Newly Diagnosed Multiple Myeloma Highlights from ASH 2022
What Newly Diagnosed Patients and Caregivers Need to Know
Multiple myeloma patient advocate Cindy Chmielewski has been living with myeloma for nearly 15 years. After experiencing excruciating back pain for two years, she was diagnosed with IgG Kappa stage 3 multiple myeloma.
In this conversation, she speaks with Dr. Caitlin Costello a hematologist-oncologist at the University of California, San Diego and Dr. Sagar Lonial, the chief medical officer at the Winship Cancer Institute at Emory University.
They discuss cutting-edge treatments and therapies for both transplant-eligible and transplant-ineligible patients, combination therapies and the necessity of stem cell transplants.

Thank you to Janssen for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Transplant-eligible and transplant-ineligible patients
- Improving frailty in patients
- Treatment for transplant-ineligible patients
- What is maintenance therapy?
- 3 vs 2 drugs (MAIA trial)
- Using 4 vs. 3 drugs for treating transplant-eligible patients
- Do you think the 4-drug combination will be the new standard of care?
- Who is eligible for quad-based therapy?
- What does it mean to be high-risk?
- Side effects for different drug combinations
- The necessity of stem cell transplant (DETERMINATION trial)
- IVIG and daratumumab
- Dexamethasone
- FasTCAR T cell therapy
- Seeing a myeloma specialist
- Conclusion
- Multiple Myeloma Patient Stories
Introduction
Cindy Chmielewski, Myeloma Patient: I’ve been living with multiple myeloma since 2008. I was a fifth-grade teacher and I simply loved my job.
Around 2006, it became very difficult to teach. I was experiencing excruciating back pain. Standing was very hard, recess duty was almost impossible, and I couldn’t even take my class on a field trip. The tears would come down my cheeks. That’s how much pain I was in.
For the next two years, I was prescribed pain medication and physical therapy. I was a very different person than I am now. I grew up in [the] age of doctor knows best so I really didn’t question what my doctor was doing, although I thought that maybe we should be taking an X-ray of my back.
I was diagnosed with IgG kappa stage 3 multiple myeloma. The multiple myeloma was in over 99% of my bone marrow.
I started treatment immediately. The treatments back in 2008 were very different than now. In the beginning, I had a tough time. The treatments were not touching my myeloma. I had initial success, but then it stopped working. I had a stem cell transplant and that didn’t work. I was devastated. I really didn’t think I was going to live much longer.
A treatment that my doctor suggested began working for me. It worked so well that it put my disease into remission.
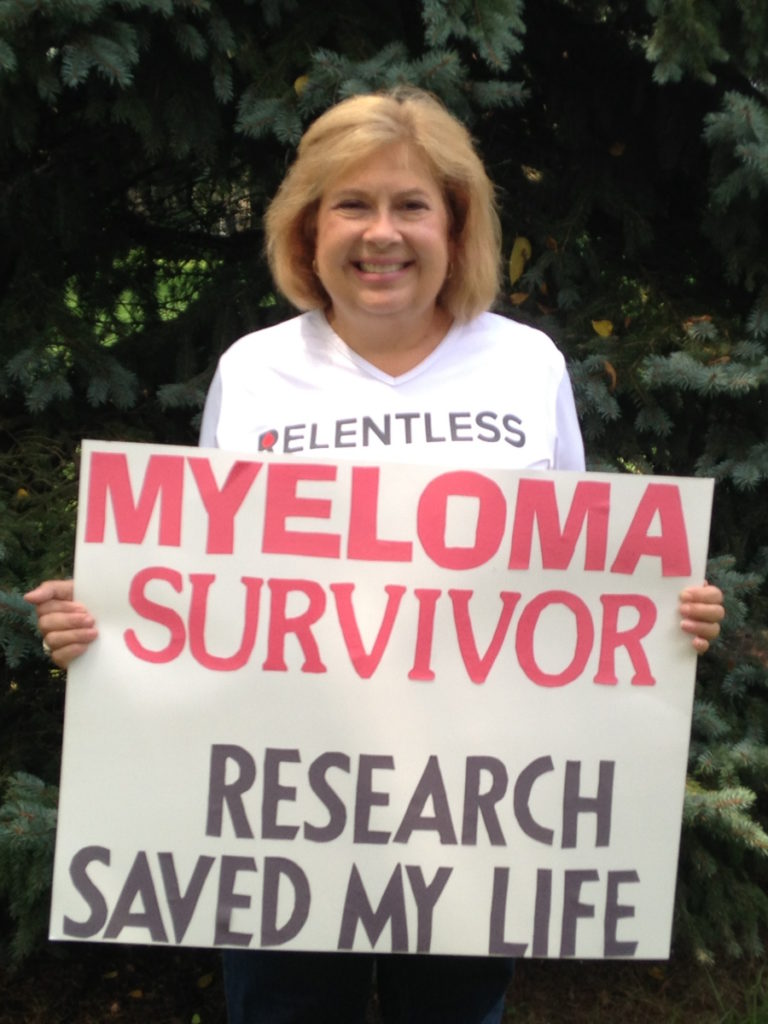

Since about 2010, I’ve been on maintenance therapy and able to live my life. In the meantime, I retired from teaching because I didn’t know what I was going to be doing.
I’m a different person now. I don’t teach fifth graders; I teach myeloma patients about myeloma and how important it is to be actively involved in your care, not to be that person like I was back in 2008 just blindly following doctor’s orders
It’s important to learn all you can about your myeloma, to ask questions, and to make decisions. It’s so exciting because now, there are so many treatments to choose from that if one thing stops working, there are so many other choices.
[In this conversation] I talk with two myeloma specialists about the latest happenings for the newly diagnosed population coming out [of] a meeting called ASH [American Society of Hematology].
Dr. Caitlin Costello is the hematologist-oncologist at the University of California, San Diego who specializes in treating multiple myeloma and participates in many of the myeloma clinical trials.
Dr. Sagar Lonial is the chief medical officer at the Winship Cancer Institute at Emory University, the chair of the hematology and medical oncology department, and a lead voice in the myeloma research community.
Transplant-eligible and transplant-ineligible patients
Cindy, TPS: Usually, newly diagnosed [patients] are broken up into two groups: transplant eligible and transplant ineligible. Before we even start talking about what’s happening in that area, how are those defined? How do you know if I’m transplant-eligible or ineligible?
Dr. Caitlin Costello: Good question and, actually, a bit of a moving target. [Transplant eligibility] is usually assigned at the time of diagnosis. A patient first gets diagnosed with multiple myeloma.
Historically, oncologists got kind of a gut instinct to say, “This patient is younger, older, healthier, less healthy, [have] a good performance status.” They’re independent [in] their activities of daily living. They can bathe themselves. They live alone. They do their own grocery shopping. Whatever it is. We’d look at a patient and say, “Healthy, not healthy, old, young,” and make generic assignments to people.
That’s really challenging to do when someone’s first diagnosed with myeloma because when you’re first diagnosed, you’re sick. You don’t feel good. You’ve spent months trying to figure out what’s going on. It may have taken a while to get the diagnosis at that point. Many bones have been affected by myeloma. It can be very painful. A lot of people just aren’t what we think normal health is.
Traditionally, we have made assignments when patients were first diagnosed to say, “You are healthy enough, strong enough, or well enough that you can get an intensive regimen called a bone marrow transplant or not.”


There’s been a bit of an evolution to the concept of transplant eligibility as some more data has emerged to say, “Does everyone have to get a transplant?” Maybe we don’t need to use those same kinds of assignments to make that determination.
I think the better way to distinguish between patients who may be able to get a transplant and patients who may not is frailty. Frailty is a little bit more of an objective, as opposed to a subjective, means of evaluating someone’s health and independence.
[It can] really help identify those patients who may be candidates for more intensive therapy throughout their myeloma diagnosis and their treatment. That is kind of where we’ve landed on transplant eligibility and ineligibility. Do we think people are well enough to undergo a bone marrow transplant?
Improving frailty in patients
Cindy, TPS: Frailty is dynamic now. It can’t be just measured at one point because, throughout the course of treatment, you may improve because the treatment is helping you out.
Dr. Costello: That’s our goal. So many patients are not well when they’re first diagnosed but can turn around pretty quickly where they perk up. Their bone pain is under control [as well as] their anemia, their kidney disease, or whatever way the disease manifested.
Treatments now are so good that patients are responding so quickly. They get better quickly. The way that your doctor first met you when you were diagnosed is unlikely the same person that they will meet two months down the road after you’ve started treatment.
Our job is to continually reassess your health and your general wellness to make that decision because what you were yesterday may not be what you are tomorrow.
Treatment for transplant-ineligible patients
Cindy, TPS: Let’s talk about that group, transplant-ineligible patients, people who may be not strong enough for their body to endure this treatment. What’s the most common type of treatment that this group of people usually get?
Dr. Costello: A bit of an evolution as well. We’ve had so many new drugs developed in multiple myeloma. When drugs get developed, they are first approved for patients who have had many prior treatments. They’re looking for the next newest and greatest.
That’s usually how the FDA approves these drugs. They approve it and say, “Let’s just start with this group of patients.” Over the years, it gets tested with more and more patients earlier on in their diagnosis.

One of the things that patients with newly diagnosed myeloma, who are not planning or not eligible or too frail to go to transplant, have enjoyed is the addition of daratumumab to the first treatment you receive when you’re diagnosed.
Daratumumab, [as] I like to describe [it], is a bit of a magnet. It’s technically called a monoclonal antibody, but it is a medicine that predominantly is given as a shot. It is particularly looking for a sign on the myeloma cells that says, “Hey, this is me.” When it finds it, like a magnet, it sticks to it.
That helps pop it open and it pops it open with many different approaches. It’s a real kind of targeted treatment and uses your immune system to help kill as well. I have seen daratumumab evolve into the gift that keeps on giving because it really has helped so many patients [at] various time points in their disease.
Now, being so effective, why wait? Why can’t we use it when patients are first diagnosed? That has really now turned into the optimal treatment as a basis for when older, frail, weak, or less healthy people are diagnosed with myeloma.
But remember, we like to use multiple drugs. I think of it as like the old game of Clue. Instead of just using a candlestick, a revolver, or a lead pipe, we want to use all the tools we have together as a cocktail so that we can approach the myeloma, sneak up on it, and kill it [in] different ways.
Daratumumab is great in combination with many different treatments. I’d say the frontrunner right now is the combination of daratumumab with lenalidomide, also known as Revlimid, plus or minus dexamethasone, which is something that we’ll get into.
What is maintenance therapy?
Cindy, TPS: Since this is a program for newly diagnosed patients, sometimes all these terms are hard to understand. Can we talk about what maintenance therapy is? Why is it important?
Dr. Sagar Lonial: That’s an important question and it gets into another important data set that was presented at ASH [2022], really focusing on [the] duration of maintenance therapy. What we know is that if you give highly effective therapy, you will get a deep response.
Many of the measures we use to evaluate how much myeloma remains are not perfect. Even MRD, which is minimal residual disease testing at one in a million or fewer, is still not necessarily a surrogate for [the] cure or elimination of the disease.
What we’ve learned is that a little bit of low-dose, non-intensive therapy can maintain that remission for a longer period of time. In randomized trials [where] patients that got no maintenance therapy versus patients that got Revlimid alone as maintenance therapy, the remission duration was at least double for the patients that got maintenance therapy.
The goals of maintenance therapy are to be low intensity and not necessarily impact [the] quality of life. While I’m aggressive about continuing maintenance as long as I can, I usually say we continue until progression or toxicity. Obviously, toxicity is an important variable in that discussion.
What we now know is that high-risk myeloma patients need more than just Revlimid as maintenance therapy. Our group, and now several other groups, have shown that a drug like Velcade added to Revlimid, or carfilzomib added to Revlimid, is able to induce deeper and more durable responses, particularly in high-risk patients. Maintenance means lower intensity, but the goal is to ultimately improve outcomes.

3 vs 2 drugs (MAIA trial)
Cindy, TPS: There were some updates in the MAIA trial at ASH [2022]. Can you tell us the latest and greatest from the MAIA trial?
Dr. Costello: The MAIA trial was designed for [the] patients that we’re talking about. They got the combination of three medicines — daratumumab, lenalidomide, and dexamethasone — and compared it to patients in that same group and only gave them two of the medicines — lenalidomide and dexamethasone.
The whole point was to understand: is three better than two? If so, how can daratumumab help improve above and beyond just the two? It was designed for patients when they were first diagnosed, not going to transplant. [They] use these treatments for as long as they are effective and as long as it’s tolerated by the patient.
It’s been a good number of years now since this trial started [and] ended. [They] are still following these patients for many years to try and see over time not only how successful it is but how durable it is.
The greatest thing and probably the most important thing we can do is [to] get people into remission the first go around. We like to say the first cut is the deepest. How can we have the most success when the myeloma is in its most kind of naive state? It doesn’t know any better. It’s not going to become resistant. We want to throw our best kind of weapons at it first.
[In] the MAIA trial, over the last many years, we’ve seen updates that come out that tell us time and time again that the three medicines combined are [an] extremely successful combination to get people into remission [and] keep them there.
The durability is because we are killing so much myeloma. The myeloma you can see above the surface [and] under the surface that’s very hard to detect. We’re just killing it all.
By making the myeloma stay away, people are living longer. We’re seeing all these outcomes and results from the MAIA trial year after year, showing that the success of these three medicines together is great because it works and it lasts.
Using 4 vs. 3 drugs for treating transplant-eligible patients
Cindy, TPS: The MAIA trial was trying to see for the ineligible patients if three is better than two. For the transplant-eligible patients, I know the question is, “Is four better than three? Should we be adding daratumumab to RVd (Revlimid, Velcade, dexamethasone)?” One thing that keeps coming up is quality of life. Can we talk about 4 vs. 3 in the newly diagnosed transplant-eligible population?
Dr. Costello: If we’ve proved three is better than two medicines together, it brings up the next natural question: is four better? That question is trying to answer if [they should be] adding daratumumab to another group of patients who have just been diagnosed with myeloma.
Let’s say that this is a younger, stronger, healthier group of people, who we have historically treated with three medicines called lenalidomide, bortezomib, and dexamethasone. For the last many years, that combination has been the mainstay. It’s been the most widely accepted, most successful treatment that we’ve been able to achieve ever. But we need to always do better.
The GRIFFIN study looked at patients who were younger, healthier, stronger, going to go to transplant, divided it in half, and said, “I’m going to give you three medicines like we always do. This is the current standard of care,” or, “I’m going to give this other half four medicines.” The same treatments that the first three got — Revlimid, Velcade, dex — and add the daratumumab to it for a group of four.
All patients got the treatment that they were assigned. All patients subsequently had a bone marrow transplant. After the transplant, all patients got consolidation and maintenance, which just means a little extra therapy after your transplant, followed by some amount of maintenance therapy, which is usually either fewer drugs or lower doses as a means of maintaining the successes you’ve had from all the treatments prior.
By comparing four drugs to three drugs for this group, again, daratumumab keeps winning. We see that daratumumab is effective at deepening response, killing more myeloma, making it get into remission more likely, [and] allowing patients to get back to themselves, to get stronger, and to continue on some amount of medicine that’s going to allow the myeloma to stay in remission in very deep ways.
Again, seeing the same outcomes we saw in MAIA, the addition of daratumumab to our standard of care allows for great successes that last.
Do you think the 4-drug combination will be the new standard of care?
Cindy, TPS: Do you think the four-drug combination is going to be the new standard of care for newly diagnosed myeloma patients?
Dr. Costello: I don’t think “will.” I’m already doing it. It’s hard to ignore the data when it’s that good. Granted, the reason I think why you’re asking is because the trial that was done was technically a phase 2 trial, where [there is] a lot of drug development and new combinations.
The people that are the most critical of statistics and evaluating successes are the ones that really want to see what we call big studies, phase 3 trials, randomized data, or you’re comparing the standard to something new and novel. Those are happening. The same drugs, the same study, more patients — it’s happening. We’ll get that information.
But on the same token, if I already have some information that shows me just how effective it is with a good number of people, I don’t want to wait. I want to do good and do well [for] these patients with these early successes that we’re seeing now. I think it’s here.
Who is eligible for quad-based therapy?
Cindy, TPS: When you’re talking about quads upfront, are we talking about all patients? How about frail, transplant-ineligible patients?
Dr. Lonial: I think it typically tends to be the transplant-eligible [patients]. If somebody is frail enough that transplant is not really an option for them, I’m a little concerned about whether you can really give them a quad.
There are some trials that are testing that right now and I’d like to see some of that data. In general, for the truly frail patient, the dara-len-dex (daratumumab, lenalidomide, and dexamethasone) combination is so good. Median remission is five years. It works regardless of age. That was evaluated in the MAIA trial.
I think that that’s a pretty good regimen and I’d like to see whether adding in bortezomib to make it four drugs really does improve not just death but [the] duration of response or lets us discontinue therapy at a certain point, which would be a huge step forward for that patient population.
Cindy, TPS: We’re talking about dara-len-dex upfront for the frail as opposed to RVd upfront. Is there a role for RVd now? Should it be a quad or dara-len-dex?
Dr. Lonial: I think there is a role for RVd in the frail patient, with weekly bortezomib in a patient that may have [a] high-risk disease. I still do believe that the proteasome inhibitor adds benefit there.
I don’t think carfilzomib is necessarily the right drug [for] a frail patient. I am still using RVd, in the beginning likely without dara, but certainly willing to add it in if I need to, if we don’t get where we want to go.
What does it mean to be high-risk?
Cindy, TPS: What do you mean by high risk?
Dr. Lonial: There are both clinical and laboratory features of high-risk myeloma that I think people should be aware of.
An elevated LDH, lactate dehydrogenase, is one evidence of that. Circulating plasma cells [are] another laboratory evidence of extramedullary disease. Genetics, meaning FISH (fluorescence in situ hybridization) testing, looking for certain high-risk genetics on the myeloma cells. Things like 17p deletion, where you’re missing p53, 4;14 translocation, 14;16 translocation. In general, those are considered high-risk features.
On the clinical side, patients that present with a lot of myeloma outside of the bone marrow, extramedullary disease if you will, tends to be high-risk disease as well. Some of these characteristics you can identify on lab tests. Some of them you can identify on exams or imaging. Those are the general rules that we use to try and evaluate risk at the time of diagnosis.
Side effects for different drug combinations
Cindy, TPS: The other thing that patients always are concerned about are side effects. Are there more side effects with the four drugs than [with] the three? What about quality of life? What are you seeing in your clinic?
Dr. Costello: The addition of daratumumab to any of these regimens, fortunately, is a reasonably well-tolerated medication. It is initially a little bit more inconvenient because of the frequency of the dosing.
This drug is given once a week for eight weeks then every two weeks for another eight times. After those first six months, it goes down to once a month, which is a very attractive option for patients. They can just come in once a month, get their blood drawn, get a shot, and get out of there. From a perspective on [the] quality of life from inconvenience, I think it’s a really nice option.
The greater side effect we think about — there’s probably two, I would say — that we’ve learned a lot in the midst of a COVID era.
One is [a] very small risk: 1 out of 10 patients with the first injection may have what we call an injection-related reaction, where patients may, kind of like a bee sting, have a variety of reactions.
Like a bee sting, you may get a little red spot, but some other people may need to have an EpiPen. With your first dose, we have to kind of stare at you a little bit [to] make sure that you’re not having those reactions. After that first administration, the likelihood of having a reaction is somewhere about 1 to 2% thereafter, so very low. The reaction risk is small but important.
The second one — and I think it’s a little bit more relevant these COVID-era days — is that multiple myeloma patients inherently have a weakened immune system. Their immune system is so busy making myeloma that it’s not making adequate amounts of your normal immunity.
If you take a drug that’s designed to kill the immune system problem, you’re going to take some innocent bystanders with it. The daratumumab is going to try and kill all those myeloma cells, but those myeloma cells are plasma cells. Plasma cells are designed to make the weapons you need to kill the bad guys, whatever it is — flu, COVID, pneumonia, whatever.
If we are taking patients who already have a somewhat weakened immune system or [are] trying to get their immune system to build back up, there is going to be some effect on the immune system that puts patients more at risk for getting infections.
It’s important to make sure we are prepared for that. Vaccinating against the handful of different things we know are important for myeloma patients, whether it’s COVID, flu, or pneumonia, and sometimes using preventative antibiotics when patients are first diagnosed.
I’m glad to say that unlike other medications that we use with myeloma that cause neuropathy where you have numbness, diarrhea, or severe fatigue — things that really can affect your day-to-day lifestyle — I don’t think daratumumab affects it as much.
The necessity of stem cell transplant (DETERMINATION trial)
Cindy, TPS: We have all these wonderful drugs that you’ve been talking about now. In the era of these novel therapies, is stem cell transplant still needed initially?
Dr. Costello: The million-dollar question. It’s ironic because it keeps getting asked. I think everyone is so hopeful that we can get rid of auto transplants because we have all these new medicines. Every time a new medicine comes out, the question is posed. A trial is done to say, “Do we still need [a] transplant or is this better?”
That’s what this trial was designed to do. It took patients who were eligible for transplant, divided them in half, and gave everybody the same medicine: our triplet combination of Revlimid, Velcade, and dex.
[Then they] said, “You get this and you go to transplant. You get this and you don’t go to transplant. Let’s see what happens between those two,” with the idea of looking at [if] one group [is] going to have their myeloma come back sooner than the other group.
The DETERMINATION study was the U.S. version of it. The French had their own version and they’re always ahead of the game with us with clinical trials. They were able to complete enrollment, get the results, [and] publish it well before we did.
They showed that patients who got [a] transplant stayed in remission longer than those who didn’t. But after looking at the data for a handful of years, what they saw was that there was no difference in how long people lived.
[There are] lots of arguments about whether that is important — and one would argue yes — [and] whether enough time had passed by to say, “Here we are. We keep applauding and patting ourselves on the back for how well these treatments are working. Maybe we haven’t had the full time pass by, enough to say that there’s going to be a great difference in survival or not.”
When the Americans did theirs, the only subtle minor difference was that after [the] transplant, patients stayed on Revlimid maintenance indefinitely, as long as the maintenance was working.
If they did not go [for a] transplant, they stayed on Revlimid as long as it was working, which was different from the French. They only took it for 12 months and then stopped.
There were a good number of people who stopped therapy and often never had progression for 6 [to] 7 years. What the American side of the trial showed was similar. The transplant group stayed in remission longer.
The survival was no different, but there did seem to be improved time to staying in remission because, we think, of the longer-lasting use of the maintenance Revlimid.
I think it begs the question: is it that we need to get rid of transplant or is it that transplant is complementary? They parsed through that data left, right, up, and down to try and understand: was it the blondes who did better, was it the African Americans who did better, or [did] someone who had different kidney function do better?
[They] tried really to see: is it a general statement we can make across the board? I think the thing that was the most helpful for me to try and parse through whether or not transplant was important or still has a role… While I would love to know that it saves lives, let me hearken back to my “the first cut is the deepest” comment.
If we are really trying to make a deep impact in myeloma when it’s first diagnosed with the presumption that that’s going to allow for the longest periods of remission until the next newest and greatest comes out, then it’s pretty clear the way they parse the data to say that those who had transplant are more likely to get to what we call MRD negativity, minimal residual disease, which is [myeloma] way under the surface.
We have lots of tricks to count myeloma. I can do a bone marrow biopsy instead of my pathologists. They look under the microscope and say, “Yep, I see it. Nope, I don’t.” But in 2023, shouldn’t we have super high-tech technology that can look for myeloma in the smallest little micron of DNA?
Dr. Costello: We want to try and get rid of every last bit of myeloma because those patients, we can tell time and time again now, are the ones who are staying in remission the longest.
The DETERMINATION study was helpful for me to say we’re not saving lives. We’re not letting people, as far as we know, live longer because of doing a transplant, but we are having patients stay in remission by doing it.
Maybe we need more time to pass by, maybe we don’t. I think for the meantime, transplant really seems to me — disclaimer, I’m a transplant-er — that it’s complementary. I think it works with our novel agents, not better or worse than our novel agents.
Dr. Costello: Maybe we can try and figure out if our initial treatments didn’t do the job, maybe that’s the group of people who should proceed. So stay tuned. Lots to come.
Dr. Lonial: I think that with the results of the DETERMINATION study, it’s pretty clear to me that even with good drugs, transplant continues to offer [a] benefit.
There are a lot of folks that say, “Well, if you’re already MRD-negative [and] it’s cycle 4, maybe you don’t need the transplant.” We actually don’t have any data that says that. My goal is to maximize the duration of that first remission because the myeloma is never more sensitive than it is at the time of the first presentation.
By the time it relapses once or twice, you may lose the ability to gain the benefit from high-dose therapy, really high-dose melphalan. Certainly, at our center, we encourage patients to go into transplant in the first remission.
IVIG and daratumumab
Cindy, TPS: What about the use of IVIG with dara? Is that being used at all?
Dr. Costello: It is. I call [IVIG] a magic trick to try and build your immunity up a bit. Whether your myeloma is not making enough of an immune system or the treatments have compromised your immune system, your IgG, which is one of your weapons to kill the bad guys, can be decreased, can be accidentally killed, [or] can [be] whatever to suppress your immune system.
If your immune system is weak because your IgG levels are low, why don’t I just give you some IgG? That’s what IVIG is: intravenous immunoglobulin. If I can give you some booster to your immune system, perhaps that will prevent some of these infections from happening.
Historically, the way IVIG has been approached is to say if someone has severe, recurrent, life-threatening infections, those patients should receive IVIG. As we’re getting more and more aware of some of these infections that can happen with a variety of different medications that are out there for multiple myeloma, I know I have become much more liberal with my IVIG use because I think it could only potentially help.
Dexamethasone
Cindy, TPS: Let’s talk about this other drug that’s been around forever. As a matter of fact, I think in ancient times it was the only drug used to treat myeloma: dexamethasone. It’s always part of every combination.
Some studies being presented show that in the frail population, after a couple [of] rounds of therapy, we can maybe start lowering or dropping dex. Can you talk a little bit about that, too?
Dr. Lonial: In my experience and those of many of my colleagues, when we use dex, particularly in older, frailer patients, we tend to use a lower dose and for a shorter duration of time.
In my mind, the maximum benefit of dexamethasone is the first four to six months. I will often start to taper after the first or second cycle to try and get to lower doses and then hope to be off between month 6 and month 12.
That approach is something that many of us are doing in general. [For] patients getting daratumumab, for instance, the label says dex before and after the dose. We only have to do that for the first two cycles at the most then you can get away with dex around daratumumab.
The same with Tylenol and Benadryl that is often used as pre-med. I know a lot of people say, “Benadryl knocks me out for the next 6 to 12 hours.” After the first few doses of dara, you don’t really need that anymore.
Some of that is just experience, knowing that that’s what we did in the early trials, and that it’s okay to do it now. If you’re not seeing somebody that sees a lot of myeloma, you may just be on a plug-and-play where everything just gets recycled from cycle to cycle without necessarily reducing or taking them off to make life easier for the patient.
Dr. Costello: Dex is clearly the drug that everyone loves to hate. I think it’s important to say that dex is an oldie but a goodie. It’s been around for a long time. It is not a chemo, but it is designed inherently to kill myeloma.
That’s an important part because patients oftentimes ask, “Well, can I just stop it?” I want to say, “Yes, but remember, consider this part of your treatment regimen also.”
It is hard. I’ve heard people say, “It’s a dex day,” and I look at the spouse or the caregiver and say, “How’s it going?” Because that can affect your quality of life more than any of the other treatments do. People plan out their lives around the days they’re taking dex or the days after their dex.
It behooves us to really understand the importance of dex for all of these regimens because if it is playing a huge role in killing myeloma, then sometimes, it’s worth it.
If we are using it for an initial period of time to make a dent in the myeloma, for example, if we can get people off dex and continue the rest of the treatment, sometimes that makes it much more manageable for everyone across the board, let alone older, frailer patients.
At ASH, we heard about a trial [that] was one of the first, if not the first, randomized trial that was done specifically for frail myeloma patients. This trial took frailer patients, divided them in half, and said, “One half, you’re going to get Revlimid and dexamethasone. The other half, we’re going to do Revlimid, but instead of the dexamethasone, we’re going to do daratumumab.”
It’s similar to the MAIA study we’ve talked about when combining daratumumab and Rev, but this time with the hope of using as little dexamethasone as possible to see if these two groups, both receiving two medicines, can have good outcomes still without using the steroid in the study arm.
Now, I’ll say that these patients did get dex for the first two cycles, I think it was. That’s important. I think dex plays a role in helping to mitigate reactions to the daratumumab. Beyond that, maybe we can get rid of it.
They compared these two groups and said, “Dara-Rev, Rev-dex, how does it go?” Again, the dara-Rev group won. It is possible, we’ve learned, to get rid of the dex on our older, frailer patients.
[It] is [likely] going to be practice changing to say if we can drop the dex as soon as possible, patients may not have the same side effects: emotional lability, water retention, feeling swollen, appetite, [and] not sleeping at night.
If it’s not going to play a huge role, it’s in the best interest of everyone to get rid of it. This was the first time we’ve seen not only for a frail group but how we can successfully get rid of dex. I think it’s practice-changing.
Cindy, TPS: My house was always the cleanest on dex stays and most organized.
Dr. Costello: It just really affects everybody in different ways, but it’s life-changing.
FasTCAR T cell therapy
Cindy, TPS: Is there anything that we did not touch upon that you think we need to share about the newly diagnosed multiple myeloma patients from ASH?
Dr. Costello: One thing I really liked from ASH [is] super exciting. I don’t know if this is here to stay. It was only 17 patients, but the FasTCAR study in the newly diagnosed myeloma.
This was a Chinese group that developed a CAR T-cell. Right now, there [are] two different CAR T-cells that are approved by the FDA for refractory myeloma for patients who’ve had more than four prior lines of therapy. Again, these are patients who had myeloma [for] a long time. They’ve had lots of treatments.
Right now, it’s not available in the U.S. for patients who are just diagnosed. The Chinese designed a CAR T-cell and have started doing clinical trials, evaluating it for someone who’s just diagnosed with multiple myeloma.
In the U.S., the CAR T-cells that we have take five [or] six weeks, sometimes longer, to manufacture. [The Chinese study] figured out how to manufacture it in one to two days. The initial results they presented at ASH showed that it worked for 100% of the people they treated and 100% of those patients were MRD negative, meaning that they cleared out every last myeloma cell.
One of the things that we are very excited about is CAR T in general, but how can we use it earlier in the disease course? This is one of the first trials we’ve seen where somebody is trying exactly that with what seems like good success. Disclaimer: it’s a very small group of people. To be determined, but exciting.
Cindy, TPS: It was exciting. I like the idea of the FasTCAR because even the FasTCAR in the relapsed/refractory setting would be helpful because too many people are waiting too long or they don’t have [the] ability to wait.
Seeing a myeloma specialist
Cynthia, TPS: This is something that patients should be asking their doctors if their doctor didn’t tell them. You’re always giving us this little pep talk that all patients at some point should go see a myeloma specialist. Can you explain that again?
Dr. Lonial: The field is moving really fast. Things [change] once, twice, three times, or 10 times a year.
We’ve had multiple drugs approved in the last four years. Even through COVID, we still saw drug approvals. I think that the field is moving fast enough that if you have a really good general oncologist, they may be able to keep up to date, but they may not know the latest and greatest.
For that reason, I think having a myeloma center of record, if you will — a place that’s close to you, a team you feel comfortable with — that can partner with your local oncologist really guarantees that you’re getting access to the latest and greatest agents or combinations [and] that your team knows what approaches are going to be the most forward-thinking approaches to keep you going for the longest period of time.
Conclusion
Cindy, TPS: We talked to Doctors Lonial and Costello about newly diagnosed myeloma patients and treatment options for them. We learned about transplant-ineligible patients and the MAIA trial. We’ve talked about transplant-eligible patients, the GRIFFIN trial, and different ways to modify treatment. We also talked about stem cell transplant and if it’s really necessary.
It’s really important to be actively involved in your care. Take some of these points of information and have discussions with your doctor to see what may be the best treatment options for you.

Special thanks again to Janssen for its support of our independent patient education content. The Patient Story retains full editorial control.
Multiple Myeloma Patient Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...





