The Latest in Hodgkin Lymphoma with Matthew Matasar, MD

Matthew Matasar, MD, is the chief of blood disorders at the Rutgers Cancer Institute of New Jersey and RWJBarnabas Health. He oversees hematologic malignancies, transplant and cell therapy, and benign hematology. He is also a professor of medicine at Rutgers Robert Wood Johnson Medical School.
Dr. Matasar sat down with Samantha Siegel, MD, a relapsed/refractory Hodgkin lymphoma patient, to discuss some of the most exciting news coming out of ASH 2022.
The American Society of Hematology (ASH) hosts an annual comprehensive meeting that covers new research, scientific abstracts, and the latest topics in hematology.
Thank you to The Leukemia & Lymphoma Society (LLS) for its support of our patient education program!
- Introduction
- Tell us about your journey into medicine
- What’s new at ASH 2022 on Hodgkin’s lymphoma?
- How do chemotherapy and immunotherapy work?
- What does staging mean in cancer?
- Where do PET scans fit in the treatment plan?
- Where does radiation fit in all this?
- Survivorship & patient care
- Advances in the treatment of the relapsed/refractory Hodgkin
- Any words of advice to patients and caregivers?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Introduction
Dr. Sam Siegel, The Patient Story: My name is Sam Siegel. I’m a mom of three, a physician [in] internal medicine, an avid jogger, and somebody who generally lives a very healthy life and enjoys life. I was pretty shocked when I was diagnosed with stage 2 Hodgkin’s lymphoma on the eve of my 38th birthday.
That’s got a pretty high cure rate of about 90%, especially if you go through with the recommended chemotherapy, which I did. I took six months of the standard chemotherapy regimen called ABVD.

I completed all six months and had a scan shortly after finishing that declared that I was in remission. I had no evidence of disease and what some people would even consider cured. But I really wasn’t feeling well. Even though the scan was clean, I wasn’t feeling right.
Ultimately, I had to get chest surgery to get a lymph node right near my heart in order to get diagnosed with the relapse. Once that was diagnosed, I started targeted therapy.
It’s been an incredible journey from doctor to patient and pretty soon back to doctor as I start easing back into practice towards the end of my maintenance chemotherapy that I’m on post-transplant. But it’s taken a long time to recover and to evolve as a person and make meaning of this experience.
[During] the first round of this, I kind of felt victimized by the whole process and that if I did what the doctor said and followed through with everything, it would be a nuisance of four to six months. I’d lose my hair but it’d be cured and I’d never hear from the thing again.


When it didn’t work out that way, I began to see it differently altogether. I choose to believe that this cancer came into my life as an opportunity to learn about my health and my well-being, about setting realistic goals and expectations for myself, about taking care of myself and making a space for my own self-care.
And that’s one of the main reasons why we’re having this conversation today with top Hodgkin’s lymphoma specialist Dr. Matthew Matasar with Rutgers Cancer Institute. What are the most up-to-date treatments? How should patients be thinking about Hodgkin’s lymphoma in this new era of immunotherapy and all the new therapies that are offered?
The landscape of treatment has really changed in the last 10, 20 years and that’s after decades and decades of very little change in Hodgkin’s treatment. So I think it’s a really hopeful time and a really wonderful time to be having this conversation.
Tell us about your journey into medicine
Dr. Siegel, TPS: Can you tell us a little bit about your journey into medicine and how you became interested specifically in blood cancers and lymphoma?
Dr. Matthew Matasar: When I was in college, I was a philosophy major and I went to medical school because I wanted to become a medical ethicist. I was told by my philosophy professors that if you want to be a medical ethicist, you need to have an MD or else nobody listens to you. You have no chops. So I went to medical school with the intention of being a philosopher [and to be] a medical ethicist.
When I got to medical school, there was patient care, research, and science. It turned out to be super interesting, fun, richly rewarding, and hard. And I was hooked.
Then [I] was trying to figure out where I could have an impact. My thinking has always been, “I want to be somewhere where what I’m doing matters and where if you’re good at it, it really matters.” If I can work hard and be good at something, I can actually make the world a better place in some small way. And that led me to cancer medicine, to oncology.
I was introduced to the field of lymphoma by wonderful mentors and I was overwhelmed by how little I knew and how little we knew about these diseases. I was like, “Yeah, I could imagine doing this for 30, 40 years, and I still won’t know everything I want to know, but maybe I can make a difference and help people along the way and I’ll never be bored.” And here we are.

My thinking has always been, ‘I want to be somewhere where what I’m doing matters and where if you’re good at it, it really matters.’
What’s new at ASH 2022 on Hodgkin’s lymphoma?
Dr. Siegel, TPS: Do you have any hot-off-the-press, new announcements in Hodgkin lymphoma that you’d like to share?
Dr. Matasar: ASH is chaos incarnate. There’s just a ton of science. Everybody is presenting everything new.
We continue to learn how best to use our best medicines in treating patients with Hodgkin lymphoma when they’ve been newly diagnosed as well as when, unfortunately, the disease has come back despite receiving good treatments.
There [are] a lot of questions about the best way to treat patients when they have a new diagnosis. We have all these good medicines — chemotherapy programs, targeted therapies, novel therapies, [and] immunotherapies. We have all these tools in our bag, each of which has good effects in terms of treating or hopefully helping to cure Hodgkin lymphoma, and each of which has bad things about it — side effects, risks, toxicities, things that it does that hurt people.
How do we mix and match all of these tools to come up with the best approach for an individual person? How [do we] personalize that approach? How do we tailor it so that we’re maximizing the chances of cure and, at the same time, minimizing short and long-term risks from treatment? This is the holy grail of Hodgkin lymphoma. How do you maximize cure and minimize risk? We have some good insights [from ASH 2022] in Hodgkin’s and [we’re] continuing to move that forward.
This is the holy grail of Hodgkin lymphoma. How do you maximize cure and minimize risk?
There’s long been this understanding that immunotherapy treatments, [which] harness the immune system to kill cancer cells instead of just poisoning them with chemotherapies, are very powerful treatments [for] Hodgkin lymphoma. We know this and there [are] many FDA-approved treatments to treat Hodgkin lymphoma when it’s come back after traditional treatments have failed. A lot of us want to figure out how best to use those medicines for patients before their lymphoma comes back. How do we use those to cure them the first go around?
There [are] a lot of different ways that you can imagine doing that. You can imagine we’re going to use these medicines in everybody who’s diagnosed with Hodgkin lymphoma — if you have a little bit, if you have a lot, if you have early stage, advanced stage, if you have bulky disease, [if] you don’t have bulky disease. Maybe everyone should get immunotherapies. Maybe nobody should get them. Maybe only people with high-risk disease should get them. Maybe we should only use them when treatments look like they’re not working as well as they should.
We’re continuing to get [a] first look at a lot of the clinical trials, evaluating using immunotherapies in combination with chemotherapy for patients with newly diagnosed Hodgkin lymphoma with the intention of trying to maximize cure, minimize risk. I would say the data at ASH is a little bit of a mixed bag. We’re seeing very good success in terms of getting patients into remission by combining chemotherapy and immunotherapy.
We also see that incorporating immunotherapy into treatment programs for patients with Hodgkin lymphoma comes with a price. And I don’t just mean financial price. They come with risks.
Immunotherapies activate the immune system. That can cause trouble because that activated immune system can then act against your body, [which] can lead to immune reactions where the immune system is injuring healthy parts of your body and causing lung inflammation, inflammation of your intestines or your skin, and vital organs like your heart. We have greater insight now into that risk-benefit profile [and] the risk balancing of using these treatments in patients with newly diagnosed Hodgkin lymphoma.
My read on the data is that we’re going to need to be a little bit choosier in who we use these powerful but not-without-risk treatments. It shouldn’t be a one-size-fits-all approach. I think that’s the wrong way to do it. The data at ASH supports that. If you use it as [a] one-size-fits-all, you’re going to lead to side effects that maybe were avoidable.
We need to be a little bit more nuanced, a little more subtle, [and] a little smarter in picking who we think needs these treatments in order to achieve cure and not have to go through the rigors of the treatments that we use to cure this disease when it’s come back after good first treatments.
We’re continuing to get [a] first look at a lot of the clinical trials, evaluating using immunotherapies in combination with chemotherapy.
How do chemotherapy and immunotherapy work?
Dr. Siegel, TPS: Could you tell us a little bit more about how traditional chemotherapies work, how immunotherapies work, and how the safety and side effect profiles compare with the two therapies?
Dr. Matasar: We can do that by taking a little bit of a walk back and looking at how the treatment for Hodgkin lymphoma has evolved over these last few years.
Since I was in medical school, the treatment was ABVD chemotherapy. A, B, V, D — four medicines. Each one of the different chemotherapy medicines [is] given in combination. These medicines [are] given by vein every other week for some number of months, up to six months in total. And this treatment cured many, although not all, patients.
We always wanted to do better. We knew that ABVD chemotherapy has side effects, particularly B in ABVD — a medicine called bleomycin — and that medicine is well-known for its risk of potentially causing lung injury, which obviously is not anything that we ever want our patients to experience. We’ve been trying to get rid of that drug and a very important clinical trial was conducted globally.
ECHELON-1 was a large randomized clinical trial. The great computer in the sky flipped a coin. If it came up heads, they would get ABVD and if it came up tails, instead of the B, they would get a new medicine called brentuximab vedotin or BV for short, and that would get switched out instead of the old bleomycin. It compared this new AVD plus BV compared to the old ABVD treatment.

In that study, we learned that patients who get the new treatment with BV are more likely to be cured and live longer than patients who receive the traditional ABVD treatment. That was a landmark event. It tells me that I now have a better tool to cure more people and help them live longer than I could before, which is awesome, so that moved us forward. Now we have AVDBV as our new and improved standard treatment.
My hope is that we will be able to cure more people using immunotherapies the first go around
The question is: can we do better and can we then incorporate things like immunotherapies on top of that? Many people are looking [and] saying, “Can we add immunotherapy onto AVDBV or switch one of those drugs out and add in immunotherapy? And can we continue to ratchet up the sophistication of our treatment to cure more people and help them live longer?” We don’t know yet. That’s the work that’s ongoing.
My hope is that we will be able to cure more people using immunotherapies the first go around but we need to figure out exactly [which] patients benefit the most, who needs it the most, as well as who’s more likely to have side effects with this medicine.
Dr. Siegel, TPS: How are those medicines given? Would that look like an infusion every couple of weeks like ABVD?
Dr. Matasar: In some ways, logistically, the patient experience is similar, whether you’re getting ABVD, AVDBV, [or] incorporating immunotherapy.
Typically, what this looks like is you come in [and] you see your doctor or his or her team to make sure you’re doing okay. They check your blood [and] make sure everything’s copacetic.
You get your treatment intravenously [by] putting an IV into a vein in the arm. If they have trouble getting IVs, [there needs to be] some way to give the medicines intravenously safely and that can be some form of a catheter, which is a tube that goes into a blood vessel in the chest, or what’s called a mediport, which is a little button that gets put under the skin of your chest with a little tube that goes out.
These treatments are typically given every other week. For patients with advanced-stage diseases, treatments are typically given for six months or six cycles or 12 treatments, however you want to parse it out. But that’s often what patients can expect to experience.
There is no stage of Hodgkin lymphoma that’s not curable… Stage is important because it tells us how hard we got to work at this.
What does staging mean in cancer?
Dr. Siegel, TPS: You touched on staging and I think that’s a really important clinical point for patients. You mentioned we’re trying to individualize treatment for Hodgkin’s patients based on their risk of relapse, their age, and their underlying health. There are terms going around like early stage but unfavorable versus later stage. What does that mean? There are a couple of different classifications.
Dr. Matasar: For a lot of cancers, stage is king. Cancers start in an organ in the body — your breast, your colon, your prostate, or some part. Stage is oftentimes the most important thing about what this is going to look like for you. What’s your experience going to be? Stage 1 — Yay! We got it so early! Stage 4 — often a very different conversation.
This is not the case for Hodgkin lymphoma. There is no stage of Hodgkin lymphoma that’s not curable. Staging is just fancy [medicalese] for describing where in the body the cancer is. Stage 1 means it’s in one lymph node or one lymph node area. Stage 2 is in a couple of lymph node areas but all on one side of the body.
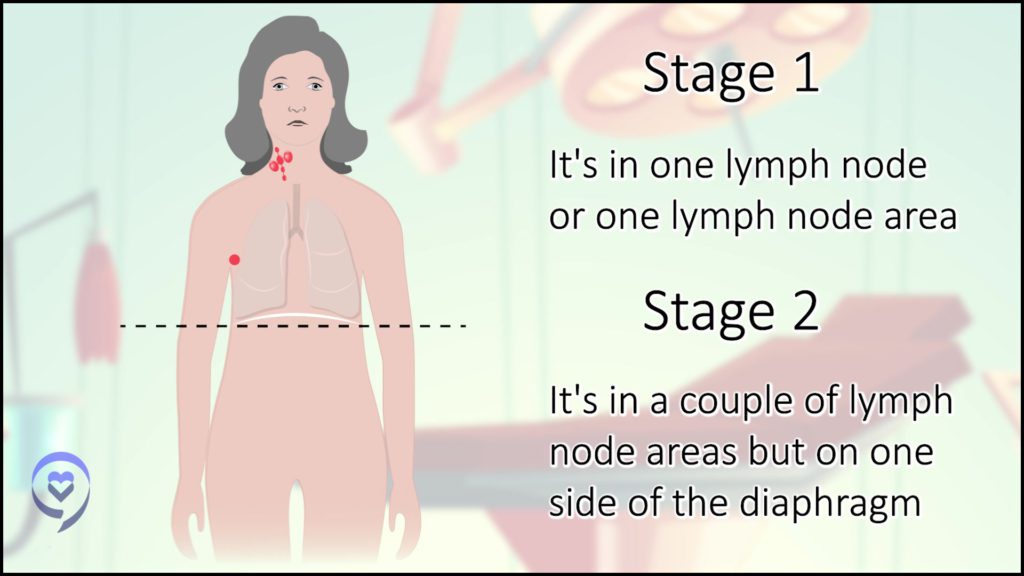
We think of the diaphragm as the Mason-Dixon line for the body. If it’s on both sides, then that’s advanced stage or stage 3 — lymph nodes above and below the Mason-Dixon line.
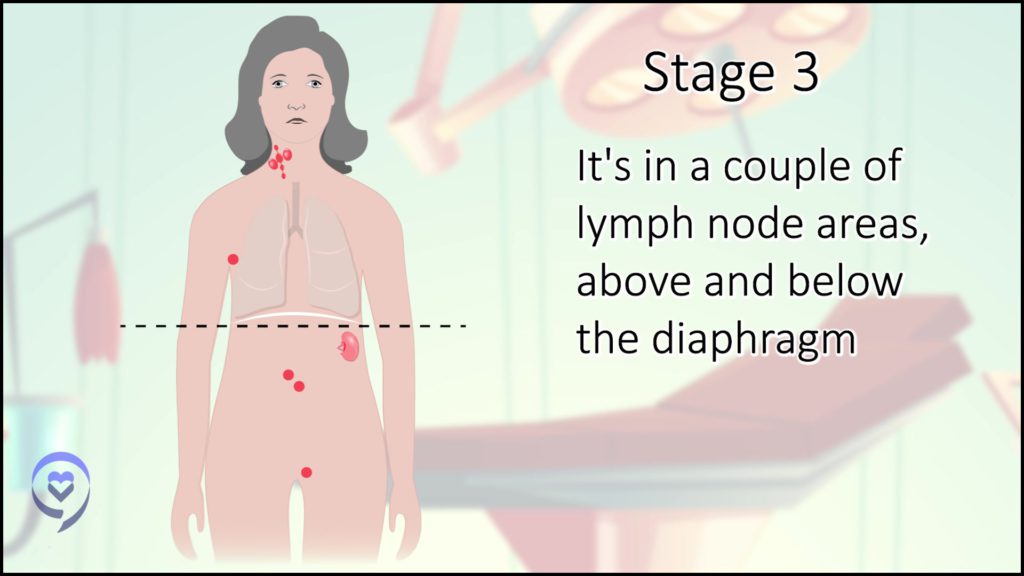
Stage 4 just means it’s in lymph nodes and something else in your body — could be an organ like your liver or your lung.
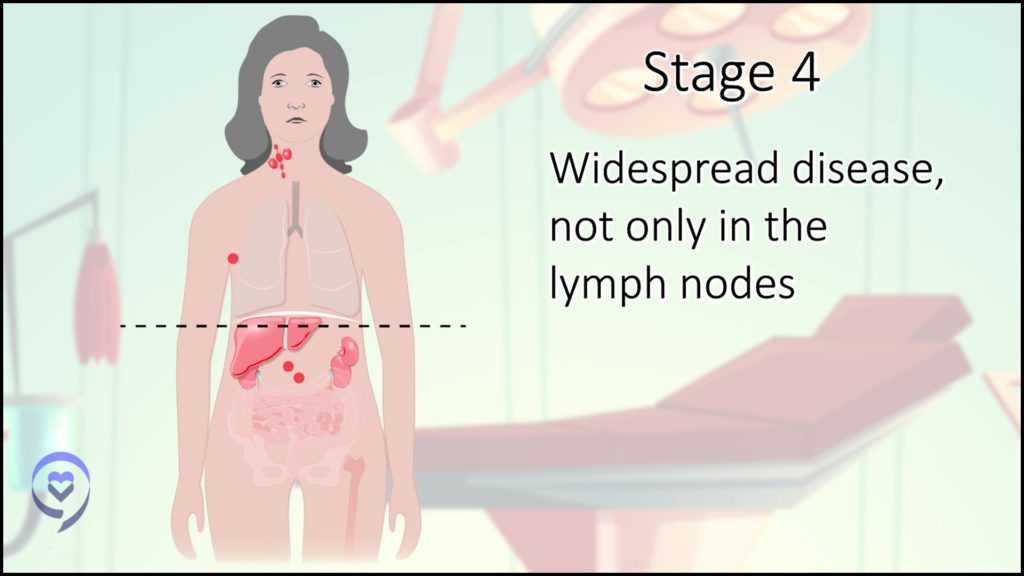
When some types of cancer have spread into other organs, that’s a very different situation from where those cancers start. Hodgkin lymphoma is a lymphoma, a cancer of lymphocytes, of immune cells, so this is [a] cancer that comes from the immune system. By its nature, your immune system is through the whole body so it shouldn’t be a surprise if these cancers show up in more than one spot. It doesn’t have anything to do with whether or not that illness is curable.
[The] stage is important because it tells us how hard we got to work at this. Patients who have less disease generally need less treatment to achieve their best chance of cure. Patients who have more disease will often need to receive a more comprehensive course of treatment in order to give them the best chance of achieving the cure, which we not only know is possible, but usually expect to achieve for our patients.
That question of whether we should do risk-adapted intensification of treatment is still, I would say, an experimental approach.
Where do PET scans fit in the treatment plan?
Dr. Siegel, TPS: Where do PET scans fit in there? There’s this idea [of] PET-adapting therapy — getting your PET scan when you start, then getting a PET scan after you’ve had some treatment, and then using that to tailor the treatment as you go. What does that mean and how can that be used?
Dr. Matasar: A PET scan is a type of body scan. It’s a way of taking pictures of inside the body, like a CAT scan where you will often use medicine that lights up the blood vessels so you can see what you’re looking at — very clear black and white pictures. A PET scan is more like an Andy Warhol painting — very bright, vivid colors and you get a lot of information about what’s going on.
What lights up in a PET scan is metabolism. It’s what parts of your body are actually using sugar for energy and the more sugar that absorbs, that sugar then is actually a little bit radioactive, and it glows for our cameras — not radioactive in a dangerous way, but radioactive in a I-can-take-pictures-of-that kind of way.
By doing a PET scan, you can see what areas in the body have unusual or abnormal metabolism. We know that Hodgkin lymphoma is very metabolically active. Those cells are using lots of energy so they light up very brightly on a PET scan. I can see those areas that are lighting up and that is really how we best stage our patients. It’s the best look at where the cancer is and isn’t at the start of treatment.
We know that many patients with Hodgkin lymphoma will have very quick improvement [in] their PET scans, even after only two months of treatment. Oftentimes, after just that little bit of treatment time, that PET scan will often be already normalized. That’s often our expectation going into treatments that the scans should get that much better that quickly.
Back when we were doing ABVD chemotherapy, I’ve already mentioned that bleomycin can be hard on the lungs. We know that the more bleomycin we have to give our patients, the more risk there is of causing lung injury. So we used the PET response adapted approach.
We would do treatment for two months and we’d do a PET scan. If that PET scan was already looking great, yeah! Awesome! We’re on the right track. Let’s not give any more bleomycin. Let’s take it easy on those poor lungs and just do AVD — no more B — and finish the next four months or six months of total treatment, but no more bleomycin to spare lung injury.
We’re not doing so much ABVD anymore. We’re doing a lot of BVAVD. We don’t have the same approach right now in terms of tweaking our treatment along the way based on that PET scan that we do after two months. We still tend to do it because we think it gives us pretty good predictive power in terms of how things are going.
There are situations in which that scan after two months may be so spooky looking to us that we may recommend moving to an even stronger chemotherapy program in order to try and make more progress. Two months, not such great news so far, kick it up a notch.
That question of whether we should do risk-adapted intensification of treatment is still, I would say, an experimental approach. We continue to see data emerging at ASH and other congresses as people look at ways of trying to address people who have an unfavorable or worrisome scan after the first two months to try to make more headway.
We recognize pretty well that radiation therapy, as effective as it is, carries a long-term risk for some patients, depending on where the radiation therapy is delivered.
Where does radiation fit in all this?
Dr. Siegel, TPS: Where does radiation fit in all this for Hodgkin’s?
Dr. Matasar: I would say that radiation therapy is still absolutely an important treatment modality that we have in our pocket. If you want to be rigorous about it, we would say that radiation is the single most active treatment in the treatment of Hodgkin lymphoma. It’s the thing you can do that is most guaranteed to get a quick response when you need it.
We are using radiation therapy a lot less than we have in months, years, and decades past and that’s because we’re trying to maximize cure but also minimize short and long-term risks. We recognize that radiation therapy, as effective as it is, carries a long-term risk for some patients, depending on where the radiation therapy is delivered.
Chemotherapy goes to the whole body from the nose to your toes so it can affect the whole body in terms of side effects. Radiation therapy is a focused treatment on a certain area and wherever the beam shines is wherever is being affected. If that beam shines on healthy tissues, there’s a risk of causing injury to those healthy tissues.
Radiation therapy for Hodgkin lymphoma is well-known for carrying certain important risks, depending on where that beam may shine. What if that beam is shining on breast tissue? In younger women and women under the age of 35 — definitely 30 — we know that if radiation therapy touches breast tissue at that young age, it can confer an increased risk later in life of developing breast cancer. And the last thing any of us want to do as doctors is to give treatments that put our patients at risk of other cancers later in life.
It’s very challenging. Do we use it anyway? Yes, if you have to. If it’s that or Hodgkin lymphoma presenting a peril to life and limb, then, of course, you have to do what you have to do. Then you are talking about how you apply good survivorship care after Hodgkin lymphoma has been cured to work to protect and safeguard a patient’s health in the months and years to come.
For patients and their caregivers, the most important thing to remember is that survivorship care is cancer care.
Survivorship & patient care
Dr. Siegel, TPS: You just touched on survivorship and some of the most important issues that survivors are facing long-term. Survivorship becomes a really, really important issue for the decades after patients are cured of their Hodgkin’s. What are some of the top things, in addition to the potential injuries to the tissues or secondary cancers that patients may get from having had the treatment?
Dr. Matasar: For patients and their caregivers, the most important thing to remember is that survivorship care is cancer care. Everybody who’s gone through Hodgkin lymphoma deserves to receive compassionate, thoughtful, wise survivorship care as they survive and live with their history of Hodgkin lymphoma.
Everybody should be able to generate what’s called a survivorship care plan, which is simply an easy, straightforward document that says this was my diagnosis — Hodgkin lymphoma. This was the treatment that I received — which medicines, which doses, how many rounds or cycles, did I need radiation therapy or not? If I did, what tissues in my body were touched by the radiation? What are the recommendations from my oncologist and their team regarding my care going forward? What do they think I need to do to be able to safeguard my health the best?
Whether it’s a digital document in your electronic medical record or something that you simply have in a file at home, that simple document can then go with you, [which] you can then share with your other doctors, your primary care providers, your other providers so everybody’s on the same page. Everyone understands what you went through and what everybody should be attentive to protecting your health going forward.
What goes into that in terms of what to do and what we advise our patients in terms of safeguarding their health depends on the treatments that you received and the risks that are associated with the various treatments that we give.
[For] people getting ABVD or BVAVD, the A in that program is a medicine called Adriamycin or doxorubicin. We know that medicine carries a risk of some small magnitude — but not zero — of increasing the risk of heart problems later in life. People that get these treatments should have attention to their heart health in the years and decades to come.
How much we need to scrutinize the heart, how often we need to do testing, and what types of testing vary from person to person based on how much of that medicine you needed and how healthy you are otherwise. Do you have other heart health problems or other medical issues that may complicate your heart health? That can be personalized in a survivorship care plan.
If there [are] complex needs, then people can actually get that care at survivorship clinics, which increasingly exist in the context of cancer centers. Patients who are survivors at [the] highest risk for complications from treatment can be followed in a more multi-disciplinary, thoughtful, data-driven way so that we can really do the very best job at protecting our survivors.
We’ve made such great strides in the treatment of patients, few though they are, who have their lymphoma come back despite good first treatments.
Advances in the treatment of the relapsed/refractory Hodgkin
Dr. Siegel, TPS: The relapsed/refractory group is a small subset of people in Hodgkin’s. My understanding from what I read of the abstracts at ASH seems hopeful even for patients who relapsed after having had a transplant and that’s really exciting for those of us who have already relapsed once.
Dr. Matasar: We’ve made such great strides in the treatment of patients, few though they are, who have their lymphoma come back despite good first treatments. Right now, we are able to cure the majority of people even when their lymphoma comes back after the treatment.
What I always tell my patient when I meet them for the first time, as I’m describing the choices that we have together to treat their lymphoma, I say, “Don’t forget that even if things go wrong and your lymphoma comes back, which is not what I hope or expect, but just remember that if it comes back, that is not a death sentence. We are still likely to cure the disease at that point. Cure meaning go away, never come back again, happily ever after, the end.
“That may require a little heavy lifting. It may require a little bit of creativity. But our expectation is still, even if it comes back, that we would and will be able to cure it. Just remember that. [On] those dark nights when you’re lying in bed and you’re worried about, ‘What if this isn’t working?’ You can remember, ‘Nope, Matt said that that’s not a death sentence and that there [are] lots of good things that we can do there.’”
That is true now after ASH just as it was true before and all the more encouraging. Where’s my encouragement coming from in this setting? I’ve been talking about those immunotherapies, as nuanced as I think we need to be about their use in patients with newly diagnosed Hodgkin lymphoma because those patients are often cured without such treatments.
In patients who have the disease come back after chemotherapy, we know that immunotherapies are very powerful and can really lead to a tremendously greater chance of cure than we had before those treatments were available to us.
We’re now understanding better how to combine those immunotherapies with other chemotherapy medicines that we traditionally use after [the] first chemotherapies have failed us. This combination of chemotherapy and immunotherapy for patients when their lymphoma comes back after good treatment is proving to be very powerful, safe, and highly successful at getting patients into remission or back into remission.
This combination of chemotherapy and immunotherapy for patients when their lymphoma comes back after good treatment is proving to be very powerful, safe, and highly successful at getting patients into remission or back into remission.
Dr. Siegel, TPS: That’s wonderful. I feel so lucky to be alive [at] this time in medical science and [have] accessibility to medicine. I think it’s just incredible. We’re so lucky that people are excited about this and interested and have continued to develop the science to help keep us alive.
Dr. Matasar: This is really a global effort. The amount of work that is being done at a global scale to improve outcomes for patients with Hodgkin lymphoma is breathtaking. And what that means is that the pace of discovery is breathtaking and our ability to continue to cure more patients safely and effectively and to restore them back to health, it’s truly inspirational.
The pace of discovery is breathtaking and our ability to continue to cure more patients safely and effectively and to restore them back to health, it’s truly inspirational.
Any words of advice to patients and caregivers?
Dr. Siegel, TPS: I agree. Any last thoughts that you think are important to relay to patients or caregivers?
Dr. Matasar: Don’t be afraid to ask questions. So often I have patients come in and they are overwhelmed — and of course. There’s so much relief to hear a plan, to hear good news that there [are] treatment options, and that cure is attainable that there’s a reluctance to want to rock the boat, to advocate for yourself, to ask questions, and to learn more.
That deference to the physician on this side of the chair? I don’t want that. I don’t need that. I would much rather be in a partnership and a conversation. What I tell my patients is that this is not my journey. This is your journey. You’re the one climbing the mountain. I’m the Sherpa. I’ll drag your bags alongside you. But this is your journey and I need you to be as prepared and ready, as informed and engaged as possible so that we can do this together.
Ask questions. Learn. Satisfy your curiosity. Ask the what-ifs. Understand your risks. Understand what your role in this is. How can I improve my outcomes? What can I do to keep myself safe [during] treatment? What should I do with exercise? What about diet? What about sexual activity while I’m on treatment? How does it affect my life? What about work? How do I disclose this to people that I’m dating? All of this stuff. The questions that naturally swarm all of our brains.
We’re trying to understand this terrible thing that’s going on. If you don’t ask those questions, you’re doing yourself a disservice and you’re not giving your doctor a chance to do the right thing with you and for you. So my one piece of advice: ask questions.
Ask questions. Learn. Satisfy your curiosity. Ask the what-ifs. Understand your risks. Understand what your role in this is.
Dr. Siegel, TPS: One of my favorite questions that my doctor asked me was, “What’s really important for me to know about you to take good care of you?” And I told him, “I love being a mom, I love playing guitar, and I love running.” The lung toxicity [was] really important to me. Neuropathy, which is really important. Knowing that was a key part of knowing how to take good care of me because we watch out for nerve issues, for trouble breathing, and things that could really impact my quality of life.
Dr. Matasar: Sounds like a wonderful oncologist.
Dr. Siegel, TPS: Absolutely. Thanks so much for taking [the] time to chat with The Patient Story. We’re so lucky.
Dr. Matasar: It’s my privilege. There’s nothing more important than this piece of things. What we do is about our patients, their caregivers, [and] their loved ones. This is all it’s ever about so the opportunity to share my thoughts is an honor.





