The Future of Multiple Myeloma Treatment: Expert Q&A on Bispecific Antibodies
A Q&A with multiple myeloma expert Alfred L. Garfall, MD, MS

- Introduction
- Immunotherapies & bispecific antibodies in myeloma treatment
- Difference between CAR T-cell therapy & bispecific antibodies
- Teclistamab
- What are the side effects of bispecific antibodies in multiple myeloma?
- Possibility of giving bispecific antibodies for a fixed duration
- Treating with more than one bispecific antibody
- Where are bispecifics administered?
- Treating high-risk patients with bispecific
- Updates on bispecific antibodies
- Conclusion

Introduction
Jack Aiello: I’m Jack Aiello, a 28-year survivor of multiple myeloma and advocate from the San Francisco Bay Area in California
I’m often asked, what did I do to be around for 28 years?
Most of my treatment was [during] my first eight years. I had a tandem autologous transplant, but that didn’t work very long for me. I had chemotherapy treatments and was in a clinical trial [but those] didn’t work too well either.
I had one option left: an allogeneic transplant where donor stem cells are given to me. That’s not done in myeloma these days because [of] its high mortality rate [of] 40-50% just from the transplant. But the reason it did work for me is it gave me a new immune system.
I’ve watched the development of an incredible number of myeloma treatments. The growth of myeloma treatment continues at a rapid pace and the landscape of all of those treatments is really quite incredible.
We’ll be talking about safer ways to use your immune system with treatments called bispecifics that again will use your immune system to fight the myeloma.
We’re happy to welcome Dr. Alfred Garfall, a myeloma expert at Penn Medicine.
Dr. Alfred Garfall: It’s an honor to be here with you, Jack. You’ve been dealing with myeloma for a much longer time than I have, for sure. Probably going back with it before I even finished medical school.
I’m an assistant professor of medicine at the University of Pennsylvania Abramson Cancer Center. I’m part of a group of six physician investigators who focus on multiple myeloma, taking care of multiple myeloma patients, conducting clinical trials with new multiple myeloma therapies, and also doing pre-clinical studies looking at developing new therapies for multiple myeloma.
The success of immunotherapy for cancer, not just in blood cancers but in other cancers, [has] been one of the big success stories in all of medicine in the last decade or so.
Dr. Garfall
I’ve been practicing since 2014. I trained with Ed Stadtmauer, the leader of our program, during some of the early days of CAR T-cell therapy. I remember being a fellow and seeing some of the first results come out from Penn using anti-CD19 CAR T-cells, now an FDA-approved therapy for leukemia and lymphoma.
The impetus for me to get involved in this work as a clinical investigator was seeing some of those results come out and being really inspired by all the progress that was happening in immunotherapy for hematologic malignancies.
Immunotherapies & bispecific antibodies in myeloma treatment
Jack: What are immunotherapies and what are bispecifics?
Dr. Garfall: Broadly speaking, immunotherapy for cancer is any therapy that tries to induce the patient’s immune system to fight cancer. The success of immunotherapy for cancer, not just in blood cancers but in other cancers, [has] been one of the big success stories in all of medicine in the last decade or so.
You can go back even further to allogeneic stem cell transplantation. The whole idea of allogeneic stem cell transplantation, which has been a therapy for blood cancers for decades now, is to utilize the immune system of a stem cell donor to recognize cancer in the patient and try and kill cancer.
You can think of a stem cell transplant or a bone marrow transplant as an immune system transplant. If your immune system has failed to eradicate your cancer or multiple myeloma, maybe if we give you the immune system of another patient, that will be able to recognize your myeloma as foreign and attack it.
That strategy has proven successful for a variety of blood cancers. It’s not used as much now for multiple myeloma for a number of reasons, but the effectiveness of bone marrow transplantation for chronic myeloid leukemia, where this bone marrow transplant procedure is very successful, was one of the founding observations that immunotherapy for cancer works.
What we’ve seen in the last 10-15 years is the success of approaches that are more pharmacological — drugs as opposed to procedures — that can replicate that immunologic effect in a more targeted and safer way. [An] allogeneic stem cell transplant is still a high-risk procedure.
We’ve seen the success of strategies to induce immune responses against cancer play out in a number of different cancers. Most notable of these is melanoma with an immunotherapy approach called checkpoint blockade that can wake up a sleepy immune system against the cancer cells in patients with melanoma.
That same paradigm has played out across a number of solid tumor cancers — lung cancer, kidney cancer, [and] bladder cancer among others— and we’re seeing that approach save lives all the time.
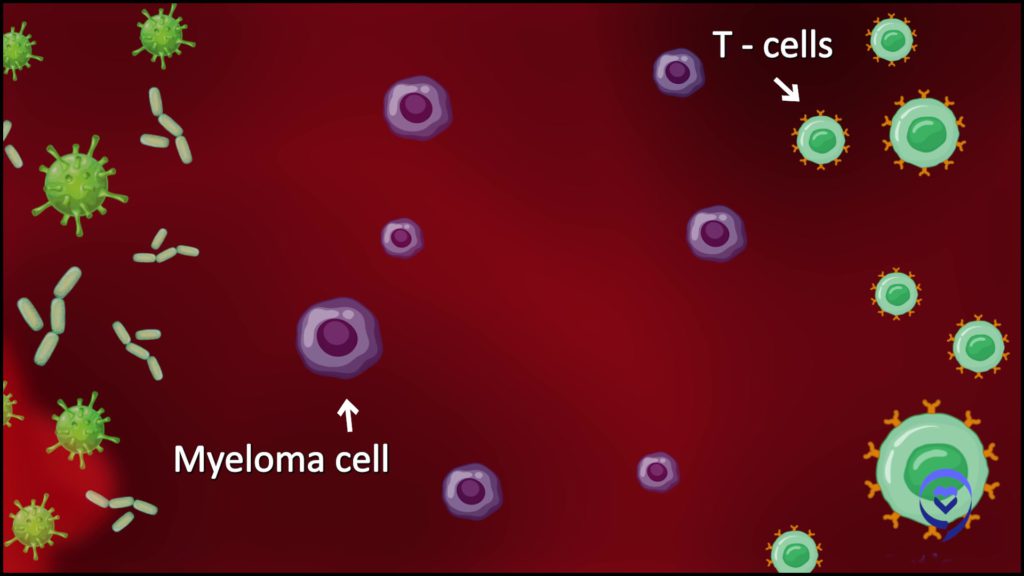
In hematologic malignancies, it’s a slightly different approach to get the immune system to fight cancer. These techniques harness T-cells, which are a part of the immune system, that play a role in fighting cancer but also [in] fighting infections. Approaches of what we call redirecting T-cells.
T-cells are the cells in your body that are trained on specific proteins. These are typically found in bugs that make you sick — bacteria, viruses. It turns out that those T-cells have the ability to kill cancer cells, but in patients with an established cancer, those T-cells aren’t doing the trick.
We want a target on the surface of the myeloma cell that can distinguish the myeloma cell from healthy cells in your body. Then we want to find a way to get the T-cells to recognize that target and kill the cells that express that target, namely the multiple myeloma cells.
Dr. Garfall
These latest therapies that have come down the pike in blood cancers, namely CAR T-cells and bispecific antibodies, redirect all the T-cells in your body away from the virus or bacteria that they might have been designed to treat and towards the cancer cell.
CAR T-cells and bispecific antibodies do that in a similar way, although there are some important differences between them. [The] approach of CAR T-cells and bispecific antibodies has been successful. We see that in [the] FDA approval of CAR T-cell therapies and bispecific antibodies initially to treat B-cell acute lymphoblastic leukemia then non-Hodgkin’s lymphoma and, subsequently, multiple myeloma.
Difference between CAR T-cell therapy & bispecific antibodies
Jack: As myeloma immunotherapy treatments, how do CAR T and bispecifics differ from one another?
Dr. Garfall: Both these approaches try to get your T-cells to recognize your multiple myeloma cells by a molecule on the surface of the myeloma cell. We want a target on the surface of the myeloma cell that can distinguish the myeloma cell from healthy cells in your body. Then we want to find a way to get the T-cells to recognize that target and kill the cells that express that target, namely the multiple myeloma cells.
How CAR T-cell therapy works
The way that’s done with CAR T-cells is that T-cells are taken out of your body and brought to the lab. Those T-cells are genetically engineered so [they] can recognize that target on the multiple myeloma cells. Those cells are infused back into your body.
With that engineering, those cells will then be able to recognize the target on the surface of the multiple myeloma cells and kill the multiple myeloma cells. It’s a bit of a complex process because in order to create this therapy for a patient, you have to make a product for that particular patient.
Every patient has to have the CAR T-cell therapy manufactured for them using their own cells. No other myeloma therapy works that way where you have the therapy manufactured for the particular patient.
Most myeloma therapies are drugs. That’s a complexity [of] CAR T-cell therapy that’s different from other multiple myeloma therapies, but it’s quite effective. We can talk more about how well it works for multiple myeloma patients, but it’s a really effective new therapy.
How bispecific antibodies work
It really is an amazing feat that you can get the same kind of clinical effects with bispecific antibodies as you can with CAR T-cells but with the simplicity of a pharmaceutical that can be given without that complex patient-specific manufacturing.
Dr. Garfall
Play the video to watch Dr. Garfall explain bispecific antibodies
Dr. Garfall: Bispecific antibodies try and do that same thing but in the form of a drug. A bispecific antibody is a molecule that’s got two arms. One arm grabs a T-cell and the other arm grabs a multiple myeloma cell by recognizing a target on the multiple myeloma cell, just like the CAR T-cell does.
This bispecific can grab a myeloma cell with one arm, grab a T-cell with another arm, bring them together, and force that T-cell to recognize the multiple myeloma cell.
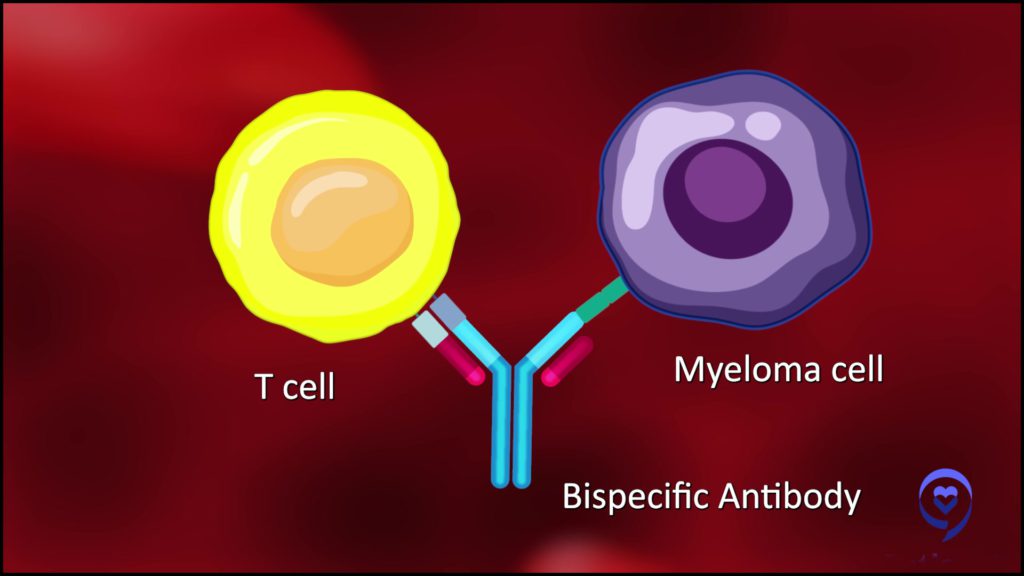
It’s the same basic strategy as CAR T-cells in that we’re trying to get the T-cell to recognize the myeloma cell, but you’re doing it in the form of a drug rather than through this complex genetic engineering process. That has the advantage of not requiring T-cell extraction and patient-specific manufacturing.
It’s a medication, like daratumumab or elotuzumab. It can be pulled off the shelf and given to a patient. You can get very similar levels of T-cell activation against multiple myeloma with bispecific antibodies that you can get with CAR T-cells.
It really is an amazing feat that you can get the same kind of clinical effects with bispecific antibodies as you can with CAR T-cells but with the simplicity of a pharmaceutical that can be given without that complex patient-specific manufacturing.
Teclistamab
Jack: We have one bispecific antibody called teclistamab, also known as Tecvayli, that’s currently FDA-approved. How is it given? Who is it given to? What are the typical responses and how long do they last?
Dr. Garfall: Teclistamab is the first approved bispecific antibody for multiple myeloma. It recognizes this molecule called BCMA.
A lot of the new immunotherapies against multiple myeloma recognize BCMA on the surface of myeloma cells. We have two CAR T-cell products that are approved for myeloma called Abecma and Carvykti; they recognize BCMA. Then teclistamab, a bispecific antibody, also recognizes BCMA.
Administration of teclistamab
Teclistamab is given as a subcutaneous injection, which is quite remarkable if you think about how simple it is compared to CAR T-cell therapy. It’s impressive progress in terms of our treatment options to have that kind of potent immunotherapy that can be administered as a subcutaneous injection.
These bispecific antibodies are actually more potent in terms of how they activate the immune system than something like daratumumab. The dose of the antibody is quite a bit lower. While Darzalex has to be given as that long, three-minute subcutaneous injection, teclistamab is just a really quick subcutaneous injection. But that’s a minor point.
It’s given as a subcutaneous injection once a week. [In] the clinical trial, it’s been shown that you can extend dosing to every two weeks or even every four weeks. We’re going to get more data on less frequent dosing. But right now, the way it’s approved by the FDA is as a weekly subcutaneous injection.
Dosing of teclistamab
Because of some of the risks of teclistamab and the concern that it might activate the immune system a little too quickly and lead to some side effects, the first couple of doses [is] given as little steps up. You start with a small dose. Then a couple of days later, you get a medium dose. Then a couple of days later, you get the full dose.
Those first few doses are typically given in the hospital so that if [a] patient’s immune system gets a little bit overactive, that can be managed quickly. But that risk seems to be really confined to those first few doses.
Once you get past those first few doses, you really don’t have that risk with ongoing dosing. It can be given in the outpatient clinic without concern for toxicity the rest of the time that you’re on the medication.
The way that it’s given right now is that you keep getting it as long as it’s working. We may hear more about alternative strategies that don’t give it forever. Right now, as long as it’s working, patients continue to get the medication on a weekly or every two-week basis.
That’s what is so exciting about medications like teclistamab and CAR T-cells.
If these therapies can show so much promise in patients whose myeloma has become really, really aggressive and refractory to therapy, we think that there’s going to be even more impact when we can use these therapies a little bit earlier on in the disease course and perhaps even in combination with other therapies.
Dr. Garfall
High response rate to teclistamab
It’s an accelerated approval so it hasn’t had the big phase 3 clinical trials that compare it to other therapies for long-term outcomes, like how long people live with myeloma [and] how long it keeps the myeloma under control. Those studies haven’t been completed yet.
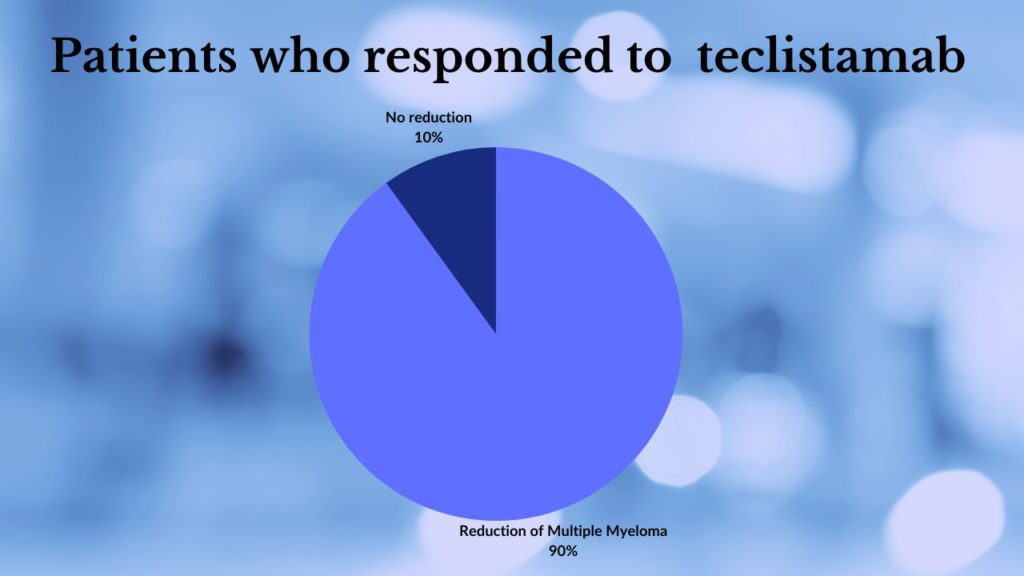
It showed really promising activity just in itself in patients with myeloma that were running out of treatment options. It showed a response rate of about 65% as a single medication, which is really impressive as a single medication. Most of these responses were really good responses. The vast majority were either very good partial responses or complete responses.
Almost all patients who responded to the medication had at least a 90% reduction in the amount of multiple myeloma in the body. That’s really impressive for patients who are running out of treatment options, whose myeloma had become resistant to all the standard medications.
For a single drug to have that kind of response, especially with the simplicity of subcutaneous injection, that’s really promising. We’re really excited that it’s out there now and we’re able to use it to treat patients who are not on the clinical trial.
The response rate [is] that much higher [and] robust in terms of 90% reductions in myeloma. We’ve learned [with] Velcade and daratumumab, once we got past those phase 1 studies, and those medications have been moved into earlier lines of myeloma therapy and combined with other therapies, that progress has led to many, many years of improvement in the expected survival of multiple myeloma patients.
That’s what is so exciting about medications like teclistamab and CAR T-cells. If these therapies can show so much promise in patients whose myeloma has become really, really aggressive and refractory to therapy, we think that there’s going to be even more impact when we can use these therapies a little bit earlier on in the disease course and perhaps even in combination with other therapies.
Daratumumab and Velcade showed 30% response rates initially. When you started combining them and moving them into earlier lines of therapy, we saw those benefits magnified many times. We’re optimistic that we’re going to see that same trend with some of these newer immunotherapies.
What are the side effects of bispecific antibodies in multiple myeloma?
Jack: Can you talk about the side effects of bispecifics?
Dr. Garfall: This is where some of the complexity comes in. We do worry when the medication is given that it can activate the immune system too quickly and that could lead to some complications.
Cytokine release syndrome (CRS)
In its simplest form, cytokine release syndrome (CRS) is just some fevers but if it gets out of hand, it can progress to difficulty breathing, low blood pressure, [the] potential to be in the intensive care unit, and even potential for patients to even pass away from this complication.
If you look across these types of therapies and different diseases, there have been patients who have passed away from cytokine release syndrome (CRS) getting out of hand. That’s why patients are watched in the hospital with those initial couple [of] doses.
The experience with teclistamab has been very favorable in that patients who get CRS for the most part have it in a mild to moderate form that is very manageable. We have not seen patients in the teclistamab studies pass away from CRS complications. But in theory, we know it’s possible and that’s why patients are in the hospital.
If somebody has a fever after they get teclistamab and it starts to get a little out of hand — maybe it’s not just one fever, but it progresses to two or three high fevers — there are really good medications we can give to calm down that inflammation. Then you can allow subsequent doses to proceed and still get the same therapeutic benefit against the myeloma but without additional fevers and cytokine release syndrome.
We think of this as a very manageable complication. It is the same kind of thing that can happen after CAR T-cell infusion and we manage it [in] very similar ways.
Right now, its use is restricted to places that have expertise in handling that complication. Not every oncology office is hooked up to a hospital with a specialized oncology unit that’s capable of managing some of these complications. In our region, it’s mainly the academic centers that are using this medication.
There are a number of bispecific antibodies that are being developed not just for multiple myeloma but for lymphoma and other cancers. With time, I do think that the oncology community is going to get more comfortable with these toxicities and have pathways in place to handle them even at a community center or community hospital so that these drugs are available not just to patients who are connected to a big center but to patients all around the country and world.
Susceptibility to infections
Dr. Garfall: There [are] inflammatory reactions that can happen with the first few doses and, fortunately, those are confined to the first few doses and not an ongoing problem.
As patients get this medication for months and months though, we’ve learned that it is immunosuppressive even as a single medication.
We do worry about infection over the long term. Infection is a concern we have in any multiple myeloma patient with any therapy, but we do think the risk is a bit higher with teclistamab and other bispecific antibodies that target BCMA.
There are some things we can do to manage that risk. We generally recommend that patients take some prophylactic antibiotic against pneumocystis pneumonia. The most common way we handle that is to give Bactrim, which is an antibiotic that’s very good at preventing that type of pneumonia.
We give patients IVIG. IVIG is antibody replacement therapy. Think of it just like if your red cell count gets low, we can give you a red cell transfusion. If your platelet count gets low, we can give you a platelet transfusion. If your antibody level gets low, we can give you an antibody transfusion. Intravenous immunoglobulin is basically a transfusion of antibodies that can raise your antibody levels.
Teclistamab kills the normal plasma cells in the body. We think of myeloma plasma cells as cancerous plasma cells, but your body also has normal plasma cells. The normal job of plasma cells in your immune system is to make the antibodies that help you fight infection.
[For] patients who get teclistamab over the long term, the drug really lowers the level of normal plasma cells in the body and therefore lowers the amount of normal antibodies being produced in the body. We can get around that by giving patients periodic transfusions of antibodies that have been collected from donors.
IVIG can be dosed every one to three months to maintain antibody levels at a level that preserves some of your immunity. But that does add complexity to this otherwise simple therapy.
While the drug itself is a simple subcutaneous injection once every one to two weeks, when you throw in that you may have to get IVIG therapy every couple of months, it does add to the burden, cost, and, even a little bit, the risk of the therapy. But it’s an important measure to reduce the risk of infection with teclistamab because we have learned that patients getting teclistamab over the long term are at significant risk of infection.
Jack: In the past, there were shortages of IVIG. Is that still an issue or do we not worry about that anymore?
Dr. Garfall: Periodically, there have been shortages of IVIG in certain parts of the country. During the pandemic, I think there were some shortages.
Also, IVIG is quite expensive. We sometimes have to fight with insurance companies to get it covered.
IVIG is more or less available in different parts of the world. We’re fortunate in the US to be able to get it for most of our patients, but it’s not as readily available in other places so that is a significant issue we have to worry about.
Possibility of giving bispecific antibodies for a fixed duration
The myeloma research community has been so impressed with the quality of the responses. We’re beginning to think maybe we don’t need to continue this medication forever. Maybe it’s a medication that can be given for six months, nine months, a year or so, and, during that time, you’re going to have to have all this really proactive management of infection risk.
If your response is really good, as many of these responses are, maybe you can stop the therapy and the myeloma will remain under control. Without the medication, the immune system will start to build back up and you can have the best of both worlds — good myeloma control and an intact immune system.
Some patients on the clinical trial had to stop treatment for one reason or another. Even after stopping treatment, a lot of those patients remained without any myeloma progression for many months.
I think that is going to be a focus of the next generation of clinical trials: trying to figure out how long we have to give these medications. Can we find a balance between long-term infection risk and myeloma control with a fixed duration of therapy?
Cevostamab study
Another bispecific antibody being tested right now that has a different target is cevostamab. The way those clinical trials were done was it was given for a year and then stopped. That one’s not FDA-approved yet. We got some results from the initial clinical trial and we’re starting to see how those patients are doing after they’ve stopped it.
In patients who had good responses after one year of therapy, none of them have really had the disease grow back if they had a good response before stopping it. That’s really promising.
As we learn more about these agents, maybe we won’t have to give them forever and deal with years of immunosuppression. Maybe we can give them for a fixed period of time and reduce the risk of infection.
Treating with more than one bispecific antibody
Jack: Why do we need more than one bispecific? What’s the benefit of that for patients?
Dr. Garfall: There are a few potential benefits. Both CAR T-cells and bispecific antibodies need to recognize the multiple myeloma by a molecule on the surface of the multiple myeloma cell. The one that’s been investigated most intensively is BCMA. Teclistamab and the two CAR T-cell products that are approved recognize BCMA. There’s a couple [of] others that are in development that recognize BCMA.
What we’ve learned though is that if you give a therapy that targets BCMA long enough, the myeloma may get smart and get rid of BCMA. What you’ll have is myeloma that’s growing. It’s evading the treatment. The myeloma has adapted and masked or turned off the BCMA molecule so the drug can’t recognize the myeloma anymore.
What’s great about other bispecific antibodies that are being developed is that they recognize a different target on the myeloma cells. Even a myeloma that is no longer expressing BCMA might be recognized by some of these other bispecific antibodies.
Talquetamab (bispecific antibody)
The next one to probably be FDA-approved is a drug called talquetamab, [which] recognizes a molecule on the surface of the myeloma cell called GPRC5D.
There are some patients who have received teclistamab, it stopped working, they’ve gone on to get talquetamab, and the talquetamab worked. [This] suggests that patients can really benefit from therapy with one bispecific antibody for a while, have it stop working eventually, and then be able to move on to benefit from another bispecific antibody that targets a different target on the myeloma cell.
Teclistamab and some others target BCMA. Talquetamab targets GPRC5D. Cevostamab targets FcRH5. We’ll have this toolkit of different potent immunotherapies that all recognize multiple myeloma in different ways. That gives us more ways to attack the myeloma with different targets and makes it harder for the multiple myeloma to evade all the therapies we have.
Jack: Both of the CAR Ts also target BCMA. If I relapse from a CAR T, does that mean that a drug like teclistamab is not really available to me because I may not have BCMA anymore? Or does the BCMA marker come back after a certain length of time?
Dr. Garfall: We’re still learning a little bit about that, to be honest. These are all new therapies. We haven’t had tons of patients who have progressed on one and gone on to receive the other.
This is a little bit premature to say but we are learning that patients who progress after CAR T-cell therapy that targets BCMA probably still have some BCMA on their myeloma cells for a variety of reasons.
It’s been reported at the 2022 ASCO annual meeting that a small group of 20 or so patients who had previously received a therapy that targets BCMA — for example, a CAR T-cell — if they go on to get teclistamab, about 50% or so of them will respond. Now that’s a small number of patients so maybe the actual percentage is a bit higher and lower, but it’s not hopeless.
Someone who progresses on a BCMA-targeted CAR T-cell could potentially benefit from a BCMA-directed bispecific antibody. There are even some results the other way around — patients who have progressed on bispecific antibodies and gone on to respond to CAR T-cells.
It is worth considering. These are really patient-by-patient decision-making processes that you go through with your doctor about whether it makes sense to try some of these.
We’re starting to get more tools available. There are some ways on a bone marrow biopsy to look and see whether your myeloma expresses BCMA. I hope in the next couple of years we’ll have some blood tests that can give us a hint at that so we can be more sophisticated and precise in our treatment decisions based on these tests that we can do. We’re not there quite yet, but it’s definitely within reach.
Where are bispecifics administered?
Jack: Do you think patients will have a chance of getting bispecifics from the community oncologist rather than having to travel? Or will patients always have to go to a medical center for those first weeks of treatment?
Dr. Garfall: I’m optimistic that this will not be confined to the big medical centers, but it might take a little while. With any new drug, it takes a little while for physicians to get comfortable with it.
There are special registrations you have to do to be able to give this drug in your practice. There’s [a] certification process you have to go through with the FDA called a REMS (Risk Evaluation and Mitigation Strategy) program where you, your pharmacy, and your office have to take some training to demonstrate that you understand the particular risks of this medication and how to manage them.
I’m optimistic that it will get there, especially because this is not just teclistamab. It’s not just this one drug. It’s not just for multiple myeloma. There’s already another FDA-approved bispecific antibody that’s approved for lymphoma. There’s probably going to be more coming down the pike for lymphoma. Once there’s that kind of momentum behind a type of medication, everybody starts recognizing that it’s really important to figure out how to give it not just in these larger centers but in the community.
I also think we’ll start to see some trials of outpatient dosing. Everybody may not [have] to be in the hospital. Certain patients who are a little sicker and [have] more problems may need to be in the hospital.
Your typical patient who is just starting to progress and not having major complications of disease progression yet can maybe be safely dosed in the outpatient setting with a lot of close monitoring. These are some things that we’ll figure out over time.
Jack: It’s only approved for patients who have had three or four prior lines of treatment, right?
Dr. Garfall: That’s an important point. It’s this accelerated approval for patients who have had four or more prior lines of therapy, who are running out of options. So far, it has only been tested in a phase 1 and a phase 2 trial.
There are phase 3 trials going on that will hopefully confirm that this is a good medication that helps multiple myeloma patients live longer with the disease. I think that will open it [for] use a little bit earlier on in therapy rather than having it be reserved for patients who are running out of options.
Treating high-risk patients with bispecific

Jack: High-risk patients are more difficult to treat than others. How do they do on bispecifics and immunotherapies in general?
Dr. Garfall: When you’re talking about a patient population that is in four or more prior lines of therapy, in some ways, those are high-risk patients. Even if a patient was low risk when they started with multiple myeloma, 10 years down the road after lots of prior therapy, that disease can be pretty aggressive.
When you see response rates of 60-plus percent with a single medication in patients who have had that much prior therapy, that includes a patient population that has [an] aggressive disease whether they were officially designated as high risk when they started or not.
We see patients with extramedullary disease — multiple myeloma started to grow as tumors outside the bone marrow. Those patients maybe have a little lower response rate to the medication, but many of them do respond. This is still a real option to try for patients, even with some of those higher-risk features, but the response rates might not be quite as high.
We’re still waiting to see how long these responses last and whether there are any meaningful differences between different groups of multiple myeloma patients.
What was also really encouraging from the teclistamab data is that if you look at patients who are responding to the medication, a year later, about 70% of the patients still have ongoing disease control. The medication’s still working for them.
We’re still waiting to see how long that can go. We have patients in our practice from the clinical trials who’ve been on the medication for three years and it’s still working.
Now, I bet that’s another way that some of the higher-risk patients will be different from the standard-risk patients. Even though it’s working for them initially, maybe the responses aren’t going to last as long. That’s true of most myeloma therapies. Patients with more aggressive disease may respond really well to all the medications, but those responses may not last as long.
Updates on bispecific antibodies
Jack: What are you interested in hearing regarding bispecifics from the American Society of Clinical Oncology (ASCO) Annual Meeting and European Hematological Association (EHA) Congress?
Dr. Garfall: I think we’ll get some updates with longer-term follow-up, on teclistamab and other bispecific antibodies, about how long these responses last. They haven’t released the actual data to know whether any new bispecific antibodies will release promising data.
I imagine we’ll hear some data on the use of CAR T-cells in earlier lines of therapy. All these therapies that are initially tested in patients who have run out of options [are getting] tested earlier on.
In the last six months or so, we have had the publication on the use of Abecma, the first CAR T-cell approved for myeloma, in patients with two to four prior lines of multiple myeloma therapy. This was one of the first phase 3 studies with Abecma where they really compared Abecma to the standard therapy. They found that Abecma worked better than the standard therapy.
I think we’ll be hearing soon about the first study with Carvykti, which is the second anti-BCMA CAR T-cell to be approved. I believe there’s been a press release that it’s also favorable. When you compare Carvykti in patients with one to three prior lines of therapy earlier on, for that first or second relapse, Carvykti seems to work a lot better compared to one of the standard options.
We’ll hopefully get more data on how much better and more detail about those responses. In the next year or so, maybe we’ll start to see some of the results from ongoing studies with bispecific antibodies.
It’s really exciting. It’s going to be confusing for us physicians to try and figure out when to use which one of these new therapies. But overall, it’s really exciting to have all these new options coming down the pike so quickly for our patients.
Conclusion
Jack: I learned an awful lot about bispecifics, an exciting treatment paradigm for multiple myeloma. Dr. Garfall, I really appreciate it. Thank you so much for spending time with us. I look forward to learning more in the future.
Thank you for joining us on The Patient Story.
Dr. Garfall: It’s been a real pleasure. Thanks so much for the invitation. It’s so nice to speak to you. I hope this was helpful.