Jason’s Stage 4 Metastatic Colorectal Cancer Story
Jason, a motorsports photojournalist and business owner who rescues cats with his wife, led a busy life. His career often involved working long hours, being away from home for extended periods, and physical challenges. When new symptoms arose such as blood in his stool and gastrointestinal issues, he put them aside and explained them away. Until the bleeding worsened.
He visited the doctor to address his symptoms and his doctor discovered elevated liver levels following blood work. Further tests and biopsies revealed a stage 4 colorectal cancer diagnosis with metastasis to the liver.
Motivated by the many positive aspects of his life, Jason refrains from talking negatively about his cancer. He discusses how he ignored initial symptoms and his encouragement for people to get checked when new symptoms arise. Jason describes the process of his cancer diagnosis, including the challenges of undergoing chemotherapy and the emotional toll it takes. He also discusses his unique perspective gained from surviving a heart attack years earlier and his tips for undergoing a colonoscopy with ease. Despite his diagnosis, he remains grateful for the fulfilling aspects of his life.

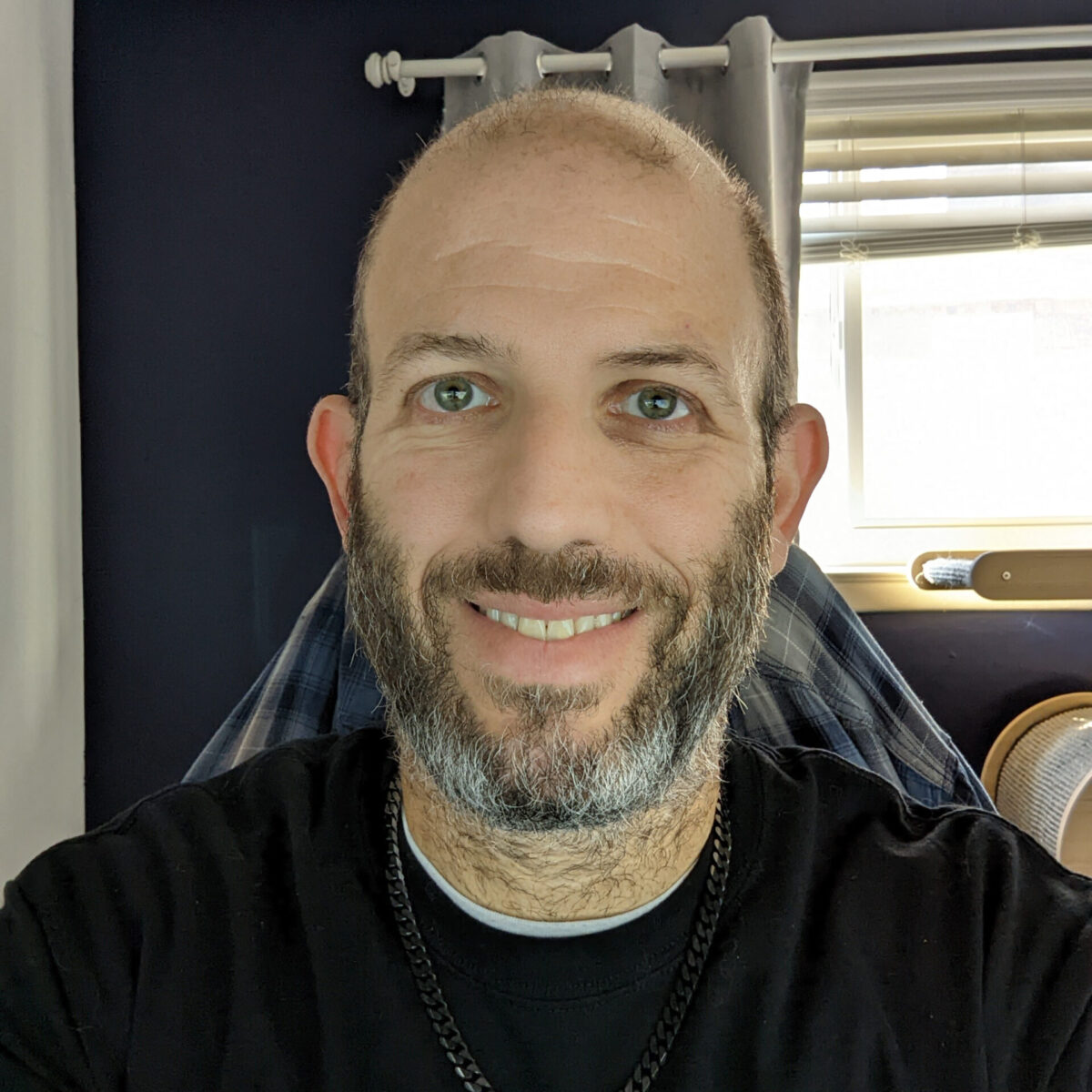
- Name: Jason R.
- Diagnosis (DX):
- Staging:
- 4
- Symptoms:
- Bleeding and spotting
- Diarrhea
- Tenesmus
- Feeling run down
- Age at DX: 47
- Treatments:
- Chemotherapy
- FOLFOX
- Avastin
- Irinotecan
- Vectibix
- Capecitabine
- Radiation
- 28 treatments
- HAI Pump
- Chemotherapy
I really try very hard to not complain about my cancer, because all the other stuff in my life is so awesome.
Jason R.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Lifestyle
Tell us about yourself
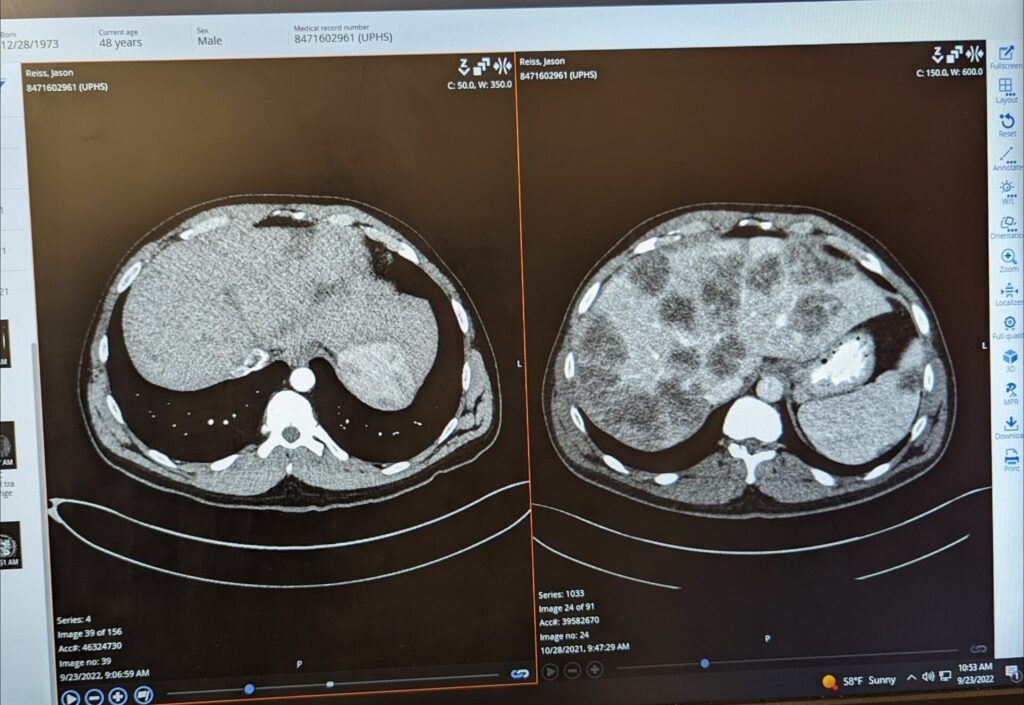
My name is Jason. I’m 49 years old and going to be 50 years old in 10 days. I am a stage 4 colorectal cancer patient with metastasis to my liver which was considered innumerable upon my diagnosis. There were so many that they couldn’t count. The last time I was scanned, there were so few that they couldn’t really find them.
I’m married. We have 5 cats. We also are active in cat rescue. We just delivered 3 cats that we had been raising as fosters. One of them already went home. Two of them are still looking for families. Those 3, I think, make 40 in the last 3.5 years through our house. More than 2 of those years we’ve been dealing with my diagnosis at the same time.
My wife is an amazing, incredible, unbelievable person. I don’t know where she finds the time, the strength, the energy to deal with my craziness. She teaches a foreign language in a middle school – that’s her job. She’s teaching 12 year olds how to speak French, and she raises all these babies. I just look good. I pose with them and I take cute pictures and they look nice with my big beard and people love that.
My wife does all the work. She gets up at 6 in the morning to feed them. She’s down there giving them medication. She gives them shots sometimes when they need it. She does all this amazing stuff and it just makes me look good. That’s the short story of us. I enjoy doing that a lot. Helping out, even just sitting down there and socializing with them, because that’s what I’m doing. I’ll go down with my laptop and sit that on my lap. They come up, they sleep on me, I pet them, and just get them used to people. Used to people’s noises and big, boomy voices like mine and things they’re going to experience.
One of the kittens, the one that got adopted the other day that just left here, went to a home with 2 dogs. She’d never seen a dog before. We already have a video of her laying on the couch, grooming the dog. Or the dog was grooming her – one or the other. For her to be that comfortable that quickly, she’s only 4 months old, we attribute that to us taking a lot of time to socialize with them, but it’s mostly my wife. I, as you might imagine, dealing with all of this stuff, takes up a fair amount of time.
What do you do for work?
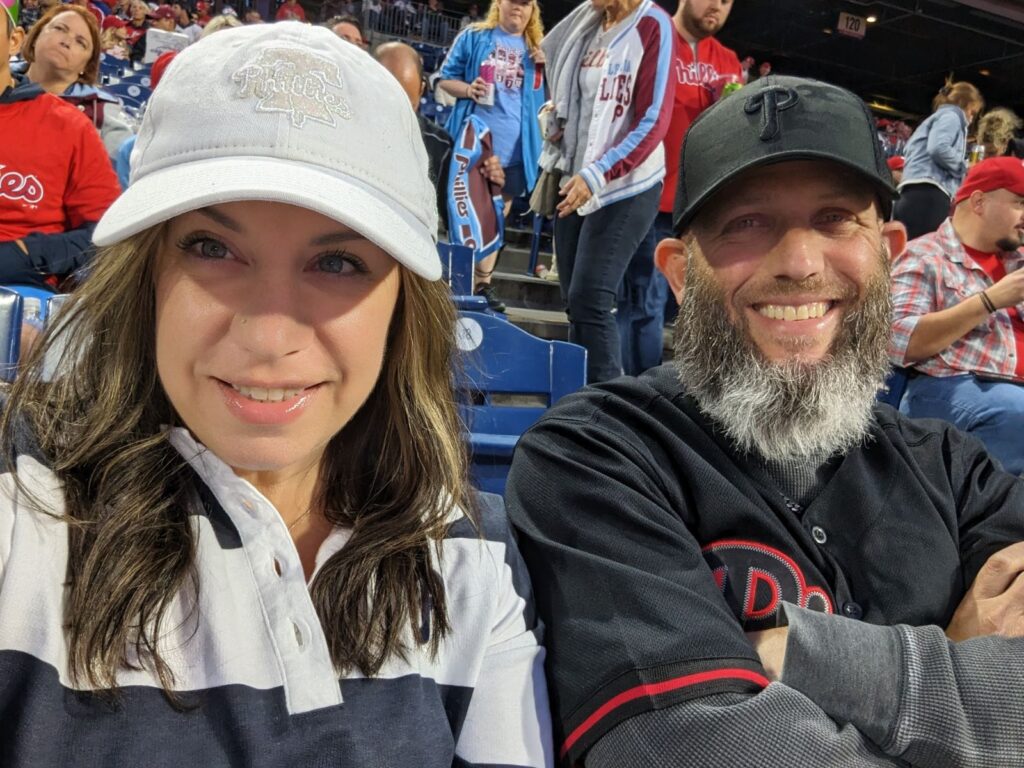
Work-wise, I have a very interesting job. At least to me. I own my own company. I’m a motor sports photojournalist. These days, that encompasses many things from managing social media to working with outside partners. I work for a racing series that puts on motorsports events around the country. I’m basically the staff photographer, social media-writer guy, and I do all of those things. I go to these events that are in North Carolina, Virginia, Maryland, Michigan, Ohio. There’s 9 events through the course of the year. We go to two tracks twice.
I travel to these events where I work 16 hour days taking racing photographs of some of the fastest cars on the planet. They go from 0 to 200+ miles an hour in an eighth mile in 3.6 seconds. I have to take a picture of that while I have cancer and not die. It’s 16 hour days, it’ll be 3 or 4 of those in a row. It’s not just one. 20,000 steps, 25,000 steps, being on the side of the track, the track temperature is 140 degrees and I’m standing next to it. That’s my life.
When I think about my cancer and I think about the things I get to do – rescue all these cats, do all this crazy work stuff – my life is like somebody else’s bucket list. We have a separate room in our house. We use the laundry room for the cats because it’s a tile floor. We don’t use it for anything else other than to do laundry. So we have a whole room of our house we could dedicate to that.
I have cancer and it sucks, but what do I have to complain about? I get to do all this other cool stuff.

We don’t have any children so it’s okay if I say to my wife, “I’ll see you in a week.” I jump in my car and I drive to a race that’s 7 states and 700 miles away, and I go shoot photos of my friends is really what I’m doing. Basically, I get paid to work with my friends and take pictures of them and help promote them in their racing programs and all the other things that’s involved in our little tiny corner of the world. That’s the very short story. This 2024 will be 23 years of doing what I do. I’m very lucky. There’s not a lot of people in the world who get to do it. There’s a much smaller subset of people who actually make a living doing it, where I do.
The racing series that I work with, I would consider like triple-A baseball. You have the major racing series, which is called the NHRA. Many of our racers will graduate and go race there. That’s my life. Yeah, I have cancer and it sucks, but what do I have to complain about? I get to do all this other cool stuff. That’s the very short, condensed story of why I fight so hard to stay alive. I get to jump in my car an go take pictures. Then I come home and I edit pictures and people pay me money for that, and I’m really good at it. Don’t get me wrong, you don’t get to where I’m at without being talented enough to get there.
What keeps you motivated?
I really try very hard to not complain about my cancer, because all the other stuff in my life is so awesome. Starting with my wonderful wife who makes it possible not only by holding down the house while she raises the animals and teaches the children and takes care of our own cats. She also carries the health insurance. Thank you, honey very much for that. And for sticking it out when work is hard, because you’re making it possible for me to be able to be here and do all this stuff.
So grateful. So thankful for all of those things that I [go] forward and I continue to live. Eventually, something’s going to take me. It might be my cancer, it might be something else. I don’t know, but I have all this other great stuff to live for, so I keep doing that.
Symptoms
What were your initial symptoms?
I probably ignored the real symptoms for a long time and explained those away by my poor diet because I didn’t have a great diet. My diet was okay, but I tend to, when I crave something, I’ll overeat that thing. If I want, let’s say, hard mini pretzels, I’ll buy a pound bag and eat half of that. I would explain away all of this gastrointestinal distress to my eating habits. If we’re getting wings, I’m going to order 25 for myself. One human does not need to eat 25 wings. 12 is probably enough. These days, I’ll eat 6 and I call that good.

I explained away a lot of the looseness. I never really looked at it, I just knew it didn’t really feel good coming out. I don’t know the last time I had a normal bowel movement until after I had radiation treatment and it helped me. They’re still not normal, but they’re so much more normal than what they were before my diagnosis and I started any treatment. I struggled with my gut for a very long time. I thought it was IBS. I’m busy. With my job, I’m gone 9 or 10 weeks, probably a third of the year most of the time. There have been years where it’s been closer to half the year I’m not here because I’m off running around the country playing race car.
»MORE: Colon & Rectal Cancer Symptoms
I would see, every so often, a little tiny bit of blood. Well, I had a hemorrhoid too. Because I had high cholesterol, do I remember to mention the blood that I saw 6 months ago to the doctor when I’m here for my yearly cholesterol check? Maybe not. I know I mentioned it to him at least once, and he said, “You probably just have a hemorrhoid, keep an eye on it and let me know.” Well, here we are. I don’t blame him. It’s not his fault. It’s my body. He can’t possibly know the other things I’m dealing with.
Overlooking symptoms
My issue is more that I didn’t put them together. Like, hey, this happens when you poop. When you eat this thing, this happens. Maybe you should go to the doctor and say, “I’m having some GI trouble.” My career at the time was so busy and so demanding. As a writer, 40 hours usually doesn’t really cut it.
When you’re trying to make a living as a writer, it’s closer to 80. It could be closer to 100 some weeks. It’s not about the amount of time you put into the product that you’re delivering. I have incredibly high standards, ridiculously high standards. I would not turn something into someone else that I would not put my name on. My name is on everything that I do, my photos and my writing. I’m not going to put my name on junk. That requires an incredibly intense commitment and a singular focus. That focus destroyed relationships. Probably contributed to a heart attack I had 12 years ago.
I’m as type A as they come. When you think of a driven type A person, I’m the one in the driver’s seat driving the bus of the type A people. That’s how insane things are in my head. I just shoved it. It’s not a thing. I eat a lot of popcorn, it tore me up inside, that’s why I saw blood. I would just rationalize and rationalize because I felt okay. It wasn’t like I felt bad. If I had diarrhea from poor eating, I knew that that’s what it was from. Most of the time I didn’t feel poorly. It was just I had this GI crap going on and I didn’t put it all together until I was pretty close to being diagnosed.

How often did you notice blood in your stool?
In the beginning, it would be once every 6 or 9 months. I would see it for a day or two and then it would go away. That very well could have been hemorrhoids. That’s why I’m not sure of when I actually started seeing what you would call symptoms or a doctor would call symptoms. I just know most of my life, I explained away all the GI crap that I had going on from a little bit of blood to having diarrhea 3 days in a row to, I eat terribly. Or I had too many wings or I drank too much lemonade, and all the sugar is tearing me up.
»MORE: Is Frequent Diarrhea a Sign of Cancer?
When you don’t feel bad, it’s easy to rationalize all of that away, so I did. I finally became ill enough to where I was like, alright, I’m going to have to do something. My wife and I were on vacation in August of 2021. We typically go on vacation for our anniversary every year. Last year and this year we couldn’t because my racing schedule is on top of it. But that year, 2021 was the middle of COVID. I avoided some stuff because of Covid. You don’t want to go to the doctor. You’re not sure if you could go out. I didn’t go to the doctor. I probably should have gone 6 or 9 months earlier, and maybe I overlooked some symptoms and stuff because all that was going on.
Symptoms worsened
Finally, we’re on vacation and I started passing blood, and it wasn’t just a little bit on the paper. I’m seeing it in the bowl. In the beginning, when I would see those little spots, it was mostly on the paper. I would wipe, I’d see some and [I’d think] I’m wiping too hard. August 2021. [I started thinking] oh, that doesn’t look good. And man, I’ve been feeling really crappy lately. That was kind of how it started for me. I was feeling really run down.
However, also in 2021, I started my own company. February 2021, I started my own business and I’m running like the devil all summer long. I’m taking on every job I could find trying to survive. Even though I have many years in my industry, I’ve always worked for someone. This is really my first time where I went on my own and said, I’m going to work for him and him and him and him and him. That whole year, I was running like the devil. Then I’m feeling run down. Now I’m passing some blood. I should probably go to the doctor. Maybe something’s going on.

I don’t remember if I told my wife about the blood. I think I just told her I was having a lot of GI distress because I was kind of embarrassed. It’s not really the kind of thing that fosters intimacy when you’re on vacation with your wife in a nice place. I tried to hide that, and I feel horrible. It didn’t make any difference to my ultimate diagnosis. It wouldn’t have mattered had I said to her, “Hey, I have blood in my stool” in August, versus when I finally got to the doctor in October. So I suffered from August into October.
The blood and stuff started progressing to the point where I was having tenesmus. Tenesmus is basically uncontrollable cramping of your butthole. It happens to radiation patients right after you have radiation, because the muscles are angry at you for doing what you do down there with the radiation. Well, I had all of that before I ever had a diagnosis. I had this problem with this cramping because of how torn up everything was. I suffered with that for a month and a half before I finally got to the doctor for the first checkup.
I covered 3 or 4 races in that span. I had all these commitments. I had committed to do things for people where they’re paying me, and that’s what’s paying my mortgage. I got to do what I got to do.
Describe your doctor appointment
I finally got to the doctor the first week of October. He did blood work. Today, I know I recognize my liver values were to the moon. I didn’t really understand what he was talking about at the time. He just said, “I see some stuff I don’t like. I’m not sure if your cholesterol medication is causing it. Come back in 2 weeks.” I didn’t really get too deep into all the blood stuff with him at that point, because it came and went. I would have 4 days where it was horrific, and then I would have 3 days where it was okay and I was all right. I go back for the second amount of blood work 2 weeks later.
A friend had colorectal cancer around this time
Now I’m going to bring someone else into this very quickly. I had a friend, Clarence. Clarence is a fellow photographer. Toward the end of this season, we had commiserated about how terrible we were both feeling. He was about 10 years older than me. To make that very short, during the time period I’m talking about, everything happened from a CT scan to a biopsy to a colonoscopy to an ultimate diagnosis.
All of those things occurred for me between October 14th and December 5th. Let’s include the port also in this time span. I got all those things, ended up with a diagnosis, had a port installed. I’m sitting in the chair on December 5th which is the day that Clarence passed away from colorectal cancer. Like I said,, my story is bananas. I haven’t even gotten into the two HAI pumps yet. I’m now sitting in the chair for the first time. I have watched Clarence basically pass away through Facebook Messenger from all of my friends who are talking with him and talking with his sister.

Today, I sit on the board of a nonprofit that his sister runs in his memory. Clarence is a very big part of my story because we were photographers together. When I went to the racetrack where he was the staff photographer, I parked in his spot so nobody else could park there. When I get into the media room, I’m the first one in there because I’m the one who works for the racing series. Clarence and I typically have about a 30 minute conversation in my head before I ever start working, because we talk about how lucky we are to be here again.
Diagnosis
Beginning chemo
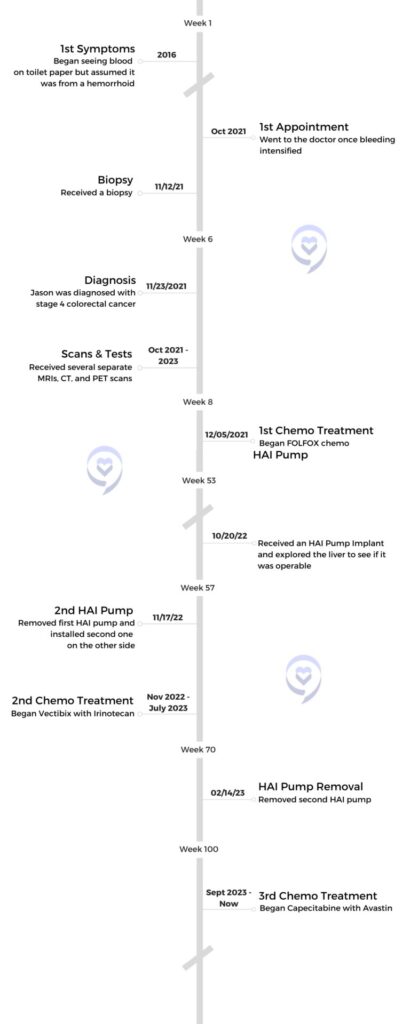
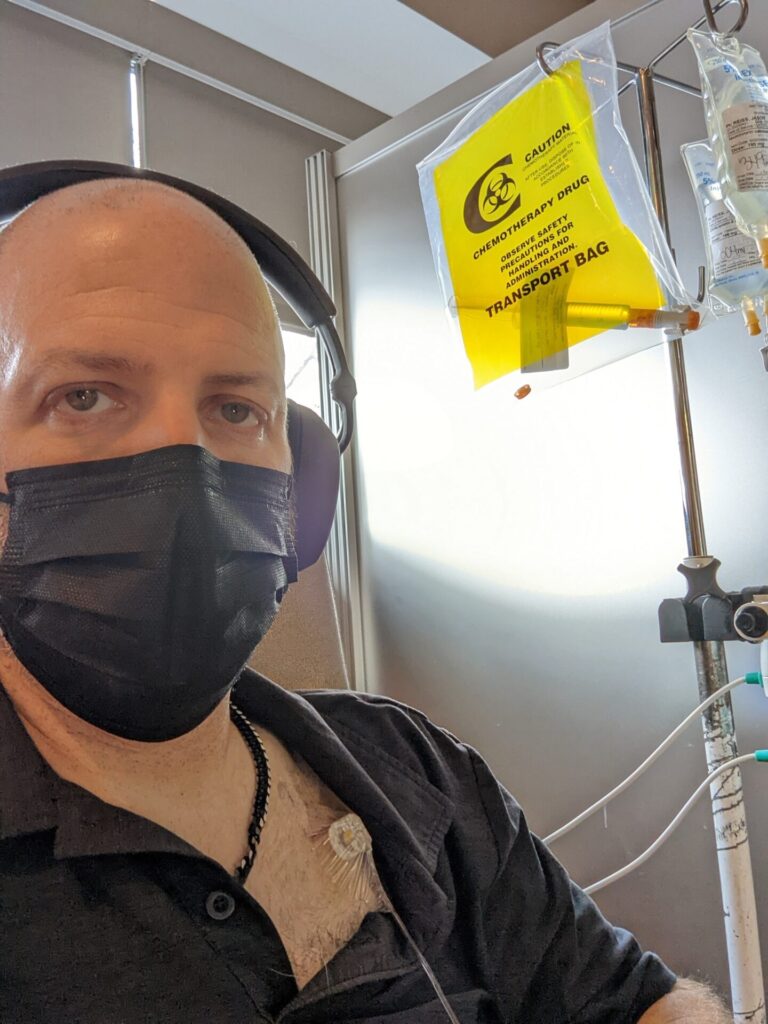
I liken the beginning of the cancer experience to being forced to learn a new language without a teacher in whatever your quick time span is. I was diagnosed, I had an official diagnosis on November 23rd. First chemo treatment on December 5th.
When you go in for your first chemo treatment and they talk to you about all the drugs and stuff they’re getting ready to try to kill you with, you realize that every piece of paper you’re signing could potentially be signing your life away. Everything they’re going to pump into you can kill you every time they do it. Not one time, not the first time, not the third time. You have to build up to dying from it. Every time you get an infusion, you could literally have a heart attack and be dead. You have to sign consent for all of that stuff. It’s like learning a new language.
You have all these new drugs you’re taking. You have all these diseases…Adenocarcinoma. I get carcinoma. I understand that from high school biology. Oh, well that’s what I have.
What did your doctor say after he received your blood work results?
I recall reading in that report that it said suspected malignancy or suspected metastatic disease.
Once my doctor got back the second round of blood work, he knew there was something wrong. I think he didn’t know what to say to me. He’s located almost an hour from where I live. He’s the doctor I’ve been going to since I was 15 years old. What he said to me was, “I still don’t like what I see. I think we need to do a CT scan to see if there’s anything going on inside.” At this point, I have no frame of reference for what that means. I’m thinking it’s like an x-ray. He didn’t say to me, “Liver values like what you have typically mean…” He didn’t do any of that.
Maybe he’s trying to be gentle. Maybe he didn’t want to say before he knew for sure. I’m pretty sure he had an idea. He found a hospital close to me where I could go get the CT. I go and get the CT scan. I’m not proud of what I’m going to say, but I have to say it because this is my story and I have to be honest about how everything went down.
If I remember right, I got the results, maybe in my email from my chart, and I don’t remember sharing them with my wife. If I remember correctly, and some of this stuff is fuzzy, I don’t remember telling my wife, but I think I recall reading in that report that it said suspected malignancy or suspected metastatic disease. I think that was the phrase that I saw. I’m not a stupid guy. I know what metastatic means. I know what disease means. I think that was when I started spiraling. Everybody does it. I know now that everybody does it, and nobody’s immune. You do what I call turtling up. You dive into your shell and you find the thing that keeps you going day to day while you figure out what the heck is going on.
That’s when I started to spiral, because at the same time, my symptoms were back. The tenesmus was very bad during this period. I was spending 4 hours a day sitting on the toilet just bleeding, not really going to the bathroom, just bleeding. It was horrible. After the CT scan, I read that. Now all of a sudden, instead of me begging for appointments, they’re calling me. “We’re going to schedule you in for a biopsy after the CT scan,” but nobody really told me what they were looking for. At least I don’t remember that. They may have said something to my wife. Ultimately they did a biopsy of my liver next because I guess whatever they saw in the CT, they were like, well, his liver is effed.
What were the results of your further tests?
Knowing what I know now, seeing my original scan photos and understanding what I’m looking at today compared to before [the] diagnosis, they probably took one look at my liver and said, “This guy is fucked. There’s not going to be anything we can do for him. Let’s do a colonoscopy and confirm it but it’s what it is.” That’s what I think the doctors are probably thinking, but nobody’s saying that to us.
We do the biopsy. Again, I got the results and at that point, I didn’t know how to link [my wife] in so she could see my MyChart stuff. I’m getting the results and I’m just like, I don’t know how to read this. We should wait for the doctor. Then the phone call came from the doctor on the 23rd, “Sorry to tell you. This is where we’re at.” If I remember correctly, the doctor who told me that on the phone was the guy who read the biopsy report. I had never spoken to him before. He had never consulted on my case. I think he was just the attending doctor at that time.
After the biopsy, they right away scheduled the colonoscopy 4 days later. I go for a colonoscopy. That doctor wakes me up and says, “I can confirm that you have cancer. This is where it’s from. It’s in your rectum. We’re going to do everything we can for you.” Obviously that’s devastating to anybody.
Finding strength to keep going
Seeing how people react today, knowing what I have been through, I see why many people refuse [chemo]. Maybe they’ve had a family member who’s been impacted and they’ve watched some of the crap that I’ve gone through, which is insane. I don’t know. I just know for me, like I said, I have all that awesome shit going on and I’m not done. I didn’t work this hard to get to the pinnacle of my career to give up because of this.
I’ve slept in my car to cover races before, driven overnight all night after working all day, being up 24 hours and sleeping for 3 hours in my car outside the gates before they open. I lived in somebody’s motorhome for 6 months, working. I will sacrifice whatever it takes to continue to be here and if that means surgeries, it’s what it means.
I have a different perspective, and I’ve had a lot of this since the beginning because of my heart attack. I already had this massive traumatic event that should have killed me because I laid on my bathroom floor for hours having a heart attack before I realized what was happening and managed to get up and get to the hospital. I’ve already had 12 bonus years whereas, when I was first diagnosed, it was 10 bonus years. Since my heart attack, I’ve always lived as if tomorrow could be it because it could be it. I had a much closer view of that than most of my friends did. I’ve lived the last 12 years of my life in a very different fashion than in the beginning. I have so much to live for. It’s going to have to go insane and crazy in my body and take me down, because so far it’s been trying really hard and it has not done that.

I’m not done. I didn’t work this hard to get to the pinnacle of my career to give up because of this.
Researching and understanding your cancer diagnosis
My initial diagnosis came from Dr. Z. He’s a couple years younger than me. Very personable guy. Very good oncologist. What he said to me at the beginning was, “You’re most likely going to be on chemo for life. We’re going to do what we can for you. If you had waited 6 more months, I wouldn’t be able to help you at all.” If I remember right, that was like our first meeting or our second meeting he said that to me. While it’s hard to hear that in the moment, I believe I have enough self-awareness to be able to [say], okay, that fucking hurt. But I see what he’s saying. My condition is very poor. It’s going to be what it’s going to be.
At this point, all I can do is succumb to what they offer me and hope it helps. I did a little bit of reading on my own at the very beginning, and then I realized that was a poor idea at the very beginning. The type of detail oriented person that I am, I will be in the weeds where I’ll be teaching [doctors] stuff. So I didn’t do that.
I tried to focus on what I knew were the big words, so that I could look those up and understand what they were talking about, without having to dive into the details. I knew the details would come. I just tried to navigate it the best I could. For me to absorb something like this, I have to break it down into chunks that I can absorb. Sometimes they become really small chunks, like single words. Adenocarcinoma, suspected metastatic disease. Because I’m a writer and because I’ve been an editor of other people for many years, I can look at the report and figure out what I’m looking at and have a decent understanding without having to read the whole thing.
Treatment
What chemo treatment were you on?
He said “most likely, you’ll be on chemo for life.” So far, he’s been right. I’ve had a little break here and there. I’ve been on chemo pretty much since we talked. At first it was FOLFOX, which is what he put me on. I was on FOLFOX starting December 5th of ’21, and I had 16 full strength treatments, which was a very bad idea.
Dealing with neuropathy
I did not understand what neuropathy felt like. I probably should have told him much sooner that I was having issues. Part of the challenge, and this might sound crazy, is that right when I started chemo, I bought all new socks. I kept thinking that the feeling I was feeling under my toes was my new socks bunched up under my toes. It’s actually the underside of my toes being deader than a doornail. Lesson learned. My toes are pretty much numb. I have some feeling in my big toes. I have some in my hands.
I did do icing where you cool your hands and feet down. However, I didn’t necessarily understand what I was trying to achieve with the icing. I used frozen water bottles because they would stay cold much longer than the gloves you could buy. I bought cycling water bottles and I was holding them and resting my feet on them. Well, the soles of my feet are fine, but from the balls of my feet forward where I didn’t use the ice, that’s the part that’s numb. Same thing with my hands. My palms are fine, and up to here pretty much is fine on each hand, but the ends are starting to become dead because I didn’t chill that area enough. Knowing what I know today, I would have handled the cold items much differently to target the proper areas that are really going to get the terrible neuropathy.

That experience is helpful to me when I talk to patients who are behind me. I get a lot of that because I’m one of the administrators at Man Up to Cancer’s Facebook group. I’m a pretty large part of what we have going on. I’m trying to advocate for myself, but also helping many, many, many new patients who come in who have all these questions about all this crap that I’m talking about. What’s going to happen to me? Well, get yourself some cycling water bottles, but make sure you hold your fingers on them and not your palms. Put your fingers on them and freeze your fingers. Freeze your toes.
That’s the stuff you need to keep nimble. Especially for me as a photographer and a writer. It’s a little discouraging to have so much numbness, but I just pushed through and it’s what it is. They work. They’re just a little more fumbly than they used to be.
It takes longer to put buttons on if I’m buttoning up a shirt. Stuff like that, but I can still do all the things I need to do. I started with FOLFOX.
What led you to want an HAI pump?
Through Man Up to Cancer and one of my friends who I’ve met there, Mike, I learn about the HAI pump. I go to treatment and I say to my doctor, “Hey, I have rectal cancer. That’s to my liver. That’s what they use this for.” “They don’t use that anymore. That’s an old technology,” is what he tells me. I’m like, “No, doc, my friend just had this done. He has one in his body.” [He said], “No, no, that’s old. That’s not going to work for you.”

I won’t say I took him at his word because I realized that he didn’t understand what I was talking about. He did what many doctors do, which is they try to bluster you into thinking they know because they don’t want to appear that they don’t know. I know at this stage of my life that it’s okay to say, “I’m not really sure what that is. Let me find out and then we can talk about it and see if it’s right for you.” Even though he didn’t do that, I’m not mad at him, I understand. At the end of the day he’s a guy trying to do his job and go home to his family. He’s doing the best he can. He probably sees a lot of people who die. I get it, I’m not mad. At that time I was a little mad, but today I have a different perspective.
Describe your experience getting an HAI pump
He told me this thing didn’t exist, so I started researching where they would do this type of stuff. I came across the NCI center where I live. I go to the University of Pennsylvania and I discover that the technology was really pioneered by somebody at MSK. The gentleman who does it here at the University of Pennsylvania trained with that person. Well, the University of Pennsylvania is 20 minutes from my house. I’m going to set up an appointment with this guy and see if I could do this. Regardless of what my other oncologist says, this guy’s a surgeon. Maybe I’m eligible for this thing.
He says, “I want to operate on you. You’re in great shape. You have no other stuff going on,” so we schedule it. We’re going to put in an HAI pump. I wind down my FOLFOX treatment at the other hospital and switch all my care to Penn. I had a little bit of a chemo break there at the end of that summer because I had to be off before he could cut on me. I was on Avastin with FOLFOX.

On October 20th of 2022, a year and 2 months ago, he put in the first HAI pump. A couple of days later, a hematoma formed on top of it. There was so much pressure that the incision popped open. We fought for a month to try to get it to heal. I went to him on November 16th, a little bit less than a month later. I went to him for an appointment so he could check it out, and he says, “I want you to come back tomorrow. I’m going to put you under and I’m either going to wash it out and stitch it up so that it’ll heal or I’m going to take it out, and I’m going to put in another one on the other side. We won’t know until I start what I’m going to have to do.”
I have to just submit to that. He just did this surgery. He opened me up straight up and down. My abs are still healing. I got this problem with the hematoma, and I’m bleeding and bleeding every day. Long story short, I go on the 17th. I wake up on the 18th with a new pump on the other side. That’s what he felt he had to do. He glued me shut again.
Side Effects

The incision opened a second time
Not long after that, it opened up again. We fought and fought and it was almost closed. I’m not sure what happened, but it opened back up like this wide. It was almost done. He put it in on November 17th. End of December, it was almost finally healed up. I don’t know if I maybe shifted wrong and it twisted and I bumped it and it opened. I don’t know if maybe I went to put my shoe on and my thigh bumped the bottom of it. It was very tough for me because I’m very lean. I don’t have any stomach fat to put it in right. I don’t have a lot of [pinching stomach]. There’s nowhere to put it.
The first one was over here [touches scar on left side of the abdomen]. This one didn’t heal at the same time as when this incision was made [points to scar in the center of the chest and abdomen], because they have to get to the artery for the liver that way. He was also looking around to see if I could be resected on that day. That incision goes from here [points to the bottom of the center of the chest] and it ruins my belly button. My belly button used to be a perfect circle. It’s not anymore.

Then he did this one a month later [touches scar on right side of the abdomen]. It didn’t heal properly, so at the end of December, now I have this incision and it’s open an inch again. Well, not only is it open by an inch, but you can see the pump inside me. The pump and the catheter. You can see a little bit of the pump sticking out of the thing. While all of this is going on and I’m dealing with this crap, somehow I still managed to convince them to pump the drug into the pump. They put a treatment in the first one while we were battling that because we thought we were going to be able to fix it. When that didn’t happen, they put in the second one and it was healing. Then we did the first treatment, so now that made two and then I think we did one more maybe. Before we did the third one is when it popped open again.
Did you let your doctor know the incision had reopened?
I knew if the doctor saw how bad it was, he was going to try to take it out, because I knew that I wasn’t healing properly. I’m on chemo. I’m on irinotecan and vectibix while this is happening. I knew he’s not going to do anything. There’s nothing he could really do to help it. I had a home nurse helping me to manage the wound. She was packing it with some Aquacel, which is like a silver infused cloth that helps you heal more quickly. She was packing it with that. She was here like every 3 or 4 days.
In an attempt to keep it from popping worse, I was only showering right before she came so that it had 3 days. I literally laid on my couch for weeks. I would wake up, I would lay there, I would eat breakfast in that spot. I’d watch TV all day in that spot and go to the bathroom once. Literally, I just laid on the couch in the same position for weeks at a time because the location when I showed you where those cuts are, those cuts are also right at the base of my ribs, which is where your body flexes when you bend. So every movement I’m making is just another movement that’s preventing it from healing.
Today, I can look back and say, “Doc, you probably should have stitched or stapled me shut.” It’s not his fault. I’m not mad. It’s what it is, but I managed to get two more treatments of the drug, because I discovered how to palpate the bump where they would fill it, and I would bandage myself in a way that all they had to do was just stab me in the bump, and they would never see the incision to say, “Yo, bro, we need to take this out of you right now, because maybe it’s infected.”

I didn’t care because I knew in my heart that that drug was the only thing that was going to get my liver to a point where I could maybe live through this. I got 3 and a half treatments of the drug before they finally took it out. Every time we check my liver, all the values are in the green for someone who is perfectly healthy. Did that do it? I don’t know. Had I given up earlier, would it have impacted me? I’m pretty sure it would have. I fought and fought and fought until I could see the edges of the incision getting red, and it felt kind of stingy before I said, “Hey, doc, I think we should probably take this thing out right now.” And he did. He took it out on Valentine’s Day, so now I don’t have either one. It’s supposed to be in there for, pretty much, life if you get to that point. I don’t have either one of them though.
Did you have any additional side effects from cancer treatment?
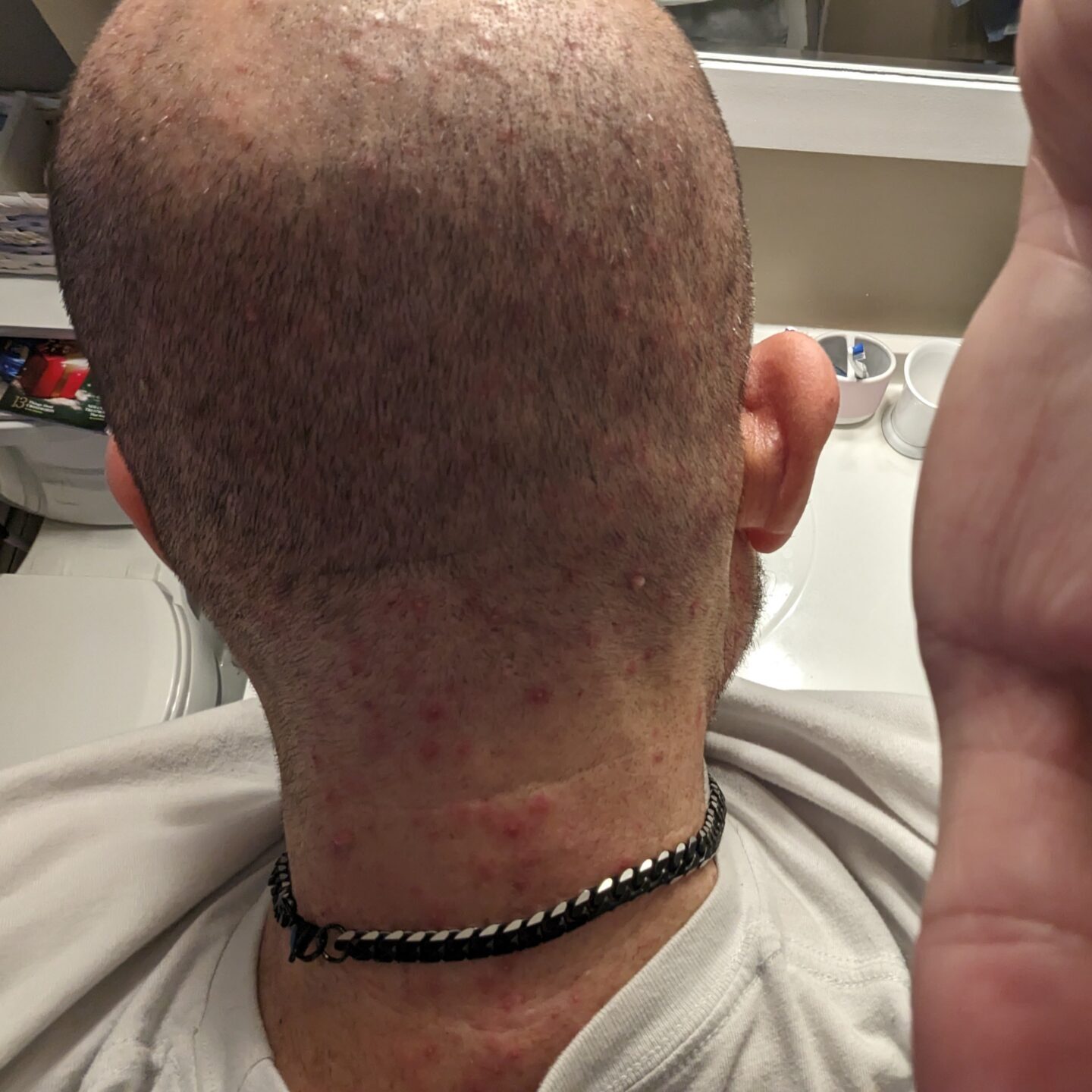
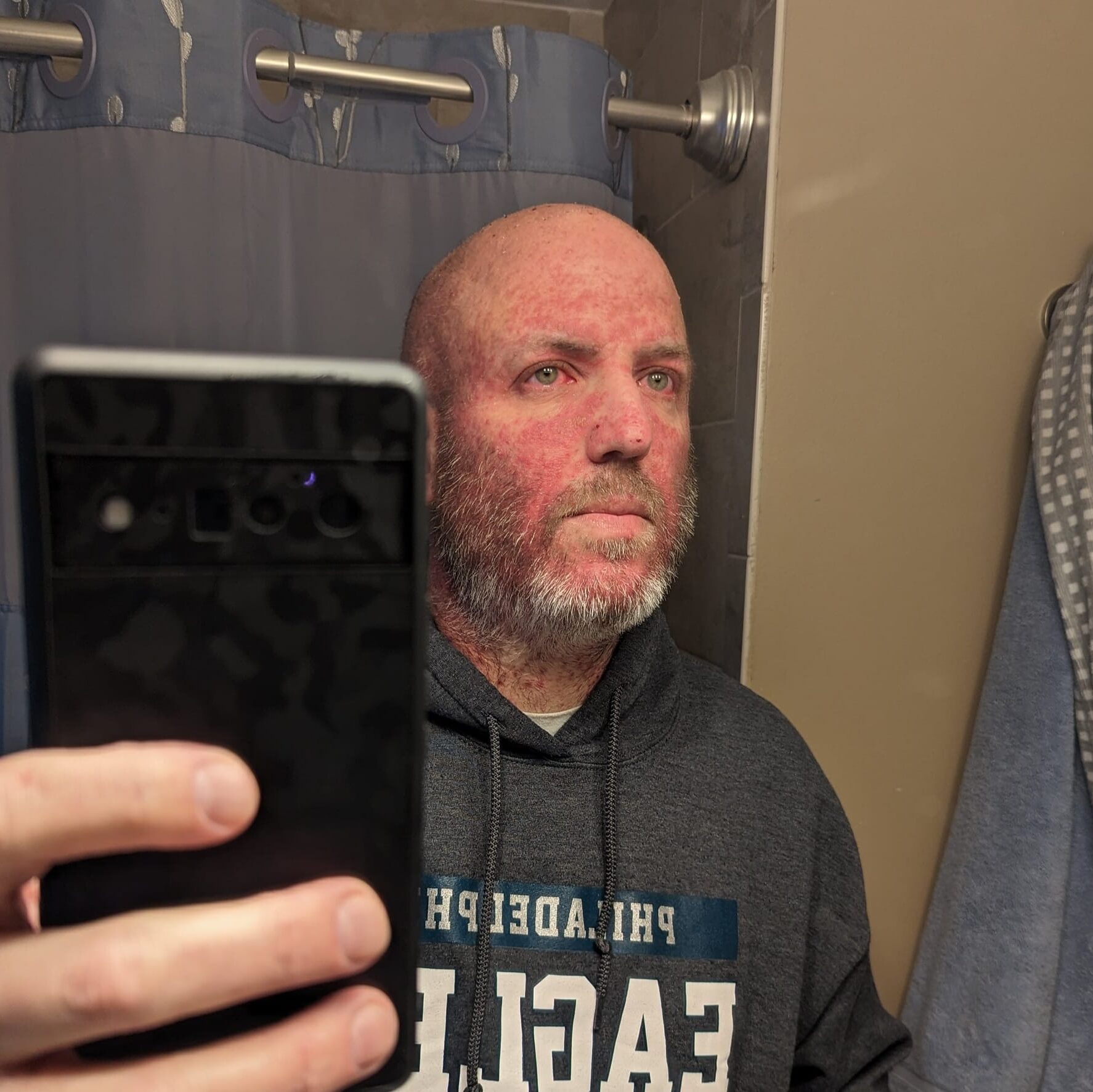
To make my story much shorter, in conjunction with the pump, they were doing vectibix and irinotecan. I had all this skin stuff going on. My chest broke out. Basically, from the waist up, I was one giant 14 year old pimple. It was behind my ears. It was in my neck. It was in my ears. It was in my nose. It was horrible. I was on that during all this stuff with the pump. I was on irinotecan and vectibix until June.

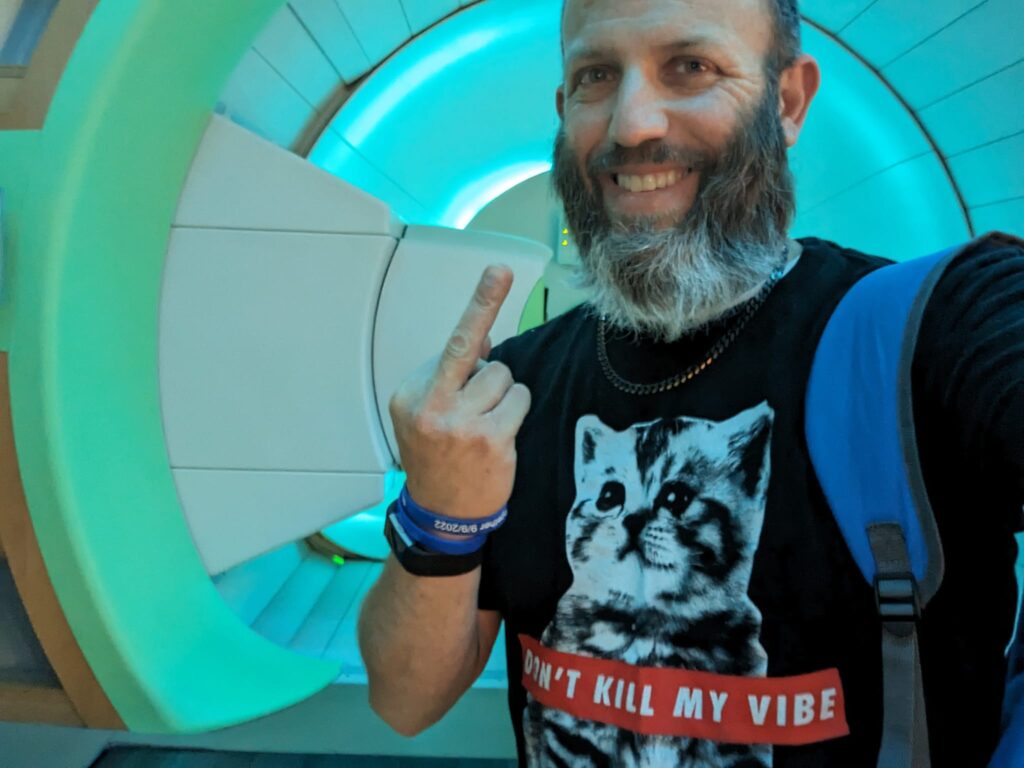
In June, we decided it was time to look at radiation for my primary tumor, which is still right where it was at the very beginning of all of this. It’s still there. I’m sitting on it right now. I did irinotecan and vectibix. Then we did 28 radiation treatments. I do not recommend them to anyone because it fucking hurts. The first 3 weeks were okay. It was the last week. All the fatigue kicked in and I was dead for like a month. I just laid around the house.
I had trouble going to the bathroom. I found out later from my surgeon who’s hopefully going to be cutting on me, that I had a fissure that I was unaware of. That was adding to the pain and the difficulty that radiation causes. There would be times going to the bathroom where I was in tears, like literally just screaming and crying in the bathroom. I had to yell at my wife to go downstairs. I didn’t need her to hear this. It’s just horrible stuff.
Considering a colostomy
Radiation is over. As I mentioned earlier, I’ve had the most normal bowel movements that I’ve had in the last 2 years. In the last couple of weeks, I’ve continued to heal from radiation. My next step is going to be a colostomy because my tumor is right above the top of the muscle stack, I guess. I’m not sure of the terminology, but my tumor is right at the top. I’m not sure whether they could reconnect me afterward.
Based on the fissure pain that I’ve had and all the other pain that I’ve had, I’m very inclined to just tell him to sew me up and do an APR and make it permanent. Not only because it relieves me of all that pain and stress, but because if I take the chance of doing the reconnection and end up being one of the people who struggles with frequency or urgency – urgency more than frequency – there are times when I’m on the side of the racetrack and I can’t get to the bathroom in 2 minutes. I’m not prepared to crap myself on the side of the racetrack in front of 4,000 people.
One and only one time, I had an urgency issue not long after radiation was complete. I was standing and doing the dishes. I farted once, and I thought, oh, I should probably get the dishes done so I could go to the bathroom. I farted again and I went, oh, I should probably do that right now. I turned around and I went, oh, I’m going to do that right now. I literally dropped my drawers and crapped into my hand in the middle of my kitchen. So an ostomy, for all of the challenges that it can bring, actually sounds kind of liberating and nice given all of the pain.
»MORE: Navigating Life with an Ostomy

The last 2 years of my life have been dominated by thoughts of how my GI is going to act or react to a stimulus, a food, or not enough water. It sounds very, very nice to think about the fact that maybe just taking care of a bag every other day, once you figure it out. I know there’s challenges to figuring it out but the consistency, the simplicity, mostly the consistency and the lack of worry.
I want to continue to live my life as long as I can. Maybe they take that out, and then I find a liver transplant and I become NED, and I’m good for another 20 years. I’d rather live that with a bag than I can’t go work for the next 20 years. Who’s going to pay my mortgage? I don’t have savings. The kind of job I have is not exactly the kind of job where you’re making enough money to save plenty of money for the future. It doesn’t really work that way. It’s what it is. But it’s like I said before, it’s been a crazy ride.
Preparing for surgery
I was supposed to have Avastin last Wednesday and they canceled it to get me off in preparation for the surgery. I had a consultation with the surgeon. We discussed it. I told him what I was interested in, which is what I just told you about. I need to be able to manage this consistently above all else. I don’t care what I look like. I don’t care if the bag sticks out of my neck. I gotta live my life and I have to be able to do that consistently. He’s the second surgeon we saw.
The first surgeon was unwilling to do anything so my oncologist recommended this gentleman who is also at my hospital. Other than my NP that works with my oncologist, he’s the only doctor I’ve had so far who’s actually asked me a bunch of questions. How are you feeling? Why do you want to do this? What do you think is next? What are your goals? Where are you trying to get to? He’s the first one who took an active interest.
BYOL: Bring your own liver
Remember I said before that I had to teach my doctor stuff? Well, I taught my first oncologist about the HAI pump and about the icing because he didn’t know that was a thing for anybody but breast cancer patients. I taught him those two things. We fast forwarded to the last couple of months. Six weeks ago I had an appointment with my current oncologist, and I brought up a program to him that they do at the University of Rochester, which is what they call a BYOL: bring your own liver. I would find my own donor once my primary tumor is gone. If I have no spread anywhere else and I get a new liver, theoretically it won’t come back.

I have a friend who’s had this done at this hospital. I go in and I say to my oncologist, “Hey, you need to get the primary out because this is the next step.” He says to me, “You can’t get on the list.” I said, “Doctor there isn’t a list for this. You bring your own person.” He said, “That doesn’t exist. You can’t get on the list because you have cancer.” I said, “Doc, I’m telling you this exists.” He said, “No, it doesn’t.” I left and I’m not mad because I know that I’ve planted a seed because of what happened with the first guy.
I go back 2 weeks later for treatment, and I’m sitting in there with my NP. I see her every time, unless it’s right after a scan. The first time was right after the scan. I’m ready to talk about doing the surgery to move forward. We’re in there for 15 or 20 minutes. She’s talking about side effects and we’re just chatting. He pokes his head in and he says, “Remember that thing you asked me about the last time – the bring your own liver deal? We’re in the middle of doing that here.” Two thumbs up, doc. I’m glad you figured it out.
But at this point, my intention is to be one of the first people on that table for that. I have to get the primary tumor out, then I have to figure out what are the requirements, and then I will go find someone. I don’t care if I have to walk every street in this country and knock on doors. I will find someone who will be willing. I have many friends who have told me, “Just tell us what’s needed and we’ll all go get tested.”
My industry attracts people who are very wealthy because it’s a hobby for them. Think of what it costs you to buy a car. Now think of racing a car and how bad that’s going to beat up the engine and the transmission and all the other parts. It’s a millionaire’s hobby in most cases. I have some friends in that club that are very kind and generous to me. They will go get tested. These are people who are public figures-ish [who’ve said], “I’ll go for you. I’ll do this for you. I don’t care, just tell me what I need.” Fingers crossed that’s where we get. That’s the hope. That’s the goal.
Reflections
Showing gratitude

I’m not sure what day today is, but last Thursday I think was day 751 since I got that diagnosis. Remember, he told me if I waited 6 more months, there’d be nothing he could do for me. We’ve now clocked 2 years. I actually sent him an email on the anniversary of my first treatment and said, “Hey, doc, today is the second anniversary of the first time you treated me. I’m very thankful that you gave me the care that you did because I’m still here.” He hasn’t responded, but I sent the email because I’m very, very grateful that all of these people have taken an interest in getting me to this point. Hopefully we’ll get to the next point.
What cancer treatments are you currently receiving?
Every 3 months we do a scan because I’ve been on a different treatment right now than I was on before. Before I was on capecitabine when I was getting radiation. I wasn’t getting Avastin at the same time, but once the radiation ended, they kept the capecitabine. They took it from just radiation days to 7 days on, 7 days off, and now you’re taking twice as much. Then they add in the Avastin. We’ll scan again in January, which was scheduled anyway.
Before I got to the surgeon, that scan on January 2nd or 3rd was already set. Once I went to him, he said, “Okay. Well, you have a scan coming here. That’s right around the time where I’m going to be ready if you stop doing Avastin on this treatment.” So that’s what we just did. We quit Avastin. I see him on the 9th.
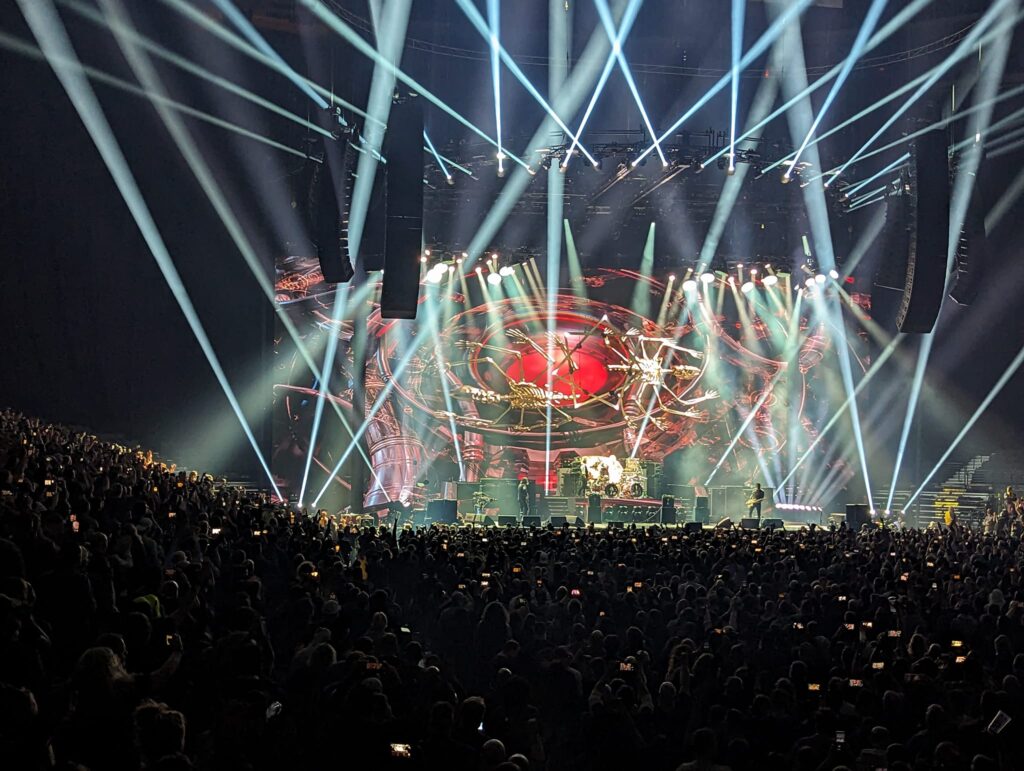
I know he’s not going to cuddle me that week because I have concert tickets for the 10th in Baltimore and concert tickets for the 12th in New York City. Same band, two different places. My favorite band. I’ve already seen him 4 times on this tour. This will make 6 and he can cuddle me the next week, but I’m going out with those two good memories of being in arenas I’ve never been in before, seeing my favorite band with new people both times. Then the surgery is going to be what it is. The next step is going to be what it is, but I can’t control any of that part. I can just get to that point, hopefully.
What tips do you have for someone getting a colonoscopy?
That’s the real trick for the colonoscopy. If it has to come out, think about what you’re putting in a couple of days before.
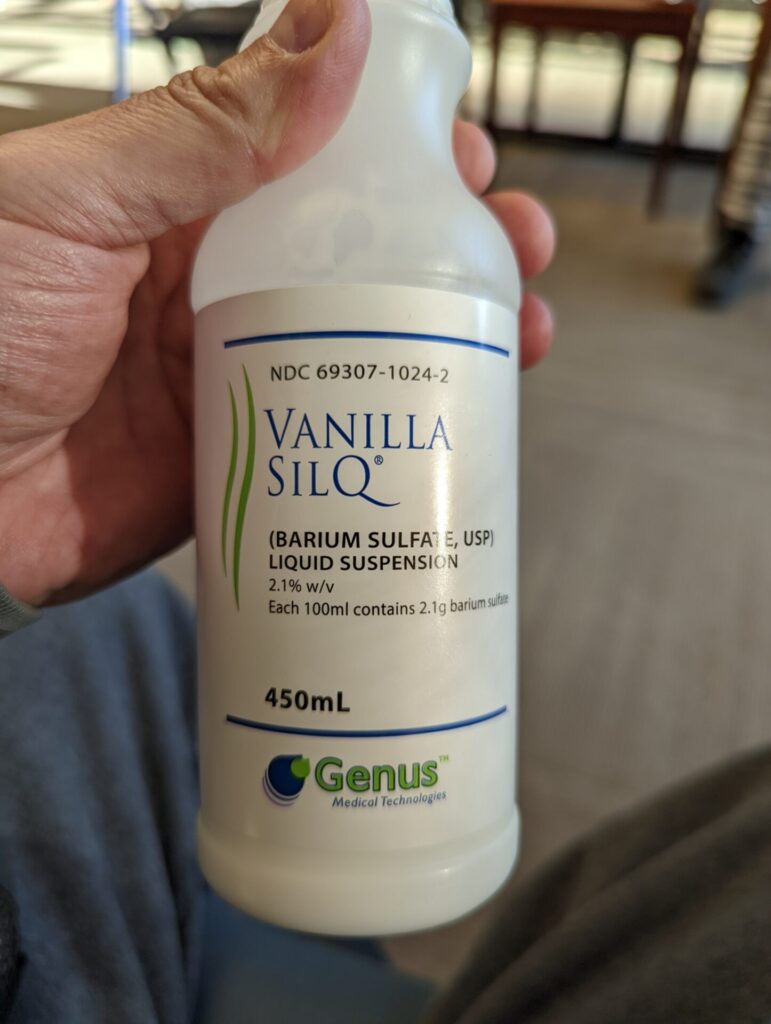
When I went for my first colonoscopy, I had no idea what to expect. All I know is I’m already dealing with the biopsy and all the other stuff and they say you have to go for a colonoscopy. Here’s the instructions. The instructions say to buy Gatorade, buy Miralax, Dulcolax I think I took also. There’s this cocktail you mix up. Don’t buy anything with red #40, green #12, whatever it says on the instructions. I went to the store and I proceeded to spend $100 on Gatorade and all this other garbage. Half of which I didn’t realize had the red in it.

But my tip for the colonoscopy, remember that everything that goes in has to come out. In the 3 days leading up to your colonoscopy, when you have to prep on the last day, if you eat a porterhouse and then you eat 30 wings, that’s going to feel like death on the way out when it’s forced out by the laxatives that you’re taking to make the process work. If you go, have eggs and French toast, maybe a turkey sandwich for lunch so you get some protein, maybe a protein bar, because that’s not going to be a giant piece of meat that your stomach has to digest. Pasta, stuff that slides in and slides out is the easiest way to explain it.
That’s the real trick for the colonoscopy. If it has to come out, think about what you’re putting in a couple of days before. Eat a couple bananas. They’re nice and healthy and they’re going to pass real easy. Maybe a prune or 3. If you clean yourself out before it’s forcibly cleaned out, there is no, “Oh, my God, this is so horrible. I’m in the bathroom all night,” because you blow it all out and it’s all gone. That’s the real trick. Once I tell people that, they’re like, “Oh my God, it really wasn’t that bad.” I told you it’s not going to be that bad. You have to listen and actually do the things.
»MORE: What It’s Really Like To Get A Colonoscopy
What advice do you have for someone who suspects they have colorectal cancer symptoms?
The first one – it’s one of the hashtags that I use every time I make a post about my cancer. Because every post that I make is public, people who I don’t know have seen them and sent me messages saying, “Thank you for talking about this. You made me go to the doctor and I’m clean.” This happens regularly so I just continue to make them all public.
That hashtag is #GetYourButtFingered, please. It’s not something to be ashamed of. We all have buttholes. We all fart. We all poop. Some of us get diseases, and it’s completely curable if you don’t ever get to the point where you have it. If you have stage 1, they can get it out of you and you don’t end up like me, turning 50 in 10 days but staring at the end of my life at the end of my hat. Please just go to the doctor if you have any poop weirdness. Weird shape, weird smell, weird color, weird anything. Any kind of blood on the paper. Any kind of blood in the stool or in the bowl. Any kind of pain. They can fix you, especially if you go before you end up like I do. Please, just go to the doctor.

Send me a message on social media. I’m very easy to find. If you have questions or anything at all, anything I can do to help. Anyone who is at this point, 45 years or older, make an appointment today. If you’re under 45 and it runs in your family, make an appointment today. Even if it doesn’t run in your family and you’re under 45 and you have poop weirdness, tell them it runs in your family because they can’t fucking check your family history. Just tell them you have a problem and go to the goddamn doctor. You can call me before that, but please, go to the doctor.
It’s so important and it’s so easy. It’s 20 minutes of your life. I can give you tips on how to make the colonoscopy easier so it’s not sucky like many people go through. Just go to the doctor. 20 minutes, it’s over and it’s a great nap. You wake up and you can go get chicken nuggets, fries, and a big soda and you call it a day. Just go to the doctor. That’s the most important thing that I could tell everybody.
More Colorectal Cancer Stories
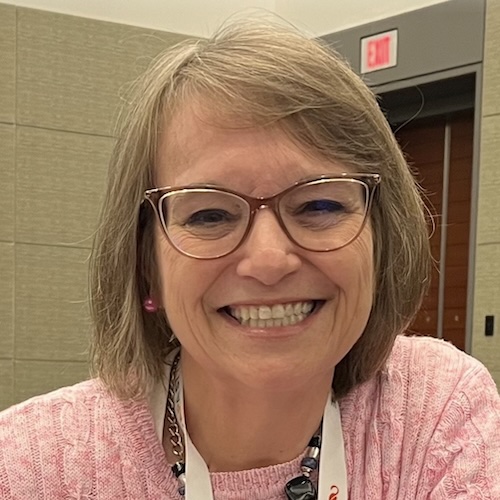
Kristie C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: None per se that she noticed; she experienced constipation and passed narrow stool, but had been experiencing constipation most of her life, and thought that these digestive issues could also have resulted from perimenopause
Treatments: Chemotherapy (including adjuvant chemotherapy), radiation therapy, ablation therapy (liver ablation), surgeries (colectomy, temporary ileostomy, ileostomy reversal, scheduled liver resection)
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy
Heather C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Severe bloating, indigestion, vomiting, rectal bleeding
Treatments: Chemotherapy, surgery (liver transplant, upcoming)