would ever come. My brother’s always had super short hair. I laughingly refer to him as my baby brother. He’s 8 years younger than I am, but he’s a foot taller than I am. He’s 6’6″. He’s this huge guy, and he wears his hair short. After my hair was just starting to grow back a little bit, for some reason, my sister had super short hair at that time. His hair was actually longer than both his sisters’ hair. We thought that was a really funny thing.
Can you describe the importance of singling out these moments of humor?
I had to. That is part of my coping skill. I have gallows humor, because sometimes you’re in the freaking gallows, and that’s all you have to work with. A little bit of humor is a great way for me to help get through impossibly difficult times.
My mother, may her soul rest in peace, would say to me, “Sometimes you make a joke of everything.” And I’m like, “Hmm, well, sometimes I have to just to get through everything.” If you can find humor in any little thing, then I think it’s a very helpful way to get through, because then you’re like, “Well, at least 1% of that wasn’t terrible.”
Reflections
Normalizing the conversation about sexual health effects
It isn’t comfortable to talk about for me, and I do want to help normalize this conversation. One of the things that we talked about at the Bladder Cancer Advocacy Network Think Tank ‘22 was that this is one of those cancers that’s below the belt.
It’s a little bit embarrassing to talk about, a little personal and all that kind of stuff. That just makes it worse. That makes it harder if we feel like there’s shame involved with talking about the kind of cancer. I didn’t choose this. Nobody chooses this.
We’re all putting ourselves out there and pushing our comfort level to help bring that conversation along. I was on a panel with 2 other men, and what I can share with you is a woman’s perspective and a man’s perspective. There’s more cancer, more bladder cancer in men than women.
Both of them said that there was sexual dysfunction as a result of going through the treatment and also the surgery. One of them still had his bladder, and he said that that was the most important thing to him. I thought, “Yes, as it was to me.”
But if they say you’re going to die if you keep your bladder, then you take it out. That’s what happens. Specifically, they were able to get erections. They were able to have orgasms. There were a couple of other [things], but it wasn’t 100%. Everything wasn’t 100% the way they’d like it to be. That was interesting to hear.
Physical effects of treatment
When you’re removing the bladder, the urethra, the whole geography down there is pretty important. I don’t know where all the important bits and pieces and nerves are. I literally didn’t know whether I was going to be able to have fun or not. But everything’s still intact — the parts that matter are.
One of the things that goes along with a radical cystectomy is that often the way our bodies are shaped, they have to take some of the vagina. They didn’t in my case. That can mean that you now have a shortened vagina, and intercourse can be uncomfortable.
There are things that can be done to address that. Just go figure it out. There are all kinds of things. Go find out ways to do that and get the life you had back as much as you can. It just depends on your situation.
Emotional effects of treatment
I would say for me, it was more emotional than it was physiological. I didn’t like being bald, and I didn’t like having a bag on my front of my body. Now I’m no longer in shape either because I’ve been through all this stuff. I feel like I’ve been run over by dump trucks.
It’s hard to re-access the feelings of intimacy and the feelings of your sexual self. I think that’s been a longer journey than I would have liked. I think it’s personal. Again, grace. Give yourself self-grace. Part of me goes, “Well, there’s no time for that because now I’m 59 years old, and who knows how long I have? I just want to go ahead and hurry up and enjoy everything.”
I think that the whole accepting of where we are — which varies maybe day by day, hour by hour — is really key. Very clear and candid conversations with my husband have been good. That’s been enlightening. We’ve had to push the boundaries on what we’re comfortable talking about. That’s a good thing.
Ask the questions and understand what is and isn’t going to be in place, and what you might expect. Then I think what’s important is to look for what’s the highest and best potential outcome that I can have with this cancer, with what’s left of my body as a result of it, and what’s left of my life as a result of it. Then go make the very most that we can out of all of those things.

What other losses did you experience around this time?
I definitely had the, “I can’t take one single more thing,” because [I was] fighting this cancer alone in the hospital by myself. The week in the hospital after the surgery, tubes coming out of me all over the place, and people come in to poke and prod and all of that. The worst beds, the food’s terrible, the TV’s worse, and there’s nothing.
I had my phone, but it was really hard. I really did think, “Okay, well, that’s it,” but that wasn’t it. The blows kept coming. It was like it was bad writing. This is not all going to happen to one person in one year. But it did.
The next thing that happened that was a blow was the loss of my mother. I was sitting in the office by myself, waiting to see Dr. Kamat to find out if the chemo and the surgery had worked. This was 6 weeks after the surgery. I was waiting to see the doctor, so alone in the office by myself.
I looked down at my phone, which I had on silent but not turned all the way off. It was ringing, and it said St. Vincent’s Hospital in Jacksonville, Florida. It’s actually the hospital I was born in. I thought, “That’s not good. That’s either my sister or my mother.”
The doctor wasn’t there, so I answered the phone, which is not what you want to be doing when you’re waiting for the doctor to come in. First of all, it’s rude, and second of all, you need to be alert and paying attention. But I thought maybe it’s an emergency, and it was.



Losing your mom
It was St. Vincent’s saying, “Your mother is here. She is dying from dementia. She has a few days to live. She can’t stay here. Also, by the way, she tested positive for COVID. She doesn’t have any of the symptoms, but she can’t go to a regular hospice place, and she can’t go to her nursing home.”
So right now she’s homeless on a gurney, essentially, in the hospital, and I’ve got to deal with that right now. I couldn’t process that. I could not. I thought, “Really? Ridiculous.” I couldn’t process it, so I just was sort of stunned. I did my kind of compartmentalizing thing.
I got that phone call, and that meant I had a lot to deal with all of a sudden. I had to deal with the fact that my mother was dying in a few days, and that meant I would never see her again because we were in quarantine, and she had COVID. That was a lot to process.
I was her power of attorney, medical power. I forget what that’s called, but I was the one in charge. It was up to me to make those calls. I had the tactical thing of this list of really hard things I needed to do right then, which I couldn’t because I was waiting for the doctor to come in.
Taking time to celebrate remission
I reached for my husband’s hand to comfort me, but it wasn’t there because he wasn’t there, because we were still in lockdown. I was like, “Oh, that’s right. I’m by myself.” I had to just sit there and wait. The doctor finally did come in, and great news! You’re cancer-free.
Oh, my gosh. That is amazing news. Also, at the same exact time, my mother is dying, I can’t go see her, and I have to figure out where to even put her for the next few days. All at the same time. Insane breadth of different emotions and feelings all at one time. After we had the good news, I had the phone on the table [to record] so that I can share that with my husband.
When he picked me up, I said, “Let’s do this. We have a 3-hour drive ahead of us. We’re going to take 2 hours, the first 2 of 3 hours, and we’re going to celebrate that I’m cancer-free. We’re going to drive through Chick-Fil-A and get a milkshake and some French fries. Then the third hour, I will get on the phone, and I will start making calls and finding things out.”

That’s what we did. As we’re driving home and talking about celebrating that I’m cancer-free, we felt like we could finally exhale. For 6 months, we’ve been trying to save my life here. We didn’t know we were going to need to do that. Here we are doing that.
Now we’ve done that. What, it’s over? It’s over, more or less. We wanted to give ourselves time to celebrate. We gave ourselves 2 hours to celebrate. Of course, there were times besides that.
Experiencing more loss
Then I had to get on the phone and start finding special COVID hospice locations that I couldn’t go visit. None of us got to see her again alive, ever. The last time I saw her was the December before that August that she died, and that was impossibly hard. Then there was processing that grief and dealing with really tough things to manage logistically during the stupid lockdown.



Then a month later, the family dog died. This was the dog that raised my kids with me. She was 14 and a half, which is really old for a big dog. I feel like she made it through the death of my mom. I feel like she hung on to get me through. That was really hard, and then that wasn’t the last one.
Then my father-in-law died the following month, and we couldn’t go. My husband couldn’t go see him before either, so it had been January. We each had lost a parent after 8 months of not being able to see them, and we couldn’t see them before. We both had to do those absurd Zoom funerals, and you do the best you can.
Getting through so much loss
It felt like I just kept posting, “Here’s another dead person. Here’s another terrible thing,” on Facebook. One of my friends is like, “Dear God, what is happening?” I’m like, “I have no idea, but it just keeps coming.”
But here I am to live and tell about it. It turns out we can get through pretty much anything. I did tell myself at times, “Okay, you don’t live in a concentration camp, so it could actually always be worse.”
I’ll share something else for all the parents out there. If your kid had cancer, what parent wouldn’t say, “Give it to me; I’d rather have it”? It was me, and I was really grateful that it was me and not my kids.
They still have a life ahead of them, and I do too now, as a matter of fact. It could have been worse. It really could. I’m glad that it wasn’t them. I’m glad it was me and that I’m here to tell about it.
You filmed a video as Wonder Woman. What did that mean to you?
I realized when I was lying down in the bed at the hospital after this cystectomy. I felt just terrible. Pain and discomfort. Now we’re in the day and age where they don’t give you pain meds anymore. They’re like, “Here’s the Tylenol,” but [it] hardly helps. I know why we do it. I couldn’t have a Vicodin or anything, so I was uncomfortable.
I was tired, and I couldn’t sleep. I’m lonely; I’m depressed. I just thought, “You know what? For the first time in my life, I actually feel a little bit like giving up and feeling like I just could go to sleep, and then that would be it. Then all of this would stop.” That is so not like me, but it’s pretty brutal.
What I told myself in that moment was, “Well, you can’t do that. You can’t do that to your kids. You can’t do that to your husband and the other people who love you. Actually, all you have to do right now is not die. You don’t have to get up and fight or feel brave or energized. You don’t need to feel anything. You can feel like crap, which is how I felt. You can feel empowered. You can feel sorry for yourself. Feel whatever you feel. Not dying today is enough to keep fighting.”
Later, when I was reflecting back on that, I thought, “Yeah, you know, I think we have this perception that fighting, whether it’s cancer or another illness or another difficult chapter in life. Persevering has to look like this superhuman, like a Marvel character persona, who’s just big and strong and has all of the energy and the strength in the world to take on these battles.”
In fact, we don’t. It doesn’t have to look like that for it to be legitimate and enough. I have focused on that. I think that being able to laugh at the idea that we need to be Thor or somebody else in order to fight whatever battles that are ahead of us is — I think that is something we need to maybe leave behind us and accept a wider view of what courage looks like.
I feel like courage is not that you feel like fighting, that you feel like continuing to go on and do whatever the hard thing is that you’ve got to do. Courage is doing it anyway. Being brave is one thing, but having courage?
That’s when the rubber hits the road and you don’t feel like doing anything, and you grab yourself by the scruff of the neck. You get yourself up or crawl, whatever you have to do.
I just wanted to expand our view of what being brave and courageous and fighting can look like, and it can look like you’re lying in bed feeling like dying. Actually, that still counts. I still didn’t die. Good for me.
Margo’s book “Gratitude in the Storm: When Not Dying Is Enough to Keep Fighting“
It didn’t come to me right away. Again, I think I mentioned that I work for a company, and we sell health insurance plans for self-employed people. As part of my job, I present to groups and teams, both virtually — well, at that point, it was still virtually.
Here’s the overview of the plans. Here’s what you do if you want to access them. Here’s what one of the plans looks like when you need it. Here’s my story, and I shared. I’m on the plans that we sell. I shared my story, and I was really surprised by the response. It’s the only story I had, so at first I couldn’t, but then I did.
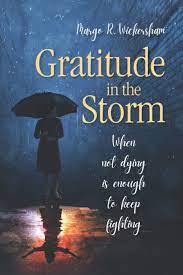
I thought, “Well, maybe this will help me process it, and maybe it will be helpful, because here’s a real person who’s actually needed to use it and what it looks like when you need to.”
I was really surprised by how emotional people felt as a result of hearing me tell this story. That really took me aback, and how caring and loving. To this day, 2 years later, I still tell the story, and they still respond in the same encouraging way, saying, “Thank you for sharing that with us. It’s inspiring.”
I thought, “If that is inspiring to the handfuls of people that I’m presenting to, maybe I could put it in a book and share it with even more people. That might be helpful for them as well.” My goal was to write a book that was easy to read and that would show people how I personally [got through it].
It’s just one way to get through all this stuff, but it has the little tips and tricks that I used to get myself through this really tough time. [My goal was to] give people hope that they can get through it, even when it looks like it’s insurmountable and impossible. Okay, feel that way. It feels that way. It does, and you can get through it. The book came out in July, and I couldn’t be happier.

Inspired by Margo's story?
Share your story, too!
