Navigating Life with an Ostomy: Tips from Patients and Medical Experts
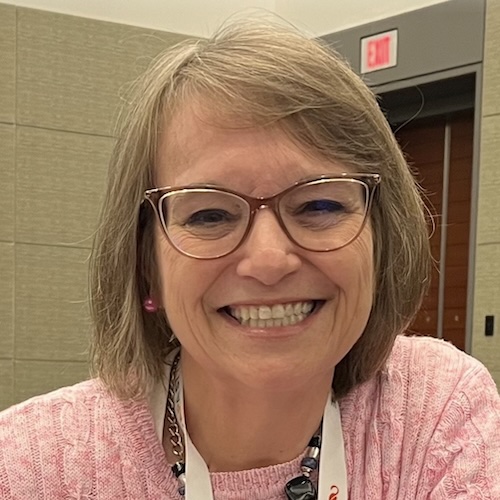
Undergoing an ostomy procedure involves major changes. To offer guidance, The Patient Story hosted a live discussion with colorectal cancer patients Amy Hart and Jason Randall, who both have ostomies, along with Dr. Vanessa Wookey, a gastrointestinal oncologist from Fox Chase Cancer Center.
From their real-life expertise, they offer practical advice about living with an ostomy, from diet and clothing tips to cleaning and skincare. Plus, Amy and Jason share how they wear an ostomy with body-positive confidence.
Living with an Ostomy full video conversation
What is an Ostomy?
An ostomy is a surgical procedure that brings a section of the intestine or urinary system through an opening (stoma) in the abdomen. Waste passes through the stoma into an external pouch or ostomy bag attached to the skin.
Ostomies allow the bowels or bladder to function after injury, disease, or birth defects. Reasons for getting one include colorectal cancer, Crohn’s disease, bladder issues, and birth abnormalities according to the United Ostomy Associations of America, Inc.
“You can still do everything you could do before. You can swim and go in hot tubs. You can do everything. It’s not limiting like you might think it is. There’s so many different kinds of bags you can use, so figuring out what’s best for you is a process.”
Catherine P.| Explore her Stage 3 Adenocarcinoma Rectal Cancer Story
Seeking Support for Daily Living Tips
Jason, who has had both an ileostomy and colostomy, highly recommends joining an ostomy support community. “It’s really helpful to ask people questions and dive into the more in-depth stuff,” he says.
Amy, who shares her experiences online, agrees. “Seeing other people, maybe four years down the road, allows you to see what your life could look like after this massive change.”
Dr. Wookey stresses the value of connecting with those living with ostomies day-to-day: “The best thing patients want is someone who can help them figure out some of the troubleshooting.”
Finding the Right Bag System
There are various ostomy pouching systems available. Jason emphasizes trying different products patiently to see what works best.
“What one person may work well for them, may not work for another person,” he explains. He started with a two-piece system but found a one-piece pouch simpler.
Amy switched her ostomy bag based on a friend’s recommendation. “It worked out great,” she says. Reaching out to manufacturers for samples helps find the optimal ostomy bag.
“Any closed system is not a good idea if you have an ileostomy, because you’d be changing it all day long. Whereas with a colostomy, it’s a little more predictable. It’s easier to manage. People tend to go with closed systems for convenience.
I used to be a 2-piece ostomy person for both my ileostomy and my colostomy. I’ve had about 2 years of colostomy and 3 months of ileostomy. With the colostomy, I’ve gone down to a 1-piece system.”
Jason Randall | Explore Jason’s Stage 4 Colorectal Cancer Story
Diet Tips
According to Dr. Wookey, there’s no singular best ostomy diet. She advises starting with a low-fiber, low-fat diet after surgery and then slowly reintroducing foods.
Amy adds, “I eat everything. I just introduced it in small quantities and with a lot of liquids.” She stresses thoroughly chewing food to aid digestion.
Jason recommends tuning into your body’s signals if certain foods cause discomfort. He takes supplements to relieve symptoms of obstruction when needed.
Preventing Leaks and Skin Irritation
To prevent ostomy pouch leaks, Jason uses special rings around the stoma opening for protection. “Getting a pre-cut bag and not cutting it yourself creates a much better seal,” he says.
For skin irritation, Dr. Wookey advises gentle cleaning around the stoma: “Using just water or a gentle soap is really the most you need.” See your doctor for significant redness or wounds.
Ostomy Clothing Tips
“My life as far as using the bathroom is altered but the only part that’s really impacted by that is the part that happens when I close the door and no one’s in there with me.
[As] life does, it takes a really long time for it to re-settle down, but it does settle back down.”
Amy Hart. | Read Amy’s Stage 3B Colorectal Cancer Story
Amy suggests stretchy, high-waisted clothing styles to accommodate ostomy pouches. She also wears bike shorts under dresses for security.
For men, Jason fuses a belt called Stealth Belt to keep his pouch securely in place during activity. This also helps prevent abdominal hernias.
Life after ostomy surgery involves adjustments. But support groups, finding optimal products, and an adaptable mindset makes thriving with an ostomy completely possible.
Colorectal Cancer Stories
Sydney S., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Constant stomachaches that only went away after bowel movements, pain after eating, changes in bowel size and shape
Treatments: Surgeries (colectomy, temporary ileostomy, ileostomy reversal), chemotherapy (FOLFOX, FOLFIRI, trifluridine and tipiracil), monoclonal antibody (bevacizumab), radiation therapy, hormone therapy
Kristie C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: None per se that she noticed; she experienced constipation and passed narrow stool, but had been experiencing constipation most of her life, and thought that these digestive issues could also have resulted from perimenopause
Treatments: Chemotherapy (including adjuvant chemotherapy), radiation therapy, ablation therapy (liver ablation), surgeries (colectomy, temporary ileostomy, ileostomy reversal, scheduled liver resection)
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy