Overcoming Racial Barriers in Clinical Trials from a Lung Cancer Oncologist
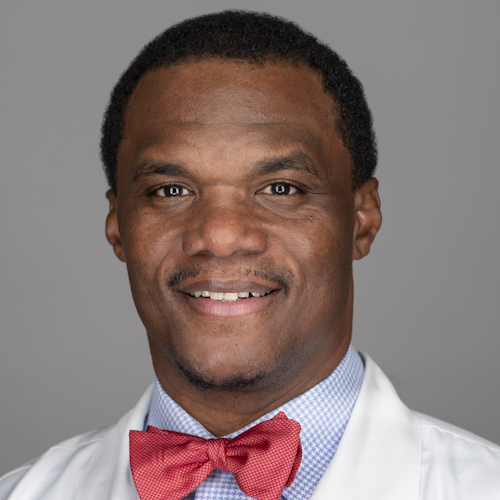
Marjory Charlot, MD, MPH, MSc, is a medical oncologist and health services researcher at UNC Lineberger Comprehensive Cancer Center. She primarily specializes in people who have lung cancer. Her research focuses on increasing awareness and access to clinical trials among Black communities and communities with low-income or persistent poverty.
Interviewed by: Nikki Murphy
Edited by: Katrina Villareal



Thank you to AbbVie, Genmab, and Karyopharm for their support of our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Introduction
- A Winding Path to Medicine
- Why Oncology Became Her Calling
- Growing Up in Mattapan
- Developing the CREATE Initiative
- Most Common Lung Cancer Symptoms
- Demystifying Clinical Trials
- A Patient’s Clinical Trial Success Story
- Overcoming Barriers in Black Communities
- The Role of Black Physicians in Healthcare
Introduction
Nikki Murphy: Tell us about yourself.
Dr. Marjory Charlot: I’m a medical oncologist and health services researcher. I work at UNC Lineberger Comprehensive Cancer Center and primarily specialize in lung cancer patients. Part of my work is working in the hospital for patients who either have a suspicion of cancer or have a cancer diagnosis but are hospitalized for symptoms of their cancer or side effects from their treatment. As a health services researcher, my research focuses on increasing awareness and access to clinical trials among Black communities and communities with low-income or persistent poverty.
Outside of medicine, I’m a wife and a mom. I have two children, one in elementary school and one in middle school. I recently completed an aquathlon, a swim-run competition, which is a big deal for me because I don’t have a great relationship with swimming. I learned to swim as an adult, so it was a big accomplishment for me to be able to complete this duathlon, so that was exciting. I also love to travel and visit different places across the US or abroad. I also love to eat. I love various types of foods.

When I completed my medical training, I knew that I wanted to be an oncologist. There was no question about that.

A Winding Path to Medicine
Nikki: What was your number one driver to becoming a doctor?
Dr. Charlot: I knew from a young age that I wanted to become a doctor. I grew up in Mattapan, a neighborhood in Boston, and I was privileged enough to have a Haitian pediatrician who had his practice in the community and did house visits. The Haitian community where I grew up was tight-knit and it was informative for me to be able to see someone who shared my heritage be a physician and be one with the community, so I wanted to be exactly like him.
My path to becoming a doctor was not straight and narrow. After I graduated from college, I spent a couple of years working in different types of advocacy work related to education and moved on to teaching middle school students about health professional careers. After that, I got my degree in public health and then after that, I went to medical school. It was a winding path to medicine, but I knew that’s where I would end up eventually.
Why Oncology Became Her Calling
Nikki: How did you end up specializing in lung cancer?
Dr. Charlot: When I completed my medical training, I knew that I wanted to be an oncologist. There was no question about that. I felt like it was the field where you develop close-knit relationships with your patients, so that was a no-brainer. Oncology was the way that I wanted to go.
Concerning lung cancer, I was influenced by my mentor. When I started my training, there weren’t that many options for lung cancer. There was chemotherapy and that was pretty much it. However, during my training, there were a lot of new therapies coming up, like immunotherapy and targeted therapy. The excitement in the field drew me to want to be a part of this growing field concerning options for our patients. The field was getting to a place where we had more options to offer our patients other than chemotherapy itself and that’s where my love and compassion towards lung cancer grew.

It was ingrained in me that we needed to think about the community and the circumstances that people are born in or the conditions they live in for the healthcare system to work.

Growing Up in Mattapan
Nikki: What motivated you to go above and beyond and focus on helping an entire community get better access to health care and treatment options, including clinical trials?
Dr. Charlot: Mattapan is a predominantly Black community and interestingly enough, my street and pretty much my whole block were folks that immigrated to Boston. I have a Haitian background, so my interest in terms of thinking about communities draws from that experience.
I lived in two different worlds. I had the world where I grew up in Mattapan, but I also always went to Catholic school, which was outside of our neighborhood. I saw the dichotomy between the school in terms of the affluence of the area and some of the students who attended that school and my neighborhood where we’re very rich in culture and pride, and hardworking, but we didn’t have the same resources.
When I became a doctor, I did all of my training at a safety net hospital, so we cared primarily for people who were underinsured or had no insurance. It was the hospital where I was born, so it was ingrained in me that we needed to think about the community and the circumstances that people are born in or the conditions they live in for the healthcare system to work.
That’s where my whole approach comes from in terms of thinking about Black communities and the importance of ensuring that they have the knowledge and the awareness of all the resources available to ensure that they have access to care and can improve their outcomes through those connections. As a physician, I think about the Black community and understand ways how we need to make those connections together for us to thrive, do better, and live healthy lives.

I used my background concerning patient and community engagement to improve access to clinical trials, cancer care, and high-quality cancer care.
Developing the CREATE Initiative
Nikki: How did you end up at UNC?
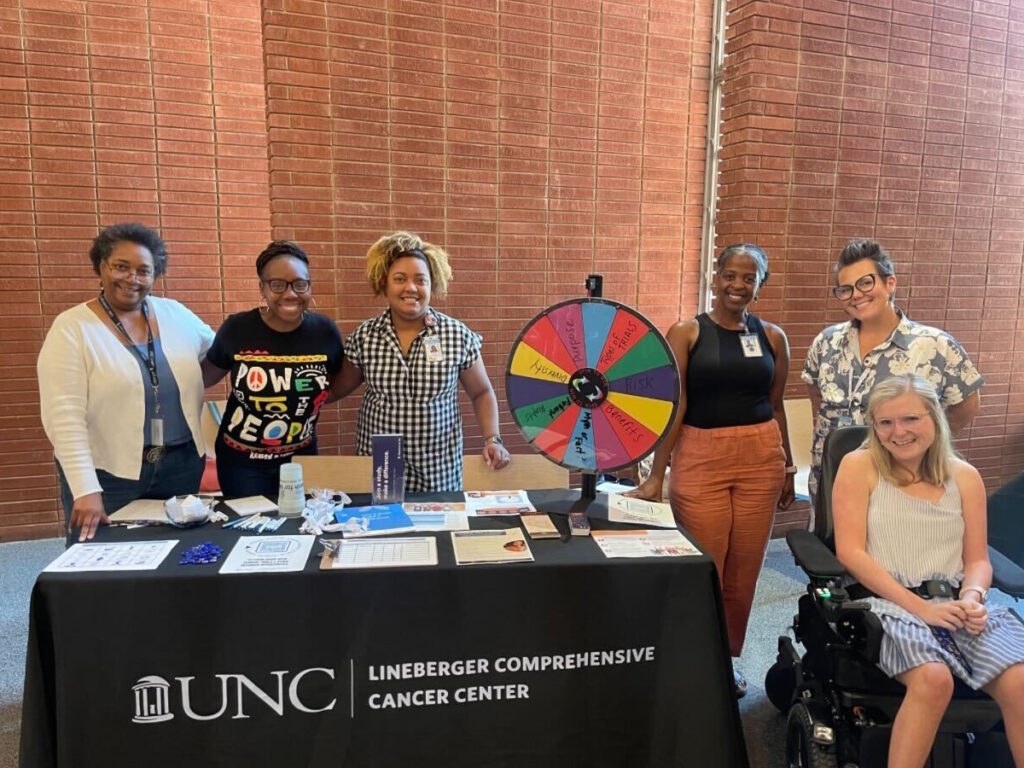
Dr. Charlot: I was recruited to UNC primarily to work as a thoracic oncologist, so my specialty in lung cancer, as well as develop a program that was focused on clinical trials and increasing equity in clinical trials. As a result of my research and clinical background, I ended up starting the CREATE initiative, which is Cancer Research, Equity, and Advocacy Through Engagement. This initiative speaks to the strong community focus and the work that we do with our community partners for the healthcare system to work and for the treatments to get to the people that they were designed to treat. I used my background concerning patient and community engagement to improve access to clinical trials, cancer care, and high-quality cancer care.
Most Common Lung Cancer Symptoms
Nikki: We understand that there’s a wide range of symptoms, but what are the most common symptoms of lung cancer? And what should people never ignore?
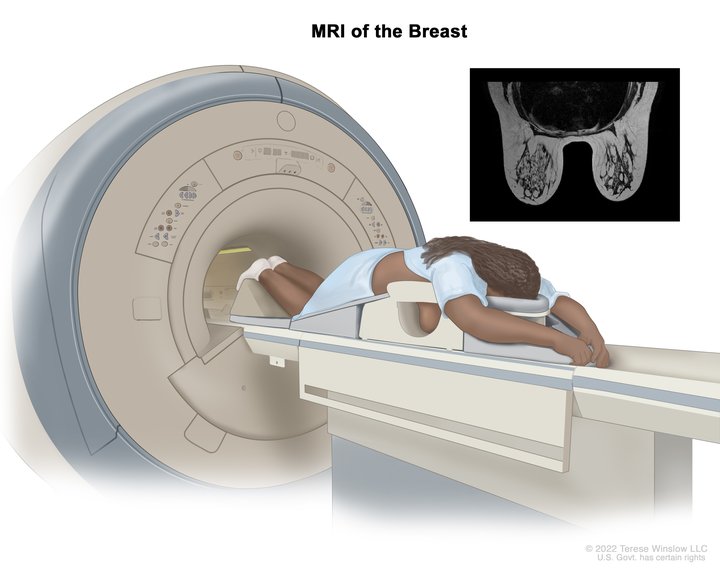
Dr. Charlot: Screening in general is meant to detect cancers early, before they cause symptoms. But generally speaking, by the time a patient is diagnosed with cancer, medical oncologists see patients after the cancer has spread or advanced and not in a stage where it could be cured with surgery. However, things have changed with cancer where we’re using chemotherapy and immunotherapy even for earlier cancer stages.
Common symptoms are generally related to shortness of breath, coughing (particularly coughing up blood), and sometimes weight loss. Those are the top three that patients describe in terms of things that they’ve noticed when they’re diagnosed with cancer.
If the cancer has spread, they could present with various symptoms, like a headache if the cancer has spread to the brain or pain in various areas, like in the bones or the joints. There could be a wide range of symptoms depending on where the cancer is.
The most important thing is to be aware that cancer screening is an option, particularly for people who have had a long history of smoking. Twenty pack-years is the recommendation. Screening is for those who don’t have symptoms, but if they do have symptoms, it’s another reason to see their doctors so they can get examined and evaluated for potential cancer.

It’s important to be able to test these drugs on a variety of people and understand how these treatments impact various groups.

Demystifying Clinical Trials
Nikki: We know that trials aren’t for everyone. What would you say specifically to Black and African Americans to convince them to learn about clinical trials?
Dr. Charlot: Clinical trials are an opportunity to get access to new treatments that are not currently available. For the Black community in particular, we know that outcomes are worse when it comes to cancer survival and mortality rates. Clinical trials provide an opportunity to get access to new drugs, which ideally will prolong life.
It’s important for all patients, regardless of background, to have access. We don’t know how these drugs are going to affect people, whether it’s based on their environment, socioeconomic status, or race. It’s important to be able to test these drugs on a variety of people and understand how these treatments impact various groups.
A Patient’s Clinical Trial Success Story
Nikki: Can you think of a specific story that shows how impactful a trial can be for someone?
Dr. Charlot: I started the CREATE initiative at Lineberger and we’re in the process of completing a research grant that I have, which is building a mobile app for Black women with breast cancer to see if it can help increase discussions about clinical trials with their providers. One of our patient research partners shared her story about participating in a trial where the trial led to her being cancer-free for a very long time in that she’s been able to see this drug become a standard of care for breast cancer treatment.
It’s important to acknowledge the historical past and some of the mistreatment that Black communities and individuals often get within the medical care system.

This goes to show that when going into a trial, we don’t know whether or not these drugs are going to work. What we do know is that when you’re in a clinical trial, you’re under such close follow-up, which gives you even an extra layer of eyes of people who are watching how you’re doing. If these drugs prove to be better than the standard of care, these drugs end up helping people live longer.
It’s fascinating and wonderful to be able to work with someone who’s been through this whole process of participating in a clinical trial and seeing that her participation led to the approval of a new drug that is now being used for breast cancer patients. There’s no better story than to live through the process of being in a clinical trial and to see how that participation led to the approval of a drug that more women and other people with breast cancer can benefit from.
Overcoming Barriers in Black Communities
Nikki: What would your message be to the Black and African-American community who are fearful of clinical trials?
Dr. Charlot: We know that our healthcare system and our research enterprise in this country have not been the best, particularly for our Black communities. At the same time, it’s important to acknowledge the historical past and some of the mistreatment that Black communities and individuals often get within the medical care system. Acknowledgment is at the forefront.
It’s also important to know that there are safeguards in place with clinical trials. It’s important for us, specifically as Black individuals, to be a part of clinical trials because it gives us opportunities that we would potentially not have to access newer drugs. Acknowledge the past and understand that we have a part and the right to have access to newer treatments and interventions.

We need to understand where our patients are coming from, know what their needs are, and partner with them.

The Role of Black Physicians in Healthcare
Nikki: What do you think healthcare professionals can do better when building trust with the Black and African American community?
Dr. Charlot: As a Black physician and even for healthcare providers who are not Black, we need to be one with our community. We need to understand where our patients are coming from, know what their needs are, and partner with them. If we do these separately in our silos, it doesn’t help improve access to care. It doesn’t help our communities thrive and live healthy lives. Making connections is what’s helped me in the work that I do and hopefully helping the patients that I’ve had the privilege to take care of over these past couple of decades as a physician.



Special thanks again to AbbVie, Genmab, and Karyopharm for their support of our patient education program. The Patient Story retains full editorial control over all content.
Stories from Raleigh, NC
Dr. Brandon Blue
Dr. Brandon Blue shares key strategies for better health care and saving lives, especially in communities impacted by multiple myeloma.
The Importance of Cancer Screening | Dr. Colin Ottey
An internal medicine physician discusses healthcare access, preventative care, patient trust, and how both doctors and patients can improve relationships for better outcomes.
The Importance of Cancer Screening | Lemuel Eley
Heart attack survivor at 44 shares his story, advocating for health screenings and proactive care in the African-American community.
Dr. Marjory Charlot, Oncology
UNC oncologist discusses increasing awareness and access to clinical trials among Black communities
Roshonda C., Rectal Cancer, Stage 4
Symptoms: Blood in stool, blood from rectum after intercourse, sensation of incomplete bowel movements
Treatments: Chemotherapy, surgery, radiation