FDA Update: Good News for Multiple Myeloma?
Unanimous vote by Food & Drug Administration (FDA) Committee Leads to New Endpoint for Multiple Myeloma Clinical Trials – And Could Lead to Changes for Other Cancers
Published April 13, 2024
“Yesterday, was a historical moment when the FDA Committee ruled on a faster way to approve therapies for multiple myeloma. We were honored to present EVIDENCE meta-analysis, work I pioneered 15 years ago.”
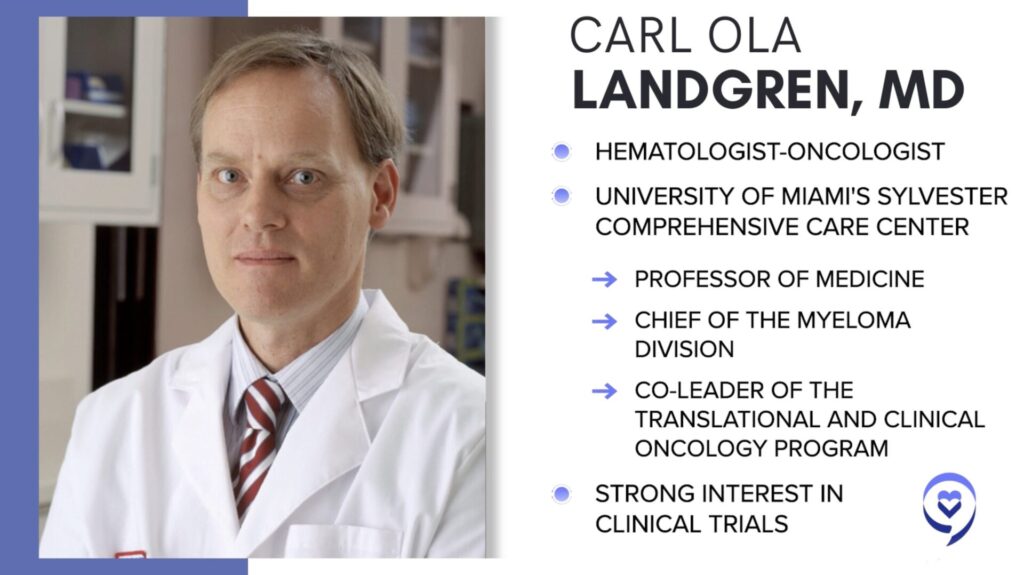
Dr. C. Ola Landgren to The Patient Story
Dir. of Myeloma Research Institute
Sylvester Comprehensive Cancer Center
FDA Update: What It Means for Patients
Approval Criteria for MRD-Targeted Therapies
Next Steps and Timeline
Addressing Potential Concerns
How This Could Lead to More Treatments
Editor’s Note: This is not medical advice. Please consult your healthcare team for your care decisions.
The rapid shift in treatments and clinical trials available in multiple myeloma has led to more options for patients. But in the process, top myeloma experts and patient advocates have said the old standard to get new treatments approved out of clinical trials has become complicated and burdensome, leading to longer times to new approvals. An FDA committee decision Friday, April 12, may lead to even more treatment options on the table for what’s largely described as an incurable but highly treatable disease.
One of the leading advocates for the change and Director of the Myeloma Research Institute at University of Miami’s cancer center, C. Ola Landgren, MD PhD, says this new endpoint may also benefit other cancer spaces soon.
- FDA Update: Good News for Multiple Myeloma?
- Unanimous vote by Food & Drug Administration (FDA) Committee Leads to New Endpoint for Multiple Myeloma Clinical Trials – And Could Lead to Changes for Other Cancers
- General summary: What does this mean for multiple myeloma patients?
- Why should I care about a clinical trial endpoint?
- What is the change in endpoints from the ODAC decision?
- Will this lead to changes in other cancer clinical trials?
- Stay tuned for more updates in multiple myeloma
- Relapsed/Refractory Myeloma Stories
- Unanimous vote by Food & Drug Administration (FDA) Committee Leads to New Endpoint for Multiple Myeloma Clinical Trials – And Could Lead to Changes for Other Cancers
Good news for multiple myeloma? The big topic of the day in multiple myeloma for many patient advocates and physicians came on April 12, when the FDA’s Oncologic Drugs Advisory Committee (ODAC) unanimously approved (12 to zero vote) using minimal residual disease or MRD a new endpoint in multiple myeloma clinical trials. The decision means the group agreed it was time for a change that would benefit multiple myeloma patients.
WATCH: ODAC meeting on YouTube
General summary: What does this mean for multiple myeloma patients?
This may lead to the FDA moving more multiple myeloma therapies in clinical research through accelerated approval. Clinical trials are how new drugs and therapies are given the green light for commercial use, which means they become available as another tool in treating patients.
Leading voices in multiple myeloma, like C. Ola Landgren, M.D., Ph.D., director of the Myeloma Research Institute at Sylvester Comprehensive Cancer Center in Miami, Florida, have been arguing that a better endpoint is minimal residual disease or MRD. He described the move as “fantastic news” for multiple myeloma patients.
“With MRD as a new endpoint, it will give patients access to new therapies much faster! This is exactly what patients need and want,” said Dr. Landgren in a University of Miami news update. “It is a milestone in the field of multiple myeloma and will set the stage for the development of novel therapies for other cancers.”
Myeloma patient advocates like Jenny Ahlstrom have said this is important because the disease, while highly treatable, is still not officially “curable,” and patients having to wait longer for a new treatment option may run out of time.
“With the acceleration of drug approvals, many patients are living 10, 15 years instead of three to five years although we still know that 40% of patients are still dying under 5 years,” said Ahlstrom, founder of Healthtree Foundation, during the nearly seven-hour long ODAC meeting. “There is still no known cure, so the innovation needs to continue and we still have an urgent need.”
Why should I care about a clinical trial endpoint?
In generic terms, the way the FDA decides whether to approve any clinical trial is based on a set of information, a lot of it comparing the study drug to the existing standard of care. The questions boils down to:
- Is this better for patients than what’s available now?
- How and why?
An endpoint is a measurement that’s used to help answer those questions. If a clinical trial does not meet the given endpoint, the FDA does not approve it.
What is the change in endpoints from the ODAC decision?
Old endpoint: Overall survival (OS)
Let’s set the stage for what has historically been used as the standard against which the FDA would decide whether to approve a study drug.
The endpoint used in many FDA clinical trial decisions, including in multiple myeloma, is something called overall survival (OS), defined as “the average length of time patients are alive after the start of treatment.”
According to the FDA’s own reporting, there are “advantages” and “disadvantages” to using overall survival as an endpoint:
- Advantages
- Easily and precisely measured
- Generally based on objective and
quantitative assessment
- Disadvantages
- May be affected by switch-over of
control to treatment or subsequent
therapies - Needs longer follow-up
- Includes noncancer deaths
- May be affected by switch-over of
But then the numbers started growing and once it got to 0.5, I started having conversations with multiple experts. ‘What would you do? How would you do it? What’s your strategy?’
Jenny Ahlstrom in her patient story
New endpoint: Minimal residual disease (MRD)
So what is minimal residual disease (MRD)? It is a measurement that indicates how many myeloma cells are still present after someone goes through treatment. Typically, the number of cells is so small that the disease is undetectable if using standard testing. The tests for MRD are much more sensitive, and can help patients and their physicians make a decision on whether they need to go for more treatment.
Ahlstrom, a long-time multiple myeloma patient advocate, shared with The Patient Story in 2023 how MRD testing helped her personally lead to treatment decisions.
“In myeloma, an official relapse is a monoclonal protein of 0.5. We were watching that number and it was 0.13. I first saw it on an MRD test that I did so it was very sensitive and started seeing some early indication. I had this faint band that wasn’t measurable for a really long time, for almost two years, so you couldn’t even quantify it,” shared Ahlstrom.
“But then the numbers started growing and once it got to 0.5, I started having conversations with multiple experts. ‘What would you do? How would you do it? What’s your strategy?’
“It took a couple of years and then once it hit 1, my doctor said, ‘Now it is time to do something.’ I got multiple opinions and I had a lot of knowledge about what my options were so I was able to weigh those in my mind.”
In a program hosted by The Patient Story in October 2023, Dr. Landgren shared the importance of MRD.
“The field has evolved. We see many patients achieving remissions and minimal residual disease (MRD) negativity so there is no detectable disease. When you don’t have those perspectives, it’s not really something brought up frequently with cure. With more and more of these drugs delivering great, deep, durable responses, it’s natural for the field to talk about it.”
Will this lead to changes in other cancer clinical trials?
Dr. Landgren says it’s very possible the move could “open the field for other diseases to move in the same direction, and it could give cancer patients access to therapy many years sooner, in a much broader context beyond myeloma.”
“It is a milestone in the field of multiple myeloma and will set the stage for the development of novel therapies for other cancers,” he added.
Stay tuned for more updates in multiple myeloma
The Patient Story is slated to talk more with top myeloma specialists on the implications of this decision for multiple myeloma patients and their families.
In the meantime, check below for our library of myeloma stories to hear from patients on their experiences after getting a diagnosis.
If you want to get first access to attend our educational programs featuring top myeloma experts and advocates and/or get an alert when a new myeloma patient story is up, please join our community here.
Relapsed/Refractory Myeloma Stories
Dr. Yvonne D., Relapsed/Refractory Multiple Myeloma
Symptoms: Severe hip pain, trouble walking due to a broken pelvis, extreme fatigue, bone pains
Treatments: Chemotherapy, stem cell transplant, radiation therapy, surgeries, CAR T-cell therapy
Michele J., Relapsed/Refractory Multiple Myeloma
Symptoms: Fatigue, anemia, persistent lower back pain, sharp leg pain during movement
Treatments: Surgery, chemotherapy, stem cell transplant
Theresa T., Relapsed/Refractory Multiple Myeloma, IgG kappa Light Chain
Symptom: Extreme pain in right hip
Treatments: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
Laura E., Multiple Myeloma, IgG kappa
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
Donna K., Refractory Multiple Myeloma
Symptom: None; found through blood tests
Treatments: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T-cell therapy, selinexor-carfilzomib






2 replies on “FDA Update: Good News for Multiple Myeloma?”
I have mugs and go for regular checkups.
What do you think my chances are for
Mgus should I worry about getting
Multiple myeloma?
I’m excited extremely excited for new meds and trails and studies to help benefit so many with Multiple Myeloma. Thank all of you Doctors for your care and concerns with your patient’s and the millions of Multiple Myeloma patients in need.