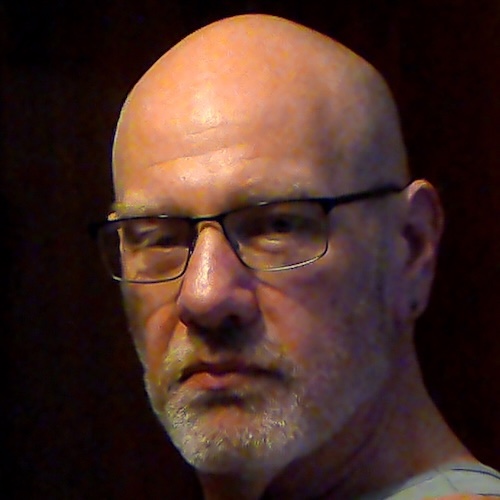
Bladder Cancer Changed Me — But It Didn’t Break Me: Danny’s Story
Danny dealt with non-muscle invasive bladder cancer head-on in 2023, a diagnosis that shook his world but also transformed his outlook. As he approached 50, he anticipated typical signs of aging — but was unprepared for the persistent back pain and relentless vomiting that led him to the ER. A CT scan revealed something suspicious, prompting a referral to a urologist who confirmed Danny’s worst fears: it was bladder cancer.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
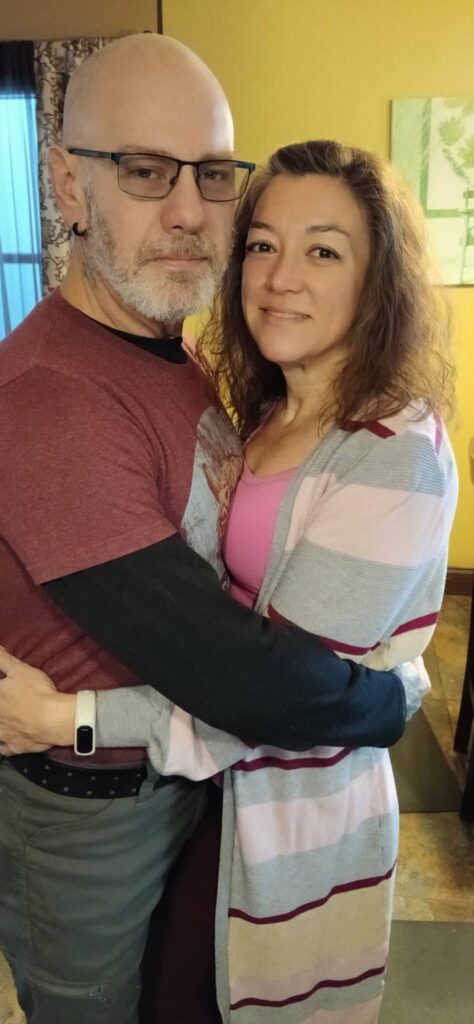
Navigating this life-altering news, Danny grappled with deep emotional turmoil, recalling the swift loss of his father to colon cancer. The shadow of that grief made his diagnosis even heavier. But Danny didn’t submit to his fear. He instead channelled his energy into self-advocacy, becoming his own most vocal health champion. His wife’s unwavering support was pivotal. She signed him up for the Walk to End Bladder Cancer, which reignited his spirit and helped him connect to a community that understood his struggle.
Undergoing transurethral resection of bladder tumor (TURBT) surgery, chemotherapy, and immunotherapy, Danny learned the critical importance of proactive health management and open dialogue about topics often shrouded in stigma, like bladder health and erectile dysfunction. His candidness regarding bladder cancer breaks barriers, encouraging others to seek support and speak openly.
Today, Danny’s focus is on preserving his health, nurturing resilience, and empowering others through his story. He wants others to know that self-advocacy, support, and staying informed are powerful tools in reclaiming health and happiness.
Watch Danny’s video and read the story for more about:
- How his ER visit revealed more than he expected.
- The pivotal moment that reignited Danny’s will to live.
- What he wishes he knew before his bladder cancer diagnosis.
- The role of self-advocacy in Danny’s recovery journey.
- Breaking the stigma: his open talk about bladder cancer.
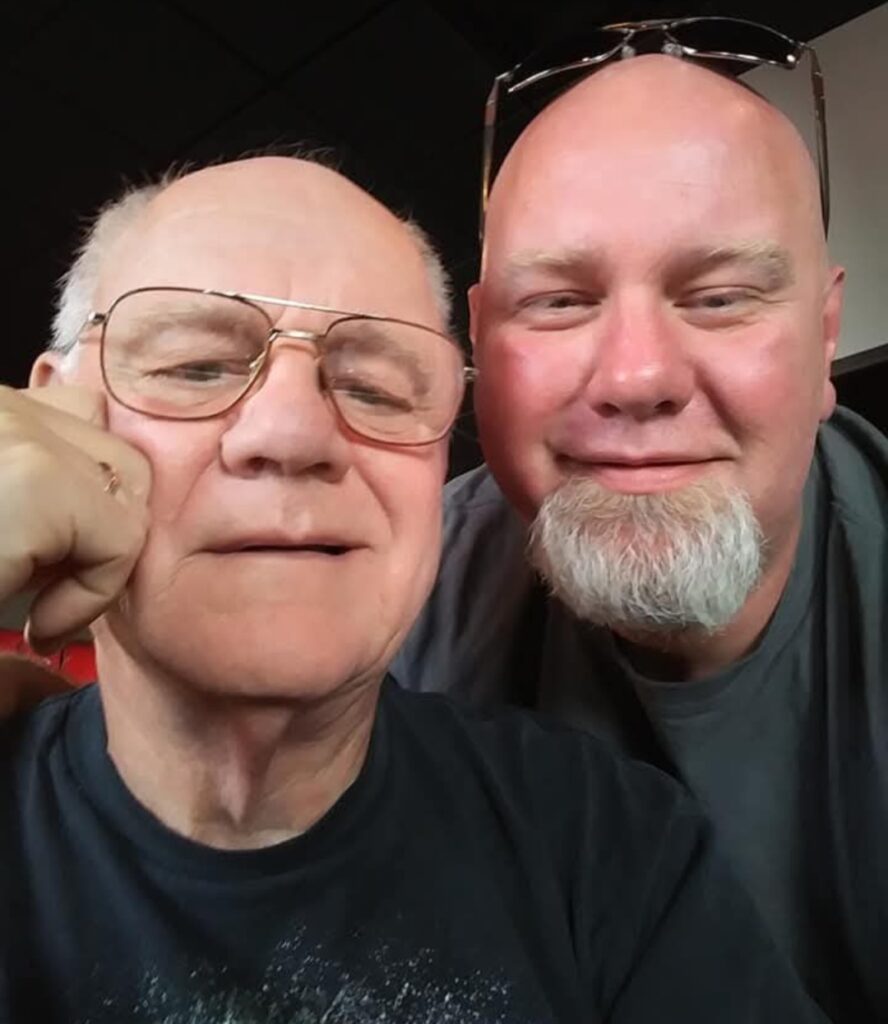
- Name:
- Danny G.
- Age at Diagnosis:
- 48
- Diagnosis:
- Non-Muscle Invasive Bladder Cancer
- Symptoms:
- Fatigue
- Back pain
- Erectile dysfunction
- Nausea
- Treatments:
- Surgery: transurethral resection of bladder tumor (TURBT)
- Chemotherapy
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
My message of hope to people who experience bladder cancer or other similar conditions is to keep your feet on the ground. Find a direction to head. Grab on to that care partner.
About Me
Hi, I’m Danny. I’m 49 years old.
I survived non-muscle invasive bladder cancer in 2023.


The Run-Up to My Bladder Cancer Diagnosis
Approaching age 50, I was ready for things like an enlarged prostate, trouble urinating, and back pain. All of these things add up to what you hear about closing in on that age.
One of the biggest changes that I started experiencing was erectile dysfunction. I didn’t know this until afterwards, but with a diagnosis such as bladder cancer, eventually, you realize that it affects everything down there. And it’s not just sexual problems. I had no idea that bladder pain could affect the back and the hips.
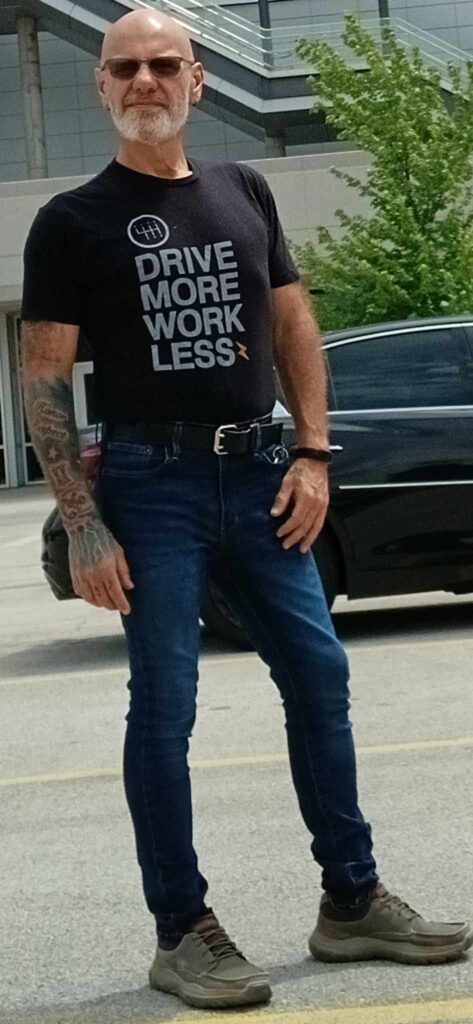
I used to be an alcoholic, and I was really out of shape, too. I used to weigh over 300 pounds. Earlier in 2023, I had quit drinking, and I started to get into shape. But when my figure had improved and I started losing weight, that’s when things started to happen.
Occasionally, I’d have a really upset stomach in the morning. But things got worse. In July 2023, I started vomiting and kept on vomiting for 12 hours. It took me a while, but I finally managed to drag myself to the ER.
The attending physician said, “I’d like to give you a CT scan to make sure you haven’t ruptured anything.” It didn’t find any internal bleeding. But when the report came back from that CT scan, after I’d already gotten out of the hospital, they told me I needed to go to a urologist.
Then things turned into a bit of a fever pitch, and I started worrying that I had cancer. I went to my urologist. He was pretty pragmatic and straightforward. He said, “I’m almost 100% sure you do have cancer. We have to do a scope, a cystoscopy, to make 100% sure it is cancer, and then we’re going to take it out.”
I remember another part of that visit very distinctly. Before seeing the doctor, I was in the waiting area. I was with a gentleman who might also have been in a similar situation. He had unfortunately missed his appointment. They told him that he was going to have to wait a month for the next slot.
This still just chokes me up, because when I was sitting there and didn’t know if I had cancer yet, I remember considering giving this guy my appointment. I decided against it, but it would have been a pivotal decision.
Trying to overcome the information gap and deal with crucial information revealing itself became important to me. I thought, I’m scared to death, but here we go. I was just on a hunt from then on out. Just information gathering.
I went to my urologist… He said, “I’m almost 100% sure you do have cancer. We have to do a scope, a cystoscopy, to make sure it is cancer, and then we’re going to take it out.”
My Biopsy and Waiting for the Results
I went in for my procedures. At the time, I had no idea what a cystoscopy was, but I’ve already undergone ten of them now.
Afterwards, I was waiting for the results of the biopsy. I took the time to thoroughly read the notes from the doctor. One thing I read made me go and see him. The doctor had put this in his notes: “Pleural nodule found during CT scan in left lung.” He’d even added, “Highly concerning.” I asked him, “Am I going to live or die?”
You see, my father died of stage 4 colon cancer in 2020. He died only a month and a half after his diagnosis, because he just let go. I was his caregiver. And, I thought, “Now I’m the patient.”
I’d watched my father die, and I buried him. When I found out I was very likely to have cancer, I was convinced I was going to die, too. So I started giving away my stuff and telling my wife to be prepared.
Every time someone brings those topics up, it just hits me right in the stomach. I’m still so emotional about it, even after all this time.
My Diagnosis, How I Took It, and How My Wife Helped Me
They finally told me that I had non-muscle invasive bladder cancer. I had a grape-sized tumor, one over my ureter from my left kidney. Luckily, later, I found out that the tumor was confined to the bladder and not the ureter.
My diagnosis hit me hard. I felt completely sucked of all energy. I felt lost and confused. I sank into depression and anxiety, and didn’t even realize it.
I spent the next six months in bed, pretty much just waiting to die.
But my wife pulled me out of it. She came into my room one day and said, “I’ve signed you up for the Walk to End Bladder Cancer in Columbus.”
That was the moment things started to change for the better. It was as if I had stepped on the edge of a pit, and I had started to dig myself out. I had been so sick the whole time during my surgery, and I felt like I had put a foot out on the path to recovery.
I ended up going to Columbus and participating in that walk. And I also started to bring that community in.
I appreciate my wife and how she cares for me. But there’s more. To this day, she’s my inspiration. She runs marathons now — when I look at her, it gives me the strength to move on.

My diagnosis hit me hard. I felt completely sucked of all energy. I felt lost and confused. I sank into depression and anxiety, and didn’t even realize it.

My Treatment Plan
When the pathology came back, I underwent TURBT. The surgeon removed the tumor using instruments and a thin tube or scope that entered my body through my urethra.
I had to have a stent placed from my kidney to my bladder because it was over the ureter, and the hole would close up. I had that stent in for a solid eight weeks before it was removed.
That removal was my second procedure, during which they put me under and pulled out the stent. I woke up for the second time with a bladder full of chemotherapy.
My nurse would administer six induction doses into my bladder via a catheter. I would then head home, lie down, and lie on each side for about an hour and 15 minutes each, to make sure that my bladder was coated with the medicine.
Part and parcel of the process was having to deal with my emotions. I would be going through my life like I didn’t have cancer, and then I would get anxious and depressed a week before each induction dose. I would be thinking, “Oh my God, I’ll be getting a catheter again next week.” Then I would get sick. It was quite daunting.
Preserving My Bladder
My bladder is definitely the most important thing in this equation. And so I need to keep it healthy. Although it didn’t occur to me right away, I was still able to find this out early enough.
There was no talk of having my bladder removed. I’ve said that my doctor was pragmatic. That’s a good thing, I’ve found. He won’t say anything unless it’s absolutely necessary, and he hasn’t brought bladder removal up at all.
I know the disease hasn’t progressed enough to become muscle invasive that quickly, because we’ve checked it so often. Additionally, extracting the bladder can bring about issues all of its own.

My bladder is definitely the most important thing in this equation.
And so I need to keep it healthy.

I’m Breaking the Stigma Around Bladder Cancer
People are naturally modest when it comes to talking about the bladder and, let’s just say, the areas around it. But we do need to talk about these things. People need to be informed.
I’m open about my experience because I want to help others. For instance, I’m frank about erectile dysfunction. It’s a natural human male thing that we have to deal with in different ways.
I thankfully no longer experience sexual dysfunction. Of course, it’s very worrisome for a man. My father went through it, and he openly admitted to me that it was quite difficult for him.
My health was a concern when it came to that issue, too. I know that it was due to the bladder cancer itself, but it was also a function of comorbidity, age.
It’s thanks to medicine, self-advocacy, proactive learning, and education that I can specifically tell you where I don’t have problems any longer.
Self-Advocacy Really Matters
Now, self-advocacy is essential. If I could give anyone just one piece of advice, it would be — don’t give up, take that first step, and make yourself vulnerable to everything that’s going to happen to you.
You need those partners and those people who will advocate for you — your friends and family. But that said, the buck stops with you. You’re going to be scared to death, but you’re on your own for a minute. You’re going to have to dig and do your own research, your own advocacy.
My situation was a stark reminder to me that life has no guarantees. I was going to be on my own. And in the two years since my diagnosis, it remains true.
It’s such a funny paradox. I have so many people in my network who are both willing and able to help me. But I sometimes feel apart from that group. So my self-advocacy kicks in, and it gives me strength.

If I could give anyone some advice, it would be — don’t give up, take that first step, and make yourself vulnerable to everything that’s going to happen to you.

What I Want People to Know
My message of hope to people who experience bladder cancer or other similar conditions is to keep your feet on the ground. Find a direction to head. Grab on to that care partner.
You’re going to have to go forward. You’re going to need to be strong. You’ll have to pick up things along the way. I tell you, by the time you reach the two-year mark, your life is going to change.
I’m living proof of that. My entire life has changed.
If you spoke to anybody who knew me before I got bladder cancer and who knows me now, they’ll agree. I’m a completely different person, both physically and mentally. I’ve got a different personality now.
I love people and can’t wait to get up in the morning. I can’t wait to help the people who need help.
I try to help at least one person per day if I can. That’s my rule.

Inspired by Danny's story?
Share your story, too!
More Bladder Cancer Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy