Understanding Biomarkers in Lung Cancer
Discussion: Jill Feldman & Dr. Christine Lovly
Edited by: Katrina Villareal
Jill Feldman lost her mom, dad, aunt, and two grandparents to lung cancer, so she researched the disease and advances in treatment and became an advocate to help save lives from the #1 cancer killer in the country. And then her life completely changed again with her own diagnosis.
Her mission now is to get that research to every cancer patient out there, including topics like the importance of lung cancer biomarkers.
The long-time lung cancer patient and advocate sits down with Dr. Christine Lovly, one of the top lung cancer specialists in the U.S., to ask the questions she believes will help change lives.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
What we try to do as doctors is figure out what happened to make a normal cell in your body become a tumor cell.
Dr. Christine Lovly
Introduction
Jill Feldman: I’m a lung cancer patient and advocate. I was diagnosed with lung cancer in 2009. I’ve had quite a journey with different treatments, but thanks to research, I’m sitting here today.
We are joined by Dr. Christine Lovly, a physician-scientist at Vanderbilt-Ingram Cancer Center. Her clinical practice and research focus primarily on the care of patients with lung cancer.
Dr. Christine Lovly: I’m so grateful for the opportunity to connect and have this conversation.


Jill Feldman: Dr. Lovly, when you started, lung cancer wasn’t where it is now. Hope wasn’t associated with and wouldn’t have been used in the same sentence as lung cancer, so that’s what makes it even more remarkable.
Dr. Christine Lovly: We have unbelievable advancements in lung cancer. It’s incredible how fast the field is moving right now and that’s good because the need is high. This is the number one cause of cancer-related deaths in the US. Anyone is at risk for lung cancer.
What are Biomarkers?
Jill Feldman: We both have had a front-row seat to the evolution of biomarkers, which has led to this revolution of advancements in research and treatment, allowing patients to live longer and better.
Biomarkers can be found in tissue, blood, and other bodily fluids, and they’re used to diagnose a disease to determine how aggressive a disease is. Sometimes they can predict how the cancer will respond to treatment, but when we talk about lung cancer, what is biomarker testing? What are biomarkers and why are they important?
When we say biomarker, we’re saying, how did the DNA, the RNA, and the proteins change?
Dr. Christine Lovly
Dr. Christine Lovly: Nobody wants to be in a cancer clinic, no matter how lovely the people you meet, like your doctors and nurses. Nobody wants to be there. We all recognize that and have huge empathy for that. When you’re in a cancer clinic, you immediately start to learn that there’s a whole new vocabulary associated with the world of cancer and one of those words is biomarker. Let’s relate it to something that makes sense in common everyday life before we get into the science.
When you build a house, you need a blueprint, which is a map of how the house is going to be built. A blueprint is how architects design the house and how they figure out all the different components, like the roof, walls, rooms, plumbing, etc.
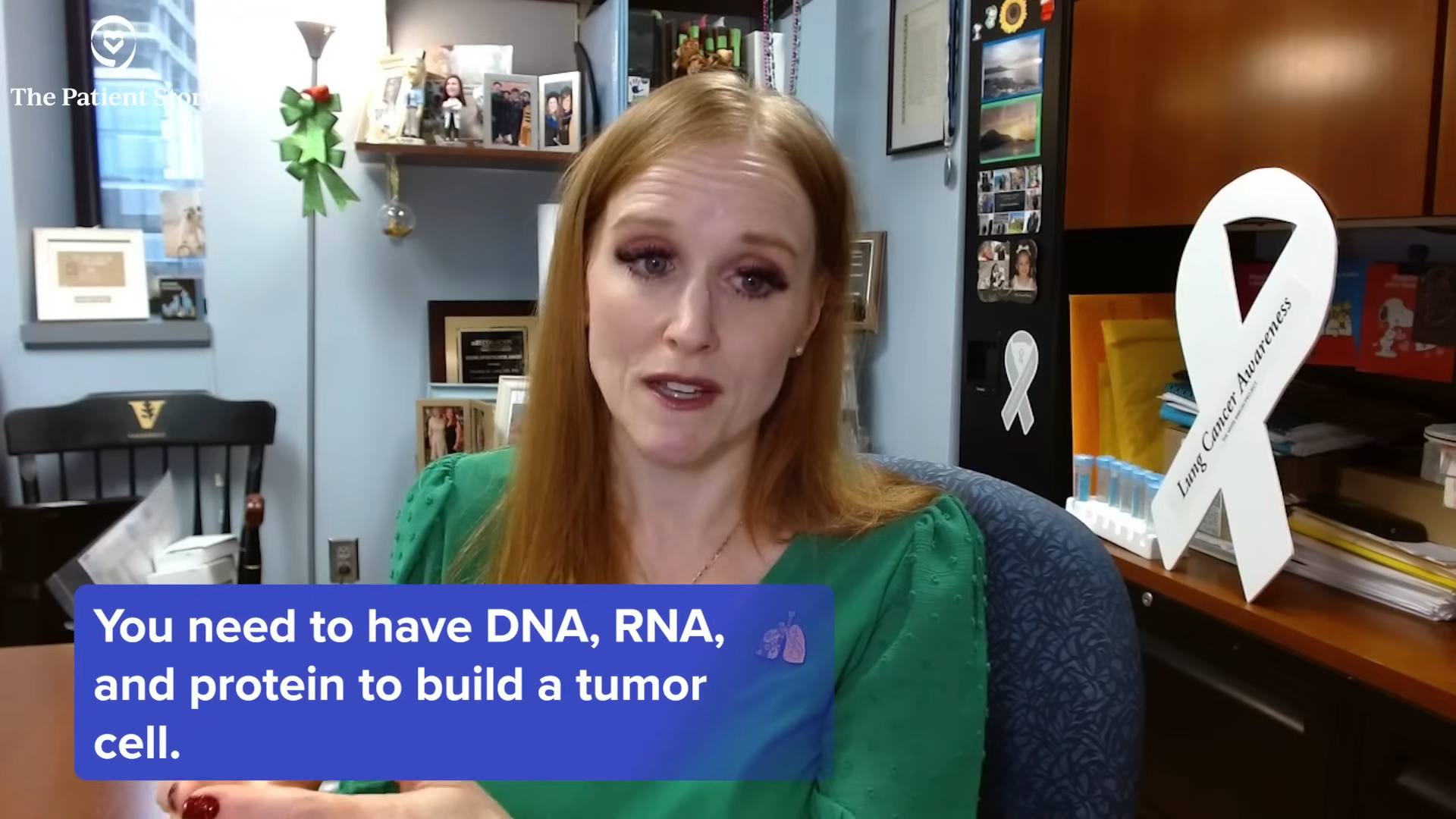
The cells in your body, including tumor cells, are very similar to that. There is a map of how those cells are made and how they act in your body. Those maps are the DNA, RNA, and protein. You need to have a blueprint to build a house. You need to have DNA, RNA, and protein to build a tumor cell.
Biomarkers look at those elements: the DNA, the RNA, and the protein. They are the architecture of the tumor cell. What we try to do as doctors is figure out what happened to make a normal cell in your body become a tumor cell. Cancer is our bodies gone wrong. It’s not something foreign. It’s our body where the blueprints have changed. When we say biomarker, we’re saying, how did the DNA, the RNA, and the proteins change? And can we detect those changes to help us pick a better therapy for our patients?
Jill Feldman: It’s hard for people to grasp that. I like that you use an analogy that everybody can relate to and emphasize the difference between inherited or germline biomarkers that are present in our DNA and all of the cells in our bodies and what’s called acquired or somatic mutations, which are biomarkers found only in cancer. They cannot be passed down to your children that we know of now. We are looking at some inherited biomarkers. We’re doing research in that area for lung cancer. We are not there yet, so the biomarkers we are talking about are the DNA, the RNA, and the protein of the cancer cell.
Dr. Christine Lovly: Exactly right. In the overwhelming majority of cases, the biomarkers that we’re looking at are something that’s changed during your lifetime and not something you’re born with. Something changed to make a normal cell become a tumor cell. The biomarkers we measure are not something that you’re born with and not something that you pass on to your children and grandchildren, but something that’s changed for a variety of reasons, some of which we don’t understand honestly, that’s caused a normal cell to become a tumor cell.
The Importance of Biomarkers in Lung Cancer
Jill Feldman: How do you test for biomarkers and why are they important in lung cancer specifically?
Dr. Christine Lovly: We’re not doing all these tests because it’s an area of academic interest. We test for biomarkers in tumors because it helps us pick the right therapies. For example, if you have biomarker A, then you get drug A, or if you have biomarker A, you don’t get drug B.
It’s important when we talk about precision medicine or personalized medicine. Lung cancer biomarkers are at the heart of driving personalization of care. We’re talking specifically about cancer, but other areas of medicine have biomarkers to help select therapy as well, so this is not exclusive to cancer.
In the context of cancer and lung cancer specifically, we’re looking for biomarkers because they help us pick the right therapy for our patients to deliver personalization of care and that’s important. There are decades of experience teaching us that we can become more refined in how we treat lung cancer when we look for these biomarkers. The goal is to put more treatment options available on the table for our patients because none of us want to say that there are no options for treatment.
Biomarkers are at the heart of driving personalization of care.
Dr. Christine Lovly
We want to be able to deliver treatments in the most precise way based on the characteristics of the tumor. That’s the goal, but there are other circumstances where biomarkers play a role. Sometimes we use them to help with prognosis, which is not the same thing as picking a therapy. But for the context of this discussion, we’re going to say we’re looking at biomarkers because we’re trying to pick a therapy for our lung cancer treatment algorithms.
Testing for Biomarkers
Dr. Christine Lovly: There are different ways to test for biomarkers and this area is evolving as well.
Let’s start with the tumor biopsy. When patients get a diagnosis of lung cancer, we have to do that biopsy by looking at whatever the abnormality is, like a mass in the lung. They take a piece of it and look at it under the microscope.
The traditional way is to look for biomarkers in the tumor specimen. You grind up the tumor and extract the building blocks: the DNA, RNA, and protein. There are ways to measure each one of those building blocks.
More recently, there’s been an explosion of technology where we can sometimes find circulating pieces of tumor in the blood. The majority of the time, we’re talking about pieces of circulating tumor DNA in the blood. This is a very rapidly emerging and evolving field. The technology is changing monthly to refine technologies for what we call circulating tumor DNA or ctDNA.
It does not replace having a tumor biopsy. A tumor biopsy is still necessary. It can help us to find the biomarkers, but not every patient has circulating tumor DNA. If we find it, it can help us make treatment decisions, but it is not exclusive. Tumor testing and blood testing to find ctDNA in the blood are complementary and not exclusionary of each other.
Not Everyone Has a Biomarker
Jill Feldman: I want to touch on a very sensitive topic in the community, which is the science behind lung cancer biomarkers and targeted therapies, matching the right treatment with the right person. It is exciting and I understand why it’s exciting, but a large number of people don’t have biomarkers or there isn’t information found, but that doesn’t mean that there isn’t necessarily a biomarker or there isn’t a great treatment option. Can you expand on that a little bit?
Dr. Christine Lovly: This is an important point. We don’t want to set the expectation that every single patient with lung cancer will have a biomarker. In the bounds of this conversation, it’s hard to get into all the details needed to understand these biomarkers. There are conferences where people spend days talking about all the different biomarkers—the DNA biomarkers, the RNA biomarkers, and the protein biomarkers—and we would need to talk about each one of those separately.
Let’s take the scenario of DNA biomarkers. Right now, there are about 10 DNA biomarkers in lung cancer that have matched therapies that are FDA-approved. Ten approved therapies are a lot for cancer, but not every lung cancer patient is going to have one of those. That doesn’t mean anything good or bad. It simply means that maybe there isn’t a DNA-matched therapy for that lung cancer patient, but there are other tools we can use, like chemotherapy and immunotherapy.
Everyone with lung cancer should have a tissue sample to do staining for PD-L1, which is a marker we use for immunotherapy. There are different levels of biomarker testing.
Right now, there are about 10 DNA biomarkers in lung cancer that have matched therapies that are FDA-approved.
Dr. Christine Lovly
Jill Feldman: That is important. When I was first diagnosed in 2009, they had recently started testing for two mutations. What was interesting about that was I was originally stage 1 and I was going to do chemotherapy after surgery as adjuvant therapy because I was young, had a family history, and my kids were little. Even though it was minimally beneficial, I needed to do everything in my power.
Everyone recommended that I do biomarker testing. All of a sudden, chemotherapy might not be the right option. It might be this targeted therapy. Taking targeted therapy as adjuvant therapy was one of the best decisions because the cancer kept coming back. Maybe it slowed down the growth of the cancer or prevented it from metastasizing. The information or the lack of information is needed to guide it, so it’s incredible.
Dr. Christine Lovly: You mentioned no information and to clarify, no information in the context that Jill is using means you had biomarker testing, but none of the biomarkers were detected. No information means you had the test, but none of the biomarkers were found. That is very different than not having the test at all. It’s incredibly important to have testing done.

How Does Biomarker Testing Get Brought Up with Your Team?
Jill Feldman: How does the conversation about biomarker testing get started?
Dr. Christine Lovly: There are multiple different ways to do the testing. Different companies can do the testing and there are different ways that different health systems do the testing. The endpoint for every patient should be the same, which is getting tested. How do you get to that end? It’s going to vary based on where you’re getting your care.
Who orders the actual biomarker testing is different from place to place…The most important take-home message is the endpoint should be the same.
Dr. Christine Lovly
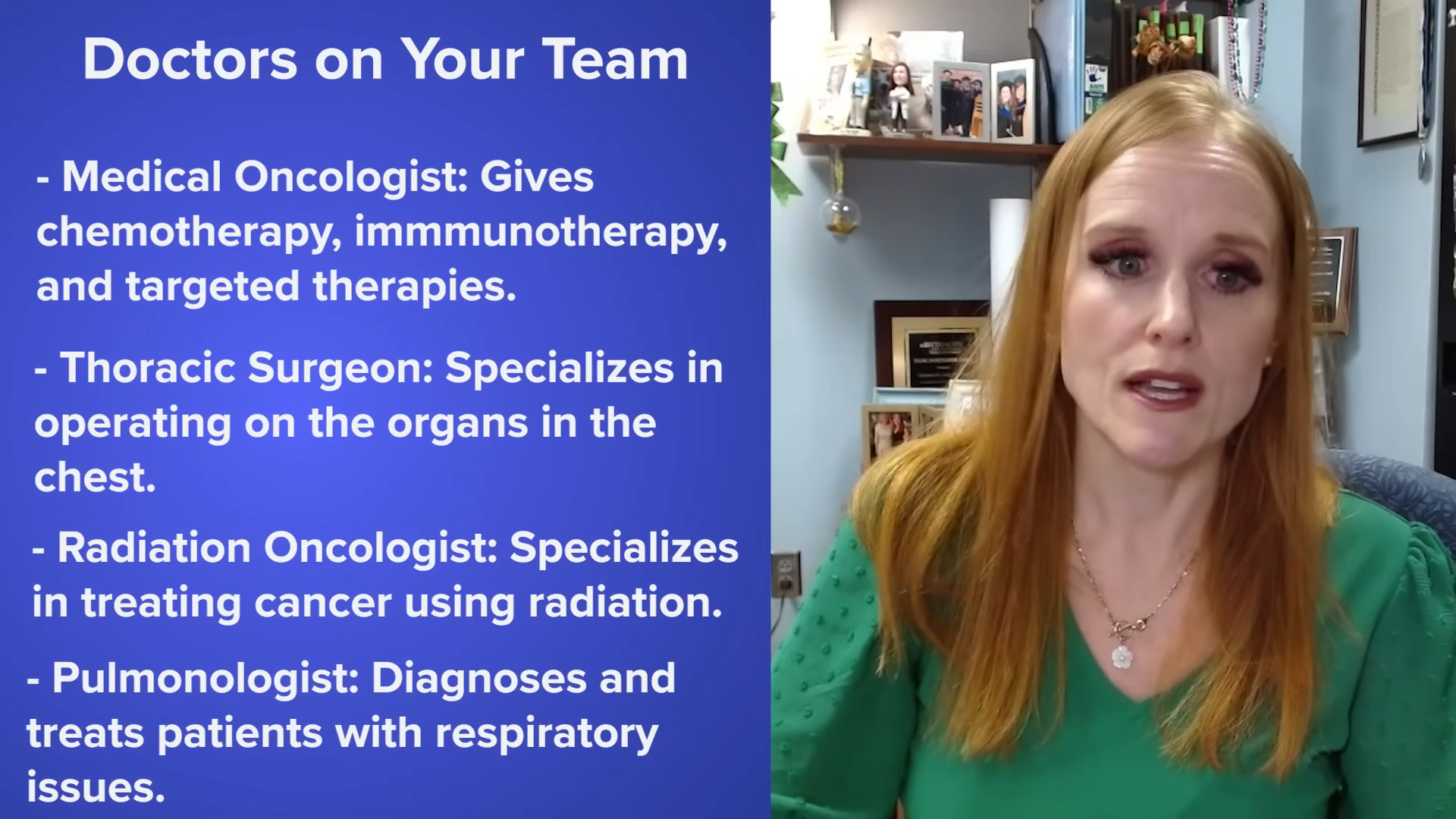
It’s very common for patients with lung cancer to have a team of doctors. I’m a medical oncologist, so I’m the doctor who gives chemotherapy, immunotherapy, and targeted therapies. You may also be seeing a thoracic surgeon, a doctor who cuts out lung cancer. You may be seeing a radiation oncologist, a doctor who gives radiation to help treat lung cancer. You may be seeing a pulmonologist, a doctor who is specialized in doing procedures like bronchoscopies where they put a tube down your throat to help get a biopsy of the tumor.
There are doctors who you don’t even meet, like pathologists who look at the cancer under the microscope and radiologists who read your CT scans and MRIs. There’s a huge team of people who are thinking about every single patient’s case and bringing it together to come up with the best plan for every individual.
Who orders the actual biomarker testing is different from place to place, so I can’t say how everyone does it, but I can say how we do it at my center. Sometimes I’m the one ordering it. Sometimes it gets what we call a reflex, where the biopsy will be done and the pathologist will reflex the order, which means they’ll put the order in before I even see the patient.
The most important take-home message is the endpoint should be the same. The patients should get biomarker testing. This is a discussion that ultimately is going to be one that your oncologist has with you because we’re the ones prescribing the biomarker-directed therapies.
If you have your list of questions in advance, people leave feeling more empowered afterward, like you’ve checked all the boxes and addressed all the questions you wanted to address.
Dr. Christine Lovly
Advice on Talking to Your Doctor
Jill Feldman: People always ask me: when should I start talking about it? How do I start talking about it? I always say that the most important question to ask is: was biomarker testing done? If it’s before taking a biopsy or before surgery, make sure biomarker testing will be done. If people are hesitant or don’t even know where to begin, what would be your advice on how and when to bring it up with their doctor?
Dr. Christine Lovly: It’s fair to ask: is my tumor going to get tested for biomarkers? Whoever you’re meeting with, chances are that the doctor is talking to the other doctors on the team as well. If they can’t answer it, then they will refer you to another doctor on the team.
My bigger advice would be to write down your questions. What happens so commonly is when you go to a doctor’s visit, the time feels very short, and it can feel very overwhelming. If you have your list of questions in advance, people leave feeling more empowered afterward, like you’ve checked all the boxes and addressed all the questions you wanted to address. There’s a huge comfort in saying you entered with all your questions and you left with all of your questions being answered to the best of the ability of the doctor or care team.
Jill Feldman: Communication is key.
Mutations in DNA act the same way. One little change in one little letter of the DNA changes the way the DNA reads.
Dr. Christine Lovly
Having a Biomarker Without An Approved Therapy
Jill Feldman: Because of the rapid advancement, you have biomarker testing. If you have a biomarker with an approved therapy, then there are steps that doctors are supposed to follow and you’re put on that particular therapy.
What happens if there are biomarkers found, but there isn’t an approved targeted therapy for it? Those can be called different things on the reports and it’s always a source of anxiety. What does that mean? If you could talk about clinical trials in this context, that would be great.

Dr. Christine Lovly: Jill mentioned a word that’s an important word that we haven’t gotten into, but it’s a cousin of the word biomarkers and that word is mutation. Biomarker testing looks for mutations. What is a mutation? A mutation is simply the word that we use for the change that happens in the DNA.
If I say DNA, which is the blueprint of our cells, the DNA reads like a sentence. If I tell you a sentence, “The big dog ran,” you would understand that sentence. It makes sense to us all. If I change one letter in one word, like if I change d-o-g to d-i-g, it becomes, “The big dig ran.” The sentence doesn’t make sense anymore. That little change changes the word dog to dig and changes the sentence.
Mutations in DNA act the same way. One little change in one little letter of the DNA changes the way the DNA reads. That’s what we’re looking for when we look for mutations in DNA. It’s as simple as that. It’s changing the way the DNA reads and the sentence doesn’t make sense anymore. It’s not what it was intended to be. That’s what a mutation is.
I’ve lived with lung cancer for 15 years and I’m alive because of these advancements. I have benefited from them.
Jill Feldman
The Hope in Lung Cancer
Jill Feldman: My family history illustrates hope, progress, and everything that we’ve talked about with lung cancer. When my parents were diagnosed, they had three treatment options: chemotherapy, radiation, and surgery. The benefits were often minimal and the treatments were worse than the cancer itself.
I’ve lived with lung cancer for 15 years and I’m alive because of these advancements. I have benefited from them. I have benefited from targeted therapies and I’m grateful for that, but we still have a long way to go. What’s your take on the future? What do you see as being most promising and hopeful for people?
Having novel treatments, especially treatments that can activate your body’s immune system to keep the cancer at bay, will be incredibly important.
Dr. Christine Lovly
Dr. Christine Lovly: If you think about any aspect of our lives, how things are now versus five years ago, 10 years ago, and 20 years ago, things are vastly different. When I was a kid, there was no Internet and now we’re completely dependent on it. The possibilities are amazing. There is a world in our lifetimes where cancer will be a chronic, treatable condition similar to other diseases, like diabetes, hypertension, and HIV. I don’t think that’s out of the realm of possibility. How do we get there? There won’t be one solution. It’ll be many and it won’t be medicines alone.
Lifestyle factors are hugely important. We don’t talk about it enough. I’m certainly not an expert in diet or exercise, but this is incredibly important. Primary prevention and screening are incredibly important. How do we screen for lung cancer or any cancer? Are we going to be able to prevent every single cancer?
Having novel treatments, especially treatments that can activate your body’s immune system to keep the cancer at bay, will be incredibly important. We already see this. I see this in my clinic every day. Patients have dramatic responses to therapies that activate their immune system to fight cancer. It’s remarkable.
There is unbelievable hope in the future for this dreadful word we call cancer, for lung cancer and other cancers. There’s still a long way to go and a lot of work to be done, but we have so much optimism that we will get there.
Jill Feldman: I’m grateful for the hope you provide.
It takes one candle to light a dark room. Light one candle and see how many are lit from that candle.
Jill Feldman
Conclusion
Jill Feldman: Thank you for joining us, Dr. Lovly. It was so wonderful to have this conversation with you. Thank you for the hope that you provide to patients and families.
Dr. Christine Lovly: Thank you so much. There’s nobody better to host this than you. You inspire people around the world and are so beloved by the lung cancer community and the cancer community in general, so thank you so much for all of the inspiration you give us.
Jill Feldman: Thank you. My mom used to say that it takes one candle to light a dark room. Light one candle and see how many are lit from that candle. That’s why I keep going.
It’s not easy, but it’s okay to not be okay. There are days when I don’t want to get out of bed. There are days when I feel like I can conquer the world. With where I am now in my advocacy, I didn’t get here overnight. It’s been years. I’m not always okay and that’s okay, as long as we keep moving forward. That’s my why, but at the end of the day, my real why is my family.

Lung Cancer Patient Stories
Chris Draft
Background: Chris' wife Keasha passed away from stage 4 lung cancer one month after they married. He's been a passionate lung cancer advocate ever since.
Focus: Leading with love, making connections to grow lung cancer community, NFL liaison
Rhonda & Jeff Meckstroth
Background: Jeff was diagnosed with stage 4 lung cancer and given months to live, but his wife, Rhonda, fought for a specialist that led to biomarker testing and better treatment options
Focus: Education of biomarker testing for driver mutations, patient and caregiver self-advocacy
Terri C., Non-Small Cell Lung Cancer, KRAS+, Stage 3A
Symptom: Respiratory problems
Treatments: Chemotherapy (cisplatin & pemetrexed), surgery (lobectomy), microwave ablation, radiation (SBRT)
Stephen H., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatments: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Stephanie W., Non-Small Cell Lung Cancer, ALK+, Stage 2B
Symptoms: Persistent cough, wheezing
Treatments: Surgery (bilobectomy), chemotherapy, targeted therapy