Nina’s Stage 2 Chromophobe Renal Cell Carcinoma Kidney Cancer Story
Nina shares her stage 2 kidney cancer story, a rare subtype called chromophobe renal cell that grows in the cells that line the tubules around the kidney, and undergoing a partial nephrectomy.
In her in-depth story below, Nina also highlights how she navigated quality-of-life issues, from dealing with how to pay for cancer treatment (financial toxicity) to the best support she got, the value in sharing your story, and how important it was to be a self-advocate as a patient.
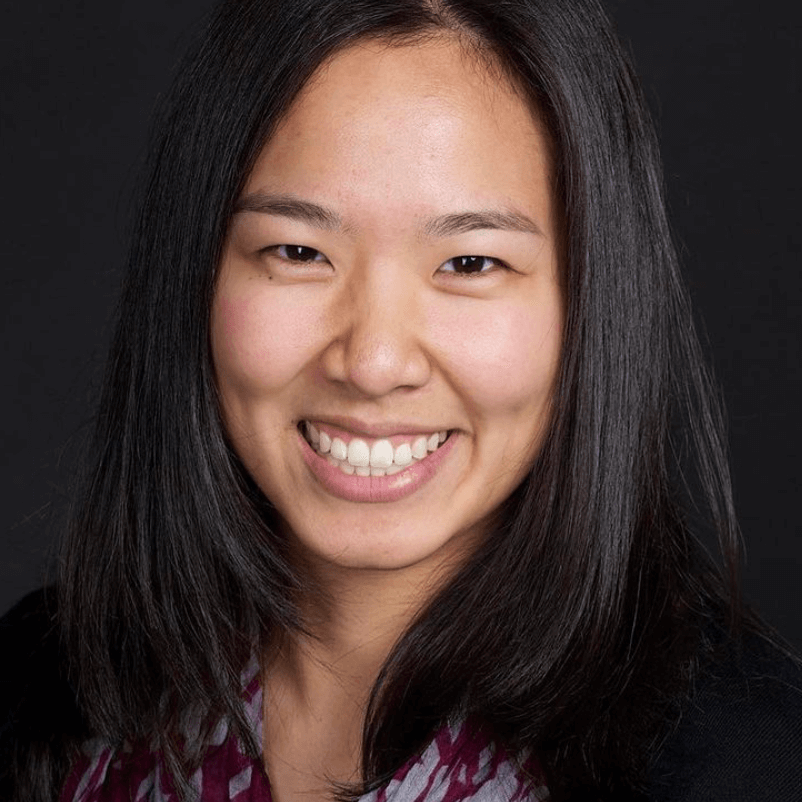
- Name: Nina N.
- Diagnosis (DX):
- Stage 2
- Chromophobe renal cell carcinoma
- Rare subtype, makes up 5% of kidney cancers
- Age at DX: 24
- Symptoms:
- Blood in urine
- Blood clots
- Intense abdominal pain
- Treatment:
- Partial nephrectomy (kidney removal surgery, right side)
- Surgical Pathology Report:
- Anatomic Location: Right kidney, superior and mid poles
- Tumor size: 16.8 cm in greatest dimension
- Lymph nodes: None
- Distant metastasis: Unknown
- Stage: 2
- First Symptoms
- Cancer Diagnosis
- Surgery
- Surgery Recovery
- Describe the surgery recovery
- Complications during surgery recovery in the hospital
- How did they monitor the seizure-like activity?
- How did they stop the seizure-like activity?
- Recovering at home from the surgery and the complications
- Lowering medication should be done progressively
- How long was recovery at home?
- When did you go back to work?
- Anything you wish you had known at the beginning of treatment?
- What’s your follow-up protocol?
- Reflections
- The day of this interview is special
- How did being a nurse impact your experience as a patient?
- Did you deal with financial toxicity paying for treatment?
- You had amazing support around you
- The cancer shifted your career path
- What was the best support you got?
- How did you get through the hardest parts during treatment?
- Dealing with uncertainty after treatment
- The value of being vulnerable in sharing your story
- What’s the importance of self-advocacy as a patient?
- What kind of support was most important to you during surgery recovery?
- “A new normal”
- Last message for other patients and caregivers
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

First Symptoms
What were the first symptoms?
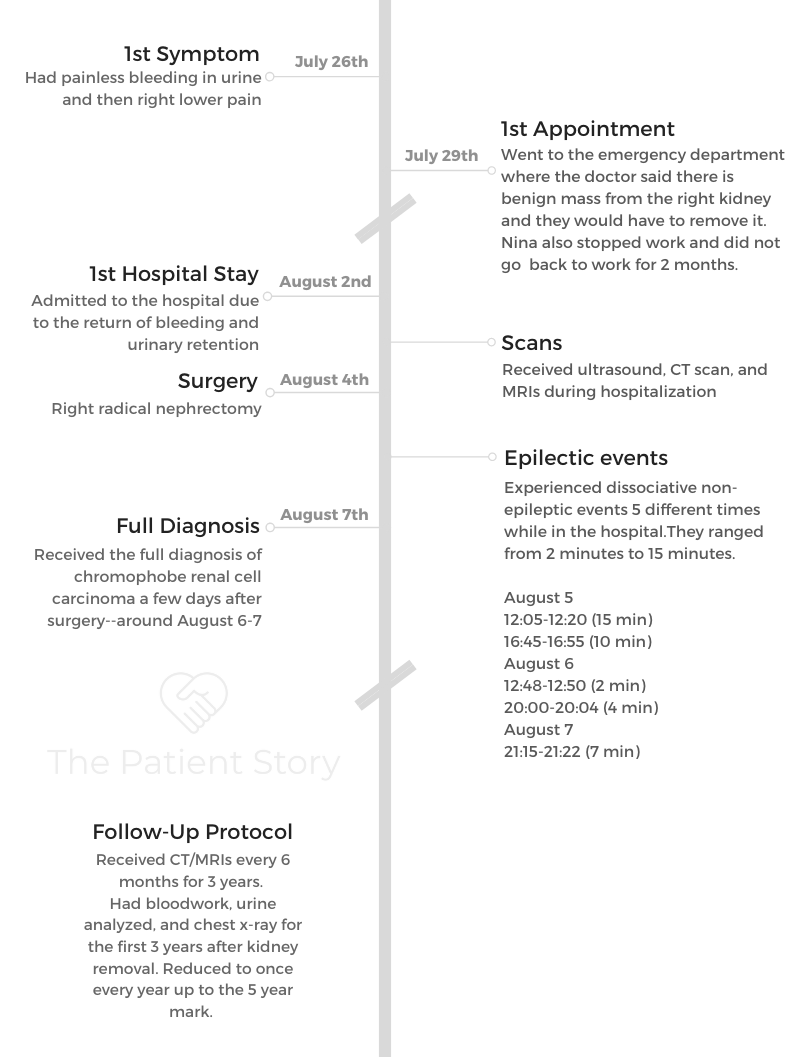
I actually kept track of the dates on my phone when it happened. July 26th was when I first had my symptoms.
I had blood in my urine. I was like, “Oh, it’s just some blood.” Then I was working night shift at the time, so I still went to work. I told my coworkers that I didn’t know what was wrong.
I was a nurse at the time, and I started having these blood clots that I would pass. They were about the size of my pinky, so I knew that wasn’t normal.
I made a doctor’s appointment and was going to go see the doctor after I worked the next couple of night shifts, but then I had intense 10 out of 10, right-sided abdominal pain after my second night of working night shift. I went to the emergency department.
Basically, my first symptoms were bleeding in the urine, had blood clots, and then I had that abdominal pain.
What happened at the emergency department
When I went to the emergency department, it was one of my first times there. It took forever to get a room. I think they were really busy, and I didn’t look like I was dying, so they admitted all the emergency people first.
I was in so much pain. I’ve never had pain like that before. I was like, “Did my appendix burst? What’s going on?”
By the time I got admitted and got a room, they gave me pain medicine. I would be in my fetal position because the pain was so bad, and it was only on my right side. At the time, I didn’t know what was going on.
Describe the ultrasound
They immediately got an ultrasound for me and scanned the area. I knew it was bad when the ultrasound tech was like, “Hold on a minute. I want to get the doctor.”
The tech came back with the doctor. They said they saw something that looked like a hematoma.
It’s like an internal big blood clot bruise that’s inside. They saw some sort of a mass and thought it was a hematoma. They wanted to do some more scans just to see what it was.
Describe the CT scan
They sent me for a CT scan, which is a little bit more in-depth. I was still in pain during this time. They gave me pain medication, but it does not always work super well.
By the time I got back to the room and the doctor looked at the CT scan, she said it was a tumor that was coming from my right kidney. She said it was most likely benign at the time and not cancerous, adding they were going to have to remove my kidney.
I had my first symptoms on the 26th of July, and I was admitted to the hospital on the 29th, so three days later it was bam, bam, bam. It progressed really rapidly for me, so I didn’t have too much time to comprehend everything.
Why did they think it was a benign mass?
The doctor said it was benign, mostly because I’m young and healthy. I was 24 at the time and didn’t drink, do drugs, smoke, so she thought it was probably fine.
They were just going to go to remove the kidney and then check the pathology to see what it was. It wasn’t until maybe like even a week later when I found out that it was cancer.
Maybe there was a misdiagnosis at the beginning, only because they were trying not to worry me and thought it was most likely benign, given my history, my age, and what they saw.
You had repeat visits to the Emergency Department (ED)
They admitted me to the hospital. In the Emergency Department (ED), gave me pain medicine, and they put a Foley catheter in me to just help with the bleeding, to flush it out. Eventually, I stopped bleeding.
They sent me home, and I didn’t get to stay home for very long before I started having the same symptoms I mentioned before, with the bleeding in the urine and the blood clots again.
I actually returned back to the ED on August 2nd. I had a period when I was briefly at home, but then they said I had had these symptoms for so long, so they’d schedule a surgery, even though it wasn’t emergent.
When the symptoms came back again, I was like, “Okay, great, here we go again.” A doctor came back.
I was like, “I need to have a surgery to get this tumor thing out because I’m having a lot of symptoms, and I need to be taken care of.”

Processing the news of needing kidney surgery
When the doctor told me that they were going to have to remove my right kidney, I remember feeling shocked. I did not come to the emergency room to lose a kidney.
I just thought something happened, I’d get pain medication, and I’ll be fine. So everything slowed down. I remember as soon as she said “kidney removal,” everything else she said was muted. I just couldn’t hear anything she said. Everything was slow motion.
I was like, “I’m going to lose my kidney.” That’s literally the only thing in my head. I remember looking over to my parents — they were there with me — and they started looking upset, crying. I started to cry, too. That was the first shock of the news.
Cancer Diagnosis
How did you process news that they found cancer?
August 4th was my actual surgery. They took the tumor out, they did the pathology report, and I didn’t find out I had cancer until August 6th, a couple days later.
When they told me that, I already actually had a bad string of complications that happened during my hospitalization. Once they told me the news, when they said it was cancer, it was like the cherry on top of every other bad piece of news I had received during the time that I was in the hospital.
I definitely felt very defeated. I thought I was going to die, because when you hear the word “cancer,” it doesn’t matter what cancer it is. It’s the C-word, and at 24 I thought I was going to die.
I asked if it had spread and what was going to happen to me. I knew I could live with one kidney, but it’s scary how even a young and healthy person like me can get something like cancer.
Cancer doesn’t care. It doesn’t care if you are old or young, doesn’t care if you’re healthy or unhealthy. It can still affect you. I was mostly scared and disheartened. I was not sure what to do next.
How did you break the news of cancer to your friends and family?
It took actually two weeks before I was even able to make a YouTube video announcing the fact that I had cancer, asking for prayers.
Between the three- and four-week mark, I started letting people come visit. I first talked to my family because I wanted my aunts and uncles, my cousin, all those my family members to know what happened to me first. Then I let my friends know, and then they were able to come visit.
I wasn’t able to have a conversation, and I looked fragile. I’m normally a pretty energetic and happy person, and the person that I was during the recovery process, especially the first couple weeks, was like a shell of the person I am today.
I couldn’t even laugh; it just hurt too much. It’s like lying around trying to heal, and it was better to not have visitors because it would have been too much for me. I would have been too tired.
»MORE: Breaking the news of a diagnosis to loved ones

How did it feel sharing news of your cancer diagnosis?
I kind of struggled with it. I’m pretty open about things, but I try not to share bad news too much because no one likes a Debbie Downer.
I prayed about it, and I was like, “I think I should share my story.” I’m a firm believer of sharing the good and the bad things that happen in your life because other people are going through bad stuff, too.
I know with social media people usually post the good stuff, but that’s a lie because not everything in life is good. Bad things happen. It is just the way life is.
So I decided to post and share because I wanted it to be an encouragement to other people, because maybe other people are going through cancer and they’re struggling, too, but they have no one to talk to.
It was very hard. There was one moment when I was talking and started crying, so I had to pause and then re-shoot it. It was very hard for me at the time. Just the word “cancer” would trigger me.
I had to do a PET scan to make sure the cancer didn’t spread, but that didn’t happen for a month after I came home. For that first month, I literally thought I was going to die. I didn’t know if the cancer spread. I was worried that they didn’t catch everything when they did the surgery, so I started planning my memorial.
I didn’t want my parents to worry about it, so I was like, “Well, if I had my funeral, this is what I would want to have happen.” I started planning and coming up with my game plan.
But I was 24, and I really thought I was going to die. I remember talking to God. I was like, “Okay, here’s the deal, if you are done with me and this is my time to go, fine, I will go.
But if you’re not done, please, please, please bless my life and help me to be an encouragement to other people, help me to love people, make sure they feel loved and appreciated, because life is so short.’ I want to make the most out of my life, my second chance at life.
And praise God, he gave me a second chance at life. For the past five years, I’ve had that mentality of “you only live once,” trying to spread as much love to other people as I can through my words and my actions, whether interacting with people at church, at work, at school, in the grocery store, or wherever.
You had your parents to support you through everything
I’m very blessed to have two parents who spoil me with a lot of love. As soon as I told them my symptoms and I was going to the hospital, they dropped what they were doing at work and just came. They were with me.
They still had to try and go to work, obviously, when I was in hospital, but there was either my mom or my dad always by my side at the hospital, which was super nice because it was really hard.
If I had to go through it by myself, I think that would have been a lot worse. There was so much uncertainty about what was going to happen next, even before the surgery.
Having caregivers helped with self-advocacy
I was really nervous about the surgery. They actually gave me a lot of pain medicine, so I was pretty doped up in the hospital. I wasn’t always thinking very well.
So it was nice to have my mom or my dad advocate for me. Sometimes I know patients can’t always advocate for themselves, so it’s always nice when a family member is able to be there for them.
I still have amazing parents to advocate for me, but they did an amazing job supporting me during that time in the hospital.
»MORE: How to be a self-advocate as a patient
Surgery
How did you decide where to get the surgery done?
I worked at a hospital as a nurse, and I should have gone to the hospital I worked at. My mom is also a nurse. I actually went to her hospital because she was there, so she could quickly go downstairs and meet me in the emergency room.
I don’t think my care at that hospital was the best, obviously, just given everything. There were a lot of other things that happened.
I don’t think they took care of me very well. I was a nurse at the time, so I knew what good nursing care looked like. I was pretty disappointed.
I had a lot of things going on, like the fact that I had cancer, so I didn’t dwell too much on it until later. But if I had a choice, I would have gone to my hospital because at least the people knew me.
I know that patients get treated very well, and also, I work there. If I had to do it again, I’d probably go to my hospital.
At at the time, I wanted to be close to my mom. She said to just come to my hospital, and so that’s what happened. It is what it is. I’m very glad that my mom was able to be there because she could just quickly work and then come down to visit me.
My dad would also come visit me after he was done working, too. Between the two of them, I always had a parent nearby. It was only because I went to my mom’s hospital that she was able to actually come up and down to check on me.

What was the overall treatment plan?
They said that once I had a nephrectomy, or the removal of the kidney, I should be okay. I was like, “Okay, if that’s what it takes.”
I did some of my own research, and it seemed like with the cancer I had, while it’s rare to have it happen to someone as young as me, it’s still pretty good prognosis once the surgery occurs.
We didn’t have to ask for a second opinion, but I felt pretty good about [it], like, “Okay, fine, we’ll remove it.” At that point, it was causing me a lot of symptoms. Clearly, we had to get it removed.
I think what happened actually was that the tumor was really slow growing. I had it for at least a decade. As it slowly grew, it started to take up more and more blood supplies and nutrients to the point where it ended up being a five-pound tumor that was removed from my body.
It’s like when a woman’s pregnant and you have a baby for nine months, your body adjusts to the extra being in you. I think for me, because it took so many years to have that tumor grow, my body adjusted because I didn’t feel anything weird.
My lab work and everything was normal. The only thing I had was high blood pressure, which is vague because it seems like everyone has high blood pressure.
Your symptoms helped lead to catching the cancer earlier
It’s only because I started bleeding. I’m glad, I guess, that I had bleeding in my urine because if that didn’t happen, I wouldn’t have known. Worst-case scenario, my tumor could have ruptured, and basically all the bad cancerous cells would have spread.
Describe the type of surgery you underwent
It’s hard to clean, get all that stuff out when it’s spread so much, compared to my situation where it was very contained, like a capsule, if you imagine that.
When they did the surgery, they were very careful to remove the whole thing, keep it contained, and then remove it.
Actually, these types of procedures can be done by a method called laparoscopic, when they make little incisions and use a machine that helps get the tumor out. Because my tumor was so big, they had to actually cut me open through my abdomen and explore the area just to see if it spread at all.
The tumor actually started pushing against my liver and against my inferior vena cava, which is like the big vein that leads to the heart. If it kept pushing, it would not have been good, and I would have started having other symptoms.
They were basically able to extract the whole thing. I asked them for some pictures. Later, through those pictures I was able to see how big it was, how much it weighed. It ended up being a baby size — a baby you don’t want.

Surgery Recovery
Describe the surgery recovery
I did take a couple months off work to recover at home. In terms of follow-up treatments, I needed to have a PET scan, a full body scan, just to see if the cancer spread anywhere.
I was actually unable to lie down flat, and for the scan you have to lie down flat. I hurt so bad from my surgical incision that it took me probably a month before I was able to lie down and not be in so much pain.
The recovery process was super hard for me. It hurt. When you think about it, they cut through my abdominal muscles. You use those to laugh, to talk, to breathe even.
Sneezing would be super painful for me, so any extra pressure that I would have just would hurt a lot. Anything that I had to use my ab muscles for.
I couldn’t actually talk, have a conversation like this, even laugh, which I love to do, for at least a week or two while I was at home. So no visitors. It was just me and my parents, and they helped me sit up. They helped give me my pain medicine.
Usually if it’s laparoscopic, it’s smaller incisions, and you recover a lot better from it, but I didn’t have that option due to the size of my tumor.
Complications during surgery recovery in the hospital
My surgery was August 4th. They knocked me out; I had anesthesia. My surgery was at noon, and I woke up at around 8 a.m. on August 5th. I heard this beeping from the IV pump. They put an epidural in me, which basically helps with pain control and helped numb me from the belly downward, so I could tolerate the incision.
Turns out that with the IV pump beeping, it said that the epidural bag wet-dry, which should never happen by the way. That’s like nursing 101 — never let a bag of medication run dry.
We let the nurse know, and they said it was going to take 15 minutes for them to mix the medication to put back in the bag. At this point, ten minutes goes by. I was originally numb all the way to my knees, and then I start getting feeling back, and slowly it comes up.
I can feel my thighs, I can feel the bottom of my belly, and I’m freaking out. I’m like, “I’m going to feel my incision.” The numbness from the epidural is wearing off, so I’m panicking.
We called the nurse, and the nurse knocked me out with like Dilaudid or pain medicine, and right before I went to sleep, the numbness went away. I remember I felt like I got cut open, which is what happened, but it was like the worst pain I’ve ever felt, even worse than that abdominal pain that was one of my original symptoms.
Then I remember knocking out. After that happened while I was asleep, the anesthesiologist was called, and they asked to give me an extra dose through the epidural.
So he gives me an extra dose. I’m not quite sure what happened, but sometimes when you put an epidural in, you can nick the dura, and the medication might actually go into the spinal space instead of just staying in the epidural space.
When that happens, it’s a little bit more potent, and I actually had side effects from the medication. The side effects that I had were seizure-like activity that can last from two minutes to 15 minutes. That happens the next three days, six different times.
My pain control wasn’t super good, and now I had this seizure-like activity. It was weird because I was still with it, but my teeth would chatter, then my head would start to shake, [and] then my whole body would start to shake. That was like seizure-like activity.

How did they monitor the seizure-like activity?
They took me to a brain CT scan just to make sure I was okay, and my brain was normal. They did tests to make sure I wasn’t having a seizure. It wasn’t an actual seizure. It was a seizure-like activity because of the medication that happened.
They got rid of that epidural. For pain control, they did something called a patient-controlled analgesic (PCA) pump, where they gave me a patient button, and it has continuous medication running through my IV. [If] for some reason I had extra pain, I pushed the button, and more medicine would come in.
They put me on a Dilaudid PCA pump for pain control, so I would occasionally hit it. That seemed to help, except when I started to hallucinate.
The good news is that my hallucinations were actually pleasant ones. I recall there was one where I thought I was talking to the respiratory therapist, having a whole conversation, and my mom was sitting on the chair in the back.
She’s like, “Who are you talking to, Nina?” I said the respiratory therapist, and my mom was like, “There’s no one there.” So I’m talking to nobody.
Then the second hallucination I had, I was starting to eat pancakes or waffles or something. I was really hungry, I guess? My poor mom, she just saw me all doped up and weird. I start eating nothing, literally eating the air, and she’s like, “What are you doing?”
Anyhow, they got rid of that Dilaudid because I wasn’t reacting very well to it, and they gave me other pain medicine. A lot of bad things happened. I had a lot of complications, partly related to the anesthesia, partly just related to the poor management of my drugs. During all this is when they told me that I had cancer.
How did they stop the seizure-like activity?
They would give me a medication like Ativan. I’m a weakling; when you give me meds, I pass out. I don’t need much. Every time they give me Ativan, I would basically go to sleep for like half the day.
That definitely prolonged my healing process, because typically after surgery, they try and get you up and moving. Being active and walking around helps with the healing process.
You want to get some blood flowing, get breathing, and open up your lungs and everything. Then they also get you to try and pee so that you can get the Foley catheter out, and then you can go home.
You always feel better at home because it’s just a comfortable space. You are in your own natural environment, and there are not a lot of sick people around. It’s also cleaner.
I stayed at the hospital an extra four to five days because of those complications, stuck in bed. They didn’t turn me. You are supposed to turn patients every couple hours so they don’t get bed sores. I actually started developing some skin breakdown on my bottom and my lower back because I wasn’t being turned.
You are also supposed to deep-breathe and get your lungs working, but because they couldn’t control my pain very well with that incision, I didn’t always do that very well. You are at high risk for your lungs not expanding well, and then you might have atelectasis.
Older people have a higher risk of lung problems if they’re not able to get back to their normal lung capacity. Definitely, the complications hindered my healing.
But once I got home, slowly but surely — I would say it took a couple weeks — I was able to feel a little bit better.

Recovering at home from the surgery and the complications
When you go home, you can’t have an IV catheter. You go home with pain medicine you take by mouth. It does work, but you have to be on top of your routine of taking the pain medicine. It’s hard to play catch-up.
Let’s say you’ve done a really good job and now your pain is under control. You might feel you don’t need the pain medication anymore.
Well, the previous pill that you took is going to start wearing off, and then you’re going to hit pain. It’s going to take a lot longer before it goes back up again and you’re able to reach that therapeutic level. It’s just hard.
When I got home, they gave me oxycodone, which is a pretty popular pain medicine you take by mouth, but I had to take a couple pills every three hours around the clock, which is a lot.
I was on a pretty good dosage of that. What you do is, as you start healing and getting better, you lower the number of pills you take. Instead of two, I would take one, for example, and then instead of every three hours, I would do every five or six hours, to the point where I only had to take one pill in the morning and then at night.
After that I just tried to walk around. I actually had a walker because my five-pound tumor was removed and caused me to feel really unbalanced.

Lowering medication should be done progressively
I tried to wean myself off the oxycodone maybe a little too fast. Once, I decided to skip the evening pill.
I actually like to do jigsaw puzzles, so when I was healing, I did a lot of puzzling. I was doing a puzzle, and then my eyesight suddenly started to go. Everything was blurry, and I couldn’t fit the puzzle pieces anymore.
Then I had to go back to the bed, and the lights started being too bright. Then I started getting weak, feeling nauseous, and basically going through withdrawal.
My body was so addicted to the oxycodone that when I tried to wean myself off too fast, I was going through withdrawal.
These are all the symptoms of an addict going through withdrawal, so I remember I was like, “Dad, I need my drugs!” I was yelling that to him.
I knew I clearly was not ready to wean myself off, so I took it a pill and felt better half an hour later, which is about how long it takes for pain medicine to kick in when you take it by mouth.
I learned my lesson. I very, very carefully weaned myself off, to the point where I actually didn’t need any more pain medicine after. It probably took a month though.
How long was recovery at home?
Officially, two months I stayed at home. They wanted me to stay at home and not drive because of the seizure-like activity. They didn’t want to rule out that it could have been a seizure, and technically if you have seizures, you’re not allowed to drive.
So I stayed another month at home just to make sure I was okay. It took about a month before I was even able to walk up and down the stairs, so I basically stayed in the bedroom, the kitchen, and the living room, where I puzzled. Eventually, I was able to get strong enough to walk up and down the stairs.
When did you go back to work?
After two months, I went back to work, but I didn’t work hard-core. I just did light duty.
That means I basically just helped a lot with the computer stuff, ran errands for my coworkers, little thing like that.
I couldn’t do patient care because they are pretty heavy, and I was not allowed to lift anything because that could affect the sutures.
If I put too much strain on the sutures and the incision, then the sutures could have broken apart.
Anything you wish you had known at the beginning of treatment?
I was lucky enough to have a good cancer doctor. I was asking if I had to change my food diet and how I might change my lifestyle with one kidney. Thankfully he said, “Just still take care of yourself. Eat healthy food.”
He also said I can’t do contact sports, so I can’t do flag football. Anything where someone would tackle me is a no-no. I have the one kidney, so I can’t afford to have someone kick me or punch me, and then I’m out. He did a good job preparing me for that.
What’s your follow-up protocol?
I also asked him about my follow-up after surgery. He says to do an MRI or CT scan every six months for three years. Then after that, do a CT or MRI once a year, up to five years.
For the first three years, I did blood lab work. They would check if my kidney function was still okay. My creatine, which usually is a good indicator of how your kidney is doing. Check my urine to make sure there wasn’t any possible infection or blood, since those are some of the symptoms I had last time.
They also did X-rays on me, which I was surprised about. I asked, “Why are we doing X-rays? My lungs are okay.”
My doctor said, “Actually, if the kidney cancer were to come back, it would more likely affect the lungs.” I was a little nervous about that, so I agreed. I actually did X-rays of my lungs for the first couple years as well.
Reflections
The day of this interview is special
Before this interview, I did my five-year MRI this morning! Today. I’m hoping that’s the last one I have to do because he actually didn’t give me any more guidelines after the five-year mark.
I was pleasantly surprised to know that I made it to the five-year mark.
How did being a nurse impact your experience as a patient?
Sometimes being a nurse, you diagnose yourself in the worst way possible. When I was going through my symptoms, I was like, “Is my appendix wrong? Do I have something wrong in my bladder? Do I have a UTI?”
I actually briefly thought I had kidney cancer, but I was like, “Nah, that can’t happen. I don’t have cancer.” I was trying to diagnose myself, which is a bad thing.
Then when I got to the hospital [and] went through all the post-surgery complications, it stunk being a nurse because I knew what good care was. It was disappointing that I had to advocate for myself and my mom, who was a nurse there, had to advocate for me, too.
I felt bad for other cancer patients who are going to the hospital and are not medical people at all. They don’t know how to advocate for themselves.
I’m hoping through not only my story, but other people’s stories, that they know, actually, you need to speak up for yourself. Ask the right questions. Then you just pray that your healthcare team will do the best for you.
A lot of places do take good care of you; it’s just sometimes things happen. It helps to be a nurse because I knew what should have happened, and I was able to have really good conversations with the doctors and the nurses. They didn’t have to dumb everything down for me because I was able to understand the medical term. That was nice.
But it definitely was weird. I had literally just finished my first year of being a new nurse, and then I got my cancer.

Did you deal with financial toxicity paying for treatment?
At the time, I was double insured. I had my dad’s insurance and my own. There were actually some complications financially from it because I went to my mom’s hospital.
If I had gone to my hospital workplace, it would have been my insurance, and it would have been fine. Instead of thousands of dollars or tens of thousands of dollars, the cost would have been hundreds, which is a lot better.
Since I went to my mom’s hospital (workplace), I had to fight with them for a year following my hospitalization because they were saying I had no insurance, when I said I was doubled insured. I had my dad’s insurance, which technically covered it.
I was fighting for a year trying to get this $10,000 bill reduced to $200. You’ll find that when you look at the cost of treatment from surgery, to getting anesthesia, to staying in the hospital for X number of days, it’s a lot of money.
I had insurance, and that helps a lot. For some of the cost that I had, I basically had a little bit of money saved up, so I was able to slowly pay it off. But if I didn’t, I would have had to take out some loans.
Because I did work for a year as a nurse, I was able to accumulate a little bit of money from that, but I will say financially the insurance did help. I just had to slowly pay off my bills.
Those bills would come months later. It’s not instant. They have to calculate it and then give it back to you. I feel like I paid a lot for treatment, the surgery, and stuff, but it was worth it.
For other people who aren’t as lucky as me, you just have to either borrow money from the bank and get loans maybe from family members to get through it.
The cost of healthcare is definitely one thing that I wish was better. You go through cancer, and it’s not your fault. Now you have to go to the hospital and get all these treatments, and it’s freaking expensive!

You’re happy you’re alive, happy you get a second chance at life, but it doesn’t make the money appear for you just because you are happy.
I think they have payment plans. Sometimes people are able to pay it off slowly, but they can be a lot. An MRI can cost thousands of dollars just for one.
You can’t plan for something like this to happen, but have an emergency fund. Hopefully you have good credit and can get a loan or something from the bank.
You had amazing support around you
I was super blessed to work at [that] place. I was an ICU nurse, and my ICU work family supported me really well.
I told them I had cancer and I was going to be out for two months. I felt bad because I couldn’t help out, but they visited me, prayed for me, and checked up on me.
It was just nice to feel love.
I am a Christian, I believe in God, and I believe he has really blessed me with amazing people in my life, from my family, to my friends, to my coworkers, to my classmates. Every group of people I interact with has been pretty amazing.
It was nice to have actually intelligent nurses and coworkers, because I would ask them questions, too. Because I was a new nurse, I didn’t know everything that was happening. Like, “Oh, should I do this? What should I do?” It was nice to ask them some questions because they’re very knowledgeable.
»MORE: What kind of support cancer patients say helped the most
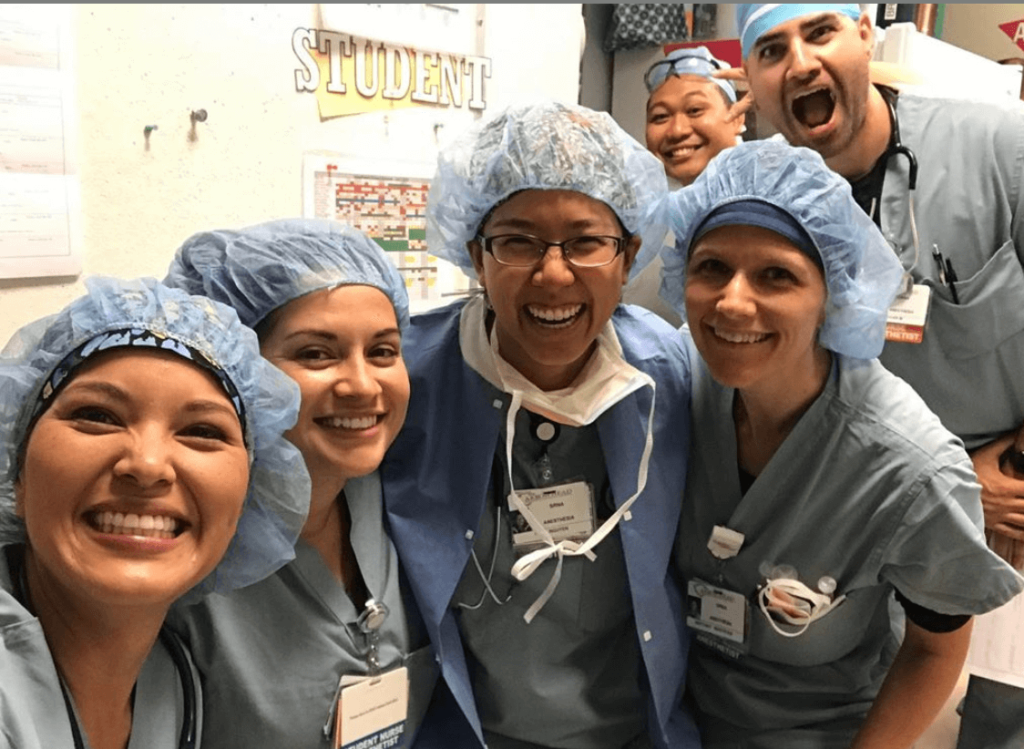
The cancer shifted your career path
The cancer is actually part of the reason why I decided to go back to school to be a nurse anesthetist. Now, I’m actually in anesthesia.
I just started working this year. I graduated during COVID-19, and I started working. I’ve been working for three months, providing anesthesia for people who are going through surgery. I think it’s been helpful to be able to relate to the patients.
It’s also been a little crazy going from nursing and having all that bad stuff happen, but then being like, “Actually, I want to continue doing more for my patients.”
Remember how I said I couldn’t do contact sports because I had to protect my kidney? Well, in the ICU, sometimes we get patients who are very violent or delirious, and it’s not necessarily always their fault.
Sometimes you’re just going through a lot of things, and they’re not in their right mind, but that means we have the possibility of getting punched or kicked.
I didn’t want to risk my kidney in that environment. I had to quit my job even though I love the people so much. [I] decided to go back to school to do something where it wasn’t as physically demanding so it can be better for my health. That was part of the reason why I decided to go into anesthesia.

What was the best support you got?
I felt very loved. My friends would drop by, and they would give me my favorite ice cream flavors. They’d give me little gifts, things to make me happy, including the puzzles and other stuff.
But I’m simple. Just having a friend or family member text, call, or visit me was enough to make me happy, because I just felt really loved.
I can only hope that other people who are going through cancer have the same support system that I did because it’s just very difficult to do it by yourself.
Kudos to everyone who’s tough, but I was lucky enough to have a good support system that made it a little bit easier to deal with everything that happened.
»MORE: What kind of support cancer patients say helped the most
How did you get through the hardest parts during treatment?
I would cry every night. My parents don’t know this, but I would wait till they went to sleep, and I would literally just silently cry. I was scared. I can talk about it now, but I was definitely terrified, thinking, “I am too young to die. This is horrible. What did I do to deserve this?”
So I cried a lot. Not in front of my parents. They were dealing with the fact that their daughter had cancer, so I think that takes its own emotional toll. I actually leaned on the Bible verses. I was like, “Okay, well, if God does save my life, I think he does have future plans for me.”
I cope with things maybe differently than other people. I tried really hard to think of the positives.
I was like, ‘Maybe it’s a compliment that I’m going through something bad because I am meant to grow and be so much more than the person I am.’
I find that when people go through life and it’s very stagnant and easy, you’re not growing. You’re just cruising through life, and I know that’s not the way I want to live. If nothing bad ever happened to you and your life, I wonder if you’re doing it right.
Bad stuff happens to people all the time, so either you’re not pushing yourself, maybe you’re not challenging yourself, or maybe you’re really lucky, which is great.
But for me I had a lot of bad stuff happen, and like Kelly Clarkson says, “What doesn’t kill you makes you stronger!”
I do find that looking at your past struggles and seeing how you survived that and how you cope with it can help you with the current struggles you’re going through with, and hopefully with the future struggles you’ll have.
Also just having friends and my family close by. When I talked to them, they encouraged me and gave me hope that I would be okay. I still was really scared, and all my human emotions were there, but I didn’t want to be a victim. I wanted to be a survivor.
To be a survivor, you have to look past what’s happening now and look to the good that can happen from it.
Dealing with uncertainty after treatment
I actually still have PTSD from some of the stuff that happened. Every time my teeth chatter, I think I’m going to have a seizure. Every time my cancer anniversary comes and my MRI happens, I’m always afraid that my cancer will come back.
I think it’s a fear that every cancer survivor has. Even if it’s “dumb” to think it would, I still think it can. I still deal with mental health issues today, just because it was such a traumatic experience.
But I also look at the good that has happened from it, and I think it helps me to cope. I think that’s a healthy coping mechanism for anyone else going through the cancer.
To just see anything good that can happen, not just the bad. Because if you just focus on the bad, it is very depressing.
The value of being vulnerable in sharing your story
Yes, because there’s always a risk that when you put yourself out there and you show the “bad or weak” side of you, people will judge you and will criticize you. They may not support you.
Me sharing that with my family, my friends, and posting a YouTube video about it — I put myself out there.
I knew people could have critiqued me, but actually I was met with a lot of support, and people didn’t say anything bad. If anything, they were just saying they’d pray for me and be there for me.
I want people to know when you’re vulnerable, don’t let the fear of being rejected or being teased about whatever you are being vulnerable about stop you from sharing your vulnerable moments.You actually might be helping more people than you think.
When they see that you’re being vulnerable, they get the courage themselves to be like, “Actually, you know what, I’m going through some stuff, too. Maybe I’ll reach out to that person and talk to them.” That’s a way healthier method to deal with some of the bad stuff in life, versus if I held at in and never got to share my cancer story.
I’ve had multiple people contact me through social media saying, “I’m going through the kidney cancer thing, too. What can I expect?” I tell them my experience, and I find that helps them.
I’ve been a social media support to somebody who is going through kidney cancer, too, for a bunch of people. I also blogged about my journey and tried to do a positive spin on it, so people can access my blog online as well.
They can read about my experience, as well as see my YouTube videos. It’s been a good step. Me being vulnerable has been positive in so many ways. I rarely have any negative feedback from it.
I encourage people to be vulnerable, but it did take a while to get to that point. I still had that mentality of wanting to be well liked by other people, showing them my good side, not my bad, because then people might think I’m weird or weak. I had to struggle with all those insecurities, too.
Thankfully, when I was able to step out of my bubble and share, people responded really well. Now I have no regrets about it, and I’m still sharing to this day. I’m always happy to share because more people need to do that.

What’s the importance of self-advocacy as a patient?
It helped that I was a nurse, so I knew when I had the surgery to ask for pain medication, fluids to avoid dehydration, stuff like that.
But for those who aren’t in the medical field, I think how you advocate for yourself is making sure you research what you’re going through.
Don’t be afraid to ask your doctor and nurses questions because you don’t want to bother them.
It’s your health, and you are the VIP.
Self-advocacy has to do with a lot of communication and saying, “Hey, I need to know this. What’s up, what can I expect from the surgery, what can I expect with the recovery, [and] what can I do for my pain management?”
Sometimes you can’t always have those questions right away. Just write it down. When you think about it, write it down so when you see your doctor or nurse, you can ask them.
Too many people are too afraid sometimes or just too shy to ask a question, but if you don’t ask, you won’t know what’s normal and what to expect. This is your first time going through cancer. It’s a scary thing, but don’t let the fear of the unknown stop you from asking the right questions.
That’s why I’m saying for self-advocacy, you have to communicate. Do your research. Don’t depend on WebMD, though. Go online, research some stuff, maybe talk to people who have gone through the same cancer.
Social media has actually been a really good resource for people going through cancer nowadays. I say use those resources to get connected, like how some people contacted me because I’m pretty open about my kidney cancer, and I was able to hopefully help them. I would like those people to then pay it forward and help other people.
Put yourself first. Self-advocacy means it’s okay to put yourself first. It’s not being selfish. You have to take care of yourself before you can take care of other people.
If you’re going through cancer, you need to make sure you take care of yourself because you’re going through a lot of stuff right now, more than the average person.
I would encourage people to communicate very well and then use your resources. Ask your family and friends, the supportive ones, maybe not so much the Negative Nancy ones. There are so many more resources nowadays with technology than ever, so why not take advantage of that?
»MORE: How to be a self-advocate as a patient
What kind of support was most important to you during surgery recovery?
We’re not meant to be alone. I think you can agree during this quarantine process, people don’t do so well. You can’t stay inside by yourself and expect to thrive.
We are social creatures, and even introverts need people. If I had to go through the cancer by myself, I don’t think I would have been able to go through it well mentally and emotionally.
Having people who have an outside view being able to listen to me vent, say encouraging words, and just show up — I think that helped me.
There are five love languages, and I am a big proponent of love languages. There’s physical touch, words of affirmation, quality time, acts of service, and gift giving. I get a lot of love from hugs, words of affirmation, and quality time.
For the quality time to happen, you have to be with people. Words of affirmation, other people need to share them with you.
The love languages are examples of what you’re supposed to do with other people. I felt very supported, and if I was lacking in any of those love languages, it would have been extra hard.
Yes, a support system is really important. I know not everyone is blessed to have one like I was, but if it’s not your family, hopefully some friends. Your neighbors are just people. Sometimes you least expect them to be there for you, but they’ll show up when you have something going on.
I had people contacting me, like some friends and acquaintances I had rarely talked to. They said, “Oh, I heard you’re going through this. I’ll be praying for you, and I’ll even visit.”
It was so surprising. It’s crazy how humanity can show up, surprisingly during the times that you need help. That’s part of being in a community. That’s part of solidarity. That’s part of having people as a support system.
Sometimes people will surprise you, and they’ll be very generous, very loving. It happens when you’re feeling at your worst, so don’t be afraid to reach out to people.
I think when I shared my YouTube video about the cancer, I was partly doing that to ask for help in a sense — like, “Please pray for me. I can’t just pray for myself; I need more people to help.” You just never know who can be there for you.
»MORE: What kind of support cancer patients say helped the most

“A new normal”
My life has been fantastic since the surgery happened. I actually made a bucket list because I thought I was going to die. It was filled with stuff — sometimes silly stuff, sometimes epic stuff — that I never had the time, the money, or the courage to do.
One of them was actually to become a CRNA, or a nurse anesthetist, which is what I am now. I didn’t think I was smart enough to do it. I still don’t think that, even though I am one right now. I went to school.
I decided why not?
I applied [and] got into a school in California. I miraculously made it, tricked some people into hiring me, and now I’m working in anesthesia! That’s been great.
I decided to skydive. I went on a cruise. I swam with dolphins. I made a 32,000-piece puzzle. I’ve done a lot of epic things on my bucket list, and I wouldn’t have had the courage to do any of that if I didn’t go through my cancer.
So I would say survivorship has been fantastic. When you think you’re going to die and then you have a second chance at life, live it up. Let’s do things that you might not have thought to do before! That YOLO (you only live once) lifestyle, I really liked it.
I think that also made me appreciate people more. I try to say a lot more nice things to people because you never know. Something can happen to me tomorrow, and then I’ll regret not saying something nice to so-and-so. Might as well say it today so then they feel loved.
All the stuff I’ve been able to do has been really fun. I visited the Taj Mahal, went on a mission trip, just random things. Sometimes some of my bucket list things are silly, like I went trick-or-treating for the first time a couple years ago, and I never did that before. I learned how to pump my own gas because in Oregon you don’t pump your own gas!
There’s been silly things that I’d like to do. I made a dance video. I like to rap sometimes. I like to put myself out there because it’s just more fun. It makes people smile and laugh.
I love making people smile and laugh because it brings a little bit of joy in their life. In this dark, dark world and in this time that we are living in with COVID, there’ve been a lot of depressing, sad things.
I’d like to try and put a little bit of happiness back into it just by being myself. I’d encourage other people to make the most out of survivorship. You never know what’s going to happen next, so spread as much love as you can.
Life’s too short to live it just as a victim in a sad way. Might as well spread some joy, take care of yourself, and have some happiness along the way, too.

Last message for other patients and caregivers
Take it one day at a time. There’s no point in worrying too much about what’s going to happen in the future. It’s easier said than done. I was planning my memorial, so I wasn’t even taking my own advice back then. I was planning too much in the future.
But there’s going to be so much coming at you when people are first diagnosed with cancer. For me, it took a week for just all these events to happen. Then I was officially diagnosed with cancer.
Depending on other people, their story, and what they are going through, just take it one problem at a time, one day at a time.
I hope you have good coping skills because this is the time to use them. Figure out [how] to take care of yourself physically, mentally, emotionally, and even spiritually, and go back to those things.
If spiritually you need to read the Bible and pray, do that. If emotionally you need to cry, do that. If mentally you need to vent to people or take up a hobby that makes you feel better, do that. Physically, if you can, go for a walk, something that helps you to calm down and relax.
You need those self-care moments. It’s all about self-care, because you are going through so much. You have to make sure you make time for yourself to give yourself something positive to look forward to.
I know some people have to go through radiation. They have to deal with a much longer process of healing from the cancer, and that can be a lot.
You are going to get chemo. You are tired all day. It’s like day after day, you do that.
So please have time set aside each day where you can do something that you love, that gives you happiness and joy, and that will help you keep going.
You can get burnt out trying to fight this thing, this horrible thing called cancer.
Take it one step at a time, find a good support system, [and] find a way to help you be resilient from all the trials. Because you’re going to be beat down every day, and you have to stand back up and fight this again.

You can’t do it by yourself. I just encourage people to please reach out to your communities. Reach out to your family and friends if you are going through this.
If you are first hearing about the diagnosis, you need to process it yourself, but you also need to have some people who can support you throughout this process, too.
Even if they can’t understand what you are going through, even if they will never understand because they are not the ones going through cancer, if they are there with you, that will help you more than you think.
Just take care of yourself, seriously. If you can find a little bit of hope, a little bit of joy each day, that’s all you need to keep going. Too often we focus on the negatives because it’s very easy to focus on the negative, and we need to fix our mindset and have a little faith. Focus on a little bit of hope, little bit of love, a little bit of joy, and I think that will help.
Sometimes strangers can be your support system. Use your resources, and you can do it. There are cancer survivors all the time. Just because you get diagnosed with cancer doesn’t mean that you are going to die.
You’ve got to fight it, keep fighting the good fight, and keep working on it. You can be a survivor, too.

Inspired by Nina's story?
Share your story, too!
Chromophobe Renal Cell Carcinoma Stories
Nina N., Kidney Cancer (Chromophobe Renal Cell Carcinoma), Stage 2
Symptoms: Blood in urine, blood clots, intense abdominal pain
Treatment: Partial nephrectomy (surgical removal of right kidney)
...
4 replies on “Nina’s Stage 2 Chromophobe Renal Cell Carcinoma Kidney Cancer Story”
Thanks, Nina. Thank you for taking the time to tell your story. My Surgery for non chromophobe RCC is in 1 month. Your story has been incredibly enlightening. Looks to me like you are back to full function. Congrats on completing your schooling and your new career. Success occurs when preparation meets opportunity. Maybe all that you went through was the preparation you needed to land you where you could be most effective and be the most relevant. You Rock.
Thank you Nina for sharing your story. I too was recently diagnosed with a Chromophobe tumour, I’m a 27 year old female, so it was a shock. Hope you are well and healthy 🙏🏻 God bless.
You are an inspiration and a miracle.❤️
Beautiful and Brave????