Al Roker’s Gleason Score 7+ Prostate Cancer Story
From TV Star to Patient Advocate
Famous Weather Anchor Shares Prostate Cancer Story, Gleason Score 7, and Passionate Plea: “Please Get Screened!”

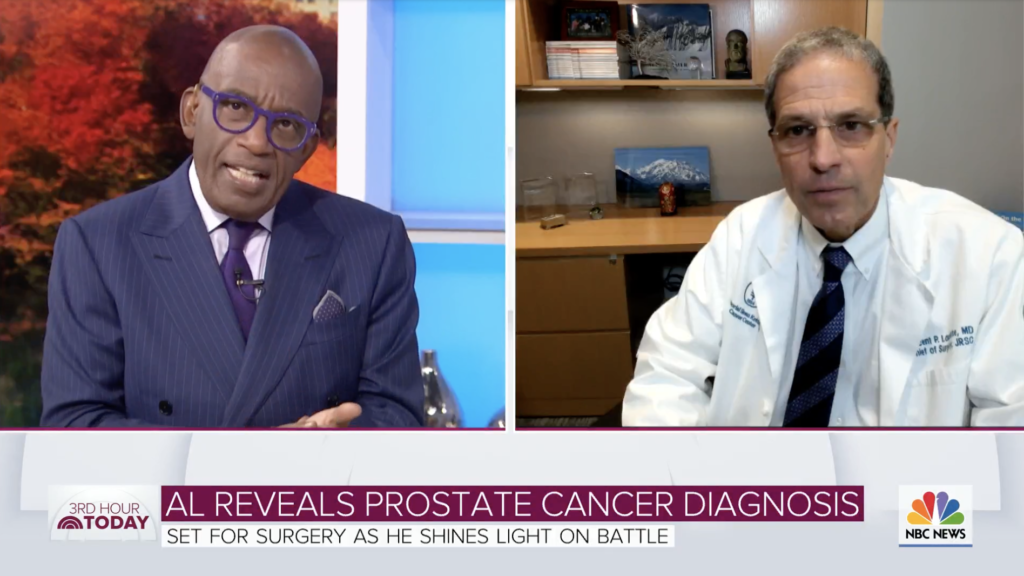
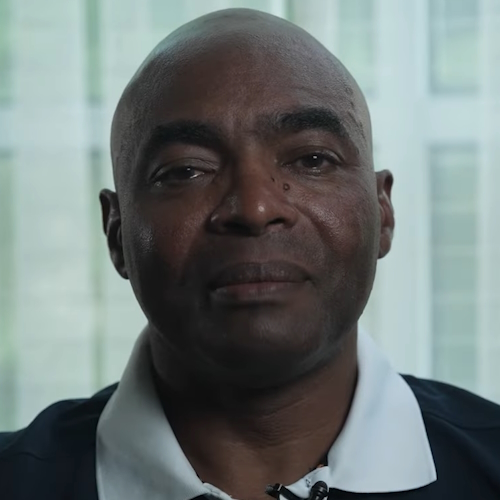
Al Roker is a celebrated TV journalist, personality, Weather & Feature Anchor for TODAY and the co-host of 3rd Hour of TODAY, and now a prostate cancer thriver and patient advocate.
Diagnosed at 66 years old with an aggressive form of prostate cancer, Al was able to catch it early through a routine PSA test at his annual physical. After surgery, the husband and father has no evidence of disease, and has used his celebrity to send a clear message to other men to screen for prostate cancer with the PSA test and digital exam.
This message is especially important for African-American men to hear, as they are disproportionately impacted by prostate cancer. Thank you, Al, for sharing your incredibly powerful voice to uplift others.
- Name: Al Roker
- Diagnosis (DX)
- Prostate cancer
- Gleason score: 7+
- Aggressive
- September 2020
- Age at DX: 66 years old
- 1st Symptoms: None, detected by routine PSA test and digital exam
- Treatment
- Prostatectomy: surgery to remove prostate, surrounding tissue & lymph nodes
- Laparoscopic (robotic) surgery
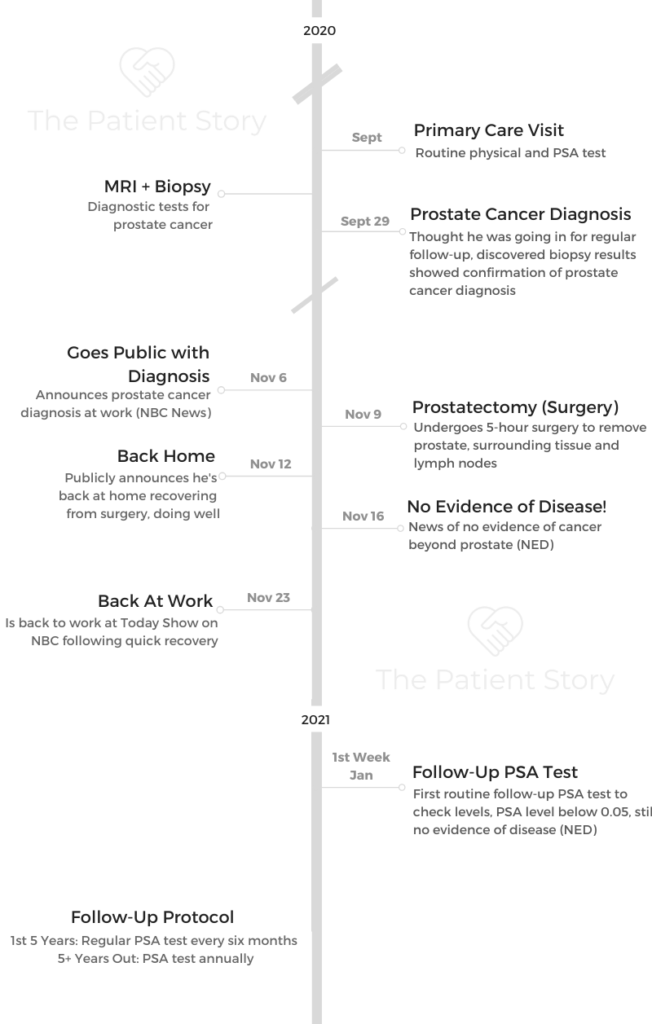
- Follow-Up Protocol
- First 5 Years: PSA test every 6 months
- 5+ Years Out: PSA test annually
- First Tests & Scans
- Getting Diagnosed
- Surgery (Prostatectomy) & Follow-Up
- Al the Advocate
- What’s your message to men who are reluctant to get screened for cancer
- What’s your message specifically for Black men, who are 50% more likely to get diagnosed with prostate cancer and 2x as likely to die from it
- Can the messaging to the African-American community be better
- The importance of access to healthcare for communities of color
- How important is it to get more diversity in clinical trials?
- What's the importance of the patient story of people like us speaking out of industries listening to patients?
- Al Inspired Others to Share Their Stories
- Prostate Cancer Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
First Tests & Scans
How did you know to test for your PSA?
You just knew about it. It was one of a battery of tests that your doctor always took along with the digital exam which everybody knows Moon River kind of thing *sings song*.
I knew about the PSA. It was just like your cholesterol and your blood pressure, and it was just one more metric that you measured your health by.
What was your Gleason score
I had a 7+ Gleason score. That wasn’t terrific obviously, but again it also speaks to having access to good healthcare. They could have easily said, “Well, let’s just watch this,” but it was like, “No. Let’s do an MRI.”

What were the scans and biopsies you underwent for diagnosis
Did the MRI. Didn’t show any target areas. It was like, “Let’s [still] do a biopsy.” That’s when we found the cancer.
It wasn’t really until I did the genetic testing on it at Sloan Kettering that it was like, “Oh, this is pretty aggressive.” There was a lot more than the biopsy showed.
How were the MRI and the biopsy
Look, it’s not a walk in the park per se. The MRI is a little easier. If you’ve ever been in one of those MRI machines, you’re lying there, you’re still. It’s, I don’t know, about 45 minutes, almost an hour of constant noise.
To be perfectly honest, it wasn’t so bad for me. I think I literally took a nap till we were done because I’m always up early.
The biopsy, you have to get anesthesia and all that stuff. That’s never pleasant, but it’s important, so you put up with it.
I’ve been through so many surgeries in the last several years that it was like, “Okay, what’s one more, here we go.”
The most annoying part about it is really the IV needle, but other than that, you’re under anesthesia so you don’t really realize it. Then you wake up, and boom, you’re done.
Getting Diagnosed
The benefit of “aggressive” doctors
I was very fortunate. I had access to good doctors, and that’s not to say other people’s doctors aren’t good or anything like that.
I had doctors who are good and aggressive. As aggressive, if not more aggressive than the cancer itself. I think that if it had been more of a wait and see, my patient story might have been a little different.
Describe the appointment when you got the diagnosis
It was one of those things where I did the biopsy and made an appointment for follow-up at the same time. I didn’t really think anything of it. I just assumed. I guess I thought that if there was a problem, they were going to call.
My doctor came in and closed the door, and he said, “I always like to have these meetings face to face.” It was my first like, “Oh. Wait. What? What does that mean?”
Then he went into it. Truly, I was thinking, it wasn’t even really about the cancer as much as I was like, “Oh, my god. My wife is going to kill me.”
Obviously, she’s very compassionate. She wouldn’t want me getting that diagnosis by myself. Realistically she’s thinking, “What’s the doctor going to think about me as a wife not being there to be there with her husband to get this potentially life-changing news?”
I took in what he said but I just kept thinking, “She’s going to kill me.” If the prostate cancer doesn’t, she will!

How did you break the news to your family
I called my wife and said, “Okay, I’m on my way back.” She said, “What did the doctor say?”
I had waited till I was almost home. Then I said, “I’m just around the corner. Let me get home.”
She goes, “I don’t like the sound of that.” I said, “I’m literally 30 minutes away. Then we can talk.” She was upset obviously.
We waited till the weekend to tell our kids. I’ve got a 33-year-old daughter from a previous marriage, and then we’ve got a 22-year-old who’s in college in Paris, and our 18-year-old son who lives with us here. The family Zoomed and I explained.
They were very upset, obviously. I said, “It’s okay. Doctor said, yes, it’s aggressive. I’m not going to sugarcoat this, but he said we caught it early.”
»MORE: Breaking the news of a diagnosis to loved ones
At that point, I hadn’t decided on treatment. In my heart of hearts, I’d decided I was going to have surgery, but I wanted to do due diligence only because I’m one of those people.
I had the idea that’s just in there and, “Well, we’ll do the radiation, and the CyberKnife, and there’s the focal thing, and then we have to wait to see that it…” I’m like, “No. Let’s just get rid of this.”
My son, Nick, is very sweet. He’s a sweet boy, and he’s got some learning issues. He was really upset and was kind of reacting.
We realized it was happening right about the same time as Alex Trebek. He was conflating pancreatic cancer with prostate cancer. I think he thought I was a goner. It’s like, “Nope. Dad’s going to be around a while longer to bother you.
It was tough on my middle girl because, at the time and still, she was stuck in Paris because of the pandemic so she couldn’t come over. They’ve been very supportive and happy that everything’s turned out okay.
»MORE: Parents describe how they handled cancer with their kids
Surgery (Prostatectomy) & Follow-Up
Describe the surgery (prostatectomy)
I had the surgery done at the beginning of November. I had a shoulder replacement in August, and I’m still doing rehab on that.
Whereas the most difficult part of this has been, you come home and you’ve got a catheter for a week, which it’s not the worst thing in the world, though not the greatest thing.
It was less of a problem than I thought. There are the issues of a little incontinence, a little erectile dysfunction, but that’s rectified itself.
What’s your follow-up protocol
Then in January, went for the bloodwork. The PSA level was below .05. Now every six months, I go get a PSA test and every six months thereafter, bloodwork, knock on wood.
ßIt’s five years with no problems, and then it’s once a year. You do bloodwork once a year anyway.

How did you process the news of no evidence of disease
Dr. Vincent Laudone was my surgeon, and he’s obviously a real pioneer in this area. Somebody like that has done a whole ton of these. He was very optimistic after the surgery.
We were doing pathology during the procedure. We took out the lymph nodes surrounding that area, didn’t see anything. I was already cautiously optimistic. You’re still waiting for that blood work. Once you get that, it’s a real weight off, and then you’re like, “Okay.”
Now the clock starts again for the next six months. You probably get a little anxious right before that, but here we go.
Survivorship: How do you manage waiting for the next test results
I always keep thinking that five minutes before the doctor walked in, I felt one way. Then five minutes or 30 minutes later, when I’m walking out the door to get in the cab, it was like always this kind of weird because I don’t really feel any different, but somebody says, “Oh, by the way, you have cancer.” Those three words.
Then all of a sudden, you don’t feel differently, you are different. It’s the same with this. You’re still going to be living every six months, but you’re alive. I don’t really think about it. It’s a good feeling.
»MORE: Patients describe dealing with scanxiety and waiting for results



Al the Advocate
What’s your message to men who are reluctant to get screened for cancer
I wouldn’t understand it. Listen, if you have problems finding healthcare or something like that, maybe, I guess. If you’re a guy who goes to the doctor once a year for the physical, you’re already there.
What’s the big deal?
Again, it’s that finger moment (digital exam). That was funny because all along doctors said whenever I had the exam, “It doesn’t seem swollen. You’ve got a small prostate,” which was great. If you’re going to the doctor anyway, why not?
What’s your message specifically for Black men, who are 50% more likely to get diagnosed with prostate cancer and 2x as likely to die from it
You can ignore it at your own peril, but if you love your family, love what you do, love the people around you, you’ve got to do this.

There’s no stigma to it. Just get it done. Make sure you’re going to be around for your family.
It is imperative.
There’s more research being done, but until that happens, you have to make sure you’re going to do what you can to minimize your risks of disease.
This is a disease that we’re more likely to get. You just have to do it. There’s no ifs, ands, or buts about it.
Can the messaging to the African-American community be better
I don’t know that it’s so much the messaging as it is access. Look, the current healthcare system is, I’m not saying this in a negative sense, but it’s a little bit of a factory to it.
Doctors, unfortunately, have to move their patients through. I’m not saying that these are not dedicated doctors and they don’t care about their patient’s health, they do, but by the very nature of the way the healthcare system works now, you can’t spend a lot of time [with each patient].
The importance of access to healthcare for communities of color
The problem with prostate cancer is, there are generally no outward symptoms, but if there are, you’re pretty well down the line with the progression of the disease.
I think making sure that in communities of color, where there can be medical treatment deserts, just like there are food deserts and pharmacological deserts, pharmacy deserts.
We have to make sure that there is access for this.

How important is it to get more diversity in clinical trials?
You look at what we just went through in the pandemic, when obviously, communities of color were far more impacted by the pandemic.
But when it came to the vaccine, there was a very huge push to have a real diversity in the folks who were tested so that we knew that this was safe across all ethnic groups, male and female, things like that.
I think from a research standpoint, especially given that this is far more impactful to men of color, the studies have to reflect that, as well.

What’s the importance of the patient story of people like us speaking out of industries listening to patients?
People have to, especially the medical industry. It’s, in a sense, kind of cut and dry, especially when it comes to diagnoses, treatments, medical interventions.
You tend to forget that these are people. I don’t think it’s a malicious forgetfulness. It’s just data and medical research treatment, there are a lot of data points, but those data points come from people.
That’s why personal stories are important.
Al Inspired Others to Share Their Stories

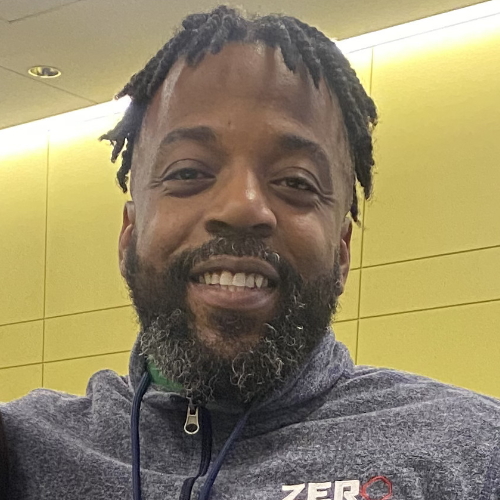
Clarence Seegars’ Prostate Cancer Story
When he read about Al Roker’s prostate cancer diagnosis, Clarence Seegars sent a message of support on social media. He wanted Al to know that he would be okay.
Hearing about it also inspired Clarence to share his own powerful story of getting diagnosed with prostate cancer.
Pictures Courtesy of: NBC News, Al Roker
Inspired by Al's story?
Share your story, too!
Prostate Cancer Stories
Eve G., Prostate Cancer, Gleason 9
Symptom: None; elevated PSA levels detected during annual physicals
Treatments: Surgeries (robot-assisted laparoscopic prostatectomy & bilateral orchiectomy), radiation, hormone therapy
Lonnie V., Prostate Cancer, Stage 4
Initial Symptoms: Urination issues, general body pain, severe lower body pain
Treatment: Hormone therapy, targeted therapy (through clinical trial), radiation
Paul G., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery), radiation, hormone therapy
Tim J., Prostate Cancer, Stage 1
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery)
Mark K., Prostate Cancer, Stage 4
Symptom: Inability to walk
Treatments: Chemotherapy, monthly injection for lungs
Mical R., Prostate Cancer, Stage 2
Symptom: None; elevated PSA level detected at routine physical
Treatment: Radical prostatectomy (surgery)
Jeffrey P., Prostate Cancer, Gleason 7
Symptom:None; routine PSA test, then IsoPSA test
Treatment:Laparoscopic prostatectomy
Theo W., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA level of 72
Treatments: Surgery, radiation
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Symptoms: Urinating more frequently middle of night, slower urine flow
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Al Roker, Prostate Cancer, Gleason 7+, Aggressive
Symptom: None; elevated PSA level caught at routine physical
Treatment: Radical prostatectomy (surgery)
Steve R., Prostate Cancer, Stage 4, Gleason 6
Symptom: Rising PSA level
Treatments: IMRT (radiation therapy), brachytherapy, surgery, and lutetium-177
Clarence S., Prostate Cancer, Low Gleason Score
Symptom: None; fluctuating PSA levels
Treatment:Radical prostatectomy (surgery)










6 replies on “Al Roker’s Gleason Score 7+ Prostate Cancer Story”
Very helpful information
I am wondering how Al treated his post surgery ED and incontinence? I am using physical therapy without much success
Al. Your story has given me hope….we’ve all been knocked out when we get the news but your face being put front and center has made me think about my treatment and many more men too. My only thing that gets me so mad is that every year I get a check up but my GP NEVER did a quick check of my prostate! My psa was alway low 2.09 last year. Why do men have to make a separate appointment to see a urologist to have this 10 second test. It should be standard procedure for our GP to do the test and if they feel anything…. Then send us to the urologist. All men out there don’t just trust a low psa.. make sure you get the prostate physically checked. Al I know with my “Life forecast “ I will see many more sunny days in my future!!! ♥️ I got this ! Fight fight fight everyone!
Thank you to all for your stories, caring.
Thank you Mr. Roker.
Mr roker I am very ecstatic that your cancer was caught in time and that you took care of it expeditiously. I admire you and have watched you for some years now. I find myself in the same boat now