LaShae’s Stage 2B Multicentric ER+ IDC & DCIS Breast Cancer Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

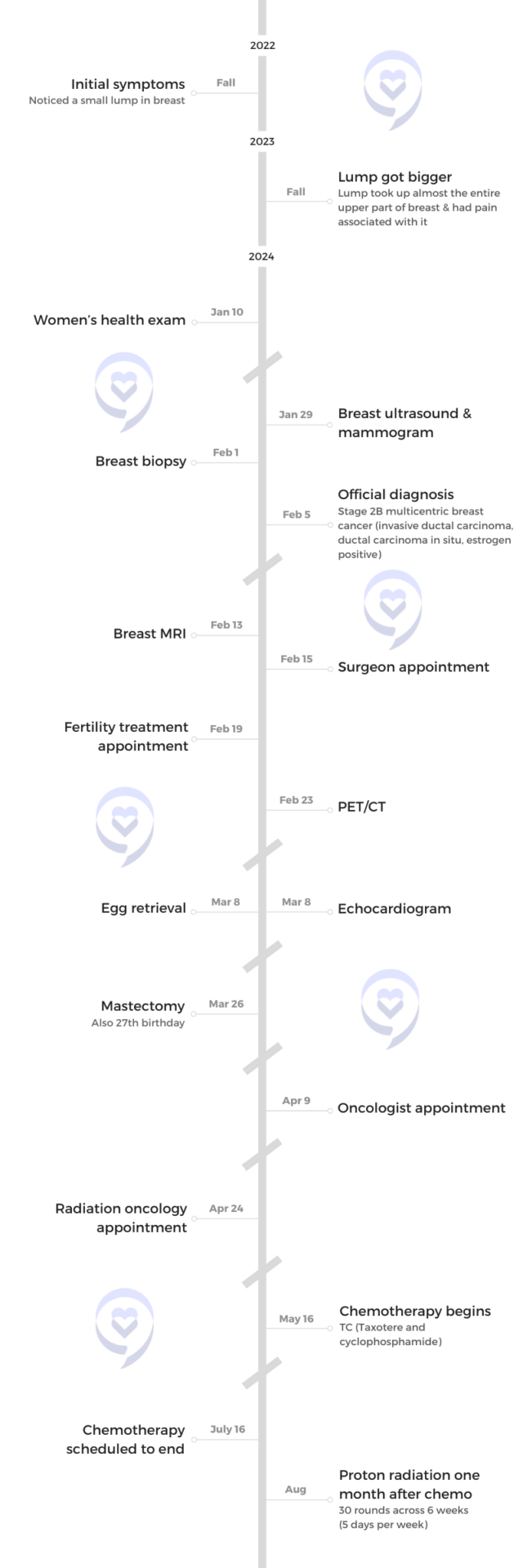
LaShae, a PhD student in cancer prevention research, shares her journey with breast cancer. She initially dismissed a small, movable lump she found in her breast due to her busy schedule, but when the lump grew and she felt pain, she sought medical attention.
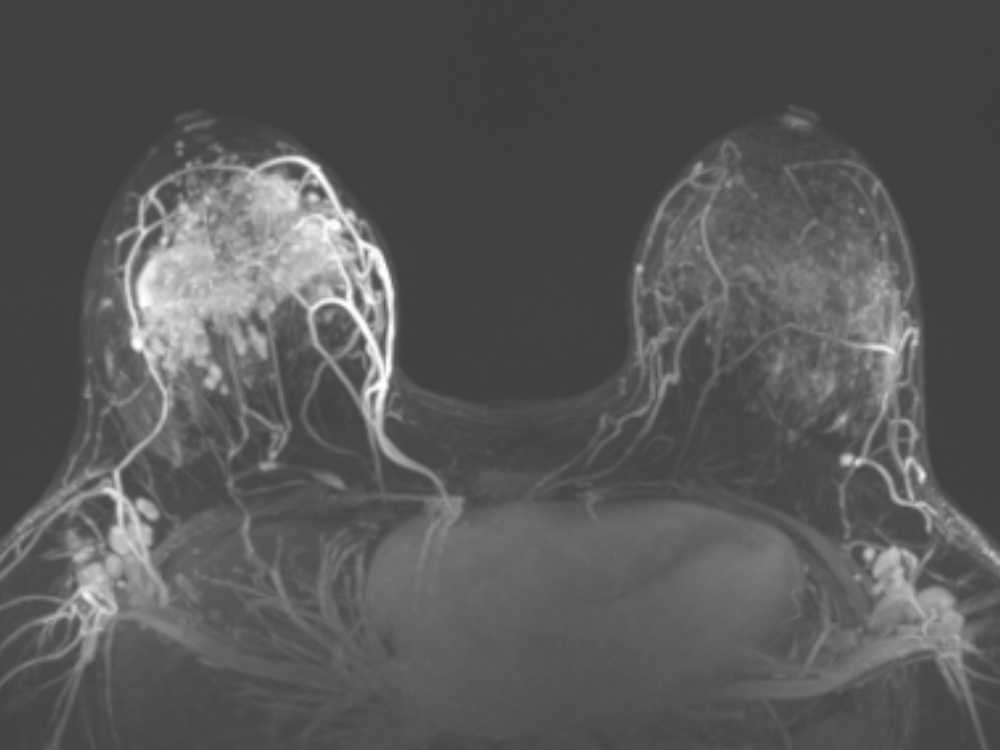
Her doctor referred her for a breast ultrasound and mammogram, revealing multiple masses and widespread calcifications. A biopsy confirmed cancer with a high likelihood of malignancy and a breast MRI revealed the spread in her breast and lymph nodes.
She had a mastectomy on her 27th birthday. Currently undergoing chemotherapy, she continues her fitness routine despite the side effects. Her experience has deepened her commitment to cancer research, particularly for adolescents and young adults (AYAs), highlighting the importance of self-advocacy and support groups.
- Name: LaShae R.
- Diagnosis:
- Breast Cancer
- Invasive ductal carcinoma (IDC)
- Ductal carcinoma in situ (DCIS)
- ER+
- Staging:
- 2B
- Initial Symptom:
- Lump in breast
- Treatment:
- Chemotherapy: TC (Taxotere and cyclophosphamide)
- Proton radiation (scheduled one month after chemo ends)

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I found a small lump about a centimeter in size… I thought I had nothing to worry about.
Introduction
I live in Miami, Florida, but I was born and raised in Nassau, Bahamas, so I am a Caribbean girl.
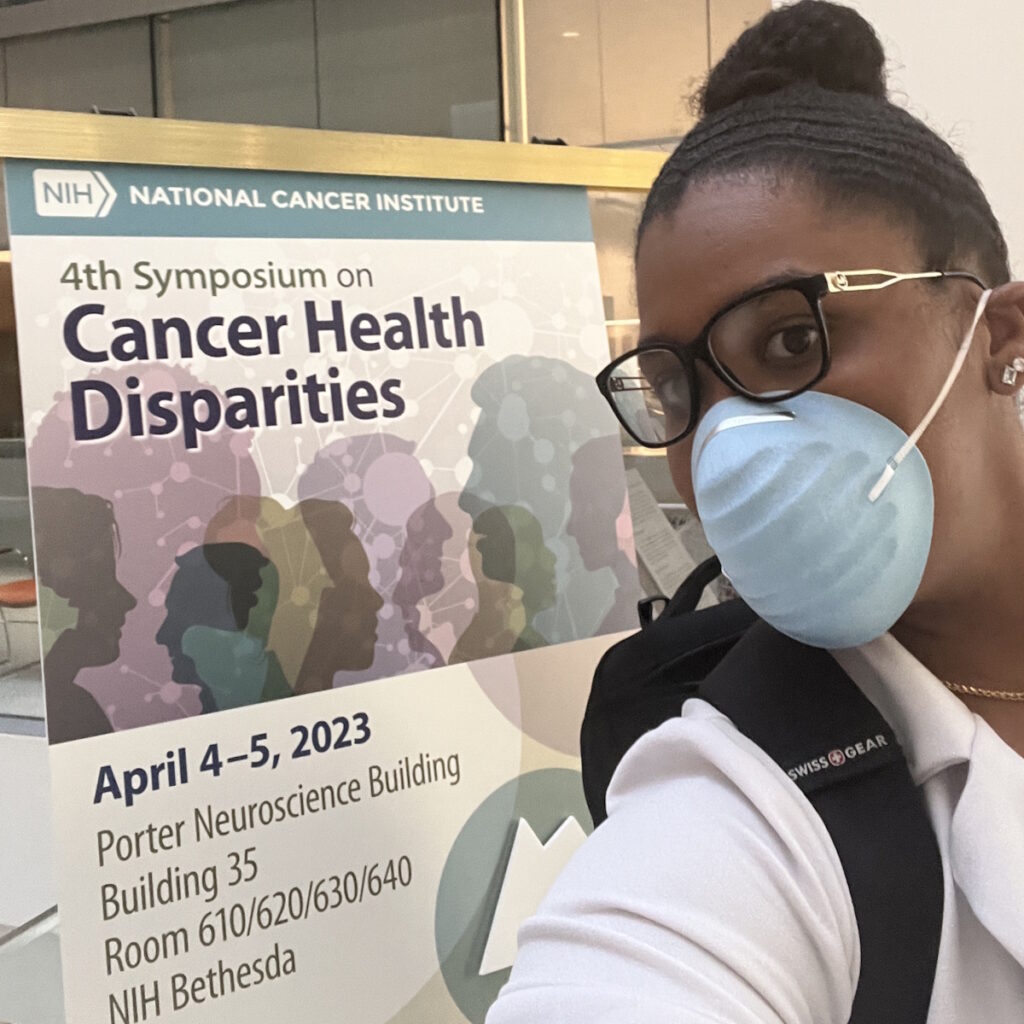
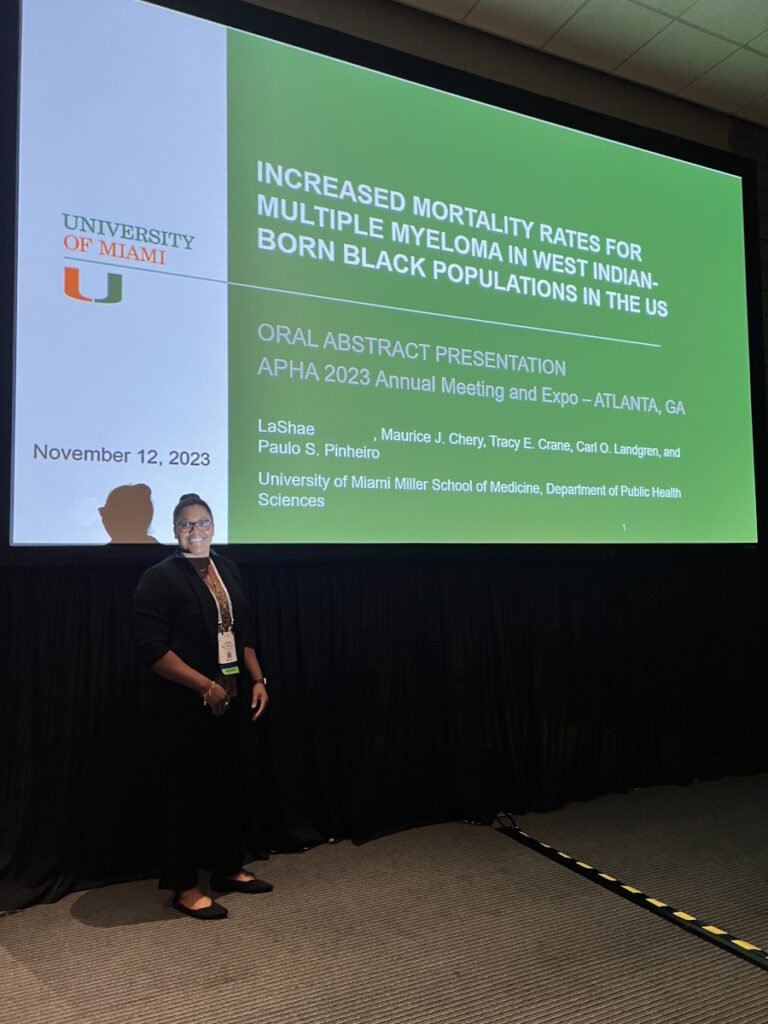
I’m currently doing my PhD in cancer prevention research.


Pre-diagnosis
Initial Symptoms
I found a small lump about a centimeter in size. I didn’t think much of it. I did some research and found out that if the lump was movable, it had a lower likelihood of being cancerous. At that time, mine was movable so I thought I had nothing to worry about.
I hadn’t been doing much cancer research yet. I was looking at obesity research and now I’m at a parallel where we’re looking at exercise and diet and how they can impact cancer outcomes. I was still a baby when it came to cancer research, so that’s a big reason I pushed it to the side.
When my PhD started, a lot was thrown at me at once. Anyone who has done any graduate degree knows. I wanted to be the best student that I could be and the best person I could be for the new lab that I was in, so I prioritized those.
Sadly, like a lot of us, health was put on the back burner, so I forgot about the lump. I’m also a powerlifter. I bench press close to 300 lbs, so if I feel any tension or pain in my chest area, I attribute it to that.
In late 2023, I felt a lump again and wondered if it was the same lump. To this day, I don’t know if it was, but it grew in size so I thought that something was wrong.
I felt pain and that was what alerted me. I scheduled a wellness exam, but I had to keep postponing it because I had a lot of things coming up for my degree. I finally got in to do it in early January 2024 at the student center.
She said they were only going to schedule the ultrasound because I didn’t need a mammogram. I was too young.
Breast Exam
The doctor did a pap smear, vitals, and all the basic things done at a wellness exam, but she didn’t perform a breast exam. When she was about to leave, she asked, “Is there anything pressing that you want to discuss or want me to do for you?” I mentioned the lump and she immediately took it seriously. She put on gloves and performed a breast exam.
She wasn’t sure what it was, but she put “Mass?” on the paper and said, “I’m going to go ahead and be extra cautious. I’m giving you a referral to get an ultrasound and a mammogram.” She gave me instructions on the things that I needed to do and told me where to call, which was very helpful. To this day, that visit and that doctor were a part of the team that saved my life.


Breast Ultrasound
I called to schedule my ultrasound and mammogram. The person on the phone said I was young to be scheduling a mammogram and ultrasound. She asked if I had any symptoms. When I listed them off, I mentioned that I had a palpable mass and pain. She said they were only going to schedule the ultrasound because I didn’t need a mammogram. I was too young.
I’m very persistent and cautious. At this point, I was taking this seriously. You might think that I’m wasting your time because I’m too young and you probably think I can’t get cancer, but I’m going to waste your time.
When I went in for my ultrasound, I was filling out a form and it asked if I was of Bahamian descent. Women from the Bahamas have a higher likelihood of getting breast cancer and having more aggressive cancers due to the BRCA mutation, among other mutations.
They said it would probably going to take about 15 minutes. When the tech started the ultrasound, the moment she put the wand on, her eyes became wide and the same with the person assisting her. I knew that there was something there because it was palpable, but what was going on?
The radiologist came in and said, ‘You have multiple calcifications throughout all four quadrants of your breast.’
Every time they see something, they would take a picture and measure it. They did about 10 of those. Then they asked, “How long have you had these masses?” I replied, “Masses? Plural? As far as I know, I just have one lump.”
Before the ultrasound ended, they brought in someone to do the 360° view because they said they hadn’t done that. As someone who knows about cancer and who’s pursuing cancer research, I knew it meant that it’s spread all over the place. It’s in four quadrants.
When they went over to the left, there was nothing there. It was quick. Then they came back to the right and got another person to come in and help. What was supposed to take 15 minutes is taking 45 minutes now.
I started to gather my stuff to leave and they said, “No, no, no! You can’t leave. We’re about to do a mammogram now. You need to do a mammogram.”


Mammogram
I immediately got pushed to the top of the line and had a mammogram that same day. When I was done, I started gathering my things again and they said, “No! You can’t leave. The radiologist is going to talk to you right now. They’re going to talk to you today before you leave.”
They took me to a quiet room. The radiologist came in and said, “You have multiple calcifications throughout all four quadrants of your breast.”
I couldn’t believe what I heard. I started to get dizzy. I power lift daily. A couple of weeks prior, I bench-pressed 292 lbs, squatted 440 lbs, and deadlift almost 500 lbs that I had to get drug tested.
They start looking at you with that look of pity. After that, I asked what the next step was and they said I needed to do a biopsy.
When I found out the results, I felt a little better than having all of that anxiety trying to figure out what I had.
Biopsy Results
MyChart popped up and I saw the notes from the ultrasound and mammogram. It said fine calcifications throughout all four quadrants of the breast spanning 12.7 cm. Then it said it was in my lymph nodes and that I was BI-RADS 5. I looked it up and it meant at least a 95% chance of having cancer. I’m waiting for the biopsy results and now I’m stressed out.
Diagnosis
Getting the Results
Three days later, I got a call. They said, “Hi, I’m calling about your results,” and asked if I had a place to sit. Every time, they give you hints. I said, “Let me try to find a place,” and then they said, “We can call you back if you like.” I’m like, “No, no, no, no, no, don’t call me back. You already just made my brain explode. What’s going on?” Then the doctor lets me know that she doesn’t have good results. It was malignant.

Reaction to my Stage 2 Breast Cancer Diagnosis
When I found out the results, I felt a little better than having all of that anxiety trying to figure out what I had. Hearing that was a relief. After I got the phone call, the surgeon’s office called and I made an appointment.
Breast MRI
The breast MRI was very uncomfortable. Based on the results, they let me know that it was confirmed. I do have widespread, cancerous-looking things throughout my breast and in my lymph nodes.
I had my mastectomy on my 27th birthday. At first, I was upset, but I think it’s good because I would always celebrate when they took the cancer out of my body.
Mastectomy
After the MRI, the surgeon let me know that I didn’t have that many options because it was in all four quadrants of my breast. Usually, people can do a lumpectomy or certain types of mastectomies, like skin-sparing or nipple-sparing. I had to do a simple mastectomy, so it’s a flat closure along my sternum to my underarm or axilla. I think that was better than having to make a bunch of decisions.
She also told me I would be doing a PET scan. When I got the results, it was localized to my breast and nearby lymph nodes, so that was a big relief.


Pre-surgery Tests
I did a chest X-ray, EKGs, blood work, blood typing and cross-matching, and other tests before surgery.
I also worked out a lot because I wanted to prepare my body for the battle. One of the things I learned is that as you go through treatment, your body goes through a lot and you can lose muscle, which is detrimental to your outcome. I kept powerlifting and retaining muscle right up to the surgery.
I had my mastectomy on my 27th birthday. At first, I was upset, but I think it’s good because I would always celebrate when they took the cancer out of my body. After the mastectomy, my surgeon came in and explained that she removed the cancer. Two lymph nodes were positive and from what I know, that’s a hit or miss. Based on the final pathology, I can either have chemo or not, but I would definitely need radiation.
When I got home, that’s when the side effects kicked in. Fatigue was number one. I immediately had to shower and then I fell asleep for 18 hours.
Treatment
TC Chemotherapy
I was passed off to the medical oncologist. I met with her after my surgery and she’s the one who’s going to be spearheading the chemo, radiation, and hormonal treatments.
She let me know from the get-go that I would need chemotherapy and that’s the standard of care. I also would need radiation and hormone treatment because my stage 2 breast cancer was ER+, so I’m going to need to be on hormone treatment for 5 to 10 years.
It was a toss-up between A-CT (Adriamycin, cyclophosphamide, Taxol) or TC (Taxotere and cyclophosphamide). I needed chemo because of the lymph node involvement and my age. The longer you live, the higher the likelihood of recurrence simply because you’re around longer.
I’m currently undergoing chemo. We decided to do TC based on the results from additional testing. We did a MammaPrint® and I was found to be at high risk for recurrence.
Chemo was what I feared the most from the beginning. I had to get to my first chemo appointment early because I was doing scalp cooling. It didn’t take that long and it wasn’t as scary as I thought. They give a lot of pre-medications. I had never taken Benadryl at that dose so I was dizzy and sleepy. It knocked me out.


Side Effects of Chemotherapy
Less than 24 hours after chemo, I went to the gym and power lifted because I wanted to keep doing what I do. I felt solid, but when I got home, that’s when the side effects kicked in. Fatigue was number one. I immediately had to shower and then I fell asleep for 18 hours. It was brutal.
I had GI side effects. It wasn’t good. I got a headache and my whole body felt sore. I work out a lot, so I know what soreness feels like, but it had nothing to do with my workouts. It was a general, full-body soreness that even my bones were hurting. I had to take Zoladex to preserve my ovaries so that I’m able to have children after this. A lot was going on.
The side effects lasted for about five days. Over a week after chemo, I feel great. I was able to do a workout and not crash afterward.
This has opened my eyes to a new group that I had no idea was part of a disparaged group: AYAs or adolescents and young adults.
Cancer Research
I’m in a unique situation as somebody who wants to do cancer research for their entire career and is in the middle of a PhD focused on cancer prevention. It was very surprising, but it helped me get to my diagnosis. I would not have taken this seriously or even known I had alarming signs if I didn’t have that base knowledge.
When I think about what has happened, all I think about is how I’m going to be a much better researcher. I knew I wanted to work with marginalized and disparaged communities to help those who needed help the most. I’ve always believed in doing that and helping the less fortunate.
This has opened my eyes to a new group that I had no idea was part of a disparaged group: AYAs or adolescents and young adults. I’m going to include them in anything that I do in research and want to do community work with that group because being a part of that group, I understand now that these are unique circumstances.
When you’re a young adult, you are just starting your life. When you go to the doctor’s office, you’re the youngest. When I went to one of my appointments, the medical assistant asked where the patient was. I was right there, but she didn’t expect me to be the patient. Sometimes I go with my mom and they think she’s the patient.
This is very emotional and very isolating. Cancer in itself is isolating, but you may also be the only one in your age bracket going through this. When you go to the doctor’s office, people feel sorry for you more because of your age.
My experience is going to make me a much better researcher. It’s going to make me more invested and make me an advocate. I used to want to be an advocate, but now I want to be a research advocate and living proof.
Cancer is very emotional from when you get the diagnosis and throughout the whole process. This is a journey. You go through different emotions. I deal with it by taking deep breaths. That helped a lot.
I joined my AYA support group. Joining support groups is vital because they are going through the same thing. They’re at different stages of the journey, so they’re able to guide you and help you get on track because you’re pulled in so many directions and it’s overwhelming.
Caribbean people tend to have more aggressive cancers when it comes to certain types and they’re diagnosed at younger ages.
Genetic Mutations
Caribbean people tend to have more aggressive cancers when it comes to certain types and they’re diagnosed at younger ages. At the Sylvester Comprehensive Cancer Center in Miami, they asked me ahead of time if I was of Bahamian descent because they’re aware of this.
We’re known to have the BRCA mutation and other mutations. I got the comprehensive panel done and it turned out negative for all. I didn’t have all the common risk factors. I’m the first person in my family to ever get breast cancer, so I could not tell you at all why I got this.


Words of Advice
For patients undergoing chemotherapy, come in with an open mind. You’re going to be scared, but don’t stress out because stress is not good for you. It won’t help with your outcome.
Get some ice compression for your hands and feet to prevent neuropathy, depending on the type of chemotherapy that you’re going to have to get infused. Taxotere has been linked to neuropathy, so I did that.
Try to eat bland foods when you’re going through chemotherapy. If you don’t eat, you’re going to feel terrible. I know all these things are going on, but you’ve got to eat something. Whenever I didn’t eat, I would feel terrible. I started to feel better when I did. Nutrition is so important.
Advocate for yourself because only you know your body.
When you feel good enough, go outside and take a walk. I’m not saying do what I did 24 hours after chemo, but go out and move because it’s been linked to way better outcomes.
Advocate for yourself because only you know your body. There are a lot of professionals who are trained to diagnose. I do research and I know the statistics. But if we rely solely on the numbers, I’m not supposed to have cancer. I’m not even supposed to get screened.
No matter how young you are, make sure to go to your physical exam every year. Be in touch with your doctors. Eat well and exercise to be the strongest you that you can be.


Inspired by LaShae's story?
Share your story, too!
More Breast Cancer Stories
Symptom: Sunken in nipple of right breast
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Symptom: Lump in right breast
Treatments: Lumpectomy, double subcutaneous mastectomy, hormone therapy (tamoxifen)
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
LaShae R., IDC & DCIS, Stage 2B, ER+
Symptoms: Lump in breast, pain
Treatments: Chemotherapy (Taxotere and cyclophosphamide), proton radiation
Dee D., Metastatic Breast Cancer, IDC & DCIS, ER+
Symptoms: Inability to produce milk on the left breast while breastfeeding, breast pain (palpable and radiating to the back), lumps in the breast and armpit
Treatments: Chemotherapy (AC-T), surgery (bilateral mastectomy & axillary lymph node clearance), radiotherapy, hormone therapy (Zoladex/goserelin), aromatase inhibitor (letrozole), targeted therapy (Kisqali/ribociclib)
Cat L., IDC & DCIS, Stage 2B, ER+
Symptom: Pain in left breast radiating from lump
Treatments: Bilateral mastectomy, chemotherapy, hormone therapy (tamoxifen)




