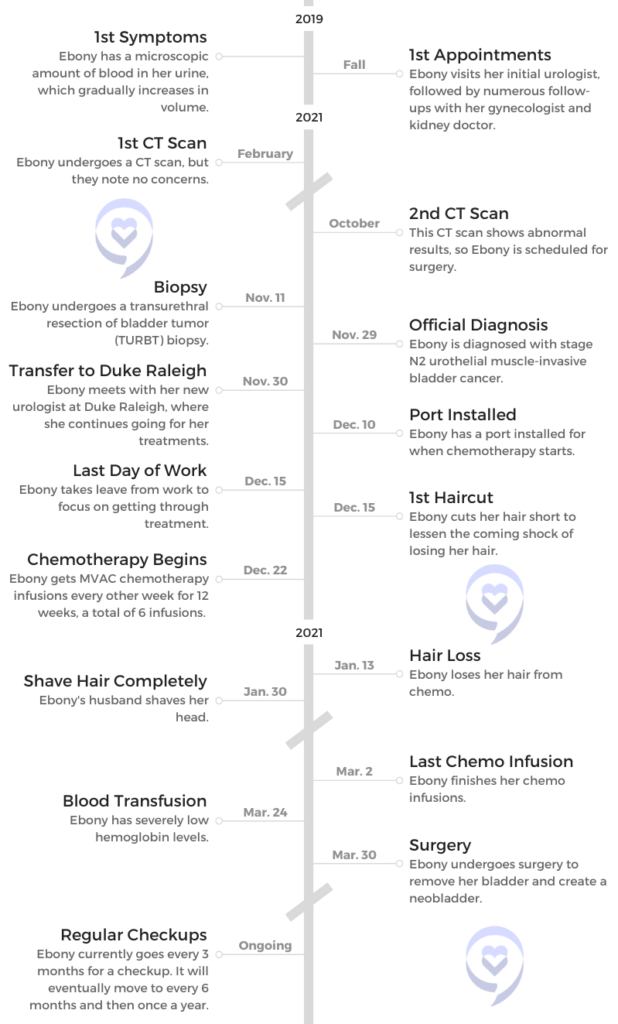
Ebony’s Stage N2 Muscle-Invasive Bladder Cancer Story

Ebony was only 45 years old when she was diagnosed with stage N2 bladder cancer. Having lost her own father at a young age, she had to process the fear of not being there for her 3 sons.
She then underwent MVAC chemotherapy and an 8-hour surgery to remove her bladder. As part of this surgery, part of Ebony’s small intestines were used to create a neobladder.
Ebony shares her cancer journey, including taking control of her hair loss, the experience of African Americans in the medical system, the importance of self-advocacy and support, and using her story to be a light for others.
- Name: Ebony G.
- Symptoms:
- Microscopic amount of blood in urine
- Increased to visible amount of blood
- Pain when urinating
- Weight gain in midsection
- Diagnosis (DX): Urothelial muscle-invasive bladder cancer
- Staging: N2
- This means the cancer has spread to 2 or more lymph nodes in the region
- Tests for (DX):
- CT scans
- Checking IUD for issues
- Cystoscopy
- Biopsy
- Treatment:
- MVAC chemotherapy
- Methotrexate, vinblastine sulfate, doxorubicin hydrochloride (Adriamycin), and cisplatin
- 6 infusions, biweekly
- Surgery
- Removal of the bladder
- Neobladder
- MVAC chemotherapy
- Introduction and First Symptoms
- Finally Getting Diagnosed
- Next Steps After Diagnosis
- Processing the full diagnosis
- Losing a parent at a young age
- Worrying about leaving your kids behind
- Telling your children about the diagnosis
- How did your urologist describe the results to you?
- Receiving treatment at Duke Raleigh Hospital
- Receiving a binder of information to prepare you
- Was the pamphlet comforting, or what did you feel looking at it?
- Hair Loss
- Treatment and Recovery
- What was your chemo regimen?
- How did your doctor describe the treatment regimen to you?
- Importance of hearing from people you can relate to
- What were your options for removing your bladder?
- How long was the surgery?
- Recovering from the surgery
- Recovery in terms of sexual health
- How long has it been since the surgery?
- Finding Support and Advice
- Reflections
This interview has been edited for clarity. This is not medical advice. Consult with your healthcare provider for treatment decisions.
Introduction and First Symptoms
Tell us about yourself
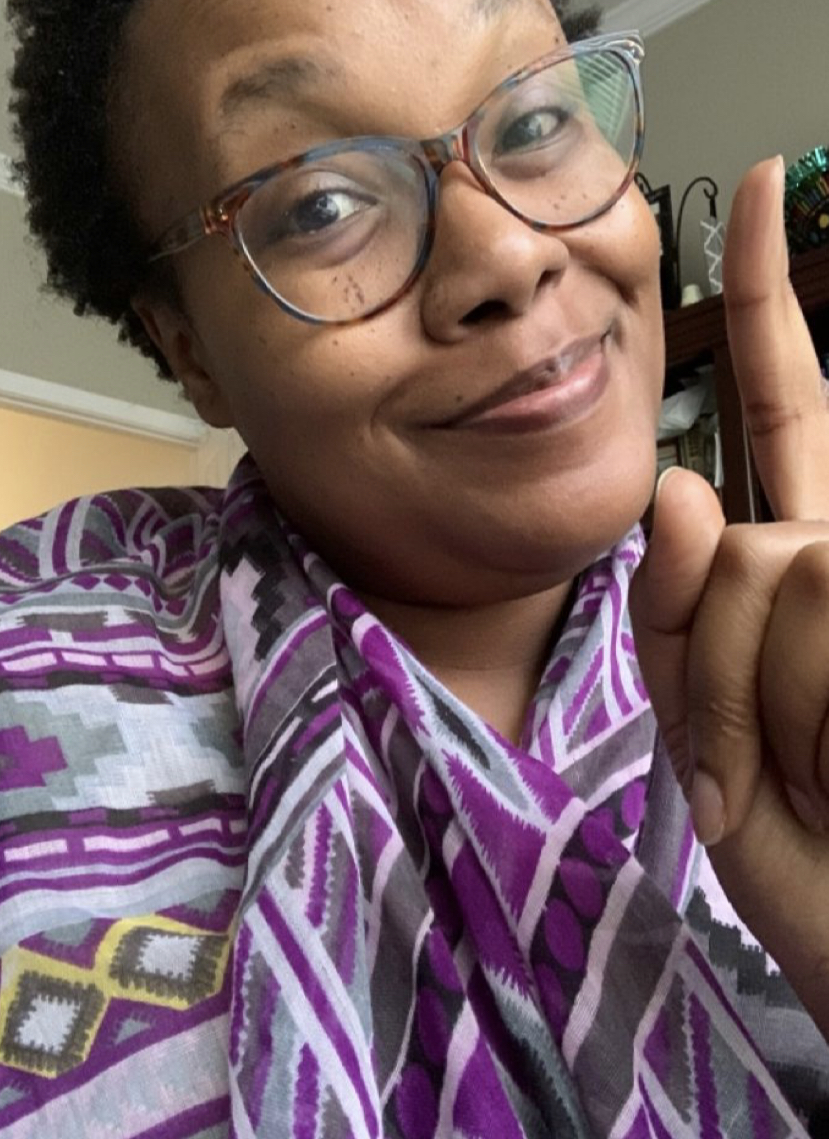
Hi, my name is Ebony, and I was 45 when I was diagnosed with bladder cancer.
I am married. I have 3 sons. I am an engineer by day. I just want to live my best life like everyone else. Those are the biggest things. I really want to live my best life and help others do the same.
What were your first symptoms?
My initial symptom was after a visit with my annual gynecologist, and they noticed that there was blood in my urine [at] a microscopic level. I couldn’t even see it, but a microscopic level of blood in my urine. They referred me to a urologist to try to look into what was going on. [It] kind of freaked me out.

That’s how it started over 2 years ago, pre-COVID actually. I proceeded with the urologist. They couldn’t find anything. I had different scans [and] different scopes that were performed and initially couldn’t find anything.
He said, “We’ll just keep you on a schedule. You’ll just keep coming every 6 months, and we’ll check on you.” I didn’t have any other red flags. Generally very healthy. [I] never went to the doctor except for my physicals. [I was] not on any other medication, [and I had] no high blood pressure, cholesterol, diabetes, no other health issues. [I] was pretty active.
The doctor was kind of like, “We’re not seeing any smoking gun, so we’ll just keep watching you.” That’s how it started. [I] didn’t have any pain [and] no other symptoms.
Looking for potential causes
We looked at several things. We initially thought it was a UTI, so I was prescribed an antibiotic and then thought, “Okay, we’re good to go.” It kept going, so then the next thing was, “Okay, let’s check your IUD. Go back to your gynecologist, check the placement of your ID, [and] make sure that that’s in place.”

[I] did that. [The] gynecologist was like, “Yep, it’s good. No problems.” Then they thought we have to confirm what the source of the blood was. Is it just menopausal stuff going on? What’s going on?
I’ve read and studied that most women are misdiagnosed because I guess our bodies are a little complicated. People go grasp for the initial things that may be probable, but all of those things were batting zero.
He referred me to a kidney doctor to look at the functions of my kidneys, and all was well. I went back to the urologist, and they were like, “Well, we’ll just keep an eye on you.” That eye on me was a check every 6 months.
What scope did they perform?
I can’t remember the technical term right now, but it was a scope where they basically filled my bladder with liquid and checked. It kind of would magnify if there was anything going on in my bladder.
There wasn’t anything to be found. Generally, it made me feel like I needed to urinate. [It] wasn’t the most comfortable feeling. That was one of the initial scopes, and then also a CT.
How were you feeling through this process?
I wanted to trust my doctors to believe that they would know what was wrong. When the doctor was telling me, “Well, we don’t know,” I was like, “Okay, if you don’t know, yeah, I’m a bit concerned.”
He even told me at one point, “There are some people that over time, as they get older, their bodies function differently, and maybe that’s just you. I was like, “No bueno. No, I’ve never had this as a problem.”
I remember telling my husband, “I feel like the woman with the issue of blood, like biblically. It just won’t stop. I don’t understand.” At that point, a year passes, and now I can actually see the blood when I went to the bathroom.
Now it’s more prevalent, and my doctor is still saying, “Maybe this is just what your body’s going to do.” I was like, “This can’t be likely. This can’t make sense.”

I even started gaining weight, particularly in my midsection. I remember thinking I never gain weight in my midsection. With each of my boys, I gained 60 pounds when I was pregnant. But every time, I always gained weight in my hips and thighs.
For me to gain it in my tummy area, I was like, “This doesn’t seem right.” But even the nurse at the practice was like, “You’re in your upper-40s, mid-40s. Maybe that’s just what’s happening. You’re just gaining weight in a different way. I was like, “Yeah, no.”
I was very concerned because they couldn’t figure out what was going on after a year and a half. It got to the point where I was like, “If they don’t find something this time —” fast-forward, that was September 2021, ” — I’m going to someone else.” I also at that point had had the IUD removed. [I was] just trying to remove every possible potential cause, and we still couldn’t find anything.
Can you list those emotions you were feeling during this?
Confusion. Despair at some points because I just really didn’t know. I was wondering if there was some underlying something. I was Googling things [and] trying to figure [it] out. [I was] just kind of confused and lost as to how the professionals don’t know.
Honestly, I had never heard of bladder cancer. It never occurred to me as something to delve more into. To be honest, I don’t ever recall my urologist saying, “If you see this additional sign, then maybe we should dig more, or let me know.” I was very concerned and stressed about what this could be.

Finally Getting Diagnosed
How did you finally get a diagnosis?
The other thing was I’m not sick typically, and I remember actually coming down with COVID [in] August of 2021. Everybody was catching COVID, but still, I was like, “I’m never sick, and now all of a sudden, here we are.”
Then I actually started feeling pain when I urinated. I was supposed to go to the urologist [for] my normal 6-month check that August. Due to him being on vacation, we rescheduled the appointment. When we rescheduled the appointment, then I ended up with COVID, and so that appointment was pushed off to October.
I went in again, and he said, “You know what? We’ll go ahead and do another CT. Then we’ll see from there.” We did another CT in October. Then he called me in his office, and he’s like, “Something’s abnormal here. We’re going to need to have a surgical procedure because I see something.”
He also did that scope, the same scope that he did that year prior. In that scope, he saw something, which freaked me out. Then he’s like, “I actually need to see you in surgery in the next 2 weeks.”
I was like, “What? 2 weeks? Surgery?” My last surgery was, at that point, probably 12 [or] 13 years ago when I’d had my last C-section.
We had the abnormal CT, the extra scope that was abnormal, and then the surgical procedure to biopsy this growth that he saw to see more of what was going on.
Processing the possibility of cancer
That was in person. For that appointment to talk about doing the surgery (prior to the biopsy), I was by myself. He did [describe it as a growth or tumor], and I instantly thought cancer.
I was like a ball of tears, and the nurse that was with me said, “You’re going to be okay.” She was extremely comforting. This was a different nurse. She’s like, “I’ve been through this before. You’re going to be just fine.”
But at that moment, I remember thinking, “I’m going to die. What is this? How did we catapult from, ‘Not only it doesn’t seem like much, [but] this is probably what you’re going to always just deal with, because this is just the way your body is functioning,’ to, ‘We need you to have surgery in 2 weeks and dig further to understand what’s going on.’”
It was pretty traumatic by myself in the office, but the nurse tried to reassure me and tell me, “You’re going to be okay.”
What was the value of having someone trying to comfort you?
Honestly, I didn’t believe her, but it was a bit comforting to know that someone had been through something similar. I didn’t have my wits about me to ask more detail of exactly what she meant that she’d been through it, and I haven’t seen her since.
After that few weeks, the urologist ended up referring me to a surgical urologist, one of the top urologists in the area, to proceed with my treatment. While it was a bit comforting, I was still like, “Yeah, I don’t know that you can relate to what I’m going through. I don’t even know how you know what I’m going through. Did you really have this procedure?”
Did you feel a shift when you found out it could be cancer?
There were 2 shifts. That was one shift because I remember thinking, “I’ve trusted you for a year and a half to try to find something, and what was it about everything that has gone on in the past year and a half where you didn’t find anything?”

Of course, we trust doctors [and] trust that people are going to do things in our best interest. But I began to wonder what other signs were there that maybe you overlooked. I honestly was a bit angry because I thought, “I’ve been coming to you for a year and a half, and you haven’t seen anything. Now, all of a sudden, I need to be in surgery in 2 weeks.”
That was one shift, and then the second shift was when he told me specifically after the surgery that the growth was confirmed to be cancerous and that he wanted to refer me to someone else that could better help me.
Undergoing a biopsy on the growth
November 11th last year (2021) was when I had the surgery. I was extremely scared because even with my 3 C-sections, I was very alert in what was going on. At this point, I’m like, “Oh, you’re going to take me under?”
I’m just a bit paranoid about, like, am I going to come out okay? Then the fact that you have had a challenging time diagnosing me, and now you’re about to take me under to try to figure out what this is. I was Googling left and right [and] Googling the report to try to figure out, “What does this mean?”
That was on November 11th. Then we had plans for Thanksgiving to go visit family. I remember thinking, “You should be able to tell me what the results are almost instantly, even if it’s a week.”
But it was November 29th, 2021, before I found out that it was cancerous. The crazy thing was, in the meantime, I got this random text from another hospital not even in the state that was something about checking into the cancer center.
[It] freaked me out because at this point, it was in between me having the surgery and getting the results. I remember texting my husband, “Oh my God, does this mean I have cancer?”
But it was a total random text from a hospital not even in the state that we live in. He was like, “Ebony, don’t worry about it. That’s just a random text. It’s nothing.” But I was like, “This is way coincidental.”

Waiting for the biopsy results
It was like 6 in the evening when I received the text. I couldn’t call the doctor’s office because it was after doctor’s hours, so after the working hours. I remember calling the doctor’s office the next day, saying, “Hey, I got this random text. Does this mean that this tumor was deemed to be cancerous?”
The receptionist was like, “Oh, no, no, no, that’s not even affiliated with our practice.” But I was like, “Of all the times to get this random text… Is this the Lord preparing me for what’s about to come?” I’m thinking all the worst.
Nevertheless, we went to visit family for Thanksgiving, but the entire time, in the back of my mind I was like, “Am I going to get this result? When am I going to get the result? And is the result going to be one of my biggest fears?”
Fast-forward to November 29th. They called me in to come get the results. I remember thinking, “Okay, the fact that they’ve called me in can’t be good.” My husband went with me for that appointment, and that’s when I first saw the verbiage on the report to say that I had a high-grade urothelial, muscular-invasive bladder cancer.
I was like, “What? What does this mean? What stage? What?” I remember that was the second shift, where I was just devastated. I don’t know that I’ve ever cried like that after getting those results.
»MORE: Patients describe dealing with scanxiety and waiting for results
What was your official diagnosis?
They diagnosed me with stage 2 urothelial muscular-invasive bladder cancer. I want to say it was staged N2 because a couple of my lymph nodes were impacted.
Next Steps After Diagnosis
Processing the full diagnosis
I remember my eyes just welling up. I couldn’t even read what was on the paper just because I was so emotional from what the diagnosis was. He was optimistic and trying to be encouraging in that visit.
I just remember thinking, “What if I hadn’t come back? I’m listening to you all, and you’re saying, ‘Oh, well, it should be fine. Your body’s just maybe designed to work this way.’ What if I hadn’t come back? What if I didn’t prioritize this visit based off of some of the other verbiage that y’all were sharing with me, yet me telling you something doesn’t seem right? What if I hadn’t come back? Now you’re telling me that I’ve got this aggressive tumor growing in my body, and now you’re telling me you’re going to refer me to someone else because it’s a little more complicated than what you thought. Really?”
Losing a parent at a young age
Imagine this. I’m a 45-year-old woman, married with 3 kids. Our sons at the time were 20, 13, and 14. When I was a senior in high school, my father passed.
When I heard the diagnosis, I instantly thought, ‘Here we go. I’m not going to be around for my children.’
It was a pretty quick sickness. I remember thinking, “He’s going to recover just fine.” But I didn’t know the seriousness of what was going on. I was devastated when he died my senior year in high school. There’s always been a part of me that has wondered, “What if that happens to me? What if my boys are left without me?”
»MORE: Parents describe how they handled cancer with their kids

I’ve gone through pretty much my whole adult life missing that presence. He wasn’t able to meet my husband. He wasn’t able to meet the boys. He wasn’t able to offer insight on different things. I wasn’t able to ask him questions like, “Daddy, what do you think about this? What do you think about that?” Just input that I would have loved to have received.
Worrying about leaving your kids behind
I’ve always wondered and prayed that that would not be my outcome. When I heard the diagnosis, I instantly thought, “Here we go. I’m not going to be around for my children. What are the things that I’ll be able to do so they’ll remember me, they’ll know me, [and] they’ll know my feelings for them? What can I quickly try to do where they will have fond memories of me?”
They’re still very young, and honestly, there are a lot of memories that I don’t have of my dad because I was young. My instant thought was, “Oh, my God.” I honestly was a bit angry with God.
I’ve had to do a lot of personal work to get beyond missing that presence of my dad and wanting him to be proud and wanting to accomplish certain things. That’s been a lot for me. To think that they would potentially be catapulted into this same space was extremely devastating and challenging for me.
I just remember my instant thought was, “How much time do I have? How much time do I have?” I didn’t know anyone with bladder cancer. I’m a bit of a fluke. The doctors would say, “You’re a unicorn. You’re checking all the boxes, [by] trying to live a healthy lifestyle. Yet here we are. You’ve never smoked. You’re not an older white male, yet here we are.”
It was extremely devastating for me because I remember thinking that my children are going to grow up without their mom. That was a space that I’ve always not wanted to be in because I hated having to experience it myself.
Telling your children about the diagnosis
I’m trying to think how we even came to how we were going to share, because I didn’t want them to worry. We decided not to share much. Initially, we weren’t going to share really much at all because my first appointment with the other urologist, it sounded like, “You’ll still keep your hair. Your hair may thin a little.”
I was planning to continue to work. I was really trying to kind of maintain that normalcy. Fast-forward [to] when we met with the hematologist. He was like, “Oh, no, boo-boo, you’re gonna lose all your hair,” which was extremely devastating. “You’re going to have chemotherapy or infusions every other week. After the second infusion, it’ll be extremely challenging for you.”
Hearing all those things made me say, “Okay, we probably need to share something.” My husband honestly did all the talking when we shared. I’m extremely emotional, and I’m a big crybaby. He was the one that shared. We didn’t discuss details of staging. We weren’t intending to, but the oldest one, who was 20, was instantly like, “Okay, what stage is it?”
We just talked as a family. This is the deal. This is what’s going on, but we will get through this. Like I said, he did all the talking because I would have been a blubbering mess. He did all the talking, and I honestly think that was the best part of it, that he was the one that kind of put a positive spin on it all for them.

How did your urologist describe the results to you?
It was a very short appointment. I remember him asking me if I had any questions, but I was like, “Yeah, I got all the questions, but I don’t know what questions to ask.” I don’t know if he was just struck by the amount of emotion that I was expressing.
It was just more of a, “I’m going to connect you to someone else that is going to help you better than I can.” I remember thinking, “Well, dang.” I was just so overwhelmed. I didn’t know what questions to ask. I had a ton of questions, but I really didn’t even know.
Of course, some of the main questions were, “How serious is this?” There was not any discussion at that time of treatment. No discussion about any of that. I didn’t really get into all of that discussion until I met with my other urologist.
Receiving treatment at Duke Raleigh Hospital
All of my treatments after that point were primarily through Duke Hospital in Raleigh, North Carolina. Honestly, that was probably one of the best decisions for me. It’s great because the treatment was relatively close to us, so we didn’t have to travel far.
After that diagnosis, there was a slew of appointments. I can’t even tell you how many appointments. Every day, it felt like I was at another appointment, and it was a whirlwind of appointments.
That surprised me because I had to go to different doctors for them to check my heart, to check my liver, to check all these different organs. The hematologist knew what my body was about to have to undergo. They were trying to make sure that my organs were going to be able to withstand all of these really harsh treatments that I was about to start taking.
Most of my treatments were at Duke Raleigh. The hematologist and urologist worked hand in hand to enlighten us on what was about to happen.

Receiving a binder of information to prepare you
My first appointment with the urologist was accompanied with this huge binder, this 3-inch binder of tons of information, including a section on hospice care.
All of it was about the medications that I was going to have to take, the potential types of urinary diversion, you name it. That binder was the gospel for me for the next several months. [It was] a little daunting to get that binder. Then there was another little pamphlet that had pictures of people, I guess, that had bladder cancer.
I remember thinking on the cover of that little pamphlet, “None of the people that have been diagnosed with this look like me.” There may have been one woman on the picture, but she wasn’t African American. Everyone on that pamphlet looked older and not like me, but I was like, “Okay, here we go.”
Was the pamphlet comforting, or what did you feel looking at it?
I looked at the different types of urinary diversions when I opened it, and I remember thinking, “Wait a minute.” I was actually kind of vain at the time. I was like, “Wait a minute. What is this? Does this mean I’m going to be left with a bag outside of my body? Does this mean I’m going to lose my hair?”
I was physically trying to think through what the impact was going to be. I remember talking to the urologist initially, and he said, “This is the new and improved one.” I remember him saying, “Your hair will likely thin,” and so I remember thinking, “Okay, I can manage that because I had a ton of hair.”
I was okay. Then right after his appointment, I had the appointment with the hematologist [the] same day. The hematologist was like, “You’re going to lose all of your hair.”
I just was devastated at the thought of, ‘How am I going to manage not having hair?’
I went from, “Okay, I think I can manage this,” to, “Like all of it, all of it?” He’s like, “Yeah, no, without a doubt, you’re going to lose all of your hair.” Again, I [was] just devastated, bawling in the doctor’s office. [I] can’t even read the material that they’re handing to me.
We didn’t tell the boys at that point. It wasn’t until for sure we knew I’m going to be physically impacted. I’m not going to be able to hide it per se. That’s when we decided to share with them.
Hair Loss
The importance of hair as a Black woman
As a black woman, actually it takes a long time for our hair to get to the lengths that we enjoy. My crown, as I call it. There’s a lot of pride and joy in my hair. Actually, for about 7 or 8 years, I had decided to become natural, so not having any chemical products in my hair, not having any relaxers to relax my curl pattern.
I had really worked hard to grow those chemicals out of my hair. [I would] keep cutting the hair and just growing out for it to be at its natural state. To get to this point, where it’s 8 years in the game of being what we call ourselves naturalistas, to find out now it’s all going to come out. Like, what?
Then I’m thinking to myself, “Is it going to grow back?” You hear stories, and you see people where it does grow back. I was like, “What does that mean for me? Is it really going to grow back?”
I just was devastated at the thought of, “How am I going to manage not having hair?” That was honestly the tip of all of the side effects that were going to come from it, but the initial thought was no hair. I’ve worked really hard to become a naturalista and take pride in this crown that I wear, and here we are.
It was incredibly devastating.
Can you describe the impacts with lack of control with identity?
I was really disappointed when I found out. I have a bit of a social media presence, too. I like to be out there and sharing with people how they can live as their best selves, how to motivate people, [and how to] encourage people.

I’m like, “Now everybody’s going to know. It’s not going to be my own personal battle, because I refuse to let this stop me from still being an encouraging force to people in my circle.”
I remember thinking, “Lord, I don’t know why you’ve given me this, but I’m going to choose to believe that it’s because you trust that I can still be a light despite whatever is going on.”
I refused. I’m not going to allow this to minimize my presence on social media. I’m not going to allow this to minimize the peace that I bring in my home. I’m not going to allow this to be that.

I remember talking to one of my sorority sisters, and she’s a breast cancer survivor. She suggested to me, “Ebony, I just challenge you, maybe you want to go ahead and cut it, because at least that part you have control over.”
I never had my hair in a short style, and I was like, “You know what? I think I will.” My first chemo infusion was December 22nd, and my birthday’s January 10th. My second infusion was going to be January 5th. I remember the hematologist saying, “After your second infusion is when your hair will likely come out.”
I remember thinking, “I’m going to be optimistic. It’s not going to happen for me in my second infusion.” I can’t remember the actual date, but between December 22nd and January 5th, I was like, “I’m getting my hair cut.”
I remember texting a close friend who owns a salon and was like, “Hey, I need you to cut my hair.” She was like, “What? You sure?” At the time, I didn’t tell her what was going on. When I actually made it for the appointment, I let her know, and she was like, “Oh my God, are you sure? We don’t have to cut it. We can just wait and see. Maybe it’ll just thin.”
I was like, “No, I’m ready to cut it.” It was a very short style. That was one of the best feelings that I had. I remember thinking that I was going to be emotional during the cut, but I wasn’t, because I remember thinking, “I’m going to enjoy this, because based on what the doctor is saying, I’m not going to be able to enjoy it for long.”
I remember getting it cut and coming home that night, and my husband started crying because he was like, “You’re really having to do this. Here we go. But we’ve got this. We’ve got this. We’re going to conquer the day.”
»MORE: Patients describe dealing with hair loss during cancer treatment
That was something he constantly said to me: “Conquer the day.” I’m a creature of habit. I will look far in the future and think, “Oh, but what if, what if, what if?” He said, “Uh-uh, conquer the day. Stay like a hitch. We’re going to stay right here, between right here and here. We’re just going to conquer the day.”
Getting my hair cut was huge for me in controlling the process. I want to say for my birthday, I still had some hair. I used to wear a scarf around my head just to kind of protect my boys from seeing. Literally every day, I would wake up, [and] there would be hair on the scarf [and] hair on the pillow. It got to the point where I was like, “I’ll just shave it.” Because, again, that was me exercising my control in this situation.
Your husband shaved your head
Yeah, he did. Honestly, that was the best. I remember him thinking, “We can take you somewhere else and get a cut.” I was like, “No.” I thought I was going to be emotional, honestly, in that phase. But I wasn’t. It was honestly freeing because I didn’t have to worry.

It was coming out in handfuls. It also was denaturing my curl pattern, so my hair was sticking up on the side of my head. It was just not the most attractive. When he agreed to shave it, it was liberating because I knew, at least now, I’m not going to have to deal with seeing it come out. Seeing it come out was the worst part.
Once it was all shaved, I still wore a scarf around my head initially. Then we had a meeting downstairs at the kitchen table. My husband told the boys, “I just wanted to let you know we shaved your mom’s head and wanted to share with you what it looks like.”
We showed the boys. I took the scarf off, and I wondered “What are they going to think?” My oldest son was like, “Wakanda forever,” which was the best feeling, because I was like, “You know what? Yes. Wakanda forever.”
What did that moment mean to you?
I totally was thinking, “I’ve lost something. I’ve lost a lot, and my boys are going to look at me like I look abnormal.” But when my oldest was like, “Wakanda forever,” I honestly remember thinking [about] the movie. It took me back to the movie and how the women whose heads were shaved look like queens. [They] looked like royalty.
There was nothing that I saw in them that was a loss. He probably doesn’t realize it, but when he said that to me, it equated to me like, “Honey, there is nothing here that is a loss. You are still a queen regardless.” Like I said, he probably doesn’t realize it, but for me, that was reassurance that that’s what he saw.
Treatment and Recovery
What was your chemo regimen?
I would go every 2 weeks, every Wednesday, and I had 4 different drugs. The acronym was MVAC, and it was 4 different drugs. I would go in for my blood work at like 8 in the morning, and then they would administer the chemo.
None of it was administered at the same time. There was a series. I can’t remember the order specifically, but there were some drugs that were administered. One of them people affectionately call it the “Red Devil,” and I was like, “Nah, that’s the blood of Jesus.” Anyway, I would try to be very optimistic when I went in there.
When I would see the nurses, they were all suited up with things to protect them from the same chemo, the meds that they’re giving me. I’m like, “This isn’t a good sign.” They would start administering the chemo, [along] with some of the meds.
There were 2 meds that were known to cause neuropathy, and so we would ice my hands and feet while the med was being administered, which was a bit challenging as well because it’s cold. I would sit with my hands in ice and my feet in ice for as long as I could bear it, then take it out for a few minutes, and then submerge everything again for as long as I could while those meds were being administered.
Generally, I would hope for a window seat because I was always surprised at how many people were undergoing care in the infusion center. All of it was in the same place, all still in Duke Raleigh. I would go upstairs to get my blood work [and] go upstairs to get a checkup.
They would tell me about how my blood work was looking, and then I would go back downstairs for the infusions. I would pretty much be there all day until like 3 or 4 in the afternoon. Some gracious souls would bring us food.
One of my close friends set up a meal train for us. People had signed up, and they knew every Wednesday she’s going to have her infusions. People would bring food for dinner on Wednesday nights. That was every other Wednesday for 6 infusions.
It ended up being 12 weeks. From the beginning of December — so through Christmas, my anniversary, my birthday, Valentine’s, all these big markers for me, I was having to go through all of these treatments — until the beginning of March.
How did your doctor describe the treatment regimen to you?
The urologist talked mostly about what the entire treatment would look like. The urologist talked beginning to end. The hematologist specifically talked about my chemo. I knew that there would be some type of surgery at the end of all this.
Actually, what they told me was, “You’ll probably do 2 to 4 infusions.” On the day of my second infusion, my chemo doctor was like, “You’re doing really well with this. We’ll actually go ahead and continue, and you’ll have 6 infusions.”
I came in thinking, “I’m halfway. I’m going to get through today. That’s going to be halfway.” Then he was like, “No, boo-boo, we’re going to sign you up for 4 more.” That was another emotional day because I remember thinking, “Wait a minute. You’re telling me I’m doing well?”
He was like, “Well, yeah, that means your body is tolerating this. We are intending to zap this cancer as much as possible before you have surgery.” Again, that was devastating because I was just like, “I thought we were doing good. We’re close to the finish.”
What the urologist explained to me was that once I was done with my infusion, then we would have to have a surgical procedure. That surgical procedure would absolutely mean the removal of my bladder because of the type of cancer that I had.
Once it was very clear that the tumor had gotten to the muscle wall of my bladder, the bladder has to come out. There’s potential spread to other organs. We were very concerned about that. I had to do additional scans to see how far potentially it spread.
Those additional scans confirmed that it only spread to lymph nodes in the immediate area. At that time, the urologist thought we may actually have to proceed with a hysterectomy in addition to bladder removal, in addition to whatever urinary diversion they would have to do.

I remember thinking, “Can’t we get a bladder? Like, can I get something donated from somebody? Surely, I don’t have to lose [it].” It seems pretty extreme.
I remember another breast cancer survivor telling me, “Ebony, at least it’s not breast cancer.” I remember thinking, “Girlfriend, no shade on whatever else you went through, but I’m about to lose a bladder. I’m about to potentially have to wear a bag outside of my body.” We don’t even know yet what the outcome is going to be, and I can make a choice.

The other concern I had with my doctor [was], “Wait a minute, how many women have you done the surgery on? I know you typically do this on older white men, but how many have you done [like] this? I need to see statistics.” The engineer was coming out in me at that point, and I was very concerned because I was reading, Googling.
I asked the doctor, “Is there a support group that I can connect with?” The nurse said, “There is, but honestly, Ebony, the people that are going to be in that support group that’s through this medical center are likely not going to look like you. You’re not going to be able to relate to [them].”
I was like, “Another day, another devastating assessment.” But then my husband was like, “Chase on the case.” I never even thought about this because I was so emotionally triggered. He looked on social media and found a group for me of women with bladder cancer, which was huge.
While there are no doctors or medical professionals in there, it was just comforting to me to know there are other women out there. It was a very small group, but there were other women out there. I can go look at their posts [and] see what treatment they chose.
There were 3 different types, 3 different potential urinary diversion surgeries that I could have. [I was] just trying to figure out what their quality of life was after their surgery. That was a little bit more about what he shared and how we connected the dots on what I wanted to do.
Importance of hearing from people you can relate to
The doctor can say all day, “You’re going to lose your hair, but it’s going to grow back. Your nails are going to turn black, but they’re going to grow back.”
It’s so incredibly helpful to know that there is someone else, a woman like you who’s probably married, who has kids, [and] who’s concerned about the effects of chemotherapy on her reproductive organs.
I wanted to see if people were able to return to their previous level of quality of life. You have a doctor saying, “You’re going to be fine.” Hearing someone else say, “Look at me. Yes, I’m fine. Yes, I can still run. Yes, I can still go to the swimming pool.” That was extremely comforting.
What were your options for removing your bladder?
There were a few options, actually. As far as what science dictates, there are 3 different options. My surgeon made it very clear that he did 2, that there were 2 options.
I could have the bag outside of the body. There’s a more technical term for it, but I can’t remember. In my brain, I was like, “Okay, that’s the option. Bag outside of my body that I would need to empty.”
Then there was an Indiana pouch, which my doctor didn’t do, and then there was the neobladder, which is what I decided to go with. The key thing that he let me know was even if I decided on the neobladder, in the surgery, they would have to determine if my body was the best candidate to undergo specifically the neobladder diversion.
I’m skipping way ahead, but even literally right before the surgery, like a day [or] 2 days before the surgery, I was marked for the procedure that would make me have to wear a bag outside of my body. I had a physical marking on my belly because they actually wanted to see how I sit, like the folds of my tummy, in the case that my intestines weren’t deemed viable.
The neobladder consists of taking a portion of your intestines, your small intestines, and creating a new bladder. If they determined in the middle of surgery that that small portion of my intestines was not viable to be used as a bladder, then that meant that they would have to punt and go back to the bag-outside-of-the-body option.

I would not know until I woke up from surgery what I ended up with. My prayer was neobladder. That was ultimately what I decided to go with, but he also made it very, very clear that the neobladder surgery is incredibly invasive and much more involved and a longer recovery time.
I was like, “Yeah, no, that’s what I want. We’re going to figure this out.” After researching and seeing the image, he also made it very clear that a lot of people, like from surveys, 50-50 will say that their quality of life is back to where it was before the surgery.

It’s pretty much split down the board. Some people love the neobladder. Some people love the other diversion (ostomy). I decided to go the neobladder route. That’s an 8-hour surgery because they have to do 3 different things: remove your bladder, take some of your intestines, create a new bladder, and then reconnect everything.
How long was the surgery?
It was 8 hours. It may have been a little bit longer for me. My husband told me recently, that apparently when they do the surgery — I didn’t remember this data point — you’re inverted.
My surgery was a robotic procedure. There are 5 incisions on my belly now to do all of that, and it blows my mind sometimes. I’m like, “That’s all? For all that you just did in my body, 5 small incisions?”
They inverted me, apparently, during the surgery. When I came out of the surgery, I was incredibly swollen. It kind of really concerned my husband. They were like, “That’s normal. She’s just been inverted. Yada, yada, yada.” The surgery itself was between 8 and 9 hours.
Recovering from the surgery
In all the materials [and] that huge binder, it talked about so many things. It talked about the meds that I was taking. I’ll definitely talk about the continence piece, but I was taking so many meds and steroids to circumvent the side effects of the chemo. That was just one thing already.
There were other sections in the binder to talk about what could happen after the surgery. One of those things was you could be hypercontinent [and] lose all ability to control how you use the bathroom. Those were the fears that I had.
Then also [it covered] how it could impact your sexual relationships, your sexual relationship with your spouse. I just remember thinking, “Okay, look, this is a whole lot more than what I initially bargained for.”
I would find myself stressing for what the outcome would be. That’s when my husband would come back and say, “Right here. We’re going to conquer the day. We’re just going to conquer the day.”
I was extremely concerned about [if] I [was] going to have to wear products to manage through the day. I work in a manufacturing facility. I was wondering how my clothes are going to fit. Am I going to have to have additional things to use the bathroom? Am I going to have to change what I wear? I usually would wear fitted things, and so now am I going to have to have this bag that’s going to dictate [that]? Am I still going to be what I thought was attractive? You name it. I thought all those thoughts.

Recovery in terms of sexual health
Some of my biggest fears started with the chemo because I also started experiencing hot flashes. There were instructions as far as after you have chemotherapy to not engage in sexual relationship because of the chemo and potentially endangering your spouse or whatever.
I remember thinking, “As a woman, am I going to be able to help you meet your needs? Are you going to be disappointed still being married to me? Because now this ‘for better or worse’ is looking a whole lot worse than when we started 16 years ago.”
He reassures me even now, “Bae, the same guy that helped you through this cancer is going to be with us as we work through getting you back to where you feel comfortable with different things.” He doesn’t pressure me. It’s just more of a, “I’m patient. I’m here.” That’s been extremely comforting as I try to figure out how to get my body to work.

How long has it been since the surgery?
The surgery was March 30th. I was in the hospital until April 27th. I came home for 4 days and then was back in the hospital with sepsis for another week and a half. That was extremely challenging.
I knew the doctor said the recovery period would be difficult. Even still, when I came home, I still had bags hanging from my kidneys because we were trying to figure out my kidney. My right kidney decided, “I don’t know if I want to work right.” That was a bit challenging.
I had a nephrostomy tube and an external bag that I would wear to help drain urine out of my right kidney. That was all the way until June 19th. I wasn’t feeling very attractive. [I] wasn’t feeling like my best person. That [was] on top of a lot of bone pain from the chemotherapy.
My husband tried his best. He was home with me the entire time. He took leave from his job. Literally from December until June, we didn’t go back. Both of us went back to work the week of Independence Day. He was with me the entire time.
It was funny because when we went back to work, our sons were like, “Wait, you’re going back to work?” It was incredibly comforting to me to be able to be home when they came home from school. Even though I wasn’t feeling up to cooking, [it was comforting] for us to still eat dinners as family when I felt able to do so. It’s been a lot.
My husband kept encouraging me to try to stay active as much as possible. That activity sometimes was just walking. Literally, when I came home from the hospital, it was walking for 10 minutes, walking around the house with the physical therapist, just to halfway get my mobility back after atrophy from being in the hospital for so long and having issues with my heart also while I was in the hospital.
He’s been extremely patient from a standpoint of, “I’m just here with you to figure it all out.” That’s been incredibly reassuring.
Finding Support and Advice
Importance of finding other patients who you have more in common with
Looking in that social media group, [I was] trying to just scroll and see who I can relate to. Even still, as I was scrolling, while there were women in the group, because it’s a group for women with bladder cancer, there weren’t any African American women. I hadn’t found one until on the day of my first chemotherapy infusion.
I have some sorority sisters that actually went and found the representative colors for bladder cancer. I didn’t even know there was a ribbon for bladder cancer. I knew about the pink ribbon for breast cancer. I didn’t even think that there are ribbons for different cancers.


They had Googled, I guess, on the side and found out what the colors were: blue, gold, and a royal purple. They knew that I was going in for my first infusion. In our separate chat on the day of my infusion, they start posting pictures. They all have on some version of blue, gold, and purple.
I’m like, “I don’t understand,” because our college colors are blue and gold. I was like, “I’m not getting it. I don’t understand.” It wasn’t until someone said, “We’ve got on our colors for you, Ebony,” and then they sent the ribbon.



I was like, “Oh my gosh.” I was so flattered, and I was just sharing with them, “Hey, y’all, this is my first infusion day, if y’all can be in prayer.” Not only were they in prayer; they all decided to be on a united front and share that with me.
I collected all of their pictures, put them in a collage, and shared it in this social media group with the women to say, “I’m just so grateful for my sorority sisters, who are standing in agreement with me today.”


There’s a hand gesture that we use, too, to indicate our sorority. From that picture LaSonya found, [it[ turns out LaSonya is part of the same sorority. [She] was like, “OMG, hi, sorority sister. We’re here together.”
That was so encouraging because I was looking for someone that looked like me. I’d scoured Instagram, trying to find different hashtags, [but I] hadn’t found anything or anyone that looked like me that was fighting and winning at bladder cancer. To find her was huge for me, because it’s like, “Yes, we can absolutely identify on even more levels.”



What does having LaSonya mean in your life?
It’s so hard. Number one, nobody wants to get diagnosed. No one wants to hear the dreaded C, right? Of course, not to downplay breast cancer. You see a lot of stories. I’ve unfortunately had a lot of friends that have been diagnosed with breast cancer.
Because more friends have been diagnosed with breast cancer, you instantly have someone that you can think of that you can say, “Hey, here’s my friend such-and-such. If you have any questions or any parts you want to relate to, she’s here. You can connect with her.”
With bladder cancer, I couldn’t find one soul that I could say, “Hey, what are you doing? How are you feeling about losing your hair? Are you going to wear a wig?” Just all that. Honestly, it wasn’t like there were that many different questions that I would ask her.
It just was an instant, “You know everything that I’m feeling. You can relate specifically to the loss of hair. You can relate specifically to darkening complexions.” [The chemotherapy] also made certain parts of my skin darker
“You can relate specifically to all those things. You’re taking likely the same medications that I’m taking.” She was actually like a month ahead of me in her journey, so I was watching her as she was going through her journey and how optimistic she still was. I was like, “Okay, you can do this, Ebony. You can do this.” That was huge for me.
Becoming a light for others
I want people to know you’re not the only one. I have fought through this. Unfortunately, there are going to be people out there — I mean, I had people coming up to me and telling me, “Some of the side effects of chemotherapy are your food is going to taste like metals. You’re not going to want to do yada, yada, yada.”
Then I said, “How do you know this?” “My husband died from it.” Thanks, I don’t want to hear those stories. I want to be the evidence, the example. I try to tell people, “I do consider myself a miracle, and if you’re ever looking for the evidence to help encourage you, let me be your evidence. Your current-day 2022 evidence that you can fight this and win.”
Knowledge and advice from other women
One of the doctors in the practice, I remember reaching out to her and saying, “Wait a minute. He’s done this surgery on men. Am I going to be good?” She’s like, “Oh, absolutely.” She actually ended up giving me another name of another doctor within Duke that I could also reach out to.
I did not end up reaching out to the other doctor because the practice really comforted me. This practice, honestly, has spoiled me. I don’t even know if I want to go back to a regular doctor because they seem to be so genuinely concerned about my welfare [and] genuinely wanting to help me.
One of the things that comes with when you have the neobladder is self-catheterization. Everyone’s outcome may be different. Some people may only have to catheterize at night. Some people may have to self-catheterize during the day.
I remember not even knowing that my urine came out of a different hole. I didn’t know. Having the nurse share with me, “I will help you find your urethra. You can try it at first. Here’s the DVD. You can look this up.”

I remember propping, being in the bathroom for the first time and having the laptop with the DVD loaded, trying to get a mirror, trying to get this catheter, and trying to figure out where to stick it. I felt like I’d struck gold when I finally was able to empty my bladder with this catheter.
It was helpful because she talked with me. I said, “Are there any things that I can do prior to surgery to help in this recovery?” She talked about strengthening my pelvic floor by doing the Kegel exercises. I hadn’t heard anything about Kegel exercises since I was pregnant like 13 years ago. I was like, “Okay, that I can do.”
Then she talked to me about finding my urethra prior to the surgery, because likely after the surgery, I would be in pain, which was another great piece. I kept putting it off. I literally found my urethra maybe 2 days before surgery. I was like, “Okay, you’re a grown woman. You’ve done things. You’ve birthed 3 children. You should be able to do this.” I had to psych myself up [and] have the pep talk.
It was very helpful to have women in the practice that could help me work through that. I said that I was marked for the urostomy bag. We even talked about different types of panties or undergarments, bathing suits, just different things that would make me feel comfortable with my quality of life if that was the route that we ended up with.
You don’t know, again, until you wake up out of surgery. [It was great] having those women present to help me find my urethra [and] to help me work through those emotions of what happens if I do have to have a hysterectomy, which I didn’t. What happens if? All the ifs. That was extremely helpful.
Advice for dealing with a neobladder
Know that you don’t have to do everything. As women, we’re used to doing everything. Let your body heal. Don’t be in a hurry to do all the things. Make sure that you stay active, even on days that you don’t want to.
Have an accountability partner that will help you stay active. Even if it’s walking 10 minutes a day, and then, in the following week, you’re walking 12 minutes and 15 minutes. Having someone meet you to say, “Okay, girlfriend, let’s go walk.” That activity was huge for me, even if nothing more than just getting out.
I had a playlist that was also encouraging to me. On those days that were rough for me, I would put that playlist on, and that would typically help me feel better. Those were some of the main things.
From a vain sense, because I keep talking about vanity, I had several loose dresses for me because I had that extra bag. I remember one of the first things when I went home from the hospital was, because I wasn’t expecting to have this extra bag, but I just wanted to go to Target. I remember not having clothes. Some of my dresses were shorter prior to, and so I needed a midi length that was loose.
I remember going to Walmart and just having dresses to wear where I still felt pretty. I also had comfortable shoes as well. My husband [and I] ordered some extra sneakers because despite all of the extra things to try to prevent neuropathy, I still have neuropathy in my feet.
Initially, I just needed comfortable sneakers to be able to get around. Not going overboard and buying a ton of stuff, but having a couple of things where you still feel cute. It’s funny because after you have a baby, they tell you you’re not going to lose all the weight immediately, and they tell you to have comfy clothing.
That, for me, was extremely helpful, and having those couple dresses to be able to [go] if I just wanted to ride to Walmart, because that’s literally what we were doing half the time.
Then when I built up the stamina to walk a little more, literally, we would walk to Target of all places, and then just walk through the aisles with the buggy to help stabilize me. My youngest son was like, “Why Target?” I was like, “Everybody loves Target.”
You got your popcorn. You got your Starbucks. You got just a normalcy. I wouldn’t even buy anything most days. Just walking around, feeling somewhat normal, was helpful for me.

Transitioning to the neobladder
There are tons of concerns because you could potentially have a UTI. I guess we’re highly susceptible to UTIs. I had issues with my kidneys. There were a lot of complications with that, but the biggest thing as far as recovery was training my neobladder.
Now you’ve got this neobladder. It can only hold so much, and so you have to train it. There was a schedule that was also in that binder that was shared with me on how to empty [it]. I would have to empty my bladder on a certain cadence.
I remember the first time I tried to do it, it took me a minute to kind of get the sensation down to understand how I actually empty it. It’s hard to describe, but I remember thinking, “Okay, Kegel exercise. Kegel, okay.”
It was the relaxation. Doing the exercise itself and relaxing the muscle is what helped me. That’s how I would use the bathroom. Anyway, there was a schedule for that. Every 2 or 3 hours, I would initially be trying to empty my bladder.

Then that period of time extended overnight. I would try to always catheter before I went to bed. I would also wear a pad when I went to sleep because I was nervous about wetting the bed. I don’t have to do that now. I do wake up in the middle of the night still to empty my bladder. Sometimes that includes a catheter at night just because it takes me time to empty the bladder.
Even now, sometimes, I’m a bit paranoid if I go to a public restroom, even at work. This is something I’m still working through. When I go to the bathroom at work, I have so many meetings that are back to back.
I can go in a stall, and another woman can come in the stall. She can empty her bladder and be done. Literally, I’m in there trying to do exercises to empty my bladder. I always wonder, “Is the person next to me thinking, ‘What’s going on over there?'” I’m still working through that, but I’m comforted in knowing that I’m alive. I need not worry about what someone else is thinking is going on in my stall.
I’m grappling with, “Do I want to tell my manager?” Sometimes I may be late for a meeting because I’m emptying my bladder. I haven’t had that conversation because I’m trying to work through that.
Sometimes, because there are meetings after meetings after meetings, I don’t have [time]. I have to literally make the time to go empty my bladder. That’s a bit of a challenge for me because if it gets too full, there’s potential for infection and all the things. I’m still working through that.
When I’m home, it’s easy. I can just go to the bathroom [and] not worry about how long I’m in there emptying my bladder. I still, straight up, have a hard time finding my urethra without a mirror. The nurse reassured me eventually it’ll be like a tampon. It’ll be where you can find it without even looking.
I’m looking forward to that day, because honestly, it is a challenge. It’s things that you don’t think about. When I travel and I’m in the hotel room — this may be TMI. I don’t know. When I’m in the bathroom at home, I have a self-standing mirror that will help me find what I need to find so that I can fully empty my bladder.
When you travel, you don’t typically have a self-standing mirror, so you’re either trying to prop your leg up or trying to find your phone, but you don’t have that many hands. You literally need a third hand to use the catheter, have something to locate the catheter, and then aim. It’s a challenge, but I’m working through that, and I am just conquering the day.
Reflections
How important is self-advocacy?
At the end of the day, no one knows your body like you do. In hindsight, I wish I’d possibly gone somewhere else sooner. I just challenge everyone out there. At the end of the day, doctors are doctors, but they are practicing medicine. They’re practicing, so they will not know everything. You know your body more than anyone else.
All I can challenge anyone out there that’s debating or [wondering], “Is there something wrong? Should I do more?” Yes, you absolutely should. Don’t debate. Don’t delay. Don’t let months go by before you inquire or search more.
Again, always remember that you know your body more than anyone else. Don’t be fearful of what the outcome can be, because the sooner you find whatever is going on, the sooner you can start treatment, the sooner you can do the life-saving work so that you can be around for those that love you.

»MORE: How to be a self-advocate as a patient
Healthcare system and the experiences of African Americans
It’s unfortunate that this is the case. I know for African Americans, we don’t see a lot of ourselves in a positive light. We don’t see us conquering things on a basis. What we do see is negative outcomes.
We see a lot of loss or, “It’s just the way it is. This is just the way it’s going to be [and] the way it’s always been. No one’s going to help you. No one really cares about you. You can be lost, and people would care less.” If you can’t afford something, you’re doomed to whatever you can piece together.

When you’ve seen that for generations — sometimes, [for] people who are not African American, it’s hard to relate. But when all you see is something negative, when all you see is, “This is the outcome. This is just the way it’s supposed to be,” it is extremely hard.
Again, I know it may not make sense. It’s extremely hard, though, for you to envision that someone does care. It’s extremely hard for you to envision that you can win. You can beat this. You can succeed. This is in every area.
I think what the medical industry can do is to put more faces in the forefront of people who are doing well, who are receiving the treatment, who have found their way, [and] who are winners.
Put people out there not only from people who have won the fight, but put people out there who are open and willing to help people win the fight. We need to see that the system cares about us. We need to see that, because for decades, we’ve seen so many systems that don’t.
Do you still question why this happened to you?
No. It’s crazy because it’s just been a year. It honestly hasn’t even been a year since the diagnosis. I keep like looking at my watch like, “Okay, no, it hasn’t even been a year. What a year it’s been.”
Maybe it’s Pollyanna-ish, but my belief is that God trusted me to go through this and be positive regardless. To go through this and show people how to overcome in the face of death. To go through this and show people that I did and they can, too.
There are times when I’m like, “I don’t like certain things.” I don’t like the whole catheter thing. I don’t like the aches in my body. But again, I remind myself, “Grace, girl. It’s not even been a year.”
I’ve had so many people message me since I shared on social media last December. They’ve either shared that they’ve received a diagnosis, not necessarily bladder cancer, but they’ve received another cancer diagnosis. They’ve been motivated by what I’ve shared.
I remember thinking when I was going through, “Lord, just get me through the surgery. Let me just get through.” It seemed like it was so far between November 29th and March 30th. It seems so far, and I still had no idea all the craziness that was going to happen after March 30th.
I just was like, “Just get me through to the end.” I thought the end was going to be, “Let’s get through the surgery, and you’re going to be good.” I had a friend share with me recently, “Ebony, maybe that was just the beginning, like the beginning of helping other people [and] the beginning of changing lives. The beginning.”
Again, I wanted to be like, “Whoa, okay, let me live my life now.” I’m looking at it now more so like, “Okay. God, me and you, we’re going to share.” I’m one that’s open to sharing. I could be wrong, but sometimes I think that he thought he could trust me to share the journey and be an encouragement to others.
What is your last message to readers?
I debated over how much I wanted to share on Instagram, to be honest, because I was like, “That’s a little bit open. People can find anything.” I remember thinking, “I couldn’t find anyone when I was looking. I’m searching all the hashtags, [but I] couldn’t find anyone.”
In general, what I would share with people is I know we have a lot of things that we go through in life. I used to think my weeks were rough prior to this, and I’m like, “Psh, that ain’t nothing compared. You’ve been there, done that.”
Anyway, I think it’s important for people to recognize that whatever they’re going through — it might not be a cancer battle. It could be a divorce, it could be depression, it could be job loss, layoff, or issues with your kids. It can be so many things.
Whatever you’re going through, you don’t have to put everything on social media, but know that social media could be a tool to help change the life of someone that you don’t even know just because you were willing to be transparent enough to say, “Hey, I’m making it through this, and I believe you can, too.”
Whatever it is, whatever you have going on, if you can, share a bit of it. I know people say social media is fake or it’s not the real deal, but I think that there are people out there that if we continue to share the real deal and share how we’re making it, it can help others.
I truly do believe that’s why we’re here: to help each other and not just kind of live in a silo. If there was anything I would share, that would be to just know that you have a voice, you have a light, and to let your light shine because it will absolutely help someone else.


Inspired by Ebony's story?
Share your story, too!

Special thanks again to Janssen for its support of our independent patient education content. The Patient Story retains full editorial control.
More Bladder Cancer Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy