Gratitude, Meditation, and Support Carried Antoinette Through Gastric MALT Lymphoma
Antoinette’s story with gastric MALT lymphoma is a powerful reminder that listening to your body can make all the difference. For years, she experienced severe night sweats, unexplained bloating, and persistent gastrointestinal discomfort. Despite living an active lifestyle and maintaining a clean diet, nothing seemed to explain her symptoms. Doctors suggested she was just a “hot sleeper.” But Antoinette kept seeking answers.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Eventually, a colonoscopy revealed the shocking diagnosis: gastric MALT lymphoma, a rare form of non-Hodgkin lymphoma. She felt numb, overwhelmed, and worried about how to share the news with her family, especially since her father was in the last stages of his own cancer experience. The emotional toll was heavy, and the reality of facing a rare cancer came with anxiety, isolation, and what she now recognises as survivor’s guilt.

Antoinette’s medical team offered options, and while initial discussions left her discouraged, more testing confirmed her cancer was at stage 1E. Radiation therapy became her path forward. The treatment was far from easy, bringing side effects like intense abdominal pain and physical exhaustion. She leaned on her “treatment tribe,” a supportive circle of friends, family, and even acquaintances who stepped in with meals, rides, and encouragement. Moments of gratitude and daily prayer gave her strength, and meditation helped her breathe and get through radiation sessions.
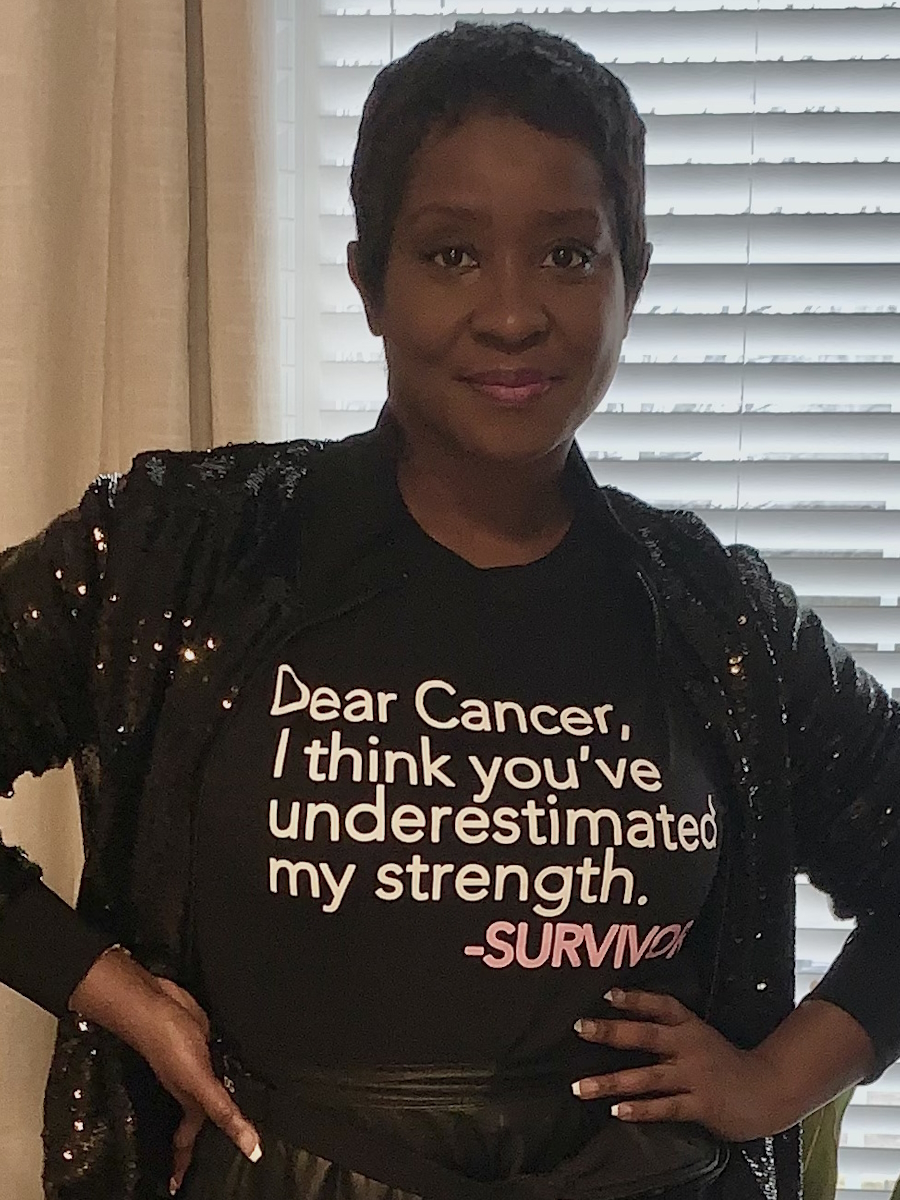
Two years after her gastric MALT lymphoma diagnosis, Antoinette reflects on the mental and emotional impact of living with a rare cancer. She highlights the unseen struggles: depression, anxiety over test results, and the sense of being alone despite having support. She’s learned to advocate fiercely for herself, trust her instincts, and build a life centered on joy and purpose. Through starting a nonprofit and creating empowering merchandise like “Cancer Conqueror,” she now channels her experience into something uplifting and inclusive for other women, particularly those who face disparities in healthcare.
Antoinette wants to remind us that living well isn’t about waiting for happiness. It’s about designing a life that feeds the soul. She encourages others to stay active, eat well, listen to their bodies, and partner with their healthcare teams with mutual respect.
Watch Antoinette’s video and browse her interview transcript to take a deep dive into:
- How she knew her body was telling her something, even when tests didn’t
- Why the unseen mental health side of many cancers is as real as the treatments themselves
- From night sweats to diagnosis: the path to finally being heard
- Why Antoinette calls herself a ‘Cancer Conqueror’ and not a fighter
- Name: Antoinette N.
- Diagnosis:
- Gastric MALT Lymphoma
- Staging:
- Stage 1E
- Symptoms:
- Gastrointestinal issues that didn’t make sense due to her healthy diet and lifestyle
- Significant night sweats
- Unexplained bloating
- Treatment:
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- I am Antoinette
- How I knew something was wrong
- The testing I was doing
- The moment everything changed
- My dad and I both had cancer at the same time
- What the doctors were telling me
- How my body handled radiation
- How I got through the hard days
- I had an amazing support team
- How I’ve navigated my diagnosis
- Some of my symptoms came back
- I had to advocate for myself
- How cancer has changed me
- What I want others to know
I am Antoinette
I was diagnosed with gastric MALT lymphoma.
How I knew something was wrong
One of the symptoms I was experiencing was significant night sweats, to the point where I said to my gynecologist, “Hey, I don’t think I’m there yet, but could I maybe be there? Am I peri- or pre-menopause?” The sweating went on for some years, actually. The gynecologist said, “Oh, maybe you’re just a hot sleeper.” I got a cooling mattress, which was wildly expensive. I got cooling sheets, I got all these other things, too. We did all these tests and couldn’t find anything wrong. I was having gastrointestinal symptoms that didn’t make any sense. Even during the years that I spent being a vegetarian, I experienced severe bloating despite being physically active. I work out quite a bit. I wasn’t able to eliminate the way that you should when you eat clean. I don’t eat pork. I hardly eat fried food. Drive-thrus are few and far between. So I have a pretty clean diet, which is why the gastrointestinal symptoms weren’t making sense. And then after I did manage to eliminate, I would look like I’m five months pregnant.
I cut out different things in my diet. I replaced white sugar with coconut sugar, which has a low glycemic index. I tried all these to see if it was a lifestyle issue or if I just had gut sensitivity.
None of it was making sense. And again, this all went on for years.
The testing I was doing
Finally, I went to the gastroenterologist and I said, “Look, something’s wrong.” We did a five-day, six-marker test. At the end of the test, at the end of the five days, I still had three markers left.
I went back for a follow-up appointment. I went, “Well, why would I have three markers left?” And she said, “Oh, some people just have a slow-moving colon.” I went, “No, the researcher in me says no. Everything has a root cause. Why would I have a slow-moving colon despite not having any lifestyle issues? I don’t have any dieting issues. There has to be a reasonable explanation.”
We were scheduled to do a SIBO test. The kit arrived. She said, “Well, we can do a colonoscopy, too.” And I said, “What will the colonoscopy show you?” She said, “Oh, it shows us everything.”
The moment everything changed
I called my family doctor and said, “Listen, I had a colonoscopy back in, I think on December 22nd or 20th, and it’s now January, it’s weeks later. Will you please help me get my results?” They were saying that Hopkins is not returning their phone calls, which I just didn’t believe.
I’ll never forget the street I was driving on. The doctor called. I answered, and she found out I was driving and said she’d call me back. I said, “Nope, what do you have? Just tell me whatever you need to tell me.” So she said, “What has your gastroenterologist told you?” “I said, “Nothing. That’s why I had to ask you to help me because you’re a part of the Hopkins network.”
She then said, “Well, I’m going to tell you because you asked me to, I won’t dance around it. Unfortunately, you have a form of lymphoma called gastric MALT lymphoma. I’ve never heard of it myself, I’m going to be honest with you. I went on our intranet to research it.” She told me what the MALT acronym stands for. She added, “I am not in a position to discuss it with you because that’s not my expertise, and I don’t want to misspeak. But I’ve already put in the referral with oncology. They’ll reach out to you today or tomorrow. Antoinette, I’m just so sorry.”
I was numb. I remember getting home, and I sat in the car for a little bit. I couldn’t move. I just sat in the car. I was able to finally grab my briefcase, my purse, and my keys, get into the house, and just sit on the floor.
Then thoughts of my kids started flooding into my mind. I thought, “Oh my God, how am I going to tell my parents this? How am I going to tell my family?” I was just numb.
I don’t think anyone thought it was cancer. I certainly didn’t think so. I had no idea what was wrong, but I certainly didn’t think the colonoscopy would come back with that diagnosis. I didn’t just have cancer, I had a rare form of cancer. I wouldn’t have thought that.
My dad and I both had cancer at the same time
Unfortunately, we had been informed just two weeks before my diagnosis that my father only had two weeks left to live due to cancer.
I was diagnosed on January 31st, and my father passed on March 7th. So my father fought hard for 18 months after he was diagnosed.
I was the one who was something of a pillar of strength to carry my father through his treatment and his battle. I would drive him three hours away to all his appointments, and so on. So, as we were preparing to bury my father, it was quite something to hear that I had cancer too.
What the doctors were telling me
When I went to see a medical oncologist, he was using the verbiage of “We can watch it, we can monitor it,” and so on. And I was like, “I don’t understand, why would we just watch and monitor it. And he said, “It’s up to you to decide whether or not you want to treat it.” I said, “Why would I not want to treat it?”
And that’s when he mentioned, “This type of cancer has no cure; you can only treat it.” And I remember looking at him and looking at the resident and saying, “Well, this was a waste of my time, because if I’m here talking to you today about just treating it and not curing it, I’m not real sure,” so I left that appointment frustrated and defeated.
That same medical oncologist called me up and said, “We got all the results back. I wanted to ask you if you want to go ahead and do oncology. It looks like your staging is 1E. If you want to go ahead and get rid of it, we can get you scheduled for the radiation and get rid of it.” I said, “Wait, what did you just say?” Because I left that last appointment with him when I was clear that this cancer can’t be cured, it can only be treated.
He said, “Yeah, if you want to do the radiation, we’re confident that 12 rounds of radiation should get rid of it. We did say it was incurable initially, but with it being 1E, we can do the radiation and get rid of it. Maybe you want to think about it, because I know how you feel.” And I said, “Well, yeah, give me the day to think about it.” We also talked about options if I decided not to treat it. What would happen if I let it get to stage 2 or 3, or, God forbid, 4? And he explained that if it got to 2 or even at 1, it started to metastasize, then my only option would be chemoimmunotherapy.
How my body handled radiation
It was awful, actually. I was scheduled to do 12 rounds. Two units per session. I had to go every day, and after the third session, I was just having significant abdominal pain, and I’ve had two children. When I tell you the pain was like giving birth, it was awful. I went ahead and went to the fourth session, because it’s radiation. I wasn’t expecting it to be a walk in the park, but finally, by day four, I said something.
I was like, “Hey, I’ve been in a lot of pain, and just overall, I don’t feel well.” I didn’t look good. I didn’t feel good. The oncologist called, and he’s like, “Hey, you’ve been having stomach pain?” I was like, “It’s more than stomach pain, it feels like.” He’s like, “Let’s take a break for a couple of days. Don’t come Friday, don’t come Monday, let’s take a break. Maybe your body is just trying to adjust to it. Let’s reconvene on Tuesday.”
So on Tuesday, I was feeling better. The pain had gone away. We were able to do the sessions again. He said as well, “I’ll reduce the dosage from 2 to 1 and a half.”
I was supposed to have 24 units total. I think we got to about 16.5. I said, “Well, what’s the probability of that being enough?” And he said, “There’s been enough studies to show that with other MALT lymphomas, people can even have single-digit treatments, and they’ve been sufficient. There’s just not enough research to support a single-digit number of treatments for gastric MALT lymphoma. But I’m sure that the research will come and will say that we didn’t actually need to do 12 treatments with you; we probably could have done 4 or 5.” And I trusted him.
Nothing’s guaranteed. But when he felt confident that the 16.5 was sufficient and that he was more concerned about what my life would look like afterward, that made me feel that much more secure.
The treatment was bad, but I was humbled that it could have been worse and that a lot of people have it worse. And that some, like my dad, don’t make it. So I’m really, really grateful that the 16.5 units was sufficient. I’m grateful that I’ve had a great medical team. That’s one of the things that I did during this entire journey.
How I got through the hard days
I recite gratitude every day, of course, I pray every day, and I pray a lot. I know sometimes God might be like, “You again.” But gratitude is what helped keep me sane during this entire ordeal. The machine that I had to use. There’s a series of appointments as well, leading up to the radiation, because you have to hold your breath while you get the treatment, while the machine is going around your body. And they literally stop your breathing, like you can’t breathe if you wanted to. And I remember one of the technicians came out. He said, “You have really long breath strides, some of the longest we’ve seen. And I was like, “Perhaps that’s the meditation.” I meditate every day.
I was so happy when I got back to ring the bell. My treatment team was there, and I was able to see them, and when they cried, I cried. We were in the hallway. Everybody was crying, and people were walking by. It was a mess, but a good mess, a good, positive mess.
I had an amazing support team
What I recently found for myself was survivor’s guilt, survivor’s remorse. And that’s something I’m dealing with. But again, I just stay in gratitude with that, and I use that as my power and as my armor to do things like this, to spread the awareness. I’m starting a nonprofit foundation for black women with cancer. Of course, it’s open to all women, but in particular, those who have a more disparate impact.
I’ve also started a line of merchandise because one of the things that I started to say to myself during this journey was that I have to have positive language, and somebody was like, “Oh, you’re fighting cancer,” and I was like, “No, that feels so heavy, that feels so negative. It’s too much for me to carry. I’m conquering cancer. It feels empowered. It feels empowering.” I’ve aligned merchandise for cancer patients that says “Cancer Conqueror.” And then even for the people who were taking me to treatment again, I didn’t want to feel needy, I didn’t want to feel disabled. I was like, “No, you guys are my treatment tribe.” The people who brought me food, the people who sent flowers.
I got so much love from people that I don’t even like. They don’t even have my phone number, but they know me or know of me.
How I’ve navigated my diagnosis
The last two years have been emotionally and mentally tough, like I’m still trying to find my footing. And I think that’s the part of cancer that many people don’t get to see. You see it when patients lose their hair, you see when they’re not feeling well, but you don’t see the depression, you don’t see the anxiety, you don’t see them say, “Oh, gosh, I have a cold, now they want to do another scan.” Yeah, it’s in remission, but maybe not. You don’t see the feelings of isolation. You can have people like I did, a treatment tribe, but you’re really in it alone. It’s you and God. Especially when you have a rare cancer.
Despite my diagnosis, I still went to work every day; that is the only thing I regret. I should have taken that time to take care of myself.
Some of my symptoms came back
We agreed that I would see him once a year. But then the night sweats came back. So he’s like, “I want you to see medical oncology.” And I’m like, “Medical oncology can only do one thing for me, which is chemoimmunotherapy, and I don’t want to do that.” But again I said, “But I trust you, so if you feel like you want me to go back to see medical oncology, I will do that because I trust you and I trust your expertise, you haven’t steered me wrong yet, and so I agreed.”
Those same spots have been there; they haven’t grown in size, they haven’t changed shape. Maybe those are just two areas that will just always be hotspots of some sort in my body. Maybe that’s just my body’s anatomy, because for two years and all these CT scans with contrast, they haven’t changed.
We did a ton of lab work. All the labs were clear.
I had to advocate for myself
So I will see medical oncology in six months, and then six months from there, I’ll see radiation oncology. I’ve accepted, if you will, my fate. I’ve accepted that this is just what it is. But they know I’m not a hypochondriac. How I got here is because I know my body, something’s not right here. I don’t take any supplements, and I’m not on any medication. There was nothing else to point to. Why would I be having these gastrointestinal issues? It’s not a lifestyle issue, it’s not a supplement issue, it’s not a medication issue. There was no other reasonable explanation. And so with that said, they know I’m the first one to advocate for myself, and so if something starts to feel like it’s going awry, I’ll be the first one to say, “Guys, we might have a problem here.”
How cancer has changed me
My immune system now is not as strong. I have never had so many colds over the last two years that I’ve had in my life. But what’s interesting, though, is this conversation I had with both medical oncology and radiation oncology. They both mentioned the same thing — that normally people with radiation, and certainly the low doses that I had, normally don’t experience compromised immune systems during the time of treatment. Maybe, but not two years removed, and I’m like, “Well, I did have a rare cancer, so there you go.
I’m grateful to be a part of any research and information that Hopkins can get and give to the cancer community to help them see increased survivorship.
What I want others to know
Do what brings you joy, not happiness. Happiness is a fleeting emotion. Do what feels good to your soul.
Live your life by design. If you know you have no desire to commute to work every day, then build a business or hire a driver. That can go several different ways. Live your life by design, because by doing that, you’ll have an inherent level of joy. But do what? Do what feels good to your soul. Do what brings you joy. Pay attention to your body. Get healthy. Stay healthy. Because when you get and stay healthy and you stay active and you have a good diet, when you do come across health issues, they’re easier to find and easier to explain.
Advocate for yourself. Ask the hard questions. As I told my oncologist, “You may be a Hopkins oncologist, but this is my life and this is my body, so we’re partners in this.” And that is also why I, as a patient, have to treat him like he’s human, too.
Be nice. Be good to your providers, and I’m fairly confident they’ll be good to you, too. As we like to say in the south, you get more bees with honey than vinegar.

Inspired by Antoinette's story?
Share your story, too!
More Non-Hodgkin Lymphoma Stories
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy