High-Risk Smoldering Multiple Myeloma Highlights from ASH 2022
What Newly Diagnosed Patients and Caregivers Need to Know

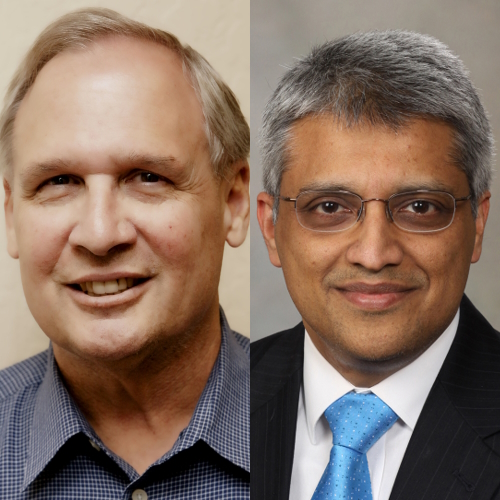
Multiple myeloma patient advocate Jack Aiello has been living with myeloma for 28 years.
In this conversation, he speaks with Dr. Shaji Kumar, a hematologist at the Mayo Clinic whose research focuses on the development of novel drugs for the treatment of myeloma.
They discuss the difference between smoldering myeloma and active myeloma, the determining factors of high-risk patients, and what high-risk smoldering patients can do to delay or possibly avoid progression to active myeloma.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- What is smoldering multiple myeloma?
- The difference between smoldering myeloma & multiple myeloma
- What is the ASCENT trial?
- How long until SMM patients are cured?
- Are there still trials open for high-risk smoldering patients?
- Asking your doctors about clinical trials (high-risk smoldering patients)
- Conclusion
- Multiple Myeloma Patient Stories
Introduction
Jack Aiello: I’m with The Patient Story. I’m a myeloma patient and have been for 28 years. I have followed this field very closely and always know that there’s more to learn.
Dr. Shaji Kumar: I’m a hematologist at Mayo Clinic in Rochester, Minnesota.
What is smoldering multiple myeloma?
Jack: Around 30,000 oncologists, researchers, physicians, pharma reps, and more from around the world attend the annual American Society for Hematology conference, also known as ASH, to hear the latest myeloma research from clinical trial investigators, like Dr. Kumar.
We’re going to primarily focus on a topic of myeloma called smoldering myeloma and that’s important because it’s a precursor to myeloma, although you may have never been diagnosed as smoldering.
Dr. Kumar, can you explain the differences between smoldering myeloma and multiple myeloma? And what determines high risk for smoldering vs. high risk for myeloma?

Dr. Kumar: With myeloma, we have precursor stages that clearly exist before patients actually get active multiple myeloma.
What we have learned is that the process that eventually leads to [the] development of active myeloma probably happens sometime in the 30s for many patients. We think it takes an average of about 15 years for that initial seed, so to speak, to grow into a stage where it is actually creating problems like active multiple myeloma does.
There are two distinct stages within this precursor phase. One of which is called monoclonal gammopathy of undetermined significance, essentially saying that you can find that initial condition. We can find some abnormal plasma cells, but they’re quietly sitting in the bone marrow, making protein that we can detect in the blood, which allows us to identify and diagnose this condition, but not really doing any major damage that we are aware of. We know that in some people, it can lead to some symptoms other than what we see in myeloma.
It’s important to note that this monoclonal gammopathy of undetermined significance is not something that is uncommon and certainly increases with age. In fact, if you take 100 people who are 70 years or older, you’re probably going to find that eight to ten of those people will have a monoclonal protein in their blood, suggesting that they do have this early condition that is sitting there.
We also know from long-term studies that [for] the vast majority of the people, eight out of ten people with that monoclonal gammopathy, it will amount to nothing. People will just live their normal life, a normal length, without it ever becoming a problem. But for the other two out of the ten, it can evolve into something that needs something to be done to it and that is often multiple myeloma.

When patients develop multiple myeloma, clearly they have damage to their body because of this abnormal group or collection of plasma cells or myeloma cells which have become cancerous. They can destroy the bone, produce high amounts of protein that get deposited in the kidneys and cause renal failure or kidney malfunction, can cause high levels of calcium, [and] can cause people to be anemic.
In some people, we can certainly identify them before these things happen or identify them at a stage where these things are very imminent and we can start treating them. But those definitions overall together [are] what you would call active myeloma or symptomatic myeloma that clearly needs treatment.
Wedged in between active myeloma and monoclonal gammopathy of undetermined significance or MGUS are people with what we call smoldering multiple myeloma. These are patients or individuals where the amount of plasma cells or proteins [has] progressed to a point where there is [a] considerable amount of those cells in the bone marrow, typically defined as more than 10% or an M protein in the blood that’s more than 3 grams.
Over time, what we have learned is these people are in between the markers and myeloma; [it] is not a distinct diagnosis, so to speak. It’s more of a collection of people who truly has more MGUS or more myeloma. We just can’t do one test and say you are more myeloma-like or you are more MGUS-like. We just have to depend on time for things to declare itself.
For at least half or two-thirds of people with smoldering myeloma, it is okay to sit and wait, but the other third may be at a higher risk of progressing. Those are the individuals [whom] we really think we could do something with the treatments we have and actually make a difference.
When we say make a difference, we mean [delaying] the time they actually get active myeloma, maybe [preventing] them from ever getting active myeloma, or maybe [curing] some of those people and we can just forget that they will ever get myeloma and not even worry about it again.
How do we identify those people? We need to be able to get to them in as precise a fashion as we can. We want to limit the number of people who might get exposed to these treatments, which may not have the same benefit [to] others.
One of the ways we do that is to use the International Myeloma Working Group criteria. Laboratory markers tell us the risk of that individual getting active myeloma in the next two years. If you think it’s more than [a] 50% chance, we feel like we need to do something about it.
There have been large phase 3 trials that have been done, which clearly show that there is a rationale for intervening in those people.
The difference between smoldering myeloma & multiple myeloma
Jack: You’re saying there is a method to determine high-risk smoldering. What’s the difference between them?
Dr. Kumar: We are talking about a stage that you may or may not have gone through. Not everybody has to be in a smoldering stage before they go from markers to myeloma, but many would have gone through the stage.
What we are trying to do here is to see [if] we can do something different for future patients, a course that is different than what you all went through.
The most critical thing that is different is, of course, whether it’s doing damage to your body — bone lesions, kidney problems, anemia, high calcium — or not. There are some individuals who may not have those characteristics, but the risk of getting that is very high: 80% plus in the next two years. Those people, we already consider as active myeloma and not smoldering anymore.

Jack: High-risk myeloma patients are more determined by mutations of certain chromosomes and things like that, right?
Dr. Kumar: That is right. When you talk about high-risk multiple myeloma or active myeloma, we’re talking about people with chromosomal abnormalities (translocations or 17p deletion), high LDH levels, or if they have stage 3 [based on] the International Staging System.

What is the ASCENT trial?
Jack: At ASH, you presented abstract 757 on the ASCENT trial for high-risk smoldering myeloma patients. What was this trial about?
Dr. Kumar: When you think about doing something different with people with high-risk smoldering, what’s our ultimate goal? We want to make sure they never get myeloma and they never have to get myeloma-type treatment that is often given continuously for long periods of time.
There are two approaches. One is obviously to give less intense treatment than what we do in myeloma and try to kind of kick the can down the road, so to speak. The other option is since we caught it so early, to see [if] we actually just get rid of it completely and maybe never even worry about it.
The former approach is what has been taken in the large phase 3 trials that the Spanish group did [and] the cooperative group in the US did. Both trials showed that people with high-risk smoldering myeloma, if you treat them with lenalidomide or lenalidomide and dexamethasone — far less intense than the three- and the four-drug combinations we use for patients with active myeloma — those interventions actually delay the progression to myeloma and, in fact, make people live longer.
What we’re really trying to do with the second approach is trying to cure the disease. There have been some trials looking: can we use more intense treatments and give it for [a] short duration to try and get rid of those myeloma cells?
The Spanish group did a trial called the CESAR trial, which was also updated at ASH [2022]. They treated people with the combination of carfilzomib, lenalidomide, and dexamethasone (myeloma-type treatment), did [a] transplant (this trial only included transplant-eligible patients), and then get them on maintenance treatments like what we would do for myeloma but give it over a defined period of three years instead of giving it continuously until [the] disease comes back.
With a longer-term follow-up [of] four-plus years, what they have seen is only five of the 81 or so patients that they enrolled have progressed to active myeloma. [For] many of those people who have progressed, the progressions have been predominantly just biochemical, meaning the M spike goes up [but] they don’t actually get myeloma.
What the ASCENT trial did was take a slightly different tact. Knowing that a significant number of people cannot go do a stem cell transplant, instead, we will do a monoclonal antibody, like daratumumab added to carfilzomib-len-dex. We use carfilzomib, lenalidomide, daratumumab, and dexamethasone for 12 cycles and then gave them maintenance for 12 cycles for daratumumab and lenalidomide. Basically, two years defined duration of treatment in patients with high-risk smoldering myeloma.
What we found was these results are quite similar to what we have seen in [a] myeloma setting. We get deep responses. Almost two-thirds of the people actually get what we call a stringent, complete response, meaning we can’t really see any protein. We can’t really see any myeloma cells under the microscope.
More importantly, nearly two-thirds of the people who got there also were minimal residual disease negative. We cannot even detect myeloma cells in the bone marrow by using highly sensitive approaches. It seems like this approach does manage to eradicate at least a significant proportion of the myeloma cells in the bone marrow.
The question that’s going to be really critical for us is: does this eradication mean that these cells will not grow back like what it does in myeloma? Only time will tell. I think both studies will continue to follow these patients over a long period of time to see if this emerging activity that we have seen is something that can be sustained over a long period of time without continued treatment.
How long until SMM patients are cured?
Jack: How long do you think you need to follow these patients before you can say these patients are cured?
Dr. Kumar: That is a good question and I don’t know if we all know the right answer to that. But the longer we can go without the disease coming back, I think the higher the probability that we may have actually eradicated this.
I’m just going to put a number out there. If in 10 years from the start of the treatment — that means eight years without any treatment — the myeloma hasn’t reared its head back up, I think I would call it successful. Obviously, each passing year is more and more of a success.
Jack: I guess we hope to see some plateau of the curve where people are no longer relapsing if you will.
Dr. Kumar: I think that is going to be the key because, in myeloma, we know that even if they get to be MRD negative, that curve never becomes flat. People continue to kind of fall off because of myeloma coming back. We’re hoping that it would be a different picture here, like what we see with some other hematological cancers like lymphoma and so forth.
Are there still trials open for high-risk smoldering patients?
Jack: At the IMF ASH symposium, Dr. Vincent Rajkumar said that treatment for all high-risk smoldering patients should either be Revlimid with or without dexamethasone or a clinical trial. Do you agree? Are there still trials open for high-risk smoldering patients?
Dr. Kumar: Yeah, I completely agree. We have to always build upon what we have learned and what we have learned in smoldering from two large trials that doing something is better than not doing anything. Giving them at least lenalidomide or lenalidomide with dexamethasone [not only] prevents the myeloma [from] coming back, [but] the Spanish trial has actually made people live longer. We owe it to our patients to have that discussion about the choices.
Ideally, if I had the option, I would definitely put everybody on clinical trials rather than using that treatment because there’s so much more to be learned. We don’t know if lenalidomide-dexamethasone is the right approach. Should we treat them like myeloma with three drugs, which is the focus of the ECOG trial?
The SMM trial is currently enrolling so that is a trial that can be considered. There’s [an] isatuximab trial that is currently accruing looking at isatuximab-len-dex versus len-dex. There [are] also multiple smaller trials in different institutions that are looking to try and see: are there specific combinations or specific drugs that might actually provide a meaningful benefit for patients with high-risk smoldering? It remains an area of active investigation so I would strongly encourage everyone to consider enrolling in clinical trials.
Asking your doctors about clinical trials (high-risk smoldering patients)
Jack: The important thing for smoldering patients is to ask their doctors: are they considered high-risk smoldering or not high-risk smoldering? If they are high-risk smoldering, they should be asking their doctor about trials. Most of these trials that you just mentioned can actually be done locally. They don’t necessarily, I think, have to be done at major cancer centers. Is that correct?
Dr. Kumar: That is right. That’s especially true for the cooperative group trial like the one we have in ECOG. It should be open in pretty much all the community cancer centers across the country.
Conclusion
Jack: Thank you so much. I’ve learned more about smoldering as well. As I said, you can always learn more about myeloma and different avenues of myeloma treatment. Any final takeaway from ASH that you want to mention?
Dr. Kumar: There’s a lot of data presented at ASH. Spanning all the way from simple questions like, “Should we be doing a bone marrow in patients with MGUS?” to obviously, “How do we treat those people or new drugs that would be potentially effective in people who have seen it all?” It’ll probably take hours to go through all that important data.
There are so many new therapies that are coming through that are so effective, especially immune therapies. We started seeing some of those being employed in the first-line treatment and the first relapse. In five years, the treatment of myeloma is going to look very different than what we are doing today.

Jack: Dr. Kumar, it’s always a pleasure talking with you and I want to thank you so much for providing your insights to The Patient Story.
Dr. Kumar: Thank you, Jack.
Multiple Myeloma Patient Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...