Acute Myeloid Leukemia (AML): Biomarker Testing and a Clinical Trial Gave Joseph Hope
In the summer of 2023, Joseph noticed unusual fatigue and chest pains while coaching mountain biking and participating in a race. A quick ER visit and a CBC confirmed his diagnosis of acute myeloid leukemia (AML).
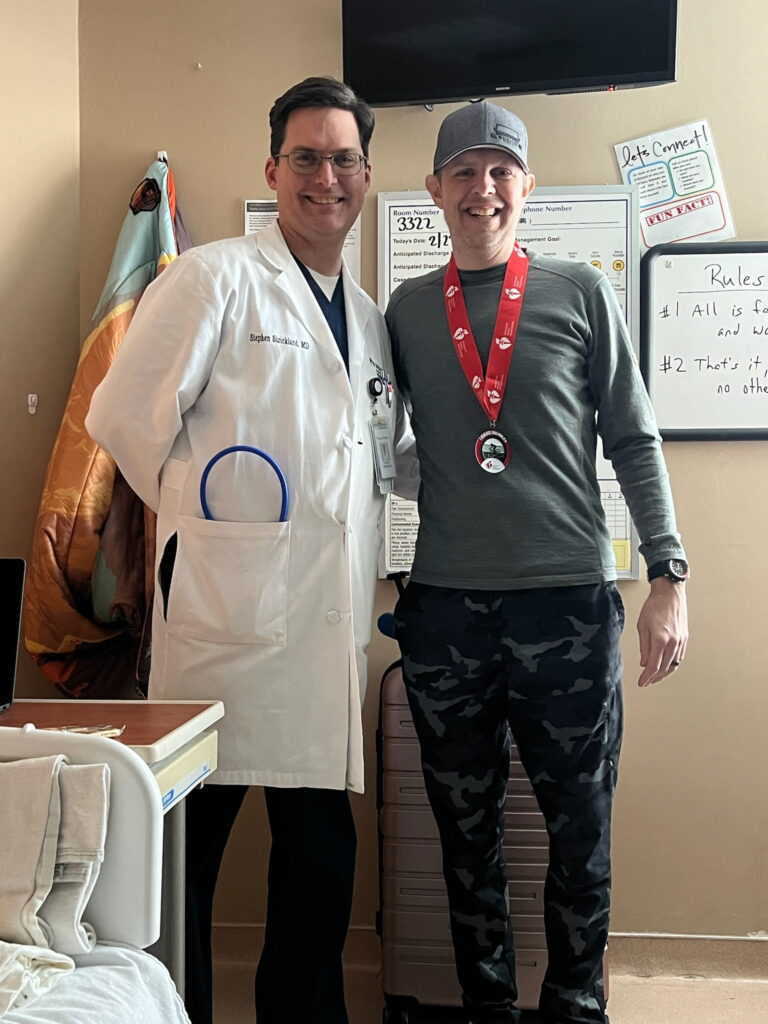
Despite the whirlwind of emotions, biomarker testing, which can include both testing of your own genes as well as the cancer’s genetic changes to personalize care, became a beacon, and it guided his treatment decisions. Joseph’s prior exposure to chemotherapy as a child raised concerns about treatment-related acute myeloid leukemia risks. Dr. Strickland, his dedicated physician, explained the significance of genetic markers, which helped tailor his treatment plan.
Joseph qualified for a clinical trial involving a new menin inhibitor, an advanced treatment for AML, alongside traditional chemotherapy, as part of what Dr. Strickland called “a tank and a sniper” approach. Joseph embraced the clinical trial, as he felt informed and supported rather than the subject of a medical experiment. Dr. Strickland and his team provided personalized and meticulous care, and the constant presence of Joseph’s wife, Heather, bolstered his confidence. He was also happy to undergo regular check-ins, bone marrow biopsies every three months, and adjustments to his medication dosage.

Today, Joseph is thriving again. He’s back to regular long-distance biking, coaches fellow cyclists, travels with his family, and actively engages his community. He urges others with acute myeloid leukemia to trust credible resources, engage with their care team, and find hope in the knowledge that a fulfilling life is possible.
Read Joseph’s story and watch his video:
- Find out how cycling helped him detect his acute myeloid leukemia
- Learn the pivotal role of biomarker testing in Joseph’s AML treatment
- See why he felt truly empowered by his clinical trial
- From diagnosis shock to biking 80 miles — trace Joseph’s path with AML
- Delve into the support system that helped him thrive through his acute myeloid leukemia treatment
- Name:
- Joseph A.
- Diagnosis:
- Acute Myeloid Leukemia (AML)
- Mutation:
- NPM1
- Symptoms:
- Suspicious leg fatigue while cycling
- Chest pains due to blood clot in lung
- Treatments:
- Chemotherapy
- Clinical trial: targeted therapy (menin inhibitor)
- Stem cell transplant

- About Me
- My Symptoms and Acute Myeloid Leukemia Diagnosis
- I Struggled With Anxiety
- Biomarker Testing and How It Narrowed Down Treatment Options
- AML Program Highlight: AML Biomarkers: How Testing Shapes Your Treatment Options
- For the rest of this interview, watch our program replay ON DEMAND.
- I Joined a Clinical Trial
- How the Clinical Trial Impacted Me
- How My Care Partners Influenced My Decisions
- What I Want AML Patients to Know About Testing and Treatment Options
- I Want Acute Myeloid Leukemia Patients to Have Hope
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
I hope acute myeloid leukemia patients can see my story and derive hope from it.
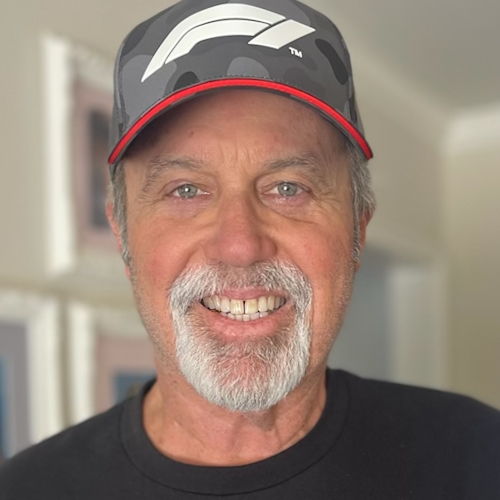
About Me
Hi, my name is Joseph. I’m a doctor, a neurologist. I’m married to my wife, Heather; we have children and a few dogs. I’ve been an avid cyclist for years and especially enjoy mountain biking.
I was diagnosed with acute myeloid leukemia (AML) in the summer of 2023. This wasn’t my first experience with cancer. I had cancer as a child and had chemotherapy to treat it.


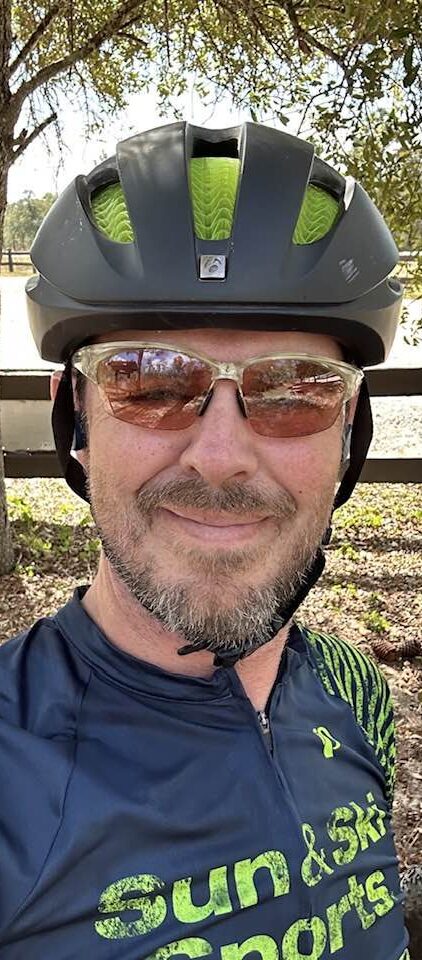
My Symptoms and Acute Myeloid Leukemia Diagnosis
My story started when I was coaching mountain biking, and I noticed that my legs were becoming fatigued very quickly. And when I joined a mountain bike race, I started having chest pains.
I went to the ER to have myself checked out. I had a CBC done. The results showed that I had AML.
I immediately got airlifted to the Sarah Cannon Institute in Nashville and started seeing Dr. Strickland, and everything took off from there.
It’s a wild ride to find out you have acute myeloid leukemia and to realize that you need to make a quick decision regarding treatment options so that you can start treatment rapidly. They aren’t something you can weigh and think about for weeks and months.
So, it was a whirlwind, if you will.
It’s a wild ride to find out you have acute myeloid leukemia and to realize that you need to make a quick decision regarding treatment options so that you can start treatment rapidly.
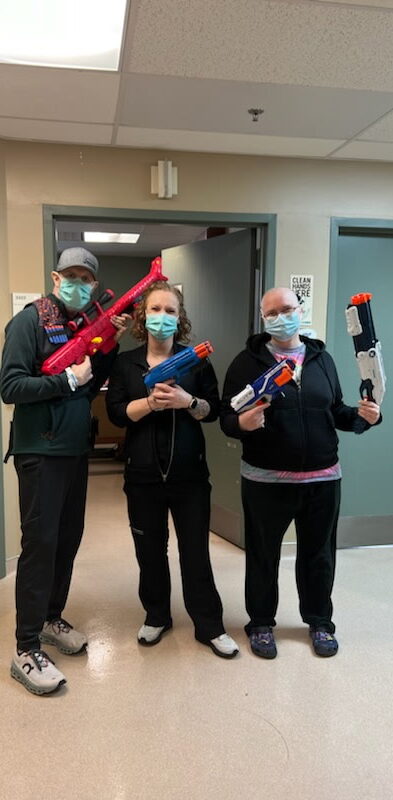
I Struggled With Anxiety
I went from someone healthy, active, and surrounded by people I love, to someone who was in this unfamiliar environment and who needed to be isolated from the world because I was going to be neutropenic in several days.
So it was a very anxious time. But I also found hope in my situation, as we discussed my treatment options.
So after three or four weeks, I was able to get a clearer picture of what the next three to six months of my life looked like. And it was then that I felt like I could settle in and realize the path that was in front of me.


Biomarker Testing and How It Narrowed Down Treatment Options
As I said, I had cancer in my youth and received chemotherapy for it. So there was a concern that my acute myeloid leukemia was related to this treatment. Treatment-related AML tends to carry higher risks.
When I arrived at Sarah Cannon, Dr. Strickland immediately explained that we’d be looking at genetic markers and what that might mean for my treatment. He talked about newer targeted therapies and potential plans depending on the results of the biomarker testing. Aside from that testing, I also underwent a bone marrow biopsy.
We started to get the results after a day or two of the biopsy. Because of my prior exposure to chemo, we opted to undergo a more aggressive initial chemotherapy regimen. And as the final testing came back, I found out that I was one of the lucky patients who might be a candidate for one of the new menin inhibitors that was being tested.
And, so, that was very exciting, this idea that I potentially could — stealing Dr. Strickland’s phrase — start out with a tank and a sniper right from the beginning, start out with both traditional chemo and one of these new menin inhibitors.
From that point onwards, the biomarker testing guided our decisions, such as the treatment course as a whole, whether to try new drugs, and, ultimately, the choice to pursue a stem cell transplant.
My Story Continues Below
AML Program Highlight: AML Biomarkers: How Testing Shapes Your Treatment Options
I sat down with The Patient Story’s patient advocate Steve Buechler and Dr. Strickland to discuss how AML biomarker testing shapes patients’ treatment options. Here are some of the key points of our discussion.

Steve Buechler: Dr. Strickland, what are biomarkers, and what are the different types? We hear about diagnostic, prognostic, predictive, monitoring — it sounds pretty complicated. Can you sort it out for us?

Dr. Stephen Strickland, MD: Historically, AML was diagnosed simply by looking at cells under a microscope. And we know now that those cells can look similar under the microscope, but the biology of AML is very heterogeneous. Looking at these biomarkers helps us understand the true diversity of the disease and helps us predict both prognosis and therapeutic options.
A lot of different biomarkers have been developed over the years. We now have a broader spectrum of testing that we do as standard of care at the time of diagnosis to guide our treatment decision-making.
Steve Buechler: For AML in particular, what biomarkers do you commonly test for?

Dr. Strickland: That’s a great question. There are different types of biomarkers, and what we’re really looking at is the biology of the leukemia cell. One major category we look at is cytogenetics — also called a karyotype — which is a chromosome analysis of the leukemia cells. These genetic changes can help us classify patients into favorable, intermediate, or high-risk categories. That classification can influence which therapies we consider, including whether to pursue a clinical trial from the beginning or look ahead to stem cell transplant if the patient achieves remission.
Historically, we’ve had cytogenetics for decades, but more recently, we’ve added molecular profiling using PCR-based tests, single-gene assays, and next-generation sequencing (NGS). These NGS panels can screen for anywhere from 35 to 200 mutations, giving us a vast amount of information.
Some mutations have become standard to test at diagnosis. For example:
- FLT3: Patients with FLT3-ITD mutations tend to have higher-risk disease, although the development of FLT3 inhibitors has improved outcomes.
- IDH1 and IDH2: These mutations have treatments now, historically used in the relapse/refractory setting, but data is emerging on using them in frontline therapy.
- NPM1: Initially important as a prognostic factor, it’s now also being considered as a therapeutic target, especially with new menin inhibitors.
We’ve seen exciting recent developments, including the approval of revumenib—the first therapy for patients with KMT2A-rearranged relapsed/refractory AML. This is being studied in combination with other therapies even in the frontline setting.

At the ASH 2024 annual meeting, data was presented on menin inhibitors like bleximenib and ziftomenib. Both showed promising results when combined with intensive induction chemotherapy, including high complete remission (CR) rates and MRD-negative CRs—which means deep remissions we can verify through molecular testing.
Importantly, these drugs also showed strong activity in patients with NPM1 mutations and KMT2A rearrangements—two groups that have historically responded poorly to standard chemotherapy. So we’re hopeful that this marks a real breakthrough in treating these harder-to-treat cases.
Steve Buechler: Do any of these biomarkers or mutations tend to cluster in specific groups of people based on age, gender, or other social factors?
Dr. Strickland:There’s a variety of factors that we can see. NPM1 can occur sort of across the age spectrum, if you will. But the other aspect is what mutations or other abnormalities are co-occurring, and that has influence. So NPM1 by itself is thought to be a favorable risk feature. But there’s also data that suggests NPM1 when it co-occurs with, say, an IDH mutation or a DNMT3A mutation, that it’s the positive impact may take a hit based on the co-occurrence of these other mutations. And for instance, when NPM1 co-occurs with a FLT3 mutation, FLT3 by itself puts patients into a high-risk category, so to speak. But FTL3 plus NPM1 puts them in an intermediate risk, whereas NPM1 patients by themselves go into a favorable risk.
So I think it’s really not just any single mutation that’s driving it, but really looking at the bigger picture of the molecular profile and the diversity even within a single patient’s leukemia to try and see what the impact is and open the door for additional therapies. We do know that the KMT2A rearrangement historically has been associated with patients who have seen prior anthracyclines, so part of this therapy-related leukemia that we were talking about earlier, some patients who receive prior anthracyclines will have a KMT2A rearrangement and that confers a higher risk disease. And so the availability of these therapies for a traditionally high risk patient population is going to be very important.
Steve Buechler: That makes sense. When I was treated back in 2016, I was given the standard 7+3 chemotherapy, and they tested only for FLT3 — which I didn’t have — and NPM1, which I also didn’t have. They said that would’ve been good to have. So I had neither and ended up in the intermediate-risk category, especially with a normal karyotype. At the time, I didn’t understand any of this — it’s a lot to take in. But thank you for that explanation. How and when do you test for these biomarkers?

Dr. Strickland: At the time of diagnosis. It’s critical to test early because it helps us understand prognosis and also informs treatment choices. Even if we have to start treatment immediately, we want to get these samples before therapy begins. That way, we have the necessary data to decide whether a stem cell transplant might be needed in first remission or whether a patient might benefit from a targeted therapy. We also retest in some cases during remission to evaluate measurable residual disease (MRD)—meaning whether there’s still any detectable leukemia at a very sensitive level.
Steve Buechler: And is this typically done through a bone marrow biopsy?
Dr. Strickland: Yes, usually at diagnosis, it’s done through a bone marrow biopsy, using the aspirate—the liquid part of the marrow.
But some of the tests can also be done from peripheral blood, especially for monitoring over time. There’s some debate over sensitivity between marrow and blood samples, but doing follow-ups through blood can help reduce how often patients have to undergo marrow biopsies. Those are not the most pleasant thing to repeat frequently.
Steve Buechler: Despite its importance, early biomarker testing still isn’t standard everywhere. Why is that, and what are the barriers?

Dr. Strickland: It’s improving, especially over the last several years, and it’s now recommended in the NCCN guidelines. But access still varies depending on where a patient presents.
If a bone marrow biopsy is done at an outside hospital that doesn’t have access to the full panel of molecular testing, we often have to repeat the biopsy once they arrive at a center like ours.
It’s not ideal, but it’s necessary to make informed treatment decisions.
It really takes a team effort—oncologists, pathologists, hospitals—to advocate for this testing and ensure it becomes routine practice.
Steve Buechler: How do biomarkers play a role in clinical trials? Can they make you either eligible or ineligible for certain trials? How do those two things work together?
Dr. Strickland: Yeah, so, you know, it’s definitely been an evolution in the leukemia research space, the clinical trial space, and I’ll say oncology research in general space, and that, you know, as we mentioned earlier, we’re trying to take advantage of the biological characteristics of one patient’s tumor. And so there are a lot of studies that are being so-called biomarker-driven. And if a patient’s malignancy has a specific marker, then we’re trying to get them access to these targeted therapies or snipers, if you will, that we referenced earlier. And so I think that there are opportunities where, you know, sometimes these drugs may be more effective on a broader scale, but at least with the initial development, we’re also trying to enrich the population of patients who are truly gonna likely, hopefully, have a benefit from the medications. And so it’s just us trying to take advantage of the characteristics we now can better understand about one person’s leukemia. Characteristics that we didn’t know existed, say, you know, 30, 40 years ago, but now we have the technology to help us identify this and identify it relatively quickly, and that can be instrumental in guiding us to either commercially available therapies or for clinical trial participation, where there may not be something that’s already FDA approved to target that.
Steve Buechler: So how does knowing someone’s biomarkers impact their treatment choices? And that includes, do biomarkers give you some idea about potential side effects or potential effectiveness of treatments?

Dr. Strickland: The biomarkers can definitely help to guide the decisions on therapy. Not so much from a side effect profile, but more so from an efficacy perspective. You know, the way that I think about our traditional therapies are kind of like going to battle with a tank. Tanks can be very effective, but they’re not very specific. And so some of these newer therapies, these targeted therapies like FLT3 inhibitors, menin inhibitors, IDH inhibitors — all of these therapies are kind of like adding a sniper to the mix. And hopefully by going to battle with maybe both tanks and snipers, if you will, hopefully we can have a more effective outcome in the battle against this malignancy.

For the rest of this interview, watch our program replay ON DEMAND.
Back to My Story
I Joined a Clinical Trial
On day one, Dr. Strickland and I discussed the whirlwind of the acute myeloid leukemia diagnosis and how we could try to navigate and come to terms with it. I felt like I was in such shock that I would be happy to try anything. We also talked about clinical trials and some of the possibilities we could explore, even before we knew what my mutations were.
Unlike in a traditional cancer course where you see a surgeon and an oncologist and then choose your treatment a couple of weeks later, to me, there was such urgency that to hear that I had options, both in the traditional sense and a trial, gave me comfort. As did the fact that they were going to run in parallel and take place simultaneously.
Multiple staff members came up to me and explained the trial, and I thought they did a great job doing so. A representative from the pharmacy also came up and talked about potential side effects and impacts. Thanks to their input and to the fact that they were practically sitting beside me and explaining everything, I found it easy to navigate the forms.
In no way, shape, or form did I feel like I was being experimented on or anything of that sort.
I felt very comfortable with the trial, and I’ve grown to love it as I’ve participated in it.
How the Clinical Trial Impacted Me
In no way, shape, or form did I feel like I was being experimented on or anything of that sort. I felt very comfortable with the trial, and I’ve grown to love it as I’ve participated in it.
There are, of course, some impacts of the trial; a lot of checkboxes, if you will, including some impact on my quality of life later on. I’ve probably gotten to see Dr. Strickland’s staff a bit more often than the average AML patient who’s in remission.
I also loved the way they presented the trial to me at the outset. They said, “Here’s a medicine, we know it works — refractory patients have had good experiences with it. Our question regarding your trial is simply — if we give it to you at the very beginning, do you go into remission quicker?”
They knew that the medicine they were giving me was effective, and they were going to see just how effective it would be for me if they transitioned it up in my treatment. I found a lot of comfort in that.
I get to have a bone marrow biopsy every three months, which is probably not on everybody’s bucket list, but I feel that it’s a small price to pay.
As far as side effects go, I’ve been pleasantly surprised. I feel like I’ve had minimal side effects with this drug. We’ve tried increasing the dose of the drug during the trial, but I didn’t tolerate that very well, and so Dr. Strickland, his team, and the company that runs the trial brought the dose down to the level I had been tolerating. Aside from that, I can say that my experience with this trial has so far been phenomenal.
How My Care Partners Influenced My Decisions
I’m happy that my wife, family, and network have really supported me through my acute myeloid leukemia experience.
My wife, Heather, is an office manager for a medical group, and they got together and told her that she could stay with me and work remotely so she wouldn’t have to leave my side. That was phenomenal and really freed me up and helped me make the tough decisions.
In addition to that, since I’m a physician as well, I had access to other doctors I could call and ask about certain things I wanted more clarity on.
But I felt comfortable with Dr. Strickland. When he entered the room the very first time, he laid it all out and there was nothing left on the table. And as more information came back, I felt he would immediately update me about it and how it would affect my options.
So Heather and I feel that we had all the information we needed to make the best decisions for my care.
I’m happy that my wife, family, and network have really supported me through my acute myeloid leukemia experience.

What I Want AML Patients to Know About Testing and Treatment Options
The best advice I can give a patient who’s just been diagnosed with acute myeloid leukemia is to access great resources. In my neurology practice, patients look up their disease or condition on Google, and they come in with all this preconceived bad information. And that’s so very scary.
But there are great websites out there, as well as professionals who can offer good information. And when I was first starting and heading into this dark time with a lot of confusion, I promised my wife that we weren’t just going to head out on the internet and read up on a bunch of iffy resources.
We were instead going to trust Dr. Strickland and his team and protocols. We were going to focus on the resources he and his team would provide.
I feel like patients would be better served by starting there, versus the huge cloud of misinformation the global internet can be.
I Want Acute Myeloid Leukemia Patients to Have Hope
Where I’m at today is somewhere that I would have loved to have known I would end up during my first month of diagnosis.
I’ve gotten back to biking — I just rode 80 miles last week, and I’m going to do it again this week. I’m an active member of my church. I coach the local mountain bike team. I travel with my family and our dogs; we love going all around the nation and seeing the sights.
I wish I could have known that was possible right out of the gate. And if I had seen an AML survivor doing this well when I was about to have treatment, it would have given me a lot of hope.
I hope acute myeloid leukemia patients can see my story and derive hope from it.

Where I’m at today is somewhere that I would have loved to have known I would end up during my first month of diagnosis.


Inspired by Joseph's story?
Share your story, too!
More Acute Myeloid Leukemia (AML) Stories
Russ D., Acute Myelomonocytic Leukemia (AMML), with NPM1 Mutation
Symptoms:Flu‑like symptoms, profound fatigue, blood pressure drop, shortness of breath
Treatments:Chemotherapy, clinical trial (menin inhibitor)
Shelley G., Acute Myeloid Leukemia (AML) with NPM1 Mutation
Symptoms: Fatigue, rapid heartbeat, shortness of breath, low blood counts
Treatments: Chemotherapy, clinical trial, stem cell transplant
Joseph A., Acute Myeloid Leukemia (AML)
Symptoms: Suspicious leg fatigue while cycling, chest pains due to blood clot in lung
Treatments: Chemotherapy, clinical trial (targeted therapy, menin inhibitor), stem cell transplant
Mackenzie P., Acute Myeloid Leukemia (AML)
Symptoms: Shortness of breath, passing out, getting sick easily, bleeding and bruising quickly
Treatments: Chemotherapy (induction and maintenance chemotherapy), stem cell transplant, clinical trials