Partner with Your Oncologist for Better Multiple Myeloma Care
The relationship between a patient and their doctor can make all the difference. A strong partnership leads to more informed decisions, personalized care, and a greater sense of control. Multiple myeloma patient advocate Cyndie Dunlap and her doctor Dr. James Berenson, president and medical director of the Berenson Cancer Center, discuss what makes their patient-doctor teamwork truly effective.
Learn how to build trust and open communication with your healthcare team. Understand the role of shared decision-making in multiple myeloma care. Hear first-hand experiences of navigating chronic cancer with your doctor by your side. Discover practical tips for advocating for yourself or a loved one during the treatment process. Explore how teamwork fosters a supportive environment for long-term care.

We would like to thank Blood Cancer United for its partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Edited by: Katrina Villareal
- Introduction
- Cyndie’s Multiple Myeloma Story
- What is Multiple Myeloma?
- The Initial Consultation
- Getting a Second Opinion
- Novel Approaches to Care
- Traveling for Your Care
- Why is Your Patient-Physician Relationship Successful?
- What Makes Your Patient Relationships Special?
- Multiple Myeloma Clinical Trials
- Key Takeaways
- Conclusion

Introduction
Tiffany Drummond: I’m an advocate who has worked in cancer research for 20 years, but more importantly, I became a care partner advocate when my mom was diagnosed with endometrial cancer in 2014. Her journey led me on a quest to find out as much as I could to help with her care. Information wasn’t easy to find, that’s why we at The Patient Story put on programs to help people navigate life after diagnosis.
This program is hosted by The Patient Story. Our multi-platform organization aims to help people navigate life before, at, and after diagnosis in human terms through empowering patient stories and educational discussions focused on how patients, caregivers, and their partners can best communicate with their doctors as they go from diagnosis through treatment with myeloma.

We want to thank Blood Cancer United for its partnership. They offer incredible free resources, like their Information Specialists, to help you communicate with members of your healthcare team and provide information about treatment options.
The Patient Story retains full editorial control over all content. Please keep in mind this program is not a substitute for medical advice.
I have two exceptional guests. Cyndie, a multiple myeloma patient, and her wonderful doctor, Dr. James Berenson, a hematologist-oncologist at the Berenson Cancer Center in West Hollywood, California, and the president and CEO of the Institute of Myeloma and Bone Cancer Research.

Cyndie’s Multiple Myeloma Story
Initial Symptoms
Tiffany: Cyndie, what were your symptoms leading up to seeing a hematologist-oncologist?
Cyndie Dunlap: I was having a little bit of back pain, but I was prompted when I got a routine DEXA scan and was told to take Fosamax (alendronate). I decided to see a bone specialist and instead of going on Fosamax, the bone specialist found myeloma.
Tiffany: Take me through that. What made you decide to talk to someone else?
Cyndie: My first career was as a critical care dietician, so I had some hospital experience and I also had a sister who had a lifelong illness. I realized to trust my gut. I knew that I wanted to see a specialist.
Finding the Berenson Cancer Center
Tiffany: How did you get to the Berenson Cancer Center, which is in a whole other state from where you live?
Cyndie: I started at a top 10 cancer hospital. I was diagnosed at the beginning of the pandemic, so I didn’t have an option. I did the standard treatment that every myeloma patient gets put on and had a transplant.
I always knew that I would get a second opinion when things opened up. I started researching and Dr. Berenson’s name kept coming up over and over and over again, so I decided he was where I was going to start.
The Berenson team absolutely fought for my treatment to get covered. They’re very skilled in navigating insurance.
Cyndie Dunlap
Insurance Concerns
Tiffany: Was it an issue having to go to a different state? Did that affect your insurance at all or was it more seamless for you?
Cyndie: It was fairly seamless. My insurance is national and Dr. Berenson accepts different kinds of insurance, so that was not an issue at all. I’ve had a great coordinator in case I had any issues.
Not that you don’t have to fight. The Berenson team absolutely fought for my treatment to get covered. They’re very skilled in navigating insurance as well, so I appreciate the teamwork on that end.
What is Multiple Myeloma?
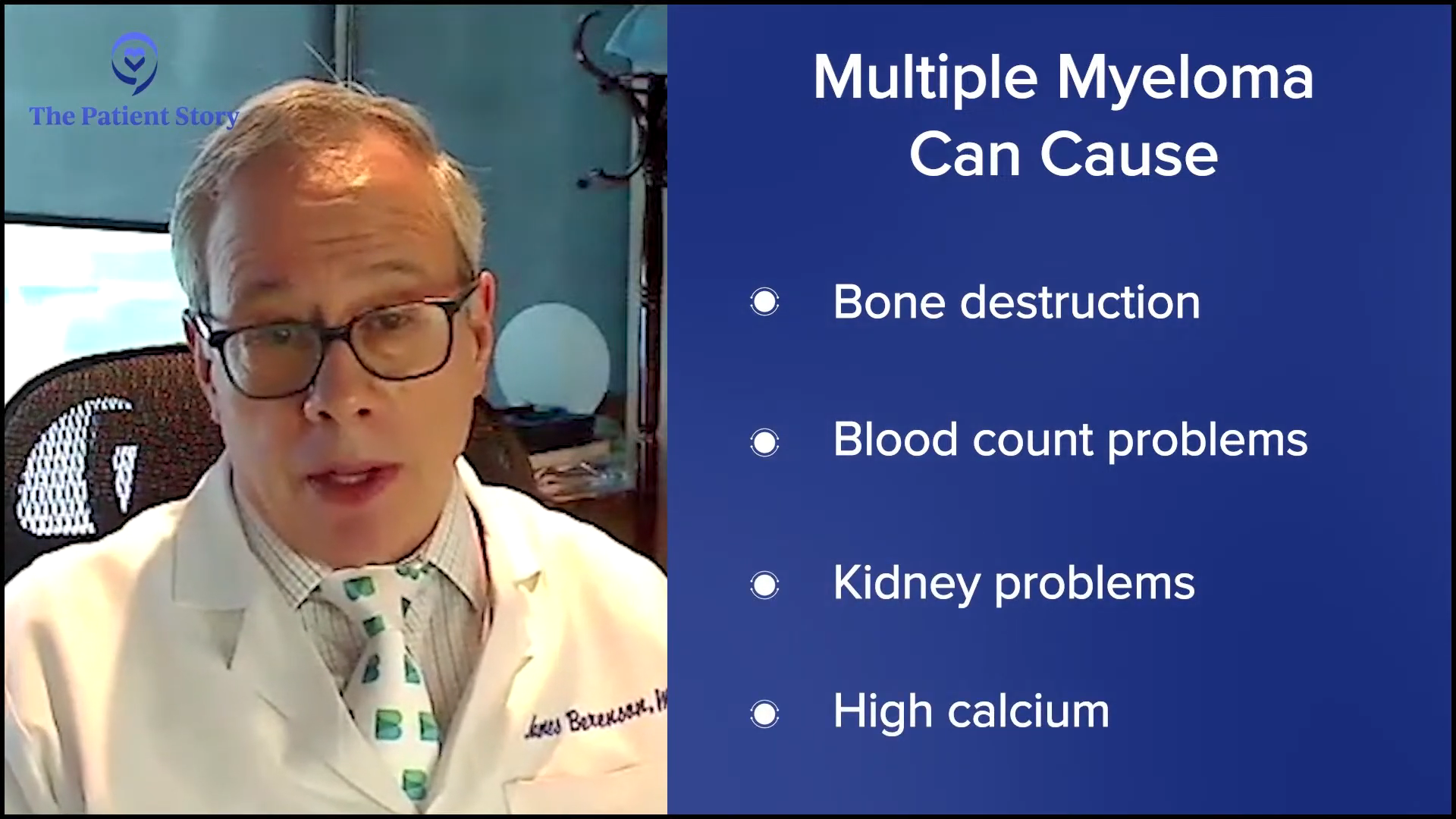
Tiffany: Dr. Berenson, can you explain in basic terms what multiple myeloma is?
Dr. James Berenson: Multiple myeloma is a form of blood cancer, but it’s bone marrow-based and it involves a type of white cell called a plasma cell. The job of a plasma cell is to make antibodies. Normally, one plasma cell makes one antibody. About a half percent of the cells in your bone marrow are plasma cells and each one makes a different antibody.
What happens in myeloma is it starts with one cell that keeps dividing and dividing. Eventually, there are billions of these cells in the bone marrow, so the protein in the blood—the antibody—sticks out like a sore thumb and tells the patient there’s a marker for myeloma.
Myeloma can cause bone destruction, blood count problems because it’s in the bone where you make all your blood cells, kidney problems, or high calcium from the calcium leaching out of your bones. However, myeloma patients are doing much better because of all the new treatments.
Tiffany: It seems very complex as opposed to a solid tumor, so thank you so much for explaining that.
The Initial Consultation
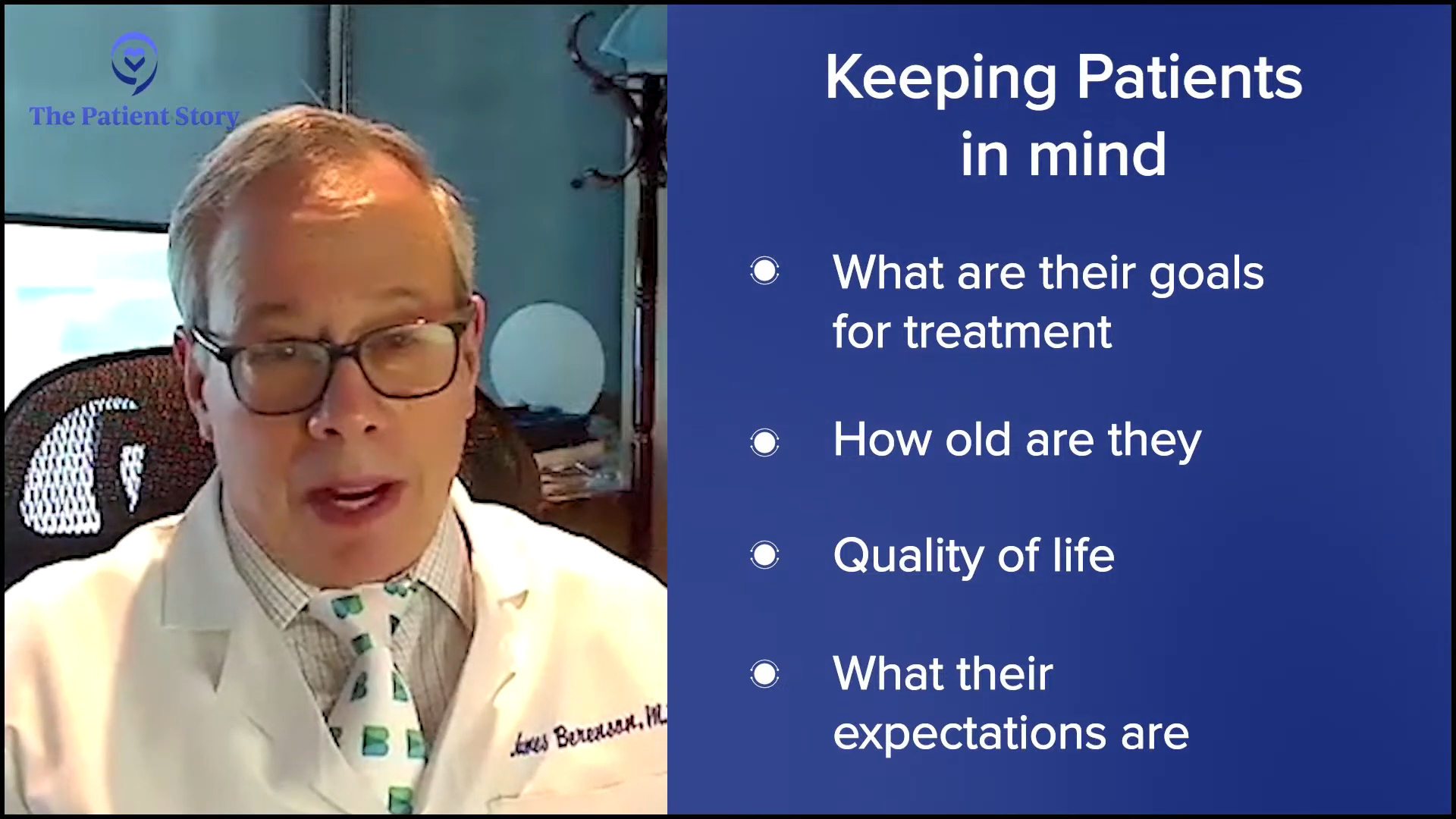
Tiffany: You get patients pretty much from all over the country. How do you approach your patients? In Cyndie’s instance when she already saw someone, what was your initial consultation like? What general questions are asked and what general information do you give at the initial consult when you meet a patient?
Dr. Berenson: I saw a new patient who came in from a kidney doctor because his kidneys were a little off. The big thing here is to make sure that you take the whole patient into account. A lot of things are blamed on myeloma. A patient who’s anemic could probably be iron deficient. Kidneys don’t quite work right, but that may be from diabetes and not myeloma.
I’ve seen this all the time. What happens many times is patients have a blinder-on type of doctor that blames everything on myeloma, they throw everything but the kitchen sink, and the patient just has iron deficiency. He doesn’t even need treatment for myeloma. They have kidney disease maybe because they took too much medication, from diabetes, or high blood pressure. When you see a patient, you have to think about the whole patient and not just the myeloma.
Take into account: what are their goals for treatment? How old are they? What’s their quality of life? What are their expectations? Do they want to travel? Do they want to stay local? All these things come into account. It’s not just myeloma.
He looked at me as a whole patient and explained things incredibly thoroughly. I’d had myeloma for two years, but he described the plan that he wanted to put me on and why he wanted to and it’s been amazing.
Cyndie Dunlap
Getting a Second Opinion
Tiffany: Cyndie, when you wanted a second opinion, you knew you wanted to go to Dr. Berenson’s cancer center where you’re getting treatment. How did that look for you? Did you already have in mind what your quality of life needed to be in order for you to sustain yourself? Or did you say you want to see what Dr. Berenson had to say first and go from there?
Cyndie: With my previous experience, I was put through some pretty hardcore treatment. It was very fear-based and not quite as helpful. I’m a very positive person, but that was probably the biggest difference when I went into Dr. Berenson’s office. We discussed. He looked at me as a whole patient and explained things incredibly thoroughly. I’d had myeloma for two years, but he described the plan that he wanted to put me on and why he wanted to and it’s been amazing.
Honestly, I’m doing things that I didn’t think I’d be able to do and I have no hesitancy doing them. One of the things that I appreciate is that I am youngish to have this disease and I live a very carefree life. I have virtually no side effects from the treatment I’m on. He had me in complete remission within, I would say, two months of starting this treatment and I had not achieved that after all the hardcore chemo.
One time, I asked him if I could go down on steroids and we discussed it and what my goals were. Ultimately, I trust his judgment. He’s one of, if not the best, in the world, but I appreciate that he takes the time to explain why he does or does not want to do something.
The goal here is to give patients a long life that they can have with great quality.
Dr. James Berenson
Novel Approaches to Care
Tiffany: Dr. Berenson, you have this novel approach to the way you do care. Do you find that most of your patients are open to that? How do you approach that when the actual treatment plan isn’t something that is a standard?
Dr. Berenson: I have the outcome data now to say we’re doing well. Our patients are living longer. As my daughter said, “They’re living better and they’re living longer.” When you walk into our clinic, you don’t even know anybody has myeloma or is sick because we don’t make them sick with treatment and yet they do well. There’s nothing better.
What Cyndie’s getting isn’t approved as a single agent, but we’ve published it works great. There’s another antibody in the company that makes it and another drug said you have to use them together. My 90-year-old, who’s been in complete remission for five years, would disagree. I won’t say everything works for every patient because it doesn’t. I’d rather start slowly and give drugs in a way that people don’t get sick.
Most oncologists don’t understand that the goal here is to give patients a long life that they can have with great quality. If people are living with better quality, they’re going to live longer and that’s shown in the results from our patients over the last 20 years.
Part of the story is our hands-on approach. Everybody has my cellphone number… We respond immediately and that makes a huge difference in outcomes.
Dr. James Berenson
Tiffany: You both are the epitome of a patient-physician partnership. You’re communicating with each other and very trusting of each other. You know that this plan is what works for you. Like you said, it doesn’t work for everyone, but your data is clearly showing that, which is promising.
Dr. Berenson: Part of the story is our hands-on approach. Everybody has my cellphone number. I don’t care when they call me, day or night. It doesn’t bother me. My daughter had a problem that a GI doctor helped with and we were all over it within an hour or two. That’s how I respond to my patients.
Cyndie: In fact, I had a GI problem and Dr. Berenson had me on the phone with the same GI doctor.
Dr. Berenson: Being available is such a big thing. I had a patient who came in with neck pain and had cord compression lower down. I got his MRI that same afternoon. Thank God he didn’t have anything on his neck, but if he did, we would have been all over it that afternoon with the surgeon and the radiotherapist. We respond immediately and that makes a huge difference in outcomes. It’s not just throwing the right brews and cocktails together of drugs, but also being available for all these other things and trying to sort them out so they don’t become major problems for the patient.
When you talk to him, you realize that he has an understanding of this disease like no one else.
Cyndie Dunlap
Traveling for Your Care
Tiffany: Cyndie, how often do you have to travel to see Dr. Berenson and what does that look like? Do you have a local healthcare team that communicates with him and shares your medical information? How does that work?
Cyndie: My treatment is every two weeks. Up until recently, I traveled every 4 to 10 days. We’ve created a special arrangement where Dr. Berenson is my primary and does all of my oncology and myeloma blood work. I receive one treatment a month locally and then I go to California for a week once every four weeks. I appreciate that he’s willing to talk to my local oncologist if I need to, but honestly, he has me in such good shape.
If anything changed and, for some reason, I needed a different treatment, I would go to California more frequently. It’s a hands-on approach. When you talk to him, you realize that he has an understanding of this disease like no one else. My kids and I all want me in his care.
Tiffany: Dr. Berenson, can you talk to me about monitoring from afar? Has the pandemic even changed how you do that? Is telehealth part of your care now? What’s that like for you when you have patients who don’t live in your local area?
Dr. Berenson: I had a consult with a guy from another country and his doctor’s the head of their myeloma unit. I wanted to give a drug that Cyndie’s on with another one because he has a very specific genetic marker. Sometimes, it’s hard to deal with other countries because they don’t have approvals and these people can’t get drugs. It’s very frustrating. I do telehealth with people all over the country and around the world, and I’m aghast at some of the care.
I have a patient in Nelson, British Columbia, who’s getting his care for his myeloma from a primary care doctor. There’s an incredible myeloma doctor I know well in Calgary, 150 miles east, but he can’t go there because it’s outside the province. He’s got a marker in which he would do beautifully on what Cyndie’s on, but he can’t go. This is frustrating for me because you know what to do, but your hands are tied.
I appreciate the way that he practices medicine and the thought behind how he approaches his patients in the clinic is filled with hope.
Cyndie Dunlap
Why is Your Patient-Physician Relationship Successful?
Tiffany: Your relationship is one that a lot of patients want to have with their physician. Cyndie, what makes your relationship with Dr. Berenson so successful?
Cyndie: He’s a very unique physician as well as an outstanding human being. There was another patient that I know who said this is a passion and not just his profession. I do believe that I am positive because I had a different experience. I appreciate the way that he practices medicine and the thought behind how he approaches his patients in the clinic is filled with hope. I appreciate the way that he treats me holistically. It’s not fear-based. I’m positive and I respond to that. I’m not alone in this feeling about him. You could survey his patients and I think you’d get similar responses over and over again.
What Makes Your Patient Relationships Special?
Tiffany: Dr. Berenson, what makes you so successful that your patients travel hundreds and thousands of miles to see you and want to keep coming back? What do you think it is that makes that relationship so special where they feel that they’re getting the best care?
Dr. Berenson: We have the best survival rate in the entire world by far. We’ll be publishing that, so I can’t say what it is right now. Let’s not let facts get in the way of opinion. If I were a patient, show me the data. Let me look at it. Let me peruse it. That will not tell you the quality of life data, but I always say if you’re feeling better, you’re probably living longer.
I don’t think very many oncologists give their cellphone numbers, but I do. Everybody has it. I don’t care when you call me. I had a patient who was worried that she had dents in her skull, which turned out to be nothing. But she was freaking out, so I said, “Come in tomorrow morning. I’ll get X-rays in the clinic.” Then I can reassure her that she’s fine. You don’t want that anxiety. You want to get rid of it with reassurance.
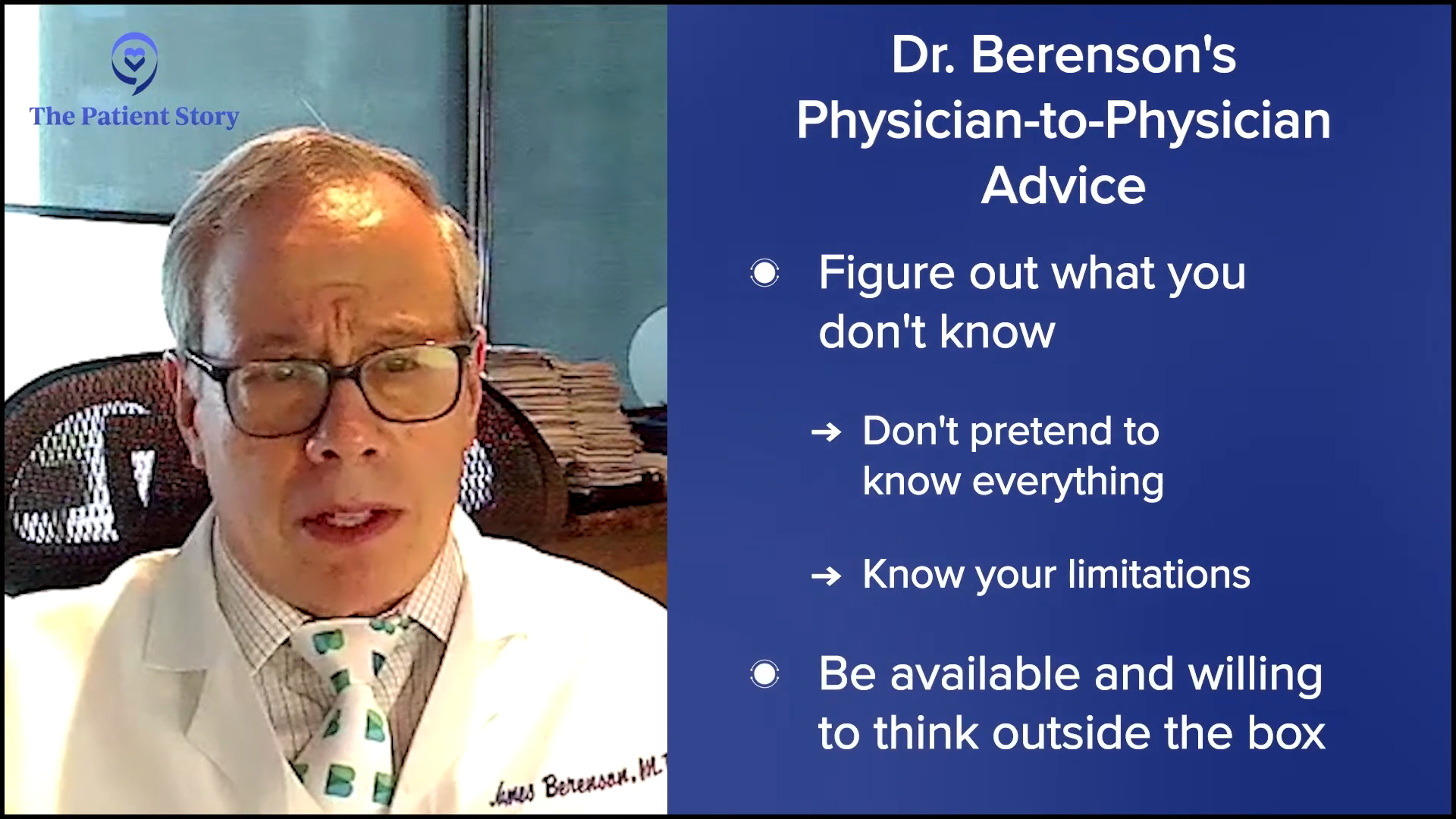
For example, like what happened with Cyndie, I got her to the guy who knows. I don’t know about her gut, but I know the guy to deal with it. Figure out a triage. Figure out what you don’t know. Don’t pretend you know everything. Know your limitations. All of that comes into play, but the big thing is availability, willingness to think outside the box, and not being afraid to try things.
I use drugs in more combinations to treat myeloma than any oncologist in the world. I’m not afraid. Sometimes you blow it and it doesn’t work, but I’m also quick to respond. We have a new marker that’s allowing us to respond. You can respond quickly if something’s going awry and that’s cool. I have a patient who’s the first person in the world going on a trial using that marker to make a clinical decision, so we’re very excited about that.
I’m more interested in trying to figure out how to use fewer drugs so we have less cost to the system and fewer side effects for patients.
Dr. James Berenson
Multiple Myeloma Clinical Trials
Tiffany: Dr. Berenson, do you conduct clinical trials at the Berenson Cancer Center or do you keep it more investigator-initiated where you’re developing it yourself?
Dr. Berenson: We try to spread the love. Sometimes, we start on a whim and we’ll try a drug that may be approved for something else, repurpose it, we’ll get an activity, and then we’ll go to the company to spread the love and do it with other sites around the country. Sometimes we’ll piggyback on larger drug company-sponsored trials.
I’m more interested in trying to figure out how to use fewer drugs so we have less cost to the system and fewer side effects for patients. Perhaps, we’re going to be able to intermittently treat with some of the newer drugs and the better markers we’re going to have to track myeloma.
I tell people that no matter where they are in the country, they should at least try to get a consultation from Dr. Berenson before they start treatment.
Cyndie Dunlap
Key Takeaways
Tiffany: This conversation has been great. It’s going to be evident to anyone how this patient-partner relationship works. Cyndie, if you could advise someone who may be newly diagnosed or even relapsed/refractory, what is something that you wish you knew?
Cyndie: I would have asked my initial oncologist: what are the other options? It was very directly said to me that my treatment was the only way to go. I tell people that no matter where they are in the country, they should at least try to get a consultation from Dr. Berenson before they start treatment. If not for the pandemic, that’s the way I would have gone. I wish that I had started with him. It would have saved me from getting a transplant and all kinds of chemo.
Tiffany: I’m pretty sure there are some people out there who feel that they’re stuck in one place. There’s no one replacing Dr. Berenson, but there may be someone close to him in your local community. Find that person if you can’t get to Dr. Berenson.
We shouldn’t allow this hands-off and less involved approach to occur… To me, it’s individualized care and getting to know everything about your patient and their life. Only then can you personalize care.
Dr. James Berenson
Dr. Berenson: You have to try to push what people should be doing. What should be the norm? The norm should be availability. The norm should be that you touch a patient and examine them. The norm should be that you spend enough time to find out whether their eyes, ears, nose, throat or something else is going on. That should be what we allow.
We shouldn’t allow this hands-off and less involved approach to occur. People are talking about personalized medicine. I find it rather ironic at a time when medicine is so much more depersonalized and I don’t think that’s the idea of personalization. To me, it’s individualized care and getting to know everything about your patient and their life. Only then can you personalize care.
Tiffany: Especially for my loved one that I was caregiving for, their care team became our family. I looked at them like I would look at family and wanted the best for them like I would family as well.

Conclusion
Tiffany: Thank you, Cyndie and Dr. Berenson, for a great discussion. Dr. Berenson is such a colorful character and brings humanization to cancer that we at The Patient Story continuously strive for. It is important to be empowered so that you and your caregivers can make informed decisions about your care.
Thanks again to our partner Blood Cancer United. Check out the links on their website and also check out their information resource center, which provides free one-on-one support. Until next time.
Special thanks to Blood Cancer United for its partnership.
Multiple Myeloma Patient Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...