Shirley’s Stage 3C High-Grade Serous Carcinoma Ovarian Cancer & BRCA1+ Story
Shirley shares her stage 3C ovarian cancer diagnosis, testing BRCA1 positive, and describing her experience undergoing surgery, chemotherapy, and maintenance therapy.
Shirley also highlights how she advocated for herself as a patient, how the diagnosis impacted her marriage, and how she managed cancer while parenting. Thanks for sharing your story, Shirley!

- Name: Shirley P.
- Diagnosis:
- Ovarian cancer
- High-grade serous carcinoma
- BRCA1+
- Staging: 3C
- 1st Symptoms:
- Pulling or cramping sensation during urination
- Pain during sexual intercourse
- Treatment:
- Surgery:
- Two debulking surgeries
- Preventative mastectomy
- Reconstruction
- Chemotherapy:
- Carboplatin & Taxol
- 6 rounds with infusions every 21 days
- Carboplatin & Taxol
- Maintenance therapy:
- PARP inhibitor
- Zejula
- Surgery:
Surround yourself with support. Reach out to people who understand. Find your tribe of people who get it.
It’s such a hard thing to process, but it doesn’t mean the end of living. It’s just thinking about life in new ways. Find people who understand that and can say, ‘Yeah, me too.’
Shirley P.

- Diagnosis
- Treatment Decisions
- Surgery
- Chemotherapy
- Recurrence and Second-Line Therapy
- Hair Loss
- Quality of Life
- How were you your own advocate as a patient?
- Managing work through treatment
- Paying for cancer treatment
- What was the lowest point mentally or emotionally?
- How has the cancer affected your relationship with your spouse?
- Talking to your kids about cancer
- Do you have advice for other parents?
- How important was it for you to have caregivers?
- It can be hard to ask for help. What advice do you have?
- What is your “new normal"?
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
My first symptom was probably a pulling or cramping sensation when I emptied my bladder. I thought I had a UTI or a bladder infection. It was intermittent. It wasn’t constant, so I just passed it off as something I would watch.
I have a five-pound chihuahua. She stepped on my abdomen one night in bed, and I thought, “Well, that can’t be right.” Then I started having pain more consistently when I went to the bathroom.
Then I noticed pretty significant pain with intercourse, and the pain eventually became constant. It was like this constant sharp ache.
My sister is a nurse, and I had asked her about it when I first started having the pain emptying my bladder. She said, “You just turned 40. Your bladder is a muscle. It’s probably just tired.”
I didn’t worry about it, but when the pain became constant, that’s when I decided I needed to do something about it.
I noticed all this stuff in early June, and it didn’t take long after the symptoms presented themselves for me to get everything going.
Hindsight being what it is, I realize now that I had been saying I was feeling bloated for a while. I felt like every time I ate, I was eating Thanksgiving dinner. I was always stuffed.

When did you go to the doctor the first time?
Throughout all of this, we went on vacation. It was probably the end of June or early July. We got through vacation, and I was still having symptoms. Around the 15th, I called my primary care because I couldn’t deal with it anymore.
I was wearing those heating wraps you use for menstrual cramps or back aches, and it was July in Florida, so I was not comfortable.
I couldn’t get in to my doctor for a couple of days, but the day after I called, the pain was just too much.
I just decided enough was enough, and I wanted to see if the emergency room could do anything for me.
I went in and explained my symptoms. They did lab work. I told them I went there because I couldn’t get into my primary care. They were pretty understanding.
When did you first hear “cancer”?
Based on my history and my basic labs coming back fine, the doctor said she was thinking colitis or diverticulitis, and she wanted to do a scan just to see.
She came back, and she closed the door. She sat down right next to me. They don’t usually do that, so I knew something was wrong.
She said, “I want to talk to you about the results of your scan. We noticed there were several masses in your abdomen, the largest of which is on your right ovary.”
I said, ‘Masses?’
She said, ‘We are concerned that these might be tumors.’
I was in shock, and of course I started crying.
I said, ‘What, you mean I have cancer?’
I had just lost my mom to a rare lymphoma ten months prior and was still grieving that loss. That was really my first up close and personal experience with cancer in general. I had to get composed.
She said it could be a number of different things, and she was concerned about a few of them, including ovarian cancer. She went to make me a disc of my scans and told me to call my gynecologist while I was sitting there. I did, and they got me in the next day.
»MORE: Patients share how they processed a cancer diagnosis
Treatment Decisions
Next steps at the gynecologist
First, they scheduled a transvaginal ultrasound. For years, I’d been seeing a physician’s assistant because she was just so nice. They wouldn’t let me see her for this particular appointment because they wanted me to see a doctor. I didn’t know of one, so they set me up with the first available.
It was my first time meeting him. The ultrasound technician was making faces and scrunching up her face, and she said, “I need to go get the doctor.”
He walked in and said, “Hi, I’m Dr. Miller. I’m sorry to be meeting you like this.”
Then he asked the lady what they were looking at. They were both making comments, and I asked if they could tell me what was going on.
He said they were seeing a mass, shadowing around my uterus, and an excess of fluid, which could mean cancer. He gave me the two things it could most likely be: peritoneal carcinomatosis and ovarian cancer.
I asked him about prognosis, and he said the peritoneal carcinomatosis is not really something you want to have.
He did tell me there was a chance that it could be benign, but the way the tumors were shaped made him pretty sure it was cancer. He told me I needed to go see a gynecologic oncologist.

Deciding on doctors
He said he could go one of two ways. He could refer me to someone who was the oldest game in town, or he could refer me to someone else who is very good but that could probably get me in sooner.
I asked him, “Who would you refer your mom or your sister to?” He said he would use either because they were both very good.
You found out it was ovarian cancer from the gynecologic oncologist
I went to the gynecologic oncologist two days later. She got me in on a Friday. My CA 125 came back, and she looked at all my scans. Based on all that, she said, “Obviously, we’ll confirm with surgery, but it’s looking like ovarian cancer is your diagnosis.”
She couldn’t get me in for surgery for a month. She said nothing was really going to change except my anxiety level. I thought that was important.
I asked her, “If you were me, would you go try to get into another office quicker?” I told her Dr. Miller had mentioned someone who was the oldest name in the game.
She rolled her eyes and said, “Yeah, Dr. Buckley.” He apparently was very well known.
Did you get a second opinion?
I wasn’t going to do it because I felt like I was cheating on my doctor.
I discussed it with my spouse and decided I would just call and see if they could get me in faster than a month. They had a cancellation a few days later, and they called me.
He made me feel much more at peace. He’s been doing it a long time, and there’s a reason he’s the best. He sat down and said he had looked at all my records and went through a game plan.
The thing that stuck out to me was the previous doctor said the surgery would take about eight hours, but he said it would take two or three hours. We asked him about it, and he paused because he was trying to be professional.
He said, “I’m sorry, but for someone to tell you that you need to be under anesthesia for eight hours for this surgery is just wrong. With what I’m looking at, it can be complicated, but eight to ten hours is just inexperience.”
The big thing was that he said, ‘I’m not sure what you want me to do. I’m assuming the other doctor told you everything, but I’ll be here to be a second opinion. I’ll talk to you about it or cry with you about it. I don’t need to do your surgery.’
He was so compassionate, and I said, ‘No, thank you. I want you to do my surgery.’
He didn’t want to wait. He said he could either do it two days later or a week after that. I would’ve loved to do it two days later, but I had to get family here because I have kids with special needs. Then I had my surgery on August 4th.
Do you recommend getting a second opinion?
I probably wouldn’t have if that first doctor could’ve gotten me in sooner. I don’t know for sure, but I think I would’ve just wanted to get the surgery done.
What I’m learning now, though, is you need to feel comfortable with your doctor.
You need to be able to trust them, and if you don’t, you should get a second opinion.
The first doctor I saw was very nice and knowledgeable, but when she said, “The only thing that’s going to change is your anxiety. Want some Xanax?” I just was like, “Huh, what?”
You can get that warm, fuzzy feeling from a doctor. There needs to be a connection with your doctor, just like with any other relationship.
»MORE: How to be a self-advocate as a patient
Surgery
Preparation for surgery
Dr. Buckley put me on clear liquids and a cleanse because there could potentially be bowel involvement. It was pretty awful for me. I had to do medical prep the night before.
I had to shower, and I wasn’t to use any lotion or deodorant or anything. I had to wipe myself down with special wipes [and] sleep in clean pajamas and clean sheets.
The next morning, I wasn’t allowed to shower. At the hospital, they repeated the wipes as I changed into my hospital gown. They gave me an antiseptic or something to brush and rinse my mouth with.
I had to put iodine in my nose to clean it. Then I got hooked up to the IV and all that good stuff.
How did you feel before surgery?
Terrified. I really felt like it wasn’t my life. I felt like I was watching someone else go through this.
I had the first surgery of the day, so I thought, “At least the doctor will be fresh.”
I had some family fly in to stay with the kids and be there for my spouse and all that, but still I was anxious. It felt surreal. I felt like I was going to wake up from a nightmare, and none of this was me.
Describe the surgery
Surgery went really well. It was very successful. I woke up feeling like I had gotten hit by a truck, but they had optimal debulking, which means they got everything they could see.
They didn’t have to take out any parts of my intestines, but there were spots there. Luckily, they got it all without resection.
There was a tumorous plaque covering my bladder. He had to remove that and repair my bladder. I had a catheter for a week.
Recovering from surgery
I was in the hospital for four days. The first day, I was still drugged up, and I felt great. About 24 hours later, I developed what’s called an ileus.
My bowels slowed down, and I started vomiting, and that was really uncomfortable with a nine-inch incision across my abdomen. I was pretty dehydrated, and my blood pressure was dropping.
All I can remember is the nurses standing there saying they needed to do something. I guess they gave me fluids and other stuff to get my pressure back up.
I also have an adhesive allergy. They had taped up the bandage across my stomach. On the sides of my abdomen, I had itching and blistering.
It looked like I had been mangled because when they took the bandages off, my skin went off with it. That healed pretty well, though. I don’t have any major scarring from that.
Long-term health from surgery went well.
I followed all the directions. I don’t overexert or lift anything. I wasn’t working full-time.

Chemotherapy
Describe your chemo regimen
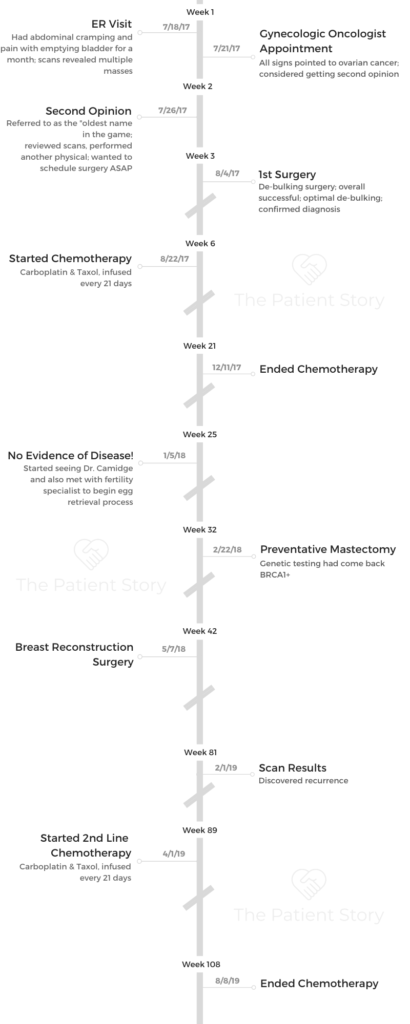
I had my port placed about two weeks after surgery. I started chemo on the 22nd of August. I had six rounds of carboplatin and Taxol, and I got infusions every three weeks.
I would take oral steroids the night before and the morning of infusions. The day of chemo, I went in to get infused with carboplatin, Taxol, and all the pre-meds that go with that.
I had a lot of reflux and nausea during infusions, so they had to give me some extra medications.
The last piece of chemo days was the Neulasta shot to keep my immune system going. That was probably the worst part in terms of side effects for the first few days.
The shot goes off 27 hours after your chemotherapy. I had pretty intense body aches from the shot. That would subside after two or three days.
Side effects from chemo
Overall, I tolerated chemo pretty well. I only had two incidents of nausea to the point of vomiting.
Both times were from the last treatment, and I’m so glad it was the last treatment because if it had been happening the whole time, I probably wouldn’t have gone back. It was horrible.
My blood counts and platelets would go low, but I never had to skip treatments. I got anemia and fatigue from the treatment, but that’s pretty standard.
I had some headaches, but we figured out that was because I wasn’t drinking enough water and was a little dehydrated. I had a little bit of neuropathy. I lost my hair.
I had a lot of reflux, and my stomach was always sour. I had to eat a lot of bland foods. That was probably the most disruptive other than the body aches from Neulasta.
»MORE: Cancer patients share their treatment side effects
What was your chemo diet?
I try really hard to eat healthy. I had gotten in the best nutritional shape of my life before being diagnosed, but during chemo, I craved the weirdest things.
During the first few rounds, all I wanted was crunchy Cheetos. I didn’t want to eat anything else.
The second time around, all I wanted was Kit Kats. I was like, “What the heck? I don’t even eat these!”
It was definitely more like a comfort thing. It was indulgent or maybe comforting, for some reason, more than anything. I was eating like a 12-year-old.
»MORE: Tips on food and drinks to help during chemotherapy
Advice for someone who’s about to go through chemo
Be kind and compassionate to yourself.
Focus on what your oncology team is telling you. Every person who loves you will have a miracle cure something that you should be doing, and it becomes very overwhelming.
If your oncologist doesn’t mind that you’re eating chocolate bars, eat them. Don’t listen to someone else who’s saying you’re going to give yourself more cancer by eating the chocolate.
Go with your oncologist’s office because well-meaning people can really overwhelm you.
Recurrence and Second-Line Therapy
You achieved no evidence of disease (NED)
My chemo ended on December 11th. I had my scan on December 27th. Then on January 5th is when they said that my scans and blood work showed no evidence of disease.
I was ecstatic. At that point, I was so relieved. We celebrated. Then, as time went on, I became pretty anxious. All the sudden, I went from seeing somebody every three weeks to every three months.
Describe the plan for genetic testing
Our plan was to move to scans every six months, which would have been June, but I was having a lot of anxiety. I also had some scar tissue forming and was having different pains and discomfort.
Because it had been about four months, they went ahead and scanned me. It came back clear.
Throughout all this, I did genetic testing, and it came back that I was BRCA1+. I had prophylactic surgeries for breast cancer. I had a double mastectomy and reconstruction.
My sisters got tested and had preventative surgeries as well. One sister actually found out she had stage 1 ovarian cancer, so she caught it early and went through treatment.
»MORE: Read our interview with a genetic counselor
You started having symptoms again
Around MLK Day of 2019, I started noticing that same cramping or pulling sensation when I emptied my bladder. I was a little concerned about that.
They said, “Let’s do a urinary culture first because it could be an infection.” That came back normal.
Then we went ahead and checked my CA 125 just for peace of mind. It had tripled.
Then I went in for a PET scan, and that’s when I discovered I was experiencing recurrence.
What was the plan for the second line treatment?
From the scans, it looked like a pretty straightforward recurrence. My doctor took the scans to the tumor board, and they decided to try another debulking surgery.
The plan was to do the surgery, achieve optimal debulking again, and do some more chemo to clean up. Unfortunately, he went in for the surgery and discovered it was much more extensive than it showed up on the scans.

Metastasis changes course of action
He couldn’t do the surgery. It had metastasized to my liver and parts of my colon. He would’ve had to do a colon resection, and the liver metastasis couldn’t be surgically resected. He basically just took enough to get some tumor profiling done.
They tested all the components of the tumor, and we went with aggressive chemo again. Typically, you switch drugs, but we wanted to be aggressive because he couldn’t do the surgery, so my regimen was the same.
Being prepared for delays in treatment
I had two delays out of six rounds because my platelets had dropped too low. I had to put off infusions for an extra week for the counts to come back up.
What were the next steps?
My last treatment was on August 8th. They did a PET scan on the 22nd of August, and on the 26th I got my results. Everything in my pelvis and my abdomen was clear, but there was a spot on my lung.
We did another diagnostic chest CT a few days later. They verified that the spot was there. They aren’t sure if it’s ovarian cancer that has metastasized to my lung or if it’s lung cancer or just an infection.
Either way, the treatment plan is still the same. I’m starting Zejula, which is a PARP inhibitor. Then we’re just going to scan again in three months rather than six.
After bringing it to the tumor board, they really think it’s more like an inflammatory process going on rather than cancer.
My next step is just to take the PARP inhibitors and wait and see. The Zejula will hopefully give me more time in between recurrences, and if it is metastasis, the drug would target that anyway. I’ll be seen every month by my oncologist, and I’ll get scans every three months.
Hair Loss
Can you talk about hair loss?
The first time around was rough. I want to say the word “devastating” because of the way it happened. I knew it was going to be happening. They had told me I would have total hair loss.
I had shoulder-length hair. My niece always called it my “talk to your manager” haircut.
I looked into cold capping, but it was incredibly expensive and looked really painful. I was like, “Okay, if I’m gonna lose my hair, I’m gonna lose my hair. Whatever.”
»MORE: Dealing with hair loss during cancer treatment

Shaving your head
With Taxol, they tell you around day 15 you’re going to start noticing some thinning. Sure enough, my hair was just shedding. It looked like tumbleweed blowing around in the bathroom.
Then a few days later, I would touch it, and it would just come out in my hands. I couldn’t touch it at all without it coming out.
Instead of going to church that day, we went and bought a bunch of hats. I knew that I couldn’t really wash my hair too often, but I didn’t think about it too much.
I went to wash my hair like three days after going and getting the hats, and it all matted up in these two palm-sized mats.
I had to shave it. That was hard because I thought it would just slowly come out like it had been, but when I washed it, it just all matted up. It was wiping right off.
I’ve been seeing my hairdresser for like 15 years, and I asked her if I could just come in so she could shave my head. She said, “Why don’t I come to the house to make it more private?” She did.
She came over and shaved my head. She brought me my first wig. It was hard, but once it was gone, I was okay. Going through that process with it matting up was not fun.
There were a few times when I was getting really bad dark circles, had no hair, no eyelashes, and had a big scar, [and] I would look in the mirror and get very emotional because I didn’t recognize myself.
Haircut second time around
I did things a little differently the second time around. This time, I prepared myself. I got a really short, edgy haircut that I never would’ve gotten before.
I got out in front of it. I did some fun things. A lot people have farewell parties when they have a double mastectomy, and that’s kind of what I did with my hair.
The second time was much easier because I realized it wasn’t as big of a deal as I thought it was.
Also, I was in control of what it was going to look like before it fell out and how it was going to come out.
Advice for someone who is going to lose their hair
I would reach out to people who understand what it’s like to lose their hair. Talk about it.
Learn from other people. Get some ideas on what you might want to do about preparing for it to fall out.
Be around people who aren’t going to try to fix it, because they can’t give you your hair back. Be around people who are going to help you get through feeling that way and move forward with you.
Quality of Life
How were you your own advocate as a patient?
I really feel like my oncologist and medical team were very responsive. They would validate my questions, hear me, and answer me. I didn’t have to really push for things, even if it was just for my mental health.
I’m also very big on advocating for myself. The first step was when I went to see the second oncologist. I work with a lot of women now who have ovarian cancer, so I recognize that a lot of people don’t have it as good as I maybe did. You have to push for yourself.
We’re in this power differential. We just assume that doctors know everything. They do know more about particular medical things, but you know your body best.
It’s super important to say something if it feels off.
»MORE: How to be a self-advocate as a patient
Managing work through treatment
I’m a therapist with a small private practice. I quit my other job, where I had to do in-home therapy with people and travel a lot. I stopped working once a month on-call at the hospital with in-patient adolescents during recovery.
I completely stopped working for six weeks between surgery recovery and chemo. I went back to my private practice slowly after that. I didn’t do anything with the hospital until chemotherapy was completed.
»MORE: Working during cancer treatment
Paying for cancer treatment
I was incredibly lucky. My spouse’s insurance covered a lot. As a social worker and therapist, I never really made a whole lot of money.
Thankfully, she was able to kind of just carry us. Her insurance really was great. Once I hit deductibles, I didn’t have to pay anything.
It was really just about adjustment for us. It’s about reprioritizing again. Playing a board game at the table is just as fun, if not more, than going out and spending 70 or 80 dollars on a meal out somewhere.
I have had to be a little bit more creative, but for us it’s more of shifting expenses. We were fortunate to not have faced incredible financial burdens.
What was the lowest point mentally or emotionally?
After remission and both of my surgeries. All of a sudden, I had no idea what the hell had just happened to me. I’m a therapist, and I was not prepared for just how depressed I was going to be.
It was because throughout treatment, I was so busy doing the next thing that I didn’t take care of my thoughts and feelings. I was constantly moving and battling.
Once everything was done, I had all of these emotions that I didn’t know what to do with.
People flood you with cards, texts, support, [and] visits, and once everything is done, everyone moves about their normal lives.
You’re left there, and nothing about you is the same.
Your perspective changes, your priorities change, and I didn’t handle that part well. I didn’t see it coming. I asked my oncologist to refer me to a therapist at the oncology center, who I still see today.
I have young kids who have special needs, so all of this was very scary for them. I didn’t necessarily deny my feelings, but there’s got to be a balance. I didn’t want to wallow in how I was feeling.
It’s good to have a positive outlook throughout your treatment, but it’s also extremely important to acknowledge how it’s affecting you and do that regularly. I don’t think I was very honest about that because I was too worried about how my emotional state would affect my family.

How has the cancer affected your relationship with your spouse?
In some ways, I think it brought us closer together as a family. As a whole, too. We take trips. We take advantage of the things we can do while we can do them. We take less for granted.
I don’t want to say it improved our relationship, but it’s definitely brought us closer and showed us what’s really important in our lives. We’ve reprioritized quite a bit.
I’m very lucky to have somebody who’s the kind of caregiver I wish everyone could have. I know that’s not always the case. I didn’t have to ask her for anything.
She told me not to worry about a thing and just to get better. We have a pretty symbiotic relationship. It was nice to not have to worry if I didn’t feel like doing the dishes. She’s a wonderful caregiver.
She’s definitely always been a doer. She doesn’t like to sit still. I’m a doer and a caretaker of other people, so some of that was a little bit hard. We found ways to laugh a lot and really talk to each other about our feelings as much as possible.
I encouraged her to talk to other people about it, too, because I couldn’t imagine what it would be like as a caregiver.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
I think we moved along pretty cohesively. Sometimes, that meant M&Ms and popcorn for dinner and live it up. We did little special things like that if we needed it. We coped pretty similarly.
For her, I think it was important to take charge. Then she felt like she was doing everything she could to help me.
Talking to your kids about cancer
I have two step kids. They’re older. Now, they’re 30 and 28. My youngest are now 19, 16, and 15, and the three youngest all have pretty significant special needs.
I initially was very vague about my diagnosis with them. My mother had just passed away from cancer, so all they knew was that people with cancer died.
I told the kids that I had to have a surgery because the doctor found some things in my body that were making me sick. I told them they needed to remove those bad germs and then give me medicine that would help me get rid of them all together.
I said it might make me sick, too, but it was also going to make me better.
I didn’t use the word ‘cancer’ until I had worked with their own therapists and doctors. I ended up just telling them because my daughter saw me looking at head covers online, and she asked me outright if I had cancer.
That’s when I told them, but I had to sit down and explain that it was a different kind of cancer than what Grandma had because that was hard for them to separate.
Do you have advice for other parents?
I definitely would recommend honesty on a level that they can understand. Don’t burden a child with terms they can’t understand, but be honest about what’s going on.
I had to tread carefully as far as the use of the word ‘cancer’ until I couldn’t avoid it anymore, but I was always very honest with them.
They need to be aware of the changes that will inevitably occur.
Use your resources. Let them go to their friends’ houses. Befriend their friends’ parents. Even though they’re older, they never went to treatment with me.
They didn’t go to appointments. They have really high anxiety, and that sort of thing would’ve been hard for them.
Also, I suggest identifying friends or adults they can talk to safely about their feelings.
»MORE: Parents describe how they handled cancer with their kids
How important was it for you to have caregivers?
It helped me a lot. It was important to have support. The hard part was that I got so much more support in the beginning.
Everybody came for surgery, and then it was hard to have people later on when I was more tired and needed it.
Because of my situation with my kids, it takes a village to take care of them now. I’ve always been their main advocate and organizer. Having my siblings and my spouse step up and take that over for me really helped me focus on getting better.
Knowing that my kids were taken care of helped me take the time to take care of myself and rest when I needed to.
It can be hard to ask for help. What advice do you have?
Look at things that you’re doing that anyone could do. Reach out to your people. Maybe start small. Talk to your spouse or closest sibling or friend. It was very hard for me to admit that I needed things.
It’s about humbling yourself and being vulnerable. You need to be able to give the tasks to other people. It takes a lot of physical, mental, and emotional energy to go through cancer, so you don’t need to be taking everything on alone.
In the beginning, you get people who say, “Let me know what I can do.” That’s great. Let them know.
People who are close to you will come take over things. Give one of them a list in the beginning because then those closest will not have to ask for permission.
They’ll just come do it. They’ll come clean your house. They’ll bring you a meal. Or if someone says they want to help, they can tell them for you.
Someone who says to me, ‘Let me know if there’s anything I can do,’ are the last [people] I would ask for help because the people closest to me are just going to do it.

What is your “new normal”?
Living intentionally. That’s my new normal. I still yell at my kids. I still get annoyed. I still get angry in traffic.
I’m a normal person, don’t get me wrong, but in the big picture, I focus on really living in a way that gives me the most about every day.
It’s the way we should all live anyway because we’re not promised anything. When you’re faced with your own mortality, you find out the things you want to be spending your time doing.
I no longer suffer through friendships that feel toxic. I focus on the relationships with friends and family members that mean something to me.
If we decide there’s something in the world we want to see, we try to make a plan to get it done. We don’t act like we have an infinite amount of time. We try to be purposeful with how we conduct ourselves.
Advice for someone who has just been diagnosed
Surround yourself with support. Reach out to people who understand. Find your tribe of people who get it.
It took me a while to talk about this whole thing, but once I started identifying and reaching out to people who had kids or who were younger with this disease, it made me feel empowered.
It’s such a hard thing to process, but it doesn’t mean the end of living. It’s just thinking about life in new ways. Find people who understand that and can say, ‘Yeah, me too.’

Inspired by Shirley's story?
Share your story, too!
Ovarian Cancer, High Grade Serous Stories
Randalynn V., High-Grade Serous Carcinoma, Stage 1C
Symptoms: Pulling sensation when emptying bladder; abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), surgery
...
Shirley P., High-Grade Serous Carcinoma, Stage 3C, BRCA1+
Symptoms: Pulling sensation when emptying bladder; abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), de-bulking surgery, PARP inhibitors
...
Suzann B., High-Grade Serous Carcinoma, Stage 3C, BRCA1+
Symptoms: Inability to urinate
Treatments: Chemotherapy, de-bulking surgery, total hysterectomy
...
Susan R., High-Grade Serous Ovarian Cancer, Stage 4
Symptoms: Pulling sensation when emptying bladder, abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), surgery
...
Sara I., High-Grade Serous & Clear Cell Carcinoma, Stage 3A
Symptoms: Random sharp pains, unrelated scan showed ovarian cyst
Treatments: Debulking surgery, chemotherapy (carboplatin & paclitaxel), PARP inhibitors (clinical trial)
...




One reply on “Shirley’s Stage 3C High-Grade Serous Carcinoma Ovarian Cancer & BRCA1+ Story”
my sister is law just got diagnosed with high grade serous. They are starting chemo tomorrow with carboplatin and taxol,
3 to 4 cycles every 3 weeks. In between ,they will be doing surgery to remove what’s left. Curious on why they are not doing surgery right away. Cancer has already travelled to lower abdomen. would like your comment on how effective the carboplatin/taxol treatment is..