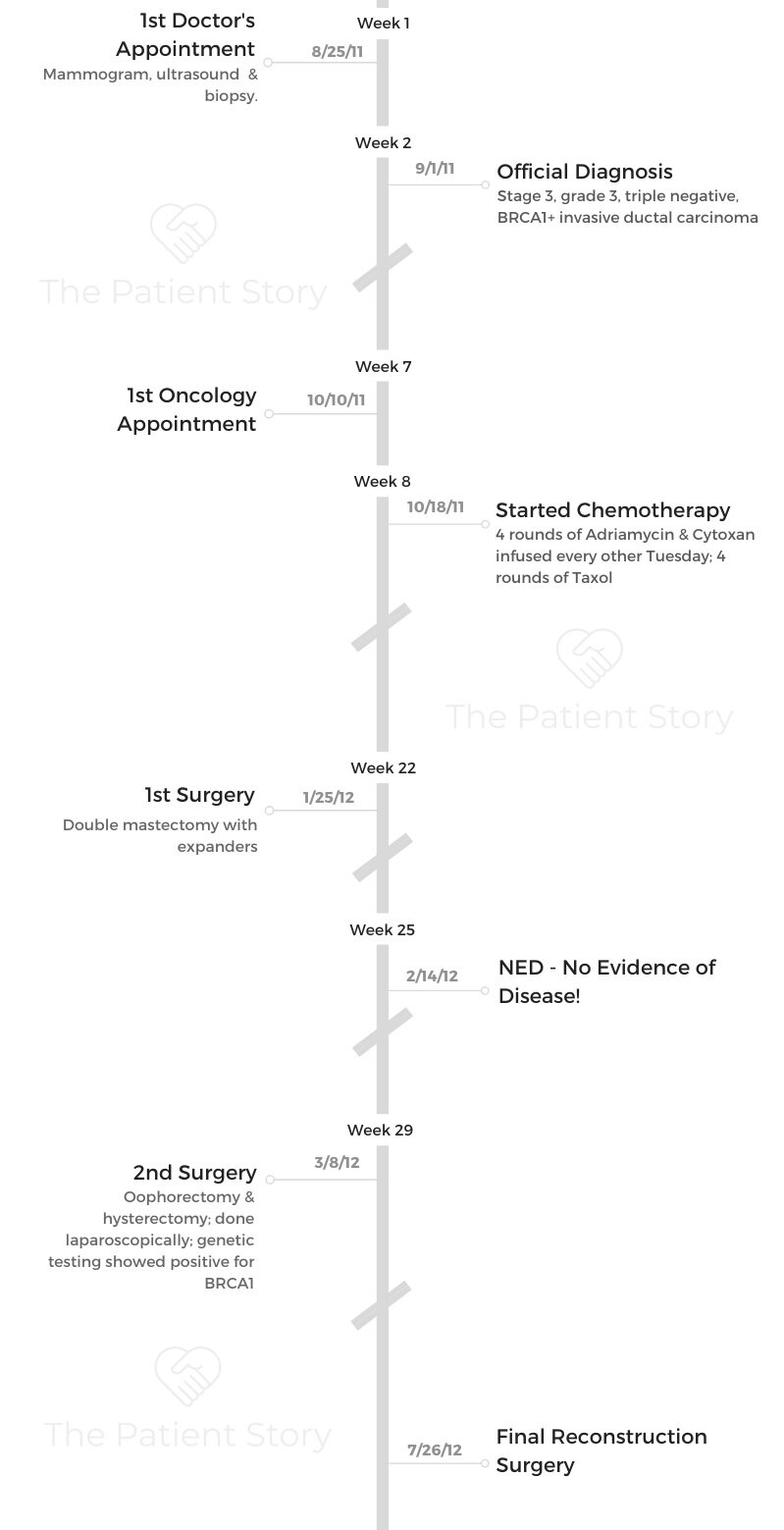
Stephanie’s Stage 3, Grade 3, IDC, BRCA1+, Triple-Negative Breast Cancer Story
Stephanie shares her stage 3 triple-negative breast cancer story, diagnosed after she found a small lump in her left breast. She details going through treatment: chemotherapy, double mastectomy, oophorectomy, hysterectomy, and breast reconstruction.
In her story, Stephanie also highlights the importance of patient self-advocacy, guidance for couples going through cancer, and how cancer changed her view of cannabidiol (CBD).

- Name: Stephanie J.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- Grade 3, triple-negative (TNBC)
- BRCA1+
- Staging: 3
- 1st Symptoms:
- Small lump above nipple in left breast
- Treatment:
- Chemotherapy
- 4 rounds of Adriamycin & Cytoxan
- 4 rounds of Taxol
- Surgery
- Double mastectomy
- Oophorectomy & hysterectomy
- Breast reconstruction
- Chemotherapy
- Diagnosis
- Chemotherapy
- Surgeries
- Quality of Life
- You’re thinking of getting a mastectomy tattoo
- Can you talk about self-advocacy?
- Can you talk about hair loss?
- How did the cancer affect your relationship with your husband?
- Do you have advice for other couples going through cancer?
- How did your kids react to your diagnosis?
- How important was it for you to have caregivers?
- How has your experience changed the way you view CBD
- What is your “new normal” after cancer?
- What is your advice for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Know that this is survivable. Breast cancer is one of the most survivable cancers.
Make sure you eat and you rest. Those are the 2 things that you’re not going to want to do because of the drugs you’re taking, but you need food, and you need rest.
You need to do everything in your power to make yourself be able to do those 2 things. That’s how your body is going to heal.
Stephanie J.

Diagnosis
Describe the lump you found
In spring, I was giving myself a self breast exam. They say you’re supposed to do them every month, but I would say I did them every 6 months or whenever I would think about it.
It was right on the top on my left breast above the nipple area. I could touch it. When it first came in, it was itty bitty. Your breasts swell because you have cycles, and when that happened, it seemed to go away.
Over the summer, though, it got to be about 3 cm. It was pretty aggressive. Triple negative is known for being pretty aggressive.
When did you go to the doctor?
I didn’t go to the doctor until August. When it was obvious it got bigger and wasn’t going away any time soon, I decided I should get it checked out.
I was self-employed, and I didn’t have insurance. I thought, “If it’ll go away, fine.”
I started researching options on how to get it checked out. I pretty much just wanted to confirm what I already thought it was at that point.
What resources did you find for getting care while uninsured?
In Dallas, we have Baylor Hospital. They have a big cancer center. I’ve always been a researcher, so I started going to the library at the hospital and asking around.
I got referred to the Bridge Breast Network. They’re a group that helps uninsured and underinsured women of Dallas and Tarrant county get diagnoses. They got me a mammogram and biopsy.

How did you get the diagnosis?
It wasn’t a terribly long process. First, it was the mammogram. They noticed the lump and did the ultrasound and needle biopsy that day.
That was weird because they numb you. I was watching the screen and the needle going into the tumor, but I didn’t feel anything.
It wasn’t as scary as I thought it was. It wasn’t bad. It took about a week to hear back on the results.
I was working part-time at a taco joint and bar. This lady came in, and she was bald and dressed in pink head to toe. She was there to see her grandson play a show next door.
I told her I just had my biopsy done, and she was so sweet. She said, “If it happens, just know that I’m almost done, and it’s survivable.” She took my info and kept up with me for a while. That helped me a lot.
My doctor called me about a week later. I feel bad for medical professionals because they have to deliver bad news all the time.
She called me and said, ‘We got your results back. It is cancer.’
It’s almost like a punch in the stomach. You know it’s coming, or you at least have a feeling that it might be coming, and you prepare yourself. Then you hear it, and it still took my breath away.
I didn’t know what I was going to do with this diagnosis since I didn’t have any insurance. The doctors called the Bridge as well and let them know the results.
They called me up and invited me in. They gave me a treatment packet. They told me all the doctors they had set me up with. They really were instrumental in me still being here.
What was your treatment plan?
Because of my staging and grading, I was given a 23% chance of living to see 5 years. Here I am 10 years later, still kicking.
Because I was triple negative, my doctor said if I responded to chemo, things would look pretty good, but if I didn’t and it metastasized, there wasn’t going to really be anything they could do.
I was going to do 4 months of chemo, then a double mastectomy with expanders and reconstruction.
They did a mouth swab for genetic testing and found out I was BRCA1+, so they wanted to clean house with an oophorectomy and hysterectomy after the mastectomy, too. They were pretty thorough. My final reconstruction surgery was about a year after my diagnosis.
Chemotherapy
Can you talk about the chemotherapy?
Chemo is the one thing everybody dreads. It doesn’t look pleasant. I wasn’t excited about it at all. Being the researcher I am, I looked into everything. I had 2 stages of chemo. The first was Adriamycin and Cytoxan. The second half was Taxol. I did 4 of each.
I researched how to endure chemotherapy. Of course, an illegal way to endure chemo is cannabis. I had never really spent much time with it, so I talked to friends that knew about it. I asked my oncologist about it, and he said he couldn’t tell me to do it because of legal reasons, but he also didn’t tell me not to use it.
I was 1 of a few patients he had on chemo at the same time. I was 1 of 2 that was using cannabis, and we were the only ones that actually gained weight on chemo.
I had infusions every other Tuesday. They had to hit me pretty hard. I was really drugged up on the first infusion day. They gave me Benadryl, steroids, and anxiety medicine. I hated the steroids. I felt like the whole apartment was spinning that first night after getting infused.
What chemo side effects did you experience?
The AC wasn’t fun. I had leg muscle pain with the Taxol. I also experienced some neuropathy. The skin on my feet and fingers was tingly and painful. The Taxol was probably harder.
Both kinds sucked, but the Taxol was harder. They also gave me Neulasta shots after chemo to make my body produce white blood cells. That made every bone in my body ache.
It took about a week for me to start to feel better. Chemo side effects are cumulative, though, so the further along in the process, the more everything hits you and the harder it is to recover.
»MORE: Cancer patients share their treatment side effects
How bad did it get during chemo?
My husband is a tattoo artist, so he works nights. He came home one night, and I was lying on the floor underneath the coffee table gripping the legs of it because I was in so much pain. I don’t like pain meds and opioids or anything like that.
That was the one time I had to call and ask my doctor for something. I was lying on the floor, crying, for a while until he got home.
That was the one time I thought, ‘This is going to kill me. I’m not going to survive this.’
What advice do you have for someone going through chemo?
I’m a big proponent of cannabis and CBD if you’re in a legal state. I don’t want to recommend that you break the law, but I will say I can’t imagine going through chemo without it. Even with it, it was really difficult, but it helped a ton.
Always talk to your doctor. They’re a part of your team. Don’t keep things from them. Know that this is survivable. Breast cancer is one of the most survivable cancers.

Make sure you eat and you rest. Those are the 2 things that you’re not going to want to do because of the drugs you’re taking, but you need food and you need rest.
You need to do everything in your power to make yourself be able to do those 2 things. That’s how your body is going to heal.
»MORE: CBD, Cancer & Treatment Side Effects
Did chemo put you in remission?
We did a PET scan before I started. I did a few CTs throughout. They would do ultrasounds here and there, but the big scan was after chemo. At the end, they did another PET scan, and that’s when I found out I was in remission.
I was glad when he told me, but I knew I still had to get through the next 5 years. Then 2 weeks after that, I did my double mastectomy.
Surgeries
What was the double mastectomy like?
Prep beforehand was really about making sure my body was strong enough and could handle surgery. I drank a lot of protein shakes and really watched my diet to make sure I could take the surgery.
The day of the surgery, we got there at like 5 a.m. It was an 8-hour surgery, so it was a long day. I was out, so I didn’t know it, but it took a while.
It was like 2 surgeries because the breast surgeon took everything out, and then the plastic surgeon came in and put everything back together with the implants.
Waking up from surgery was one of the most painful experiences of my life. I’ve had 2 sons naturally, and getting my breasts removed was on par with that.
Waking up from surgery was terrible. They have to split the chest muscle, so it was rough. That’s what really tore me up, I think.
I was in the hospital for a few days, went home, and rested and recovered. I was nervous about being able to handle the recovery. I had 2 drains coming out of me. I had to learn how to take care of those. I didn’t want to cause any infections.
What were the oophorectomy and hysterectomy like?
They did both at the same time. The gynecological oncologist who did the surgery was in the other room and was controlling a robot. I don’t know how to describe it other than it’s just really cool science stuff. I was only in surgery for 3 or 4 hours.
They inflate you, and they make tiny incisions in the bikini area. Now I can hardly see my scars. That surgery recovery wasn’t nearly as bad as the double mastectomy. I didn’t really have a lot of pain or anything. I had gas built up from being inflated. That’s not so fun, but that’s about it.
I couldn’t drive for a while after the hysterectomy. It took about 6 weeks before I was cleared to drive.
What was the reconstruction surgery like?
Throughout my treatment, I was getting my breast expanders filled. When they filled the expander, they would take a magnet and it sticks to a metal valve. When it sticks, that’s how they know where to add the fluid. They do a little at a time, so it wasn’t painful really.
The reconstruction surgery was a nice little day surgery. I felt better after that surgery because the expanders are heavier than the implants.
I felt lighter. I just had to live in a sports bra for a while. It was no big deal.
Quality of Life
You’re thinking of getting a mastectomy tattoo
I haven’t done it yet, but we’re planning a mastectomy tattoo. My husband is going to do it for me.
He was horrified by the apparatus in the plastic surgeon’s office that they use to tattoo nipples. He takes his work very seriously.
We’ve been trying to decide on a design. A tattoo artist is going to be good at realism, so I’m sure he could do a 3D nipple, and we might go with that.
But while you’re there, why not add a cool design? I’m a creative professional, and I’m pretty tattooed already, so I’m working on something a little more involved.
We’re thinking of doing some filigree design with hearts. My scars travel from nipple to pit on each side, so we might do some sort of vine with flowers following that.
You can tattoo over scars. I don’t have a lot of feeling near my scar, so it’d probably be the easiest tattoo I’ve ever gotten.
My husband is just going to bring his stuff home, and we’ll do it on the house.
Can you talk about self-advocacy?
During the process of going through cancer, you just lose all autonomy. You’re no longer your own person for a little while. Knowledge is power.
Sometimes we get scared, and we don’t want to know, but it’s best to be a student of the disease. Learn everything you can and be your own best advocate.
All of my doctors were very open and communicative. They saw early on that I asked a lot of questions and knew my stuff, and I think they appreciated that.
»MORE: How to be a self-advocate as a patient
Can you talk about hair loss?
I asked them about hair loss, and my doctor said it would happen on day 14. I thought that meant I was going to wake up on day 14 and have a ring of hair on my pillow.
It wasn’t like that at all. I buzzed my hair in preparation. I woke up, and I still felt my fuzz.
I went to run some errands with my friend. We were in the bank parking lot, and I went to scratch my head, and it was all full of hair. We both looked at each other, looked at my hand, looked at each other, and started crying.
Now I look sick. Now people are going to know I’m a cancer patient. That was harder for me. Having no hair meant that people would know I had cancer, and that bothered me because I hate the sympathetic head tilt.
Eventually, all my hair fell out all over my body. Something people may not realize this, but even your nose hairs fall out, so your nose is constantly running. I only grew about two-thirds of it back, so I always have tissue on me.
If you can, buzz your hair. It feels like it would be more traumatic if it was long and coming out in big clumps than if you just go ahead and buzz it and start getting used to the short hair or no hair.
Plus, when the fuzz comes out, it’s a little easier to handle than I imagine it would be if my hair was its normal length.
It usually comes out in patches, so if it’s buzzed, it comes out easier. After the fuzz started coming out, I went ahead and shaved it. I went through chemo in winter, so it made it really easy to have knit caps on all the time. If not, I would just rock the bald head.
»MORE: Dealing with hair loss during cancer treatment
How did the cancer affect your relationship with your husband?
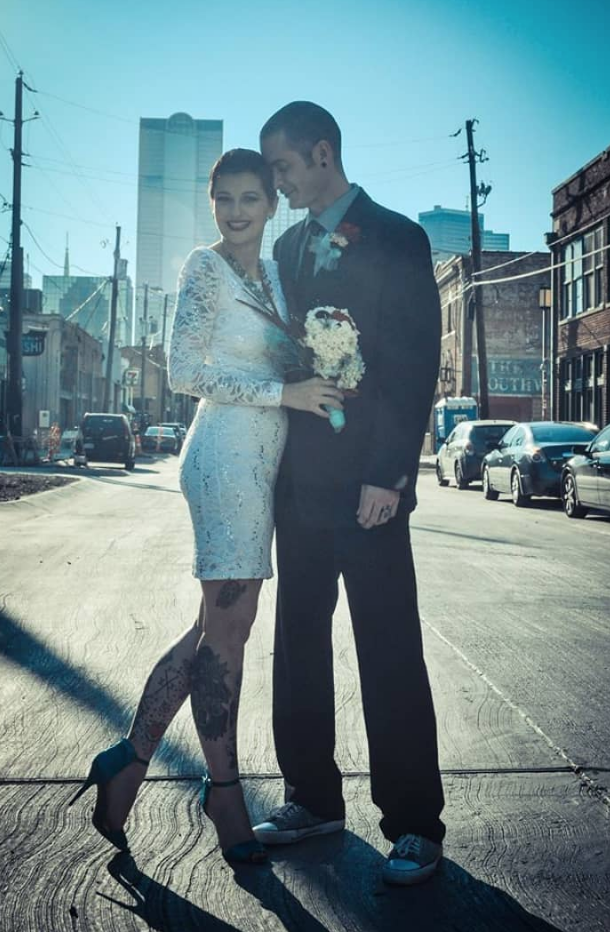
It’s funny because we were just friends when I got diagnosed. We hung out with the same people. He would come around and check on me when I worked at that bar. He’d come sit, but I’m clueless, so I never got it. I don’t do signals well.
Then I got diagnosed. A week after I got the diagnosis, I posted on Facebook that I wanted to have a nice night out before treatment started. He was like, “I’m down. Let’s do it!” I’m still clueless at this point, but I of course agreed.
We ate sushi and went to a concert. At one point, the band was taking a break, and there was just overhead music playing. He leaned over and said, “I want to be with you through everything.” I was like, “I don’t even know what everything means.” He just said it again more emphatically.
We’re about to have our 5th wedding anniversary now. He never missed an appointment or surgery. He’d work until 2 or 3 in the morning and have me to pre-op by 5 a.m.
He would tell me I was beautiful even when I had drains and no hair. He’s just a good dude.
Do you have advice for other couples going through cancer?
The human brain is wired to be scared of things because we want to survive. In order to make a relationship work, you have to push through fear to get to the love.
People often get this mixed up: the opposite of love isn’t hate. The opposite of love is fear.
Thankfully, my husband pushed through his fear, and we’ve made it through to the other side now.
As a caregiver, that’s good to keep in mind. It’s okay to be scared, but you just have to get through it.
You’re on a journey together. It’s okay to cry together and experience it together. The cancer patient is the patient, but the caregiver has feelings, too. If you need to go to some type of counseling to get through it, do it. Therapy works.
Always be patient. Understand that the both of you are going through it. Try not to isolate yourselves. Be together.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
How did your kids react to your diagnosis?
They were both in high school. My younger one was a freshman. I just thought, “I want to live long enough to see them both graduate high school.”
I’m a matter-of-fact kind of girl. I just tell the truth and deal with it. So, I met with them and their dad. I talked to their dad first and told him we needed to tell them together. We sat them down and just told them.
They had just lost their grandfather to throat cancer a few years before this, so naturally, they were both terrified. I just let them know that I was going to put in my best effort.
That was hard to know they were scared I was going to die. Deep down, I was scared of leaving my children, but I didn’t say that to them obviously.
Telling your kids is an emotional time. I’m grateful they were old enough to understand and take care of themselves if they needed to.
I imagine it’s incredibly tough for mothers with younger children, who can’t understand. I knew if I didn’t make it for some reason, they would at least be able to comprehend it.
»MORE: Parents describe how they handled cancer with their kids
How important was it for you to have caregivers?
The support system I had is another big reason I’m still here. My husband, my friends, and women I met through the Bridge Network. They also had therapy.
Baylor offers things like that. That’s a great thing. People in medicine are realizing there’s a whole body wellness. The mind and the body are connected.
Having mental and emotional support was really instrumental in my recovery.
I had friends come over with food, and we would watch bad TV together. Another friend came over to teach me how to draw my eyebrows on. Little things like that got me through the bad stuff.
»MORE: What kind of support cancer patients say helped the most
How has your experience changed the way you view CBD
I work for an ad agency, and we do a lot of work with CBD and marijuana companies. It’s really nice to be on this side as a Gen X person. It’s neat to be able to put my experience out there and try to change the stigma.

I had a friend who was sick, and she couldn’t take pain meds very well. I brought her some CBD ointments and things so she could at least try to rest.
Being able to take my knowledge and skill set to help other people maybe find a product to help them get through cancer is amazing.
After my cancer, that’s when I really started wanting to be in this space. I was a DARE-generation kid, so it was a shift for me.
To this day, it helps with my chemo-induced IBS, hot flashes, and neuropathy.
»MORE: CBD, Cancer & Treatment Side Effects
What is your “new normal” after cancer?
For me, it was living every day with intent. I don’t stress about the things I can’t control as much anymore. I can only control how I react to things.
Also, I’ve got new fuel for my fire to do things I want to do. I want to photograph all the state parks in Texas before I die. Things like that. I try to go for things more.
I also care for myself more than I used to. Self-care and taking time to make sure I’m rested used to be on the back burner a bit, but it’s not now.
I like to read, so I try to make sure I dedicate more time for that. I love to be in nature, so 1 or 2 weekends a month, I go to a state park. Self-care is subjective, so you get to choose what feeds your soul.
Time with my family and time doing things I enjoy are what’s important to me, but self-care is about what’s important to you.
What is your advice for someone who has just been diagnosed?
Research. Communicate with all of your medical professionals. Don’t be afraid to venture into spaces that have been scientifically proven to help you. Knowledge is power. I think research is the number one thing you can do for yourself once you’ve been diagnosed.

Inspired by Stephanie's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




