Endometrial Cancer: Know Your Treatment Options
Discover the Latest Developments Used to Treat Advanced or Recurrent Endometrial Cancer
Edited by:
Katrina Villareal
Patient advocate Tiffany Drummond and gynecological cancer expert Dr. Brian Slomovitz of the Mount Sinai Medical Center in Miami, Florida, discuss the latest treatments for endometrial cancer.
Develop a comprehensive understanding of advanced and recurrent endometrial cancer, enhancing your knowledge about the disease’s progression and challenges. Learn about the current treatment protocols and how they offer hope and recovery to patients dealing with this severe form of cancer.
Explore how immunotherapy is transforming the treatment landscape, providing new avenues for potentially more effective and personalized care. Discover cutting-edge developments in the field, including promising clinical trials that could offer new hope and treatment options for patients. Gain insight into advances in robotic surgery, including techniques using the da Vinci Surgical System, which offers precision and reduced recovery times.
- Introduction
- What is Endometrial Cancer?
- Current Treatments for Endometrial Cancer
- Advanced & Recurrent Endometrial Cancer
- Biomarkers in Endometrial Cancer
- Highlighting Endometrial Cancer Clinical Trials
- Maintenance Therapy Options in Endometrial Cancer
- Endometrial Cancer Treatment Side Effects
- Diversity, Equity & inclusion (DEI) in Cancer Trials
- Setting Expectations for a Patient’s Clinical Trial Experience
- Requirements and Responsibilities of a Clinical Trial
- Improving Diversity in Clinical Trials
- June is Uterine Cancer Awareness Month
- Final Takeaway
Introduction
Stephanie Chuang, The Patient Story Founder
Stephanie Chuang: I’m the founder of The Patient Story and a cancer survivor. Mine was non-Hodgkin lymphoma. During that time, I realized how important connection was and that became the genesis of The Patient Story. This multi-channel community seeks to connect, educate, and empower patients and care partners. We do this primarily through in-depth patient story videos and educational programs with a thread of self-advocacy, asking questions, and sharing more about what you’re experiencing with your medical team, which is so important in cancers, especially like endometrial cancer where it’s critical people understand what is available to them and what to ask their doctors.
The Patient Story retains full editorial control of all content. While we hope you walk away with more understanding, this discussion is not meant to be medical advice or a substitute for your medical care.


The discussion will be moderated by Tiffany Drummond, who has more than 15 years of experience as a clinical research professional. Tiffany lost her mother Leonora Jean Drummond to endometrial cancer in 2016 and ever since, her mission has been to promote women’s health and wellness. Tiffany works with ECANA, the Endometrial Cancer Action Network for African-Americans, which is incredible in helping to create community.
Tiffany Drummond, Patient Advocate
Tiffany Drummond: As a clinical research educator, I’ve been doing hematology-oncology research for about 20 years, and most importantly, I’m a patient advocate and daughter of someone who I lost to endometrial cancer.
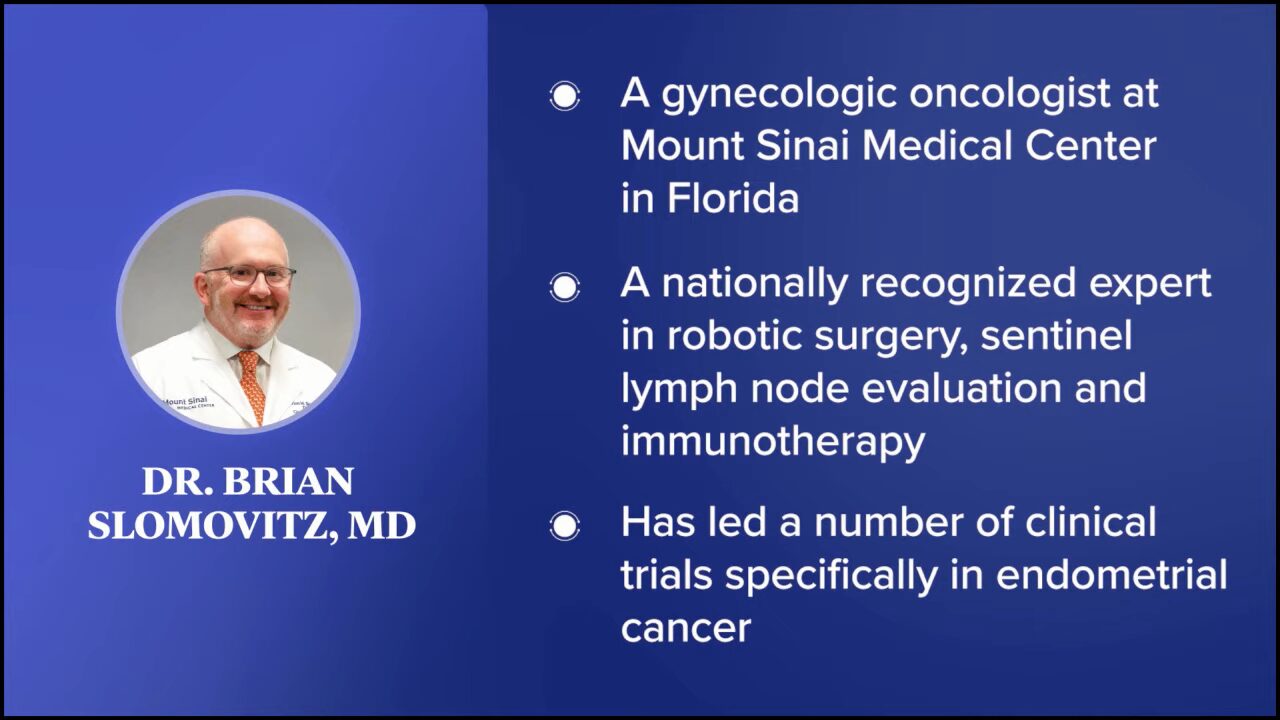
Dr. Brian Slomovitz, Gynecologic Oncologist
Tiffany: Dr. Brian Slomovitz is a gynecologic oncologist at Mount Sinai Medical Center in Florida. He’s a nationally recognized expert in robotic surgery, sentinel lymph node evaluation, and immunotherapy, and has led a number of clinical trials specifically in endometrial cancer. Dr. Slomovitz, what drew you to this field?
Dr. Brian Slomovitz: When I was thinking about which specialties to go into, I enjoyed surgery. I also enjoyed the why and the how of things and what we can do for the complete care of our patients not just surgical management, medical management, or preventative management.
As a gynecologic oncologist, I focus on complete patient care, including prevention or early diagnosis, initial treatment options, cure, and survivorship. I also focus on how to manage recurrent and advanced disease, improving one’s quality of life while trying to control cancer, and ultimately leading a woman through her disease course.
For me, it’s promising and rewarding. One of the things that was introduced to me in this area is clinical research and the importance of research in offering the best care for our patients.

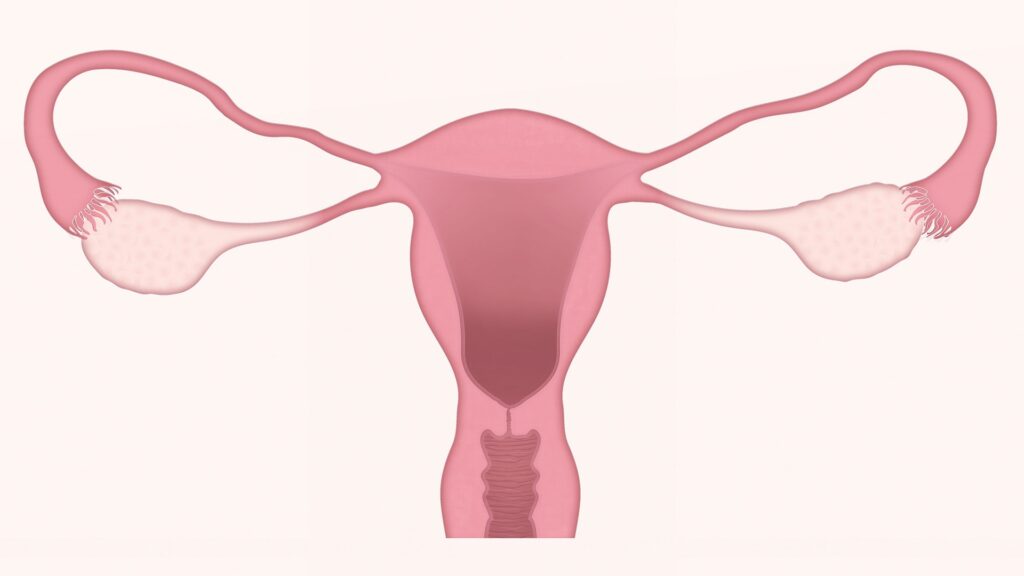
What is Endometrial Cancer?
Tiffany: What is endometrial cancer?
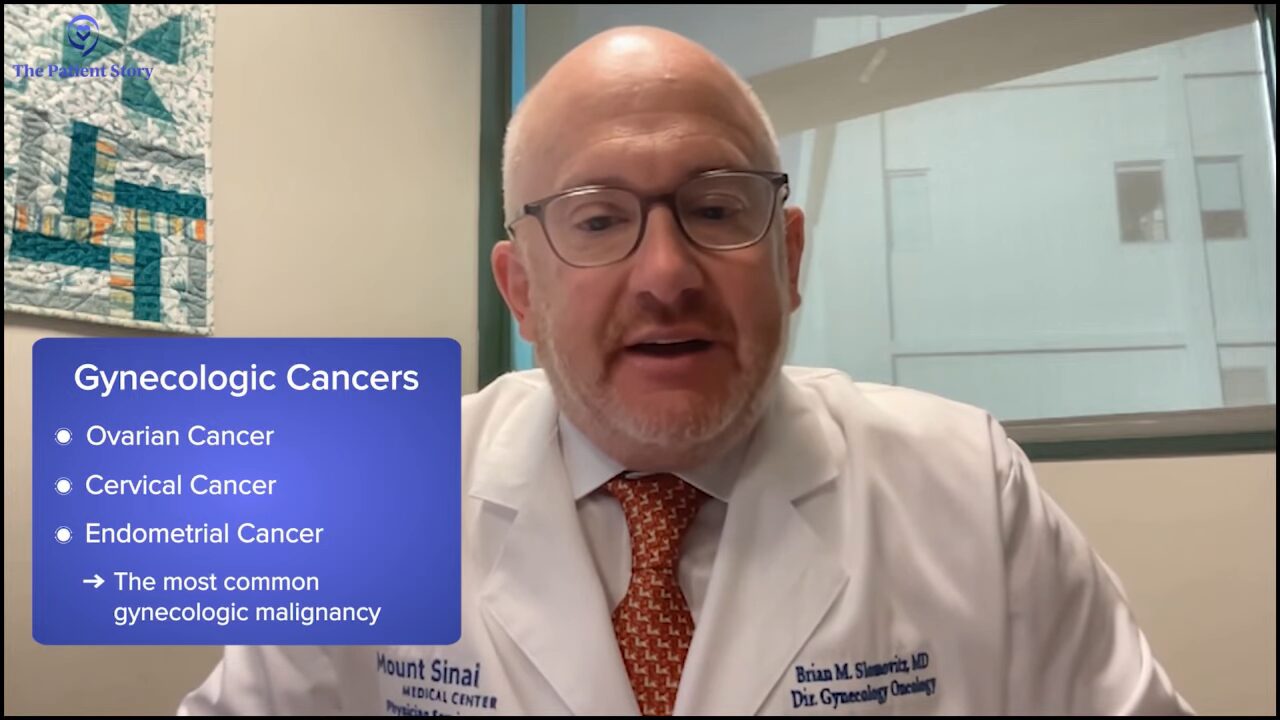
Dr. Slomovitz: In gynecologic oncology, we deal with three major types of cancer: ovarian cancer, cervical cancer, and endometrial cancer. Endometrial cancer is the most common gynecologic malignancy. It’s much more common than ovarian cancer and cervical cancer.
Historically, we didn’t think about it as much because most women with endometrial cancer do well from their disease and will die of something else. But as we focus more attention on it, we’re learning that endometrial cancer has a subgroup of patients with metastatic or recurrent disease that represents an unmet need. We need to come up with better treatment options for them and that’s what I’m focusing a lot of my time on.
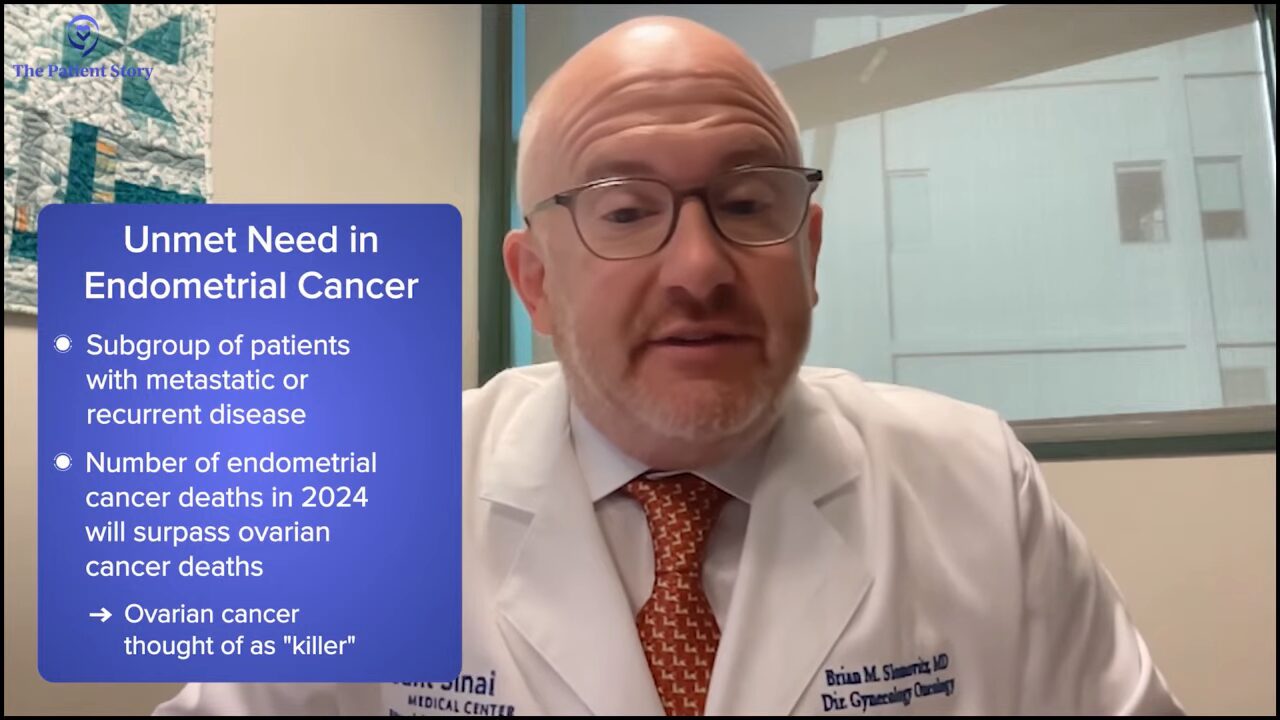
In 2024, the number of deaths from endometrial cancer will outnumber the deaths from ovarian cancer, which highlights the unmet need. We need to do better. We always thought about ovarian cancer as a “killer.” The fact that there are more deaths from this disease is something that frustrates us and something that we need to do something about.
Symptoms of Endometrial Cancer
Dr. Slomovitz: Abnormal bleeding is a symptom of endometrial cancer. A lot of times, people think it’s postmenopausal bleeding, which is true if you’re in menopause and have spotting. It would be best if you had an appropriate workup with a provider who does gynecologic exams. Some people see their family practice doctor or primary care doctor, but it’s important to see a gynecologist or someone who does gynecologic exams, which would include an endometrial biopsy as well as an ultrasound.
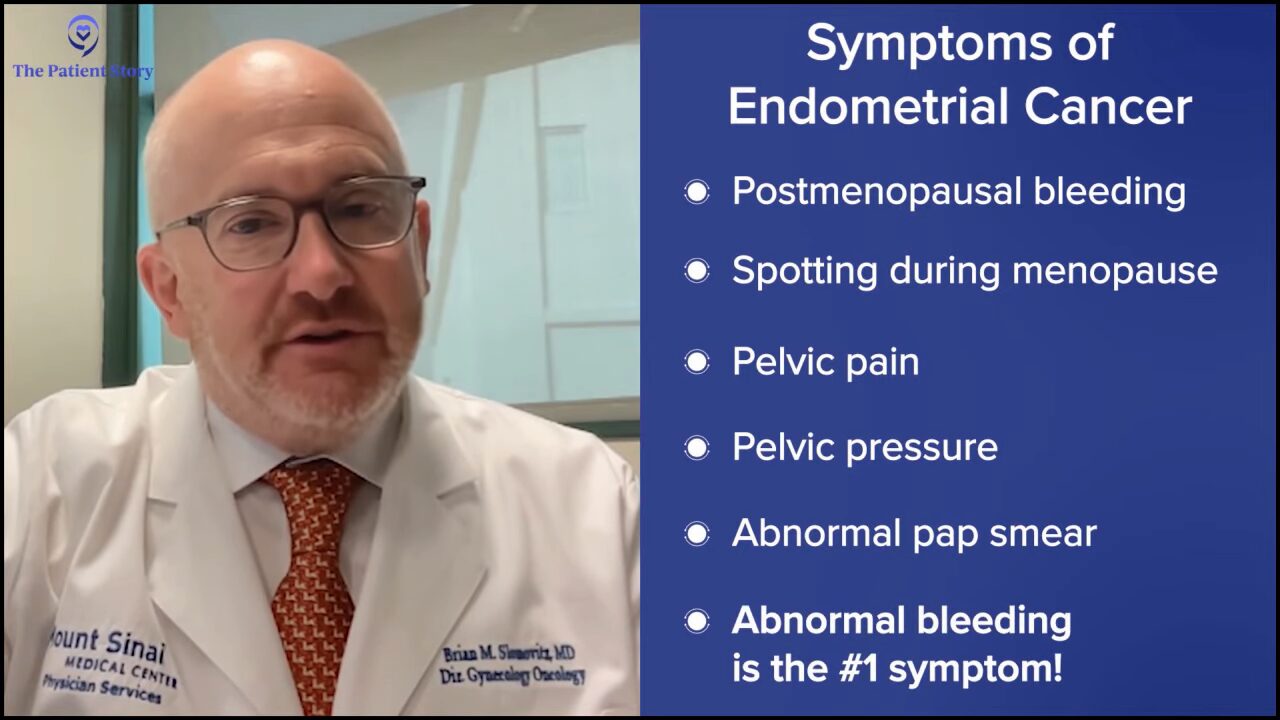
Other symptoms include pelvic pain, pelvic pressure, and abnormal pap smears. Any symptoms that last from 10 days to two weeks or get progressively worse need to get checked. We need to encourage women to see their healthcare provider, but abnormal bleeding is the number one issue that we worry about.
Tiffany: For my mother, it was postmenopausal bleeding and I’m not sure why, but she didn’t think it was something that needed to be looked at. She thought it was normal. I say this for women in general: our GYN care is going to help us throughout our lives. It doesn’t stop when you go through menopause. Always be aware of that.
Current Treatments for Endometrial Cancer
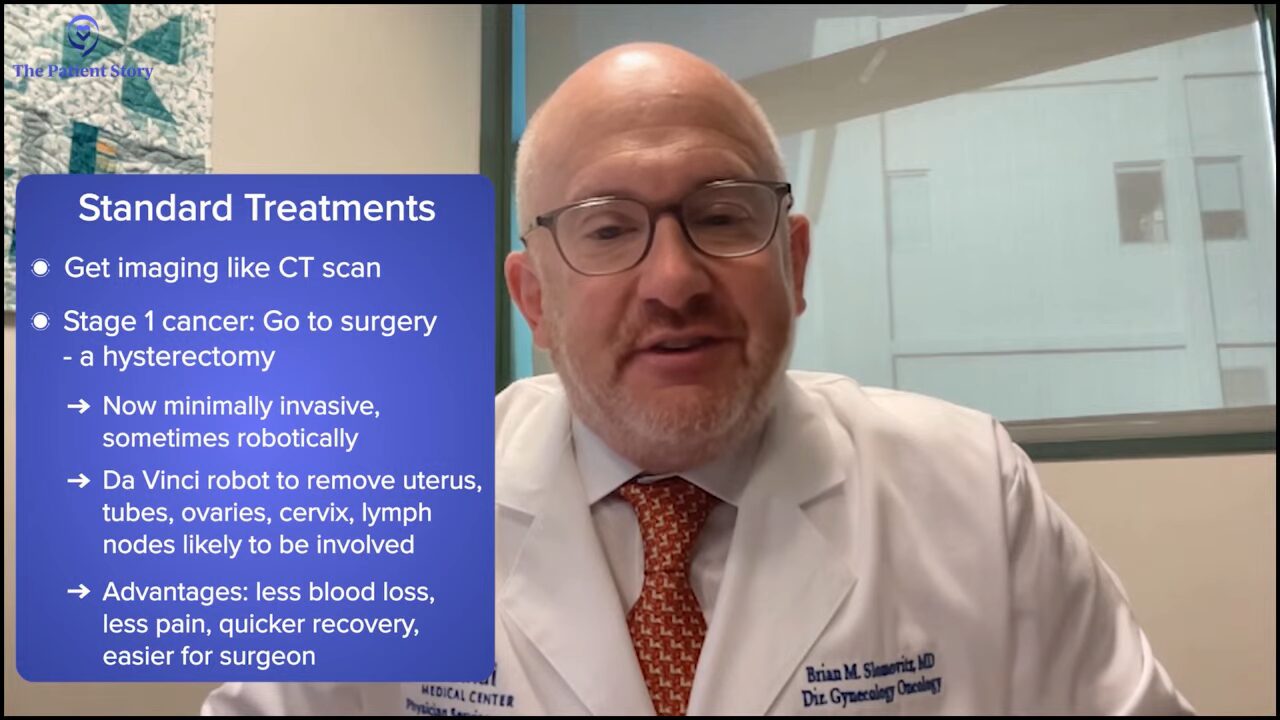
Tiffany: What are the current standard treatments for endometrial cancer?
Dr. Slomovitz: For women who are initially diagnosed, the first step is usually surgery. After we get imaging, like a CT scan, a lot of these patients will have clinical stage 1 disease surgical resection, which is a hysterectomy. Traditionally, we did these with an up-and-down incision. Patients would be in the hospital for a long period of time. Now we’re doing most things minimally invasive.
I do mine robotically with a da Vinci robot. We’ll remove the uterus, the tubes, the ovaries, and the cervix. The advantage there is less blood loss, less pain for the patients, and a quicker recovery. It’s a little easier for the surgeon too, which I don’t mind. It’s best for our patients. They can go home the same day or the next day.
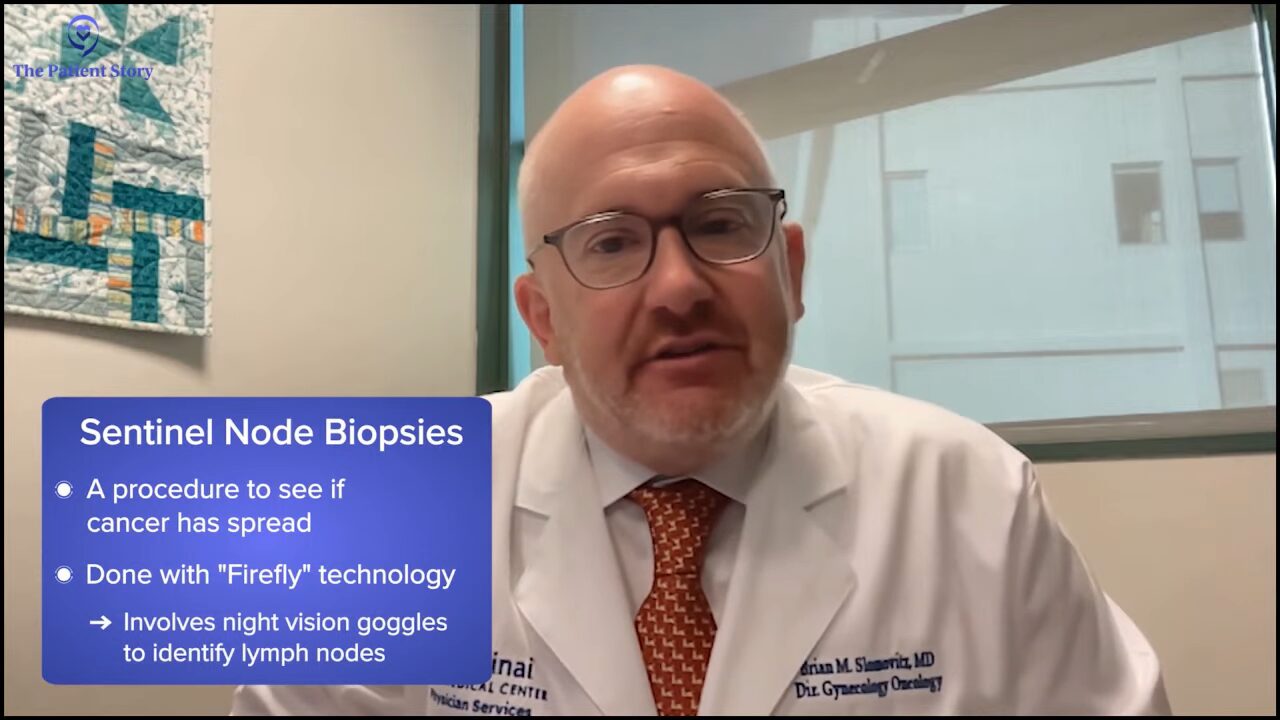
We do a sentinel lymph node biopsy using the Firefly technology. It’s like using night vision goggles to identify nodes that are most likely involved.
Tiffany: I’m so glad that these advancements exist.
Advanced & Recurrent Endometrial Cancer
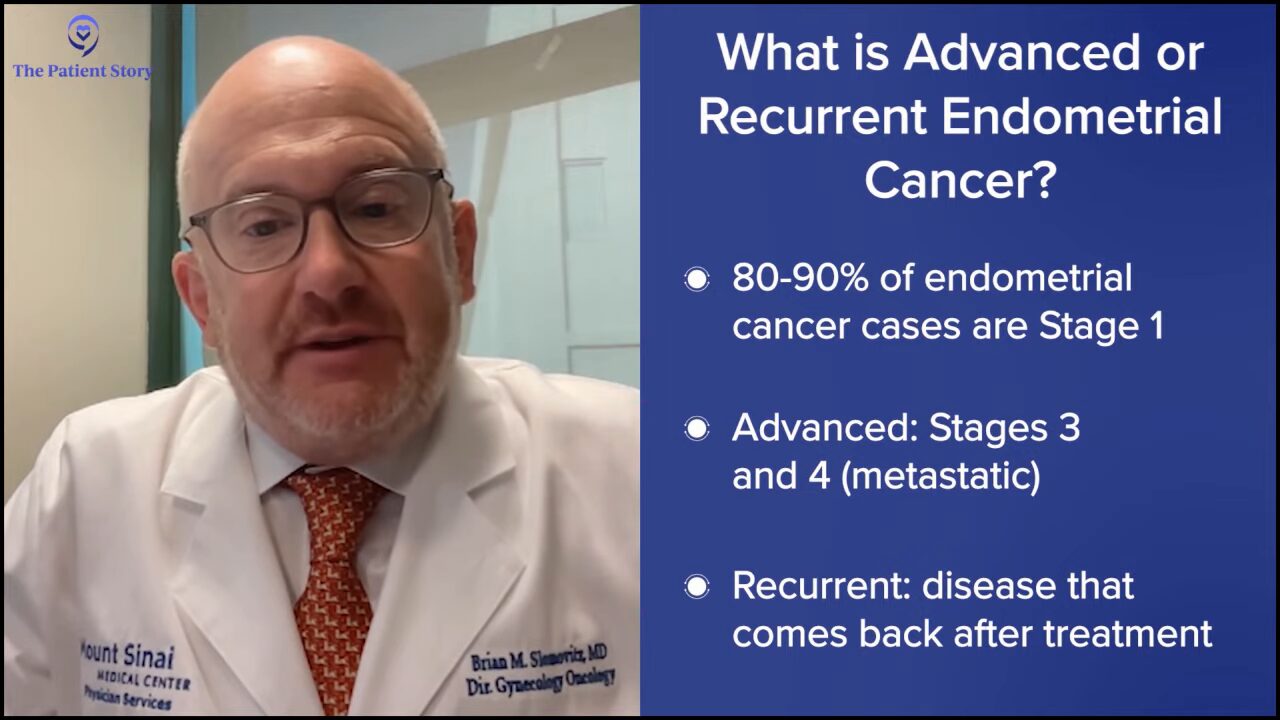
Tiffany: My mother had recurrent endometrial cancer and was diagnosed at stage 3. Can you talk to us about recurrent and advanced endometrial cancer and the current options for them? When we say advanced and recurrent, what do they mean in terms of endometrial cancer?
Dr. Slomovitz: Women who are diagnosed with stage 1 endometrial cancer will make up 80 to 90% of the patient population. It’s the patients with advanced disease that we’re worried about. Similar to your mom, lymph node positivity stage 3, widely metastatic disease stage 4, and the subgroup of patients with earlier stage disease that recur represent a diagnostic or treatment challenge and an unmet need.
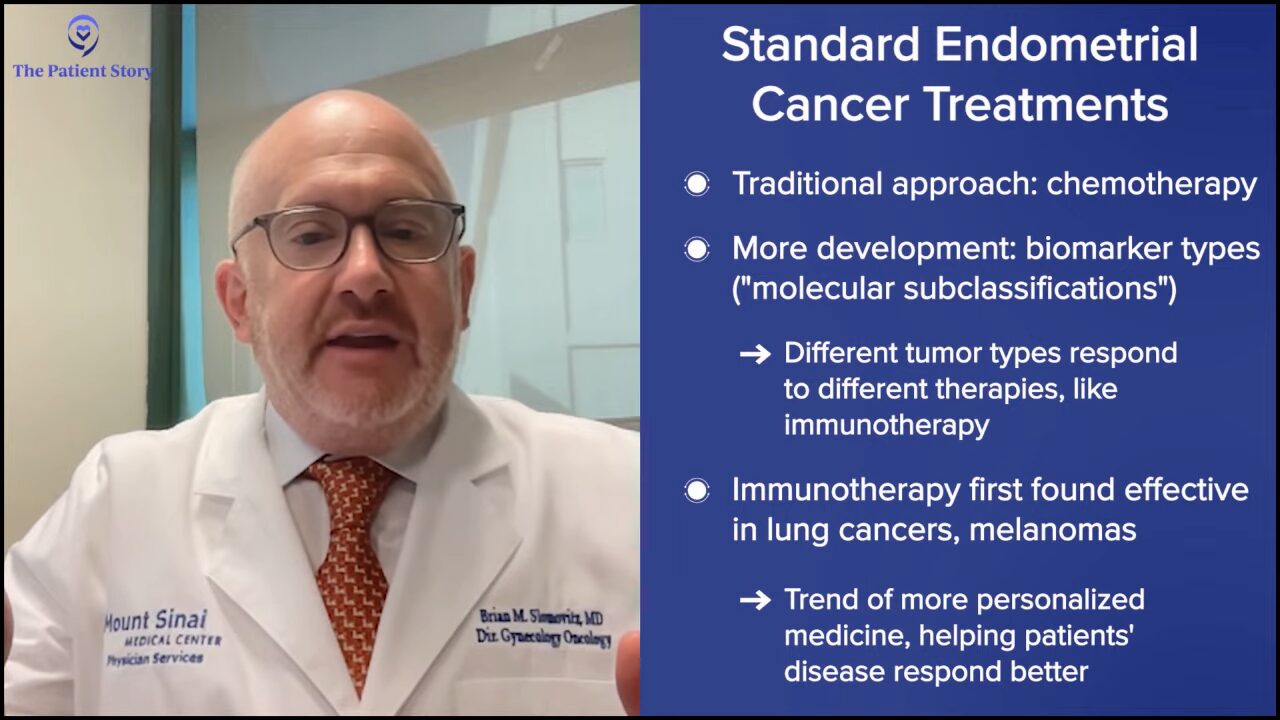
Traditionally, we would use chemotherapy, but as we’re learning more and more about the disease and being able to look at the molecular subclassifications of endometrial cancer, we’re learning that different types of tumors can respond differently to different types of therapies.
Immunotherapy was originally found to work extremely well in non-small cell lung cancers and melanomas. When we learned more about endometrial cancer, not only did we find that there’s activity of immunotherapy in endometrial cancer, but there are distinct subgroups within patients with recurrent or metastatic disease that respond more favorably to immunotherapy. Those are areas that we need to exploit, taking knowledge that we have, and then pushing that forward into the clinical setting.
Not all patients are the same. We need to offer more unique, personalized medicine, and to do so, we need to better understand the biology of the disease to execute a better treatment strategy.
Biomarkers in Endometrial Cancer
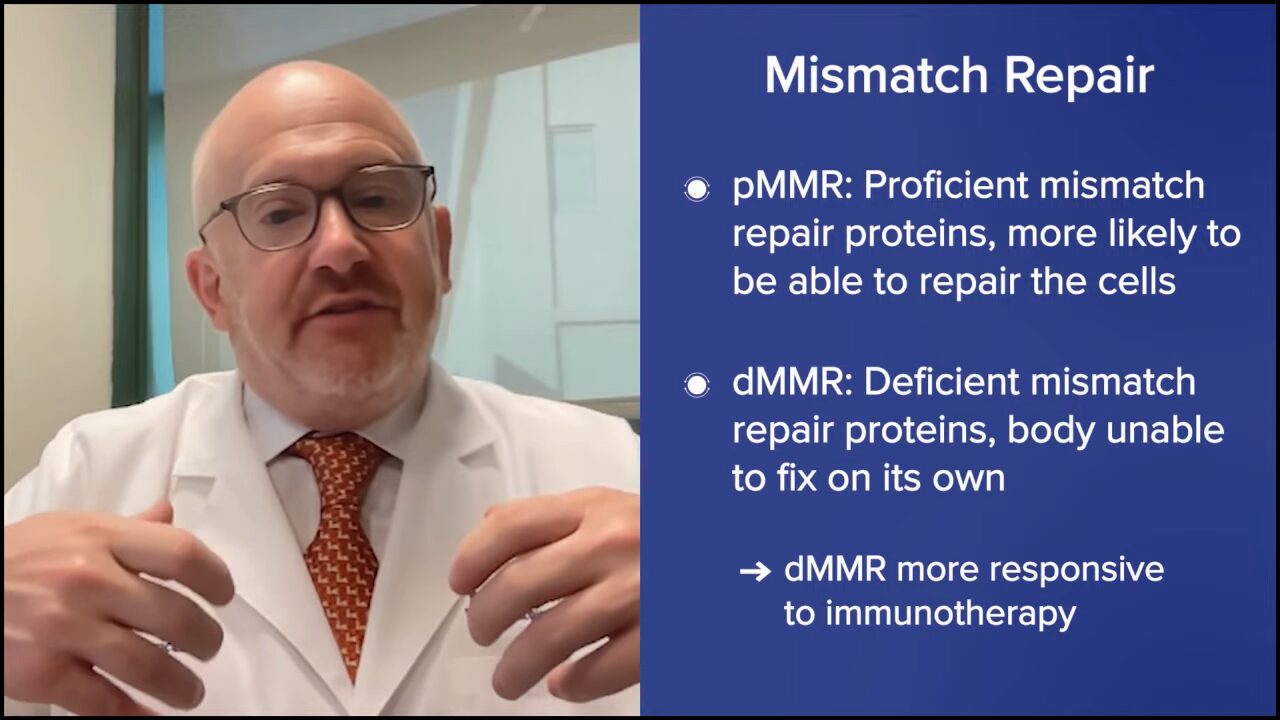
Tiffany: We’re hearing about biomarkers and a lot of patients are becoming more familiar because they’re being told that they either have or don’t have certain biomarkers. Can you break down the biomarkers dMMR and pMMR and why they are important in guiding treatment decisions for our patients?
Dr. Slomovitz: When cells divide, normally there are errors in the process. Cell division isn’t a perfect process. The body normally recognizes the errors and corrects them. The team of proteins that does this is called the mismatch repair (MMR) proteins. If cells are proficient in mismatch repair proteins, they’re more likely to be able to repair those cells and move forward. That’s pMMR.
The dMMR is a different subgroup deficient in mismatch repair proteins. These are the ones that the body’s unable to fix. By not having these “fixed cells” or cells that look normal, these cells look like they shouldn’t be there. They look more like non-self instead of self, so they respond better to immunotherapy.

Immunotherapy is not a poison that we give cells. Immunotherapy is sort of a stimulant of the body’s immune system to fight off something that shouldn’t be there. When we think about tumors or cells that are more responsive to immunotherapy, it’s more of the non-self cells, cells with a high mutational burden, or cells that have some different molecular characteristics. DMMR is more responsive to immunotherapy. PMMR, while they still respond to immunotherapy, they don’t respond as well. We need to treat them differently.
Tiffany: I’m assuming the typical first-line treatment approach is immunotherapy. Are there other alternatives?
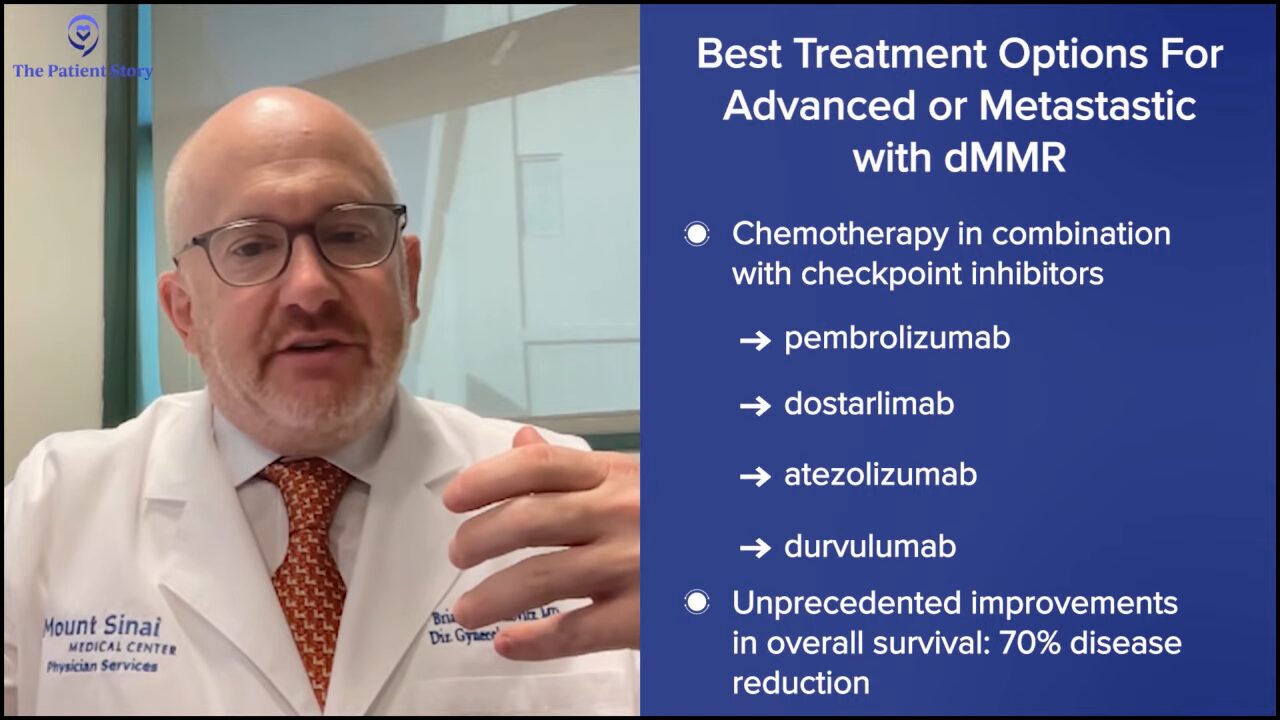
Dr. Slomovitz: For the dMMR population, the best treatment option for patients with advanced or metastatic disease is chemotherapy in combination with checkpoint inhibitors. Over the last year and a half or so, we’ve had landmark trials looking at drugs including pembrolizumab, dostarlimab, atezolizumab, and durvalumab, which are all checkpoint inhibitors. Given in combination with chemotherapy, they have shown unprecedented improvements in overall survival and progression-free survival in patients with dMMR tumors. There was a 70% reduction, which is remarkable.
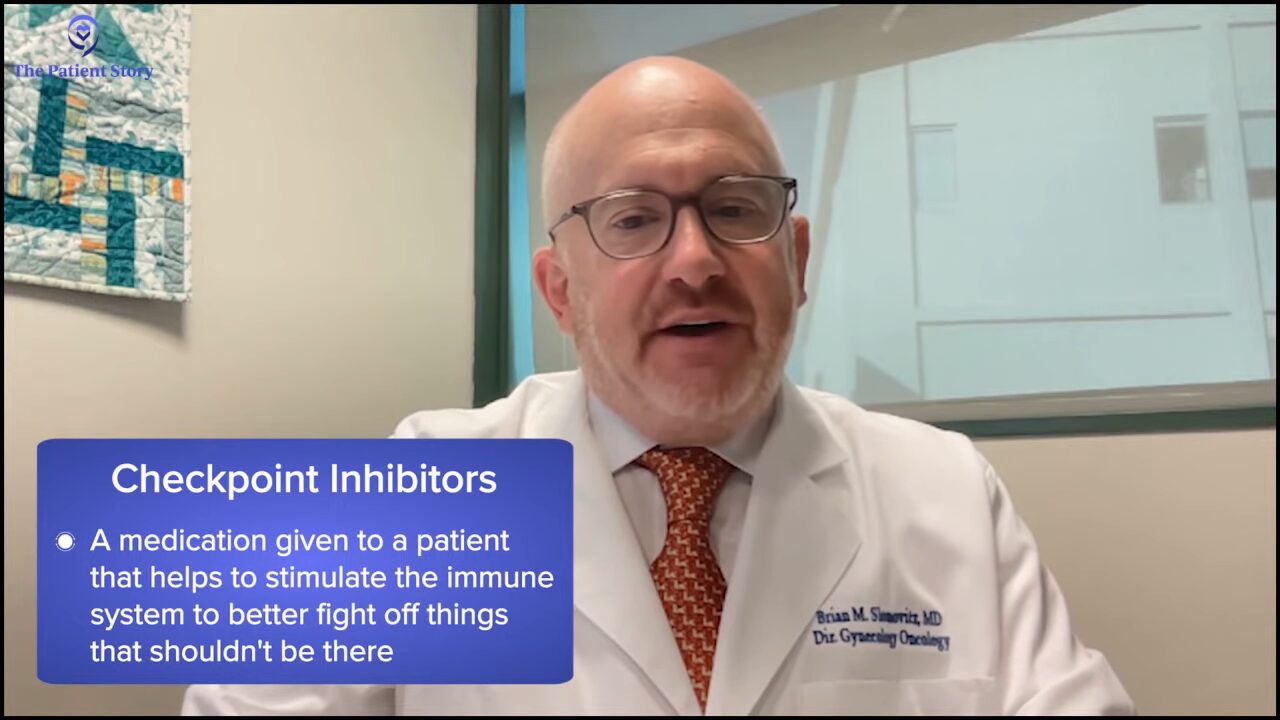
Tiffany: What is a checkpoint inhibitor?
Dr. Slomovitz: A checkpoint inhibitor is a medication given to a patient that helps to stimulate the immune system to better fight off things that shouldn’t be there. When we give it to a patient to attack a tumor, the dMMR tumors are recognized by the body as something that shouldn’t be there more than the pMMR tumor, so that’s why checkpoint inhibitors work better in that setting.
Highlighting Endometrial Cancer Clinical Trials
Tiffany: Let’s talk about the changing treatment landscape. Immunotherapy is likely to become a more common treatment for women with advanced endometrial cancer. Following the results of these clinical trials that you were talking about, can you talk more about this and what these breakthroughs were with these results?
Dr. Slomovitz: The initial results showed that giving immunotherapy with chemotherapy works better. As we move forward, what we’re focusing on is to see if we can give combinations or single agents in the first-line setting before chemotherapy to eliminate the use of chemotherapy but to get the same effectiveness.
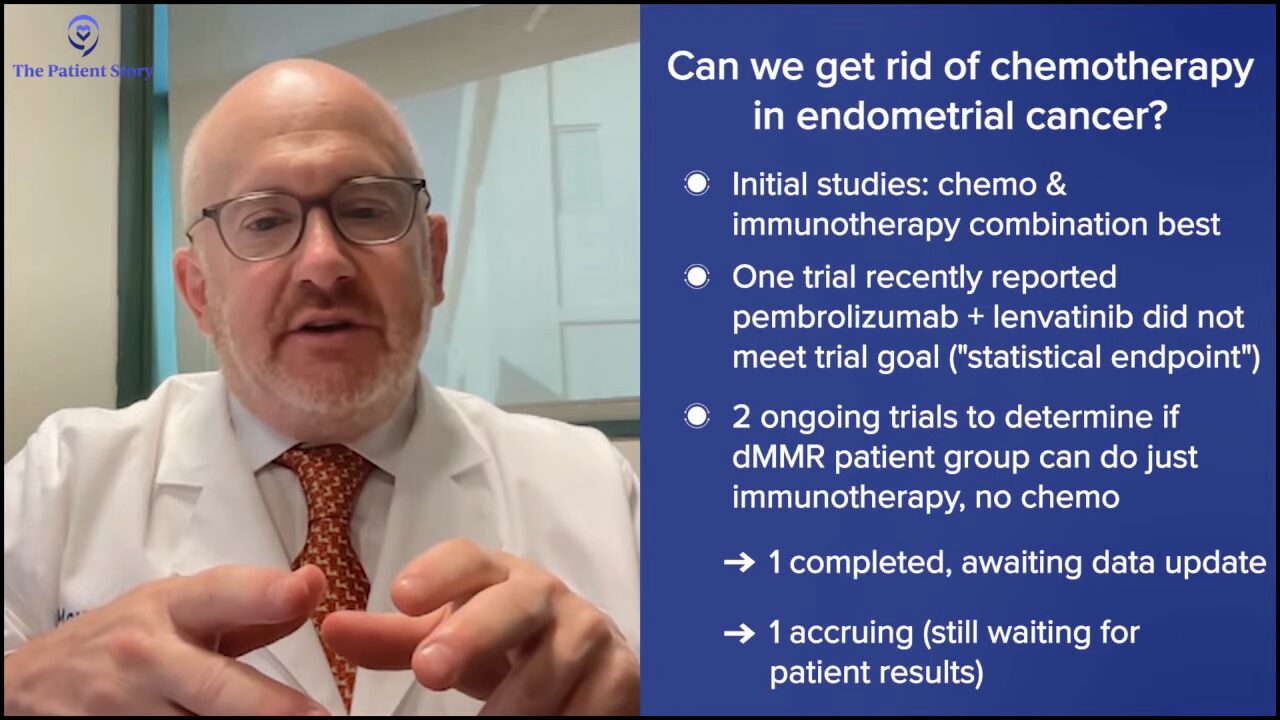
Recently reported was one trial looking at a combination of pembrolizumab and lenvatinib in the first-line setting. That didn’t meet its statistical endpoint, but that looked at all comers, pMMR and dMMR.
There are two ongoing trials now: one’s completed accrual but hasn’t read out and one’s still accruing, looking specifically at the dMMR population to see if a checkpoint inhibitor alone can work in those patients. I’m the global lead on one of those. We’re looking at pembrolizumab in patients with dMMR tumors and comparing it to chemotherapy to see if we can get rid of chemotherapy for that population. Now if we can, it’ll be amazing.
Tiffany: Very promising. This is why I’m such a proponent of clinical research and increasing diversity and participation, so we can get good data.
Tiffany: Let’s talk about adding immune checkpoint inhibitors, like pembrolizumab and dostarlimab. What is the conversation about this becoming the new standard first-line treatment for advanced or recurrent endometrial cancer patients with dMMR tumors? Is this something that needs more research or more data to fully understand the scope?
Dr. Slomovitz: I would say with certainty that for the dMMR population, unless there’s a contraindication to immunotherapy checkpoint inhibitors, those patients deserve or should get checkpoint inhibition as the standard of care based on the promising results. It’s not as much of a slam dunk for pMMR, but for the dMMR population, treatments should include a checkpoint inhibitor, without a doubt.
Maintenance Therapy Options in Endometrial Cancer
Tiffany: Let’s talk about some clinical trials that are actively enrolling in the advanced and recurrent setting, with late-stage endometrial cancer, such as selinexor as a first-line maintenance therapy. What trials are ongoing that people can learn about and be eligible for?
Dr. Slomovitz: In addition to leading the division of gynecologic oncology at Mount Sinai Medical Center in Miami Beach, I also serve in the GOG Foundation and lead the uterine cancer clinical trial portfolio. In that capacity, we have a lot going on in uterine cancer, which is exciting. Wearing my Mount Sinai hat, we’re excited that most of those trials are opened up at Mount Sinai.
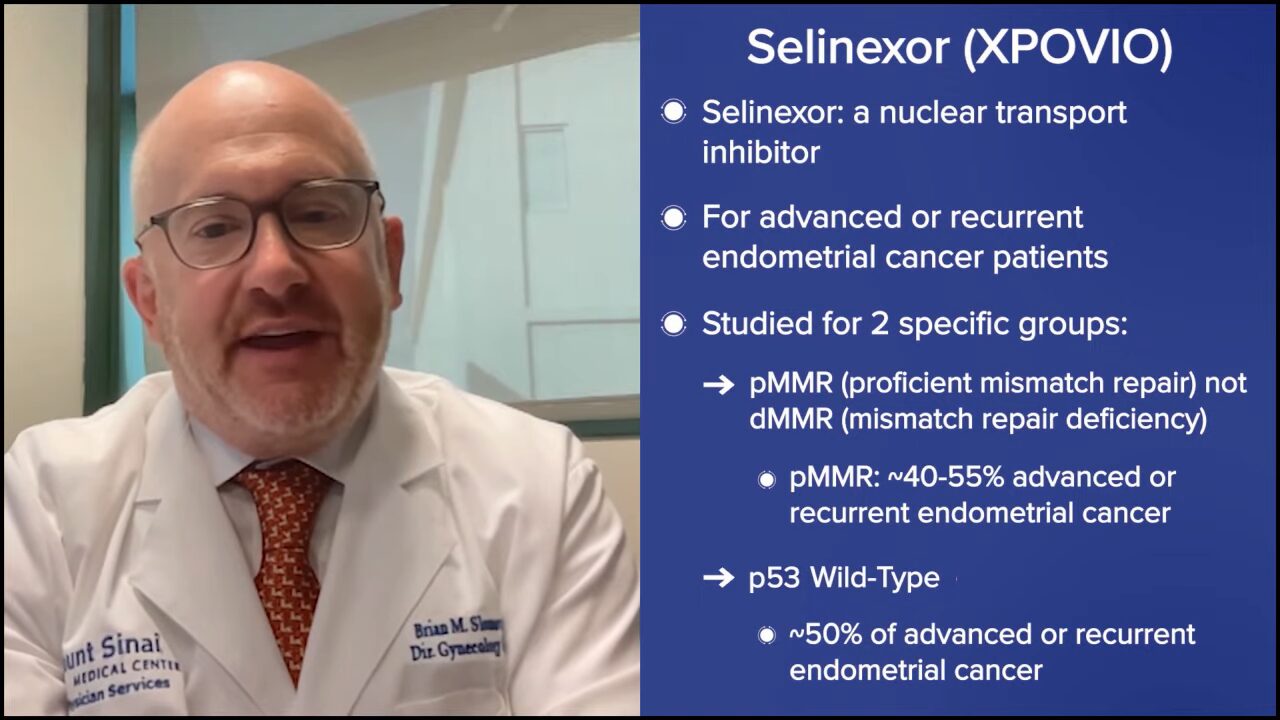
Selinexor is a nuclear transport inhibitor. This is for pMMR, most likely p53 wild-type, which is a biomarker in the cell. The trial doesn’t require pMMR but knowing that they get checkpoints, it’ll probably all end up being the pMMR population. Chemotherapy versus chemotherapy and maintenance selinexor.
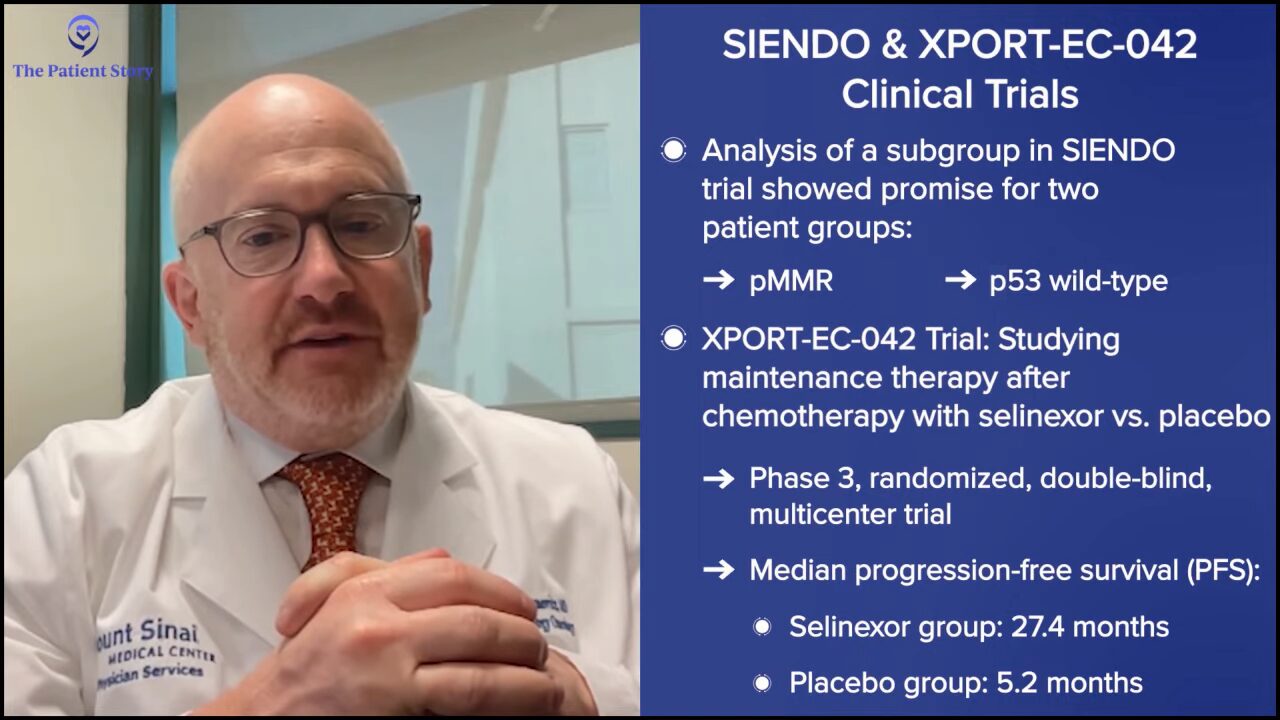
Now we did the preliminary trial, called the SIENDO trial, where we looked at all comers, whether they’re p53 wild-type or mutated, and found that the primary outcome didn’t benefit the selinexor group. But if we did a subgroup analysis, if we looked at patients with p53 wild-type tumors, there was a big difference in outcomes. Outcomes improved in patients treated with selinexor.
We then went to the FDA and said, “Wow, look at this outcome. This will be better for our patients.” The FDA agreed, but appropriately, they said we needed to do a separate study looking at that to see if it works and that’s one of the trials that we have open accruing globally. It’s called the XPORT-EC-042 trial. We’re looking to see specifically in chemo-naive, p53 wild-type patients if adding selinexor can help improve outcomes.
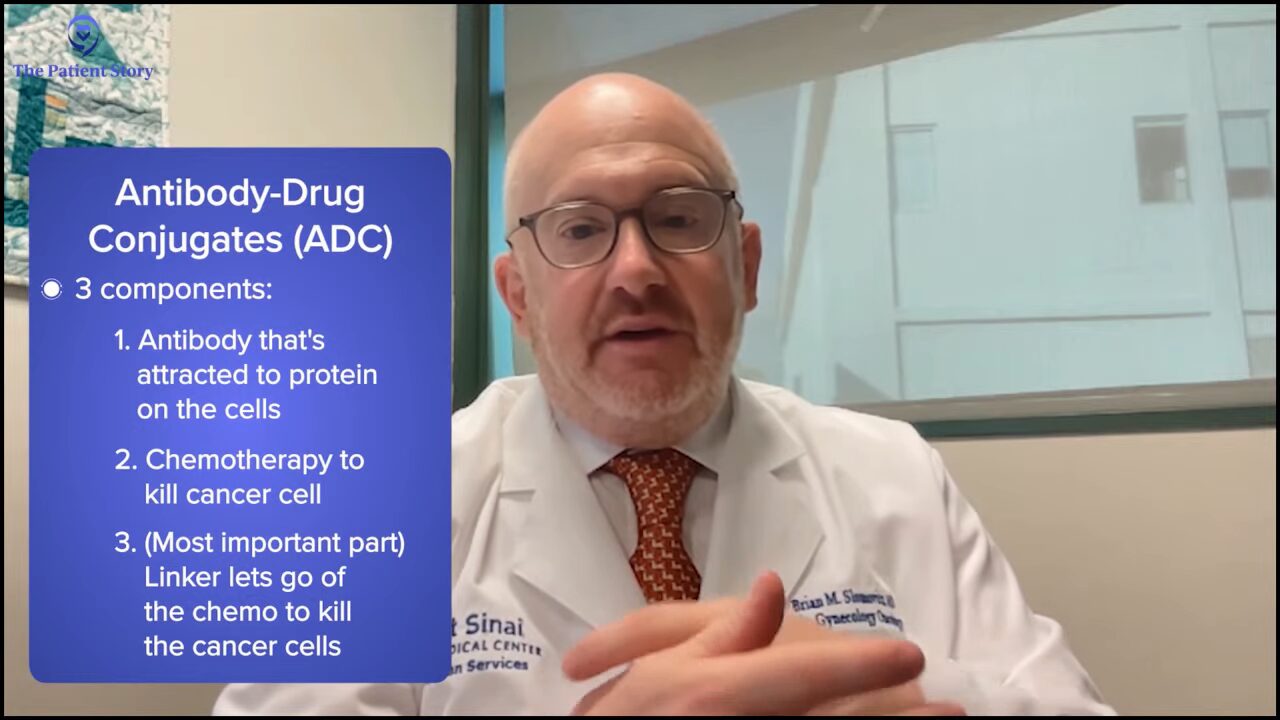
Other areas are taking off in endometrial cancer. There’s a class of drugs called antibody-drug conjugates (ADCs), which is a novel class of drugs. They have three components. They have an antibody that’s attracted to a protein on the tumor cells. Then there’s a chemotherapy kill, the part that helps kill the cell. The third and most important part is the linker.
When the drug is given, it travels throughout the body and only goes to the cancer cells because of the antibody-protein interaction. Once it gets there, the linker lets go of the chemotherapy, which then goes in and kills the cells.
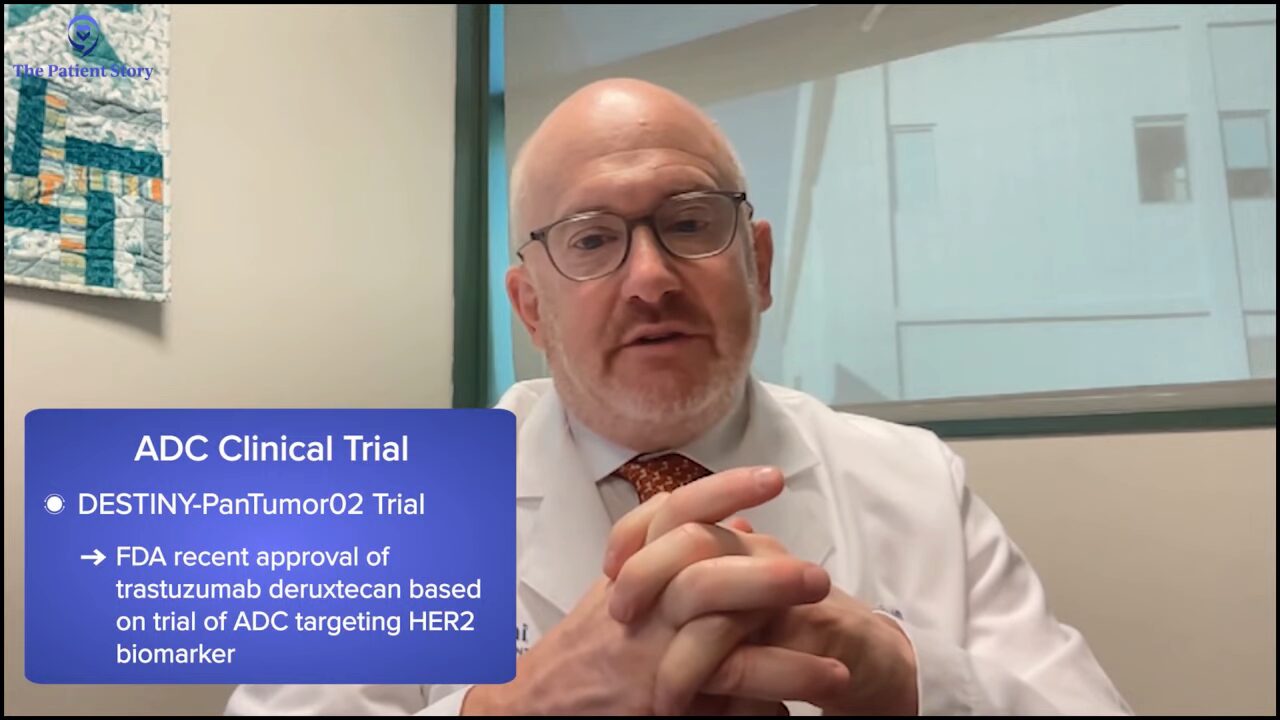
In endometrial cancer, we recently got FDA approval in all comers for trastuzumab deruxtecan (T-DXd) based on the DESTINY-PanTumor02 data, which is an ADC that’s attracted to the HER2 protein on tumor cells. That had unprecedented response rates in the recurrent setting.
Tiffany: We have a lot going on in the clinical research world with endometrial cancer. I’m so excited because it wasn’t always as robust, so I’m glad to see researchers taking steps to improve that.
Endometrial Cancer Treatment Side Effects
Tiffany: Let’s talk about clinical trials in terms of side effects. We know that a lot of these drugs are toxic and have a lot of side effects.
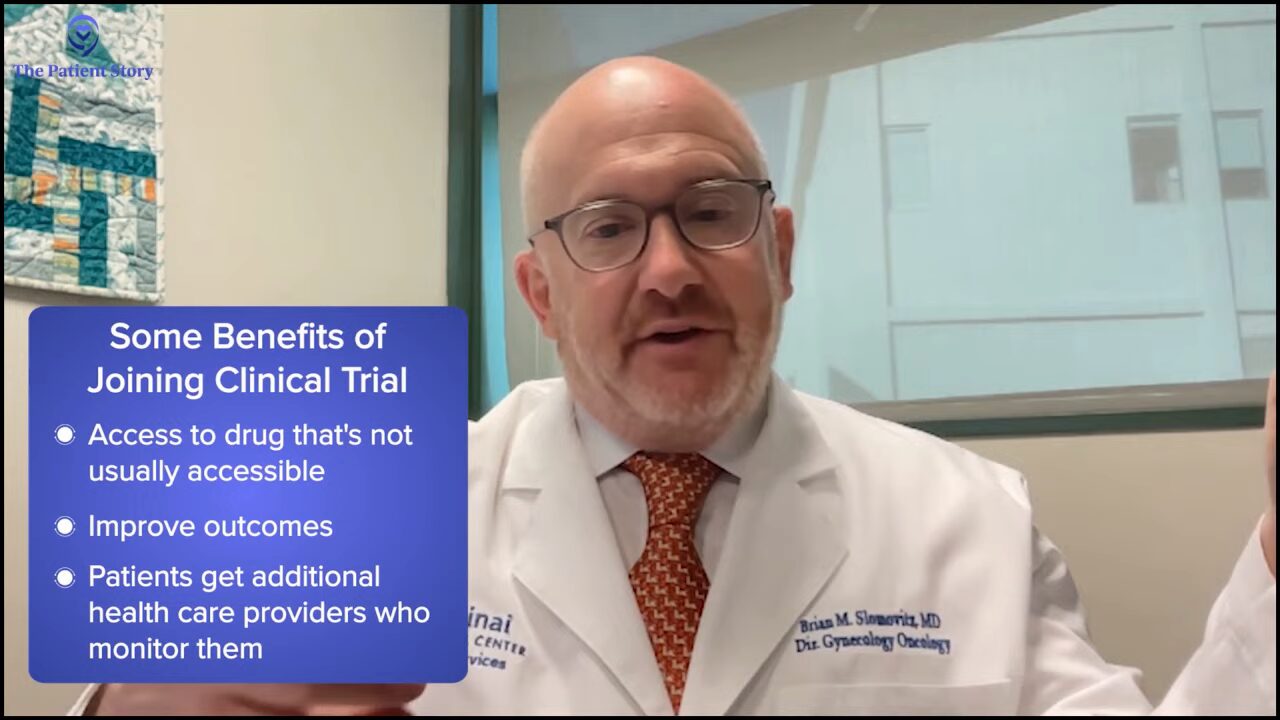
Dr. Slomovitz: Clinical trials allow patients to get a drug that they normally wouldn’t be able to get, which hopefully, improves outcomes. New drugs can have new side effects that we need to be aware of. One of the things that I talk to my patients about when they go on a clinical trial is they get two teams of healthcare providers following them. It’s not only me and my team with our nurse practitioners and nurses, but the whole clinical research team.
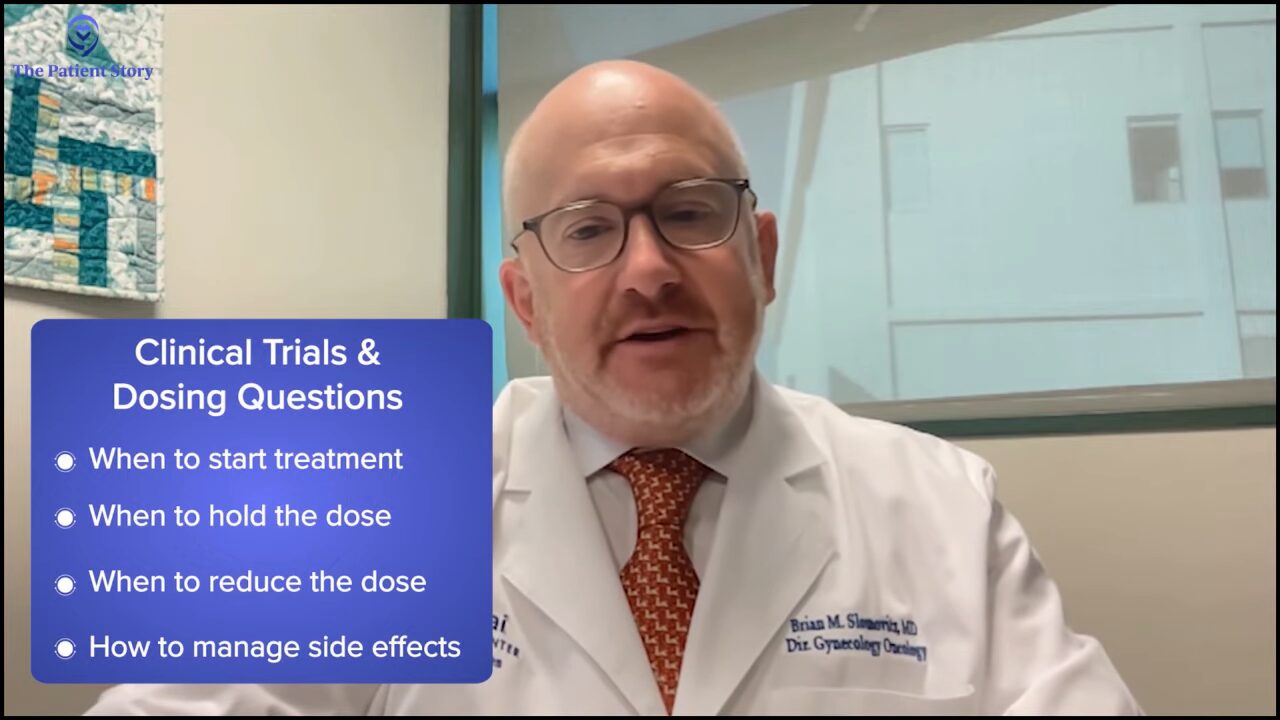
Clinical research is like following a cookbook. To get FDA approval, we try to make treatment as homogeneous as possible without a lot of differences. We follow the cookbook to say dosing, when should things start, when to hold the dose, when to reduce the dose, how are the side effects being managed, and all those things. Between the research team and the clinical team, we communicate closely with our patients. We follow the side effect profile. We look for new signals.
Tiffany: That’s an excellent point you made. When I listen to the experiences of people in clinical trials, they tend to have the sentiment that they get more comprehensive care because they have this whole team of people including other providers outside of their GYN oncology. One of the benefits of clinical research that I think a lot of people don’t know because they’re afraid to jump into the unknown is that you’re getting looked at a lot more than you probably would.
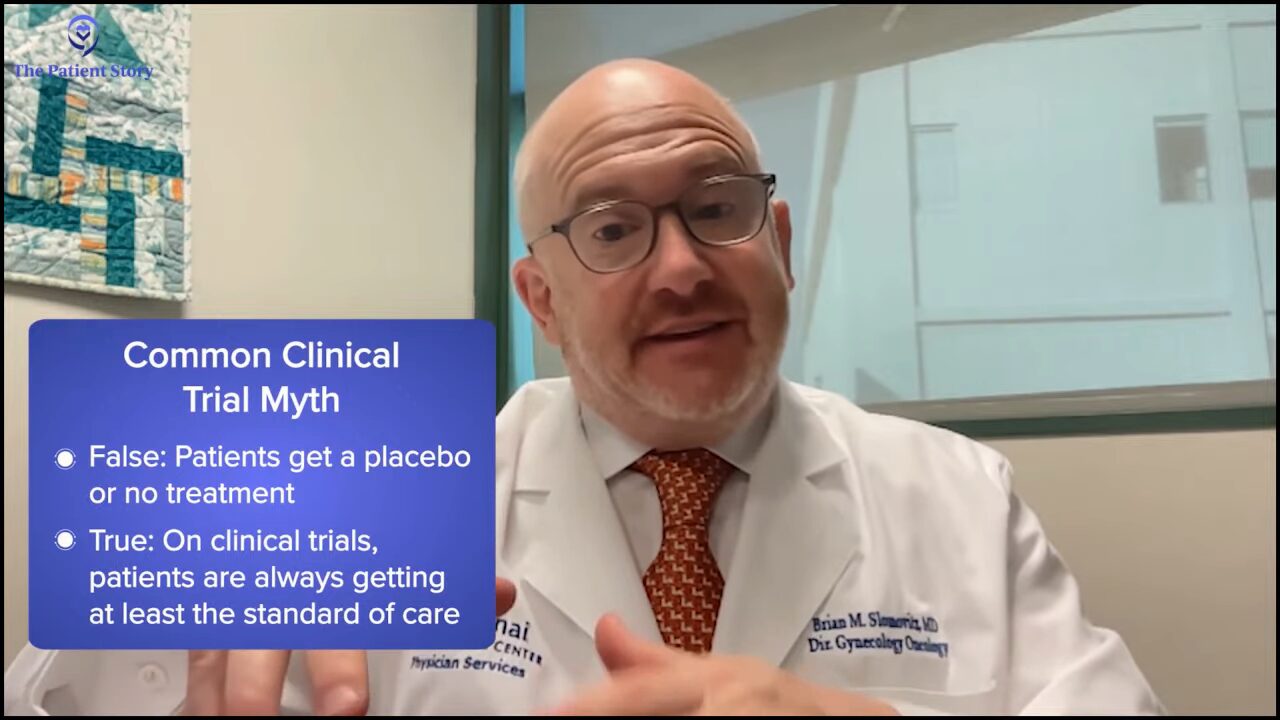
Dr. Slomovitz: It’s important to highlight one of the fears patients have in going on clinical trials is not the side effects they’re going to get; it’s getting a placebo. Whenever patients are on a clinical trial, they’re at least getting the standard of care.
We do not experiment on patients. We do clinical research and study if the new treatment options do better, the same, or worse than the standard of care. Unless the standard of care is observation, we don’t give a placebo. I have to highlight this in every single talk I give.
I don’t want patients to think that if they’re going on a clinical trial, they’re actually getting worse care or they’re being studied incorrectly in a way we did historically. Over the last 20 years, the way we do research in the country has been completely revamped to be ethical, sound, and looking out for the best of our patients. There’s an understanding that we need to do better and make sure we give patients at least the standard of care. We need people to acknowledge that in the research community, we’ve changed. At worst, they’re getting standard of care, but even with the standard of care, they’re getting two teams watching.
Tiffany: I’m so glad that you brought that up. I drive that point home every time I’m talking as well because a lot of patients, specifically on cancer trials, do think that they don’t want to be experimented on. At the minimum, you’re going to get whatever the standard is. Thank you for driving that point home.
Diversity, Equity & inclusion (DEI) in Cancer Trials
Dr. Slomovitz: There’s something that we often mention in the last five minutes of these interviews that needs to be mentioned in the first five minutes. Diversity.
Once you talked about a patient signing on and not getting a placebo, patients need to know that they’re being represented on these trials and that they’re not the only person from their community from coming in on the trial. They’re equally represented. It’s crucial. We need to make sure that the results of the trial translate across different populations.
I’m going to throw the numbers out there, which are disturbing to hear but are facts. Black women are nearly twice as likely to die from endometrial cancer than white women. There’s no other way to say it. We need to do better.
In these research trials, we need to make sure that there’s an appropriate representation of all different diversities for the results to translate to those groups. If we have a clinical trial with 100% white women and it works, that doesn’t mean it’s going to work in Black patients, Hispanic patients, or Asian patients.
We must have this conversation at the beginning of the interview because we have to focus on it. We need to increase the diversity in our clinical trials and then we could ensure not only to get better outcomes but better outcomes across different populations.
Tiffany: A man after my own heart. This is something that I have a personal and professional passion for, increasing diversity in clinical trials and how important it is that when we look at these approvals, it’s representative across populations. The FDA came out with guidance that when you’re submitting investigational new drug applications, you need to have a diversity plan. I hope that researchers and investigators measure their success with that and not simply saying they tried but didn’t make it. Thank you for being a proponent of that.
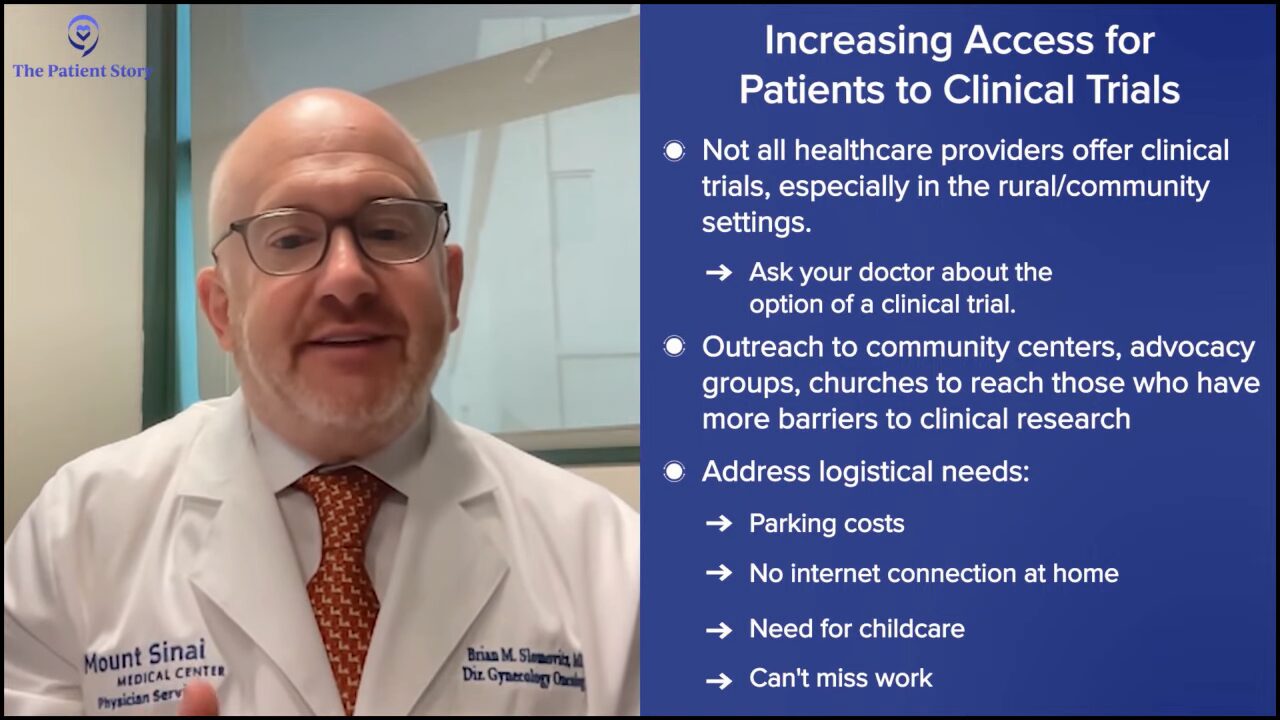
Dr. Slomovitz: Patients need to reach out to their providers to talk about the option of clinical trials. As physicians, we want what’s best for our patients, even if it means taking care of a patient with the best standard of care at the hospital down the street if there’s a clinical trial available. We’re working towards having a community to be able to offer patients clinical trials. Fortunately, we have a lot going on at Mount Sinai Medical Center, which I’m able to offer to our patients.
Making patients aware of clinical trials is important. How do we do that? We have to go into different settings and different areas where we’re not used to. We used to put up a flyer on the wall that said, “Come to the hospital to learn about clinical trials.” We have to understand that certain populations either can’t get to the hospital, don’t want to go to the hospital, or don’t know what’s going on in the hospital. Going out to community centers, advocacy groups, churches, and places like that is extremely important to help overcome those barriers and biases against clinical research.
We don’t realize there’s not only the fear of research but there’s also the practicality of research. For example, sometimes we send our patients a questionnaire to fill out before an online visit. A lot of patients still don’t have access to Wi-Fi, so what do we do about that? Or we ask them to come to the hospital for a three-hour appointment. Who will take care of that person’s children or sometimes their grandchildren when they’re the primary caregiver? What if that person works and if they don’t, they can’t afford dinner? Those are things we need to do better at.
We’re working closely with sponsors to help overcome some of the things that we can overcome. We can’t do everything, but if it means having a sponsor pay for four hours of child care to get a patient on the research, it’s important to do that. The DEI plans that you mentioned include some of these ways to overcome the barriers associated with research to increase diversity, which will make the outcomes of trials better.
Setting Expectations for a Patient’s Clinical Trial Experience
Tiffany: Hearing the word “research” can be scary, but what can someone who has endometrial cancer expect when they go on a clinical trial?
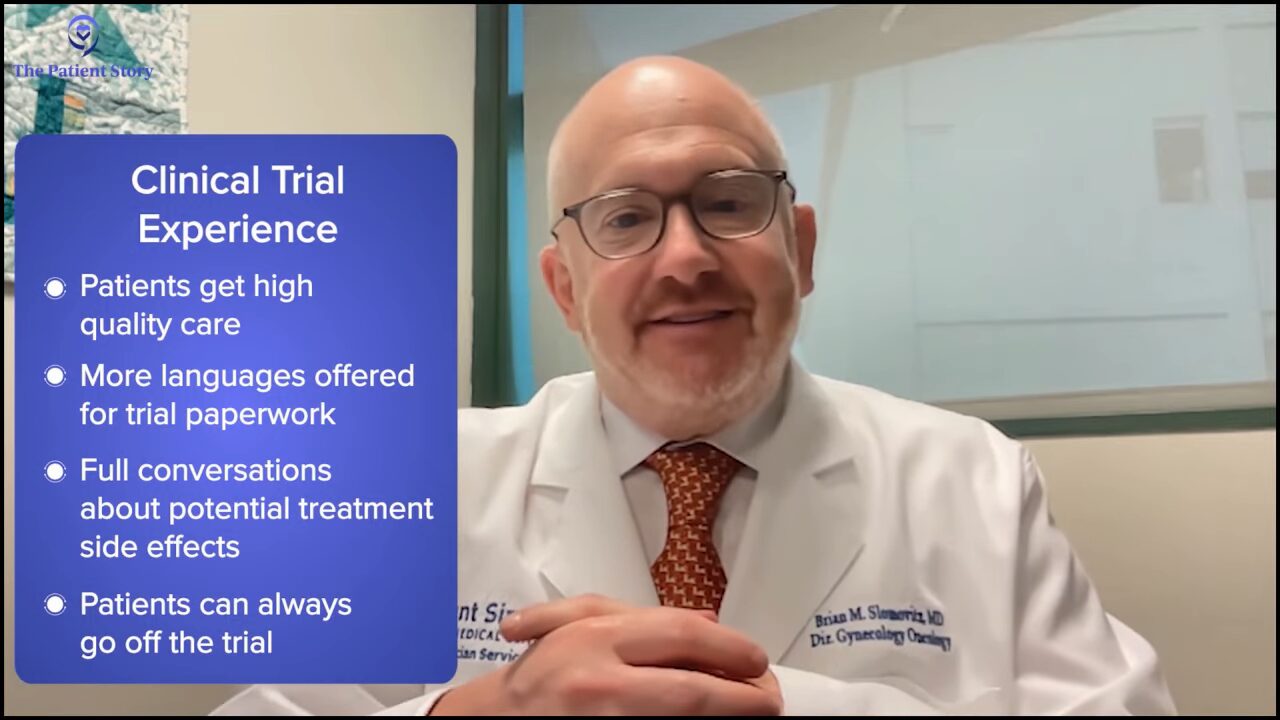
Dr. Slomovitz: There needs to be an understanding that they’re going to get at least the best care if not better care than they would get off a clinical trial. They need to be comfortable in the environment.
Here in Miami, much of the population doesn’t speak English, so we need to educate patients about clinical trials in their language as best as we can. The cold comfort is the fear of the word research and fear of not being able to understand the information, so all of our consent forms and patient information are offered in multiple languages.
They need to understand that they’re watched closely. They may have some side effects that we’re not expecting, but just the same, they may have some outcomes that we’re not expecting either.
They need to know that it’s not a lifelong sentence. Part of the consenting process is if they decide to back out, they could back out. We’re not here to force people to do anything. We’re here to recommend. We’re not here to be paternalistic. Patients sometimes ask, “What would you do if it’s your family?” We’re honest with them about that, but we need to make it an experience that patients appreciate.
There are better rewards than a patient not responding to a trial, but a patient who’s not responding to a trial who says, “Doc, what’s next? What’s the next clinical trial for?” That means we’re doing a good job in offering that patient a trial. We knocked down barriers and that’s a patient who wants to do the best for herself.
Tiffany: I do tell people who are thinking about participating in a trial as well that they’re not only doing it for themselves, they’re doing it for future patients. If we’re altruistic, then participating in clinical trials is one thing that we can do to help others.
Requirements and Responsibilities of a Clinical Trial
Tiffany: Let’s talk about the actual procedures and tests that are done. People might be surprised that they already get these done anyway. What can someone expect?
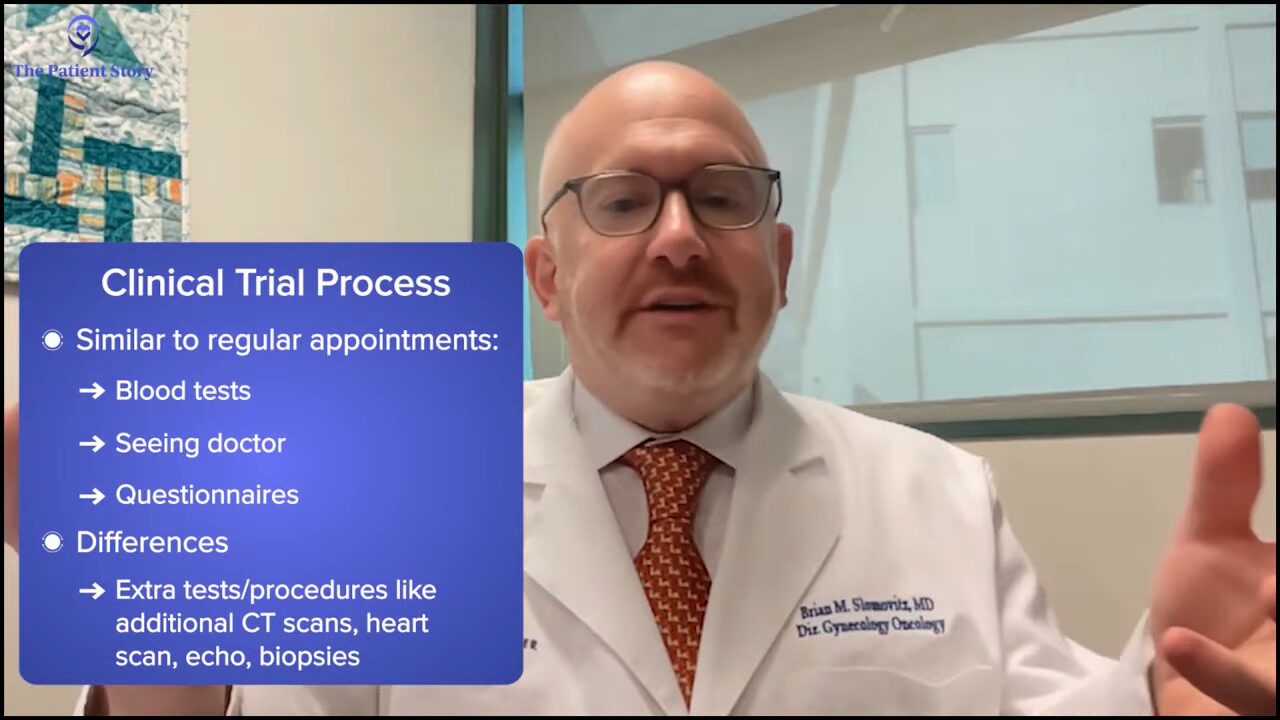
Dr. Slomovitz: There are some similarities and some differences. Similarities include blood tests, appointments with doctors, signing consent forms, and answering questionnaires. These things take a bit longer, but they’re part of the process that we need to go through to get them on a trial. Those are things that we normally do but they’re a little bit more intense in a trial. It’s part of the standard of medical care not only of research care.
In addition, there are tests that we need to do that are outside the standard of care but important for a particular trial. For example, we don’t normally have to do a heart scan and an echo, but for a certain drug, we might have to do them.
The most annoying thing patients may need to do will be an extra biopsy. A lot of our trials now are biomarker-directed and some of these biomarkers are novel, so we don’t have that information unless we do a new biopsy. Any procedure you do has its risks and benefits. Fortunately, a lot of times, biopsies are relatively straightforward.

Improving Diversity in Clinical Trials
Tiffany: How can we improve clinical trial awareness and education in underserved communities?
Dr. Slomovitz: When we talk about a cancer that’s deadly and may end their life prematurely, it’s important to know all the options from the beginning, even if they’re not coming to the office from day one and thinking about or eligible for a clinical trial. Maybe not now but in the future. It’s the education process that says we have things on the standard of care and off the standard of care. It’s important to share the results with our patients so they see that we’re moving forward, knocking down some of the biases.
We talked about things like financial toxicity, time toxicity, and effort toxicity, and helping to overcome those barriers. There are resources out there. Sometimes patients can’t drive. Some of the car companies have different deals. The American Cancer Society supports that and things like that.
It’s a process. We’re getting better, but we still need to do better. I’m not going to be happy until we have a clinical trial option available for all of our patients with advanced recurrent disease to allow them to get the best standard of care before they are defeated by cancer.
Tiffany: The average life cycle of a clinical trial, from the time it starts to the time it gets market approval, could be anywhere between five-plus years. But if you are participating in that clinical trial, you get first-hand results on what’s going on in your care and that data is going to be used to push those approvals.
June is Uterine Cancer Awareness Month
Tiffany: You and I are very passionate not only about diversity in clinical trials but also about education and promoting clinical research. June is Uterine Cancer Awareness Month. Can you talk about that and why that’s important? What are you and Mount Sinai Medical Center doing to promote Uterine Cancer Awareness Month in June?
Dr. Slomovitz: We saw an unmet need. There’s Cervical Cancer Awareness Month in January, Ovarian Cancer Awareness Month in September, and Breast Cancer Awareness Month in October. We needed to make Uterine Cancer Awareness Month, so we started that in 2023.
Mount Sinai is making a big effort here and leading it in South Florida. They also have been supportive of my work with the International Gynecologic Cancer Society, the global leader in gynecologic cancers.
Final Takeaway
Tiffany: What is your takeaway for patients who are newly diagnosed and starting this journey?
Dr. Slomovitz: It’s important to describe why they got it or if we can know why. Sometimes these are obesity-related, hereditary, or caused by other factors. What can they do to get the best treatment options?
Make sure you’re comfortable with your care. Many patients can get a second opinion to make sure that they’re getting the best care. If they’re uncomfortable with the first opinion, seek out a second opinion because this is an important decision. It’s not only the surgery but the follow-ups. Not to say that the first doctor may have done something right or wrong, but when there are different options that patients weren’t made aware of from the beginning, it’s extremely frustrating.
Make sure that clinical trials are an option. If your doctor doesn’t do clinical trials, make sure that he or she is willing to send you to a center that has some of those clinical trials.
Create your medical team. That includes the patient, the patient’s family, friends, doctors, nurses, and navigators. It takes a team to defeat cancer.
Tiffany: Share this discussion with your family, friends, and loved ones. As Dr. Slomovitz said, don’t be afraid to have these discussions, especially when it comes to GYN care and health. A lot of times, we don’t want to talk about that as women and that’s something that we need to get around as well.
If you have a symptom that you know is not normal for you, speak up. Go to your provider and get the care that you need.
Dr. Slomovitz, thank you for the work that you do at Mount Sinai Medical Center in Florida and around the globe. Keep pushing the needle forward. I’m very hopeful that five years from now, we’re going to be in a whole different space with endometrial cancer, so I can only imagine where we’ll be 20 years from now.
Dr. Slomovitz: Tiffany, thank you so much. The future is bright and I’m excited about what it brings. I look forward to talking with you in the future when we talk about our victories too.
Stephanie: Thank you so much, Dr. Slomovitz. I couldn’t agree with Tiffany more. Thank you for being a global leader in this space. The rapid pace and shifting of the landscape of treatment options and all the research that’s happening is incredible. Please continue to do the great work that you do.
Thank you also, Tiffany, for leading this conversation to infuse that patient-care partner voice, which is so important for us here at The Patient Story and our community.
Check out ECANA: Endometrial Cancer Action Network for African-Americans and the work that they do. They create a community for African-Americans who have endometrial cancer or have been impacted by an endometrial cancer diagnosis.
Thank you so much for joining us. We hope to see you at another program.