“My Nose Was Changing Shape”: Vikki’s Nasal Squamous Cell Carcinoma Experience
Courage, Connection, and Acceptance with Nasal Squamous Cell Carcinoma
What began with a series of small nosebleeds in late 2019, would become a diagnosis Vikki never expected: nasal squamous cell carcinoma, a rare cancer that can be classified as head and neck cancer or a form of skin cancer. Living in the United Kingdom, Vikki is a young mother devoted to fitness, nature, and her children. These nosebleeds persisted for years. Multiple doctors treated her for infections and prescribed cauterization, but no one recognized the underlying issue. Over time, her nose visibly changed, her septum collapsed, and the pain intensified.
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez
Only after demanding a biopsy in summer 2024 did Vikki finally learn the truth: squamous cell carcinoma had invaded her septum and bone. The diagnosis of this kind of head and neck cancer was confusing and shocking, yet came with little support. Vikki said, “I think I’ve just been told I’ve got cancer. What’s happening?”

As she sought answers, Vikki’s head and neck cancer experience quickly accelerated. She underwent aggressive surgeries, including substantial removal of nasal tissue, and months later, reconstructive surgery on her skull, skin, and arm. Hospital stays were grueling, and she chose not to see her two-year-old daughter until she recovered some sense of herself.
Vikki endured daily radiotherapy, weekly chemotherapy, and challenging, life-altering side effects: she lost her sense of taste, struggled to eat, and had to learn to live with a major facial difference. She had periods during which she couldn’t leave the house because she couldn’t deal with people staring at her.
Her head and neck cancer experience, however, is a testament to personal transformation. Vikki found new confidence and meaning through connection, community, and self-acceptance. It heartened her to learn that her appearance was the least interesting thing about her. Today, she advocates for awareness, encourages others to find the right support, and insists that appearance is never the measure of a person’s worth.
Watch Vikki’s video and scroll through the edited transcript of her interview below. You will:
- See that persistent symptoms deserve thorough investigation. Keep pushing if answers aren’t clear
- Learn that appearance changes from head and neck cancer can cause deep psychological distress, but can never diminish one’s worth
- Realize that who you are matters more than how you look. As Vikki says, “It is the least interesting thing about you”
- See how support groups and sharing with others facing facial differences can reduce isolation and build resilience
- Explore Vikki’s transformation: From valuing external beauty to embracing connection, self-compassion, and a broader definition of identity
- Name: Vikki F.
- Age at Diagnosis:
- 34
- Diagnosis:
- Head and Neck Cancer (Nasal Squamous Cell Carcinoma)
- Symptoms:
- Nosebleeds that persisted for years
- Nose changed in shape
- Nasal pain
- Migraines
- Treatments:
- Surgeries: subtotal rhinectomy, reconstruction surgery including radial forearm free flap, bone grafts, and cartilage
- Chemoradiation
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- I'm Vikki
- My early symptoms: nosebleeds and pain
- My nose changed shape
- My diagnosis experience was shocking and confusing
- I had mixed emotions, relief, and realization
- Finding the right care team
- We found that my cancer was aggressive
- Facial reconstruction, hospital stays, and my recovery
- My treatments had brutal effects
- Mental health, identity shift, and life lessons
- My advice for other patients
I’m Vikki
I’m Vikki. I live in the UK. I was diagnosed with nasal squamous cell carcinoma in August 2024.
I love rock climbing, being in the sea, surfing, and hanging out with the kids on the beach. I’m passionate about health, fitness, and longevity, and I’m a keen reader.
My early symptoms: nosebleeds and pain
Around October 2019, I started having little nosebleeds. I assumed it was winter, it was because of me getting older, or it was due to the air conditioning drying out my nose.
Over the next three years or so, they got worse and more frequent. Every time I touched my nose, when I’d wash my face or anything, it would bleed, sometimes for 5 to 10 minutes. My nose became quite sore. My stepson would accidentally bop my nose, and I’d see stars from the pain. It would bleed for a whole toilet roll’s worth.
Doctors treated me for sinus infections and kept cauterizing the sore, hoping the bleeding would stop, but no one knew the true cause.
My nose changed shape
By October or November 2023, I noticed my nose was changing shape. A red patch appeared, and I was getting a bit of a hump. I had to produce photos of my side profile: summer 2023, my nose was straight, and by summer 2024, there was a big dip and a hook. My septum had collapsed. That made doctors finally pay attention.
I couldn’t wear sunglasses due to pain, and I had migraines, which worsened.
My diagnosis experience was shocking and confusing
Eventually, someone biopsied me. Inside my nose was a kind of skin cancer.
After insisting, I got a biopsy in July 2024. A few days later, I had a three-minute appointment. “It’s SCC,” or squamous cell carcinoma, they said. I asked, “What’s that?” They said, “You need treatment.”
I got a leaflet, “You have cancer,” and was told to call a nurse. Nobody explained what was happening.
When I reached the nurse on Monday, she booked an appointment with the head of ENT and a Macmillan cancer nurse. Only then did my husband and I learn it had spread and taken a lot of my nasal tissue, but the hospital couldn’t even say which team would treat me.
I had mixed emotions, relief, and realization
The symptoms had worsened for so long that part of me expected something serious. But nothing had suggested cancer. I was relieved to know what it was. Everyone was light-hearted since “SCC is the best skin cancer to have.”
But Googling showed how serious it could be if it spread. And scans revealed it had gone into my septum and nasal bone.
I was convinced I was going to die; I experienced panic attack-level fear. No one told me about the risks or the need for additional tests.
Finding the right care team
I’m lucky to live near Southampton General Hospital, a specialist cancer center. I was referred to skull base and maxillofacial specialists due to concerns that it was in my skull.
They did more scans. The teams decided the cancer had not spread to the skull bone, so I stayed with the Maxfax team for treatment planning.
I was invited to an MDT meeting and met the leading head and neck surgeon in the UK. Scans showed that the cancer had spread around one nostril and deep into the septum and nasal bone. Half my nose was okay, but the cancer breached the skin.
The plan was to remove all cancerous tissue and my whole septum. Because I was young, they prioritized the cosmetic outcome and immediately involved a plastic surgeon. The option was to do a subtotal nose removal, then see how much could be saved.
The surgery was scheduled for late October or early November, with histology afterward to determine the next steps.
We found that my cancer was aggressive
Histology took over three weeks and showed the cancer was very aggressive. It had started to get into the nerves and capillaries.
Although it hadn’t spread to lymph nodes or lungs, my team decided to throw everything at it: additional surgery to clear margins, daily radiotherapy, and weekly chemotherapy. No reconstruction until six months after completion.
Facial reconstruction, hospital stays, and my recovery
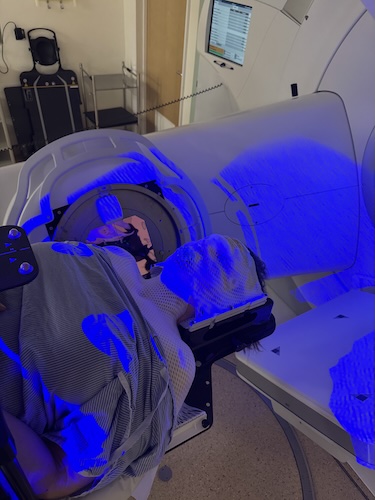
I had my first reconstructive surgery in June; multiple smaller surgeries will follow.
The process was physically and emotionally grueling. Post-surgery, nerves, tissues, and even bone from my skull and skin from my arm were repurposed for my face.
I wore a cast on my arm. I had wounds on my hip and a swollen neck. I stayed nine days in the hospital for close monitoring.
I opted not to let my two-year-old daughter visit at first because I didn’t look, sound, or smell like “mummy” and was heavily medicated.
It was the longest I’d ever left her. It was incredibly hard. Dad handled things at home, though.
For the first two years, monthly scope checks and six-month CT scans are standard. Additional surgeries are scheduled, and I have another nine months of adjustments ahead.
My treatments had brutal effects
Radiation to the head and neck is brutal: within days, I started experiencing side effects like swollen lymph nodes, severe mouth blisters, and constant vomiting after chemo. I needed to take morphine for the pain.
By week four, I had permanent “sunburn” on my face, hair loss where the radiation shot through, dry mouth, and chronic mucus.
Eating was nearly impossible; I survived on protein shakes with numbing agents.
Despite knowing treatment had an end date, the life-changing effects were the facial difference and the changed appearance. Not leaving the house because I had to face stares and comments was the hardest thing.
My confidence grew slowly, and a cancer appearance styling workshop became a turning point.
Compelling Quote: “Without sounding arrogant, I was a reasonably attractive, young woman. And now I have a substantial facial defect… I’ve had periods where I couldn’t leave the house because I couldn’t deal with people staring at me.”
Mental health, identity shift, and life lessons
My mental health has been up and down; with previous experience in therapy and coaching, I could sometimes pull out of spirals, but pain and shame were frequent. The shame was both for my appearance and for having cancer “impact my family.”
Nutrition, exercise, and kindness helped speed recovery.
Cancer shifted my identity from valuing appearance and work to embracing connection, kindness, and fun.
My self-worth no longer rests on how I look. “It is the least interesting thing about you.”
My advice for other patients
Sometimes cancer just happens; it’s not your fault.
Many head and neck patients will experience visible changes, but appearance isn’t the most important part of who you are. If anyone judges you for it, they’re not your people.
Head and neck cancer isn’t well-known, even among doctors. I had nosebleeds for four years and never suspected cancer; neither did anyone treating me. Appearance changes make patients more likely to hide, and there’s a gap in awareness, both socially and medically.
Support groups were hard to find, especially UK-based. Americans share resources not available in the NHS system, but the Head and Neck Cancer UK group was helpful. After treatment, I found a dog bite support group for facial reconstruction, too.
Sharing my story is my way of helping others feel less isolated.

Inspired by Vikki's story?
Share your story, too!
More Head and Neck Cancer Stories
Vikki F., Head and Neck Cancer (Nasal Squamous Cell Carcinoma)
Symptoms: Nosebleeds that persisted for years, nose changed in shape, nasal pain, migraines
Treatments: Surgeries (subtotal rhinectomy, reconstruction surgery including radial forearm free flap, bone grafts, and cartilage), chemoradiation
...
Alyssa N., Adenoid Cystic Carcinoma
Symptoms: Persistent jaw pain, lightning-like facial pain during the first bite of meals
Treatments: Surgery (tumor removal), radiation
...
Eva G., Oral Cancer, Stage 4
Symptoms: Sore on the tongue, which caused pain during eating and speaking; changes in the color and texture of the tissue where the sore was located
Treatments: Surgery (partial glossectomy, radical neck dissection, reconstruction), radiation
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...
Kandi B., Adenoid Cystic Carcinoma, Stage 3
Symptoms: Fatigue, headaches, depression, occasional feeling of tongue being on fire or inflamed, appearance of tumor on salivary gland on tongue
Treatment: Surgery
...