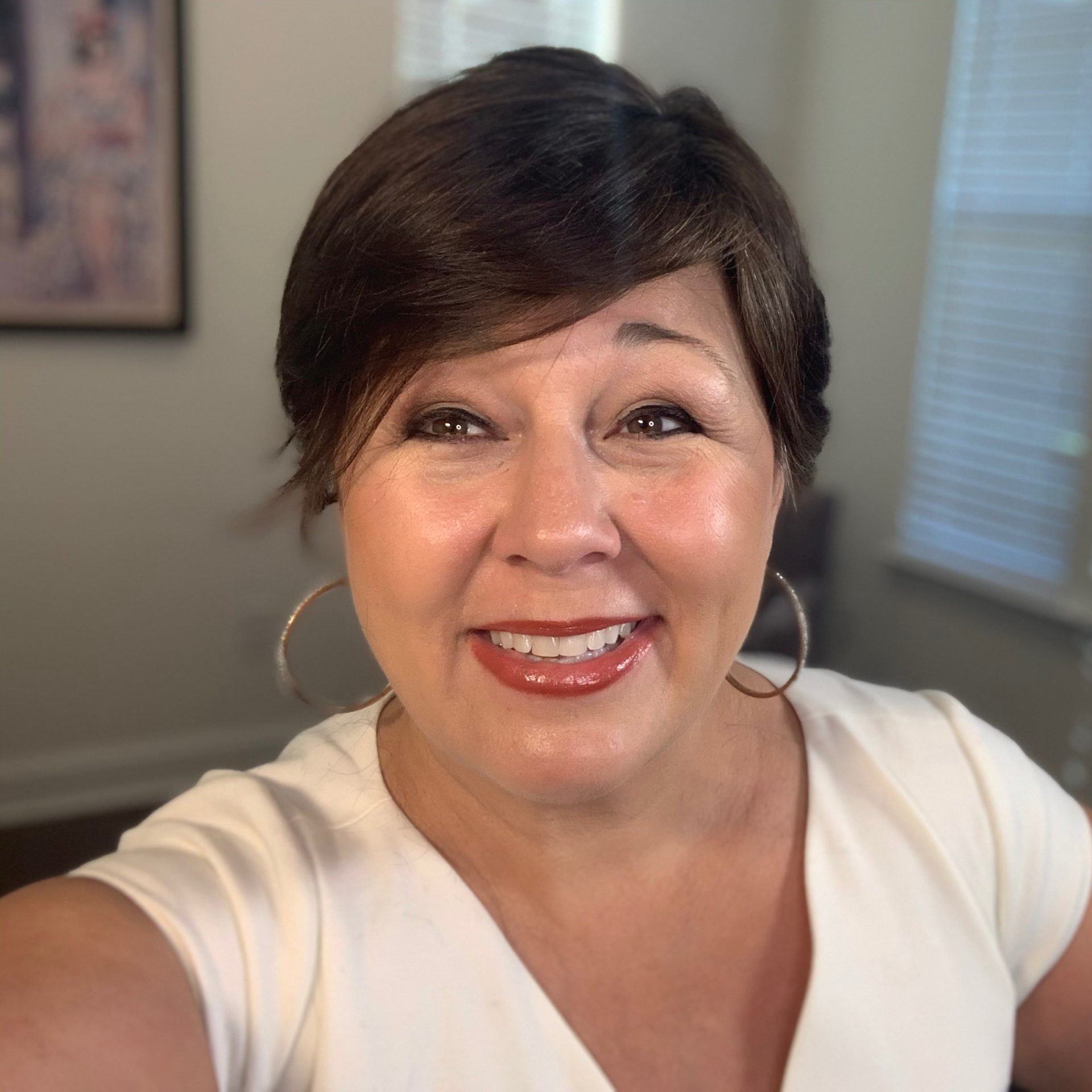
Jeremy’s Myeloproliferative Neoplasm (MPN) Story

Jeremy Smith has been living with a myeloproliferative neoplasm (MPN) for 33 years. Jeremy has both polycythemia vera (PV) and chronic lymphocytic leukemia (CLL).
Jeremy hosts MPN Forum Live, a podcast focused on sharing stories and advice from other MPN patients. He also discusses the importance of an anti-inflammatory diet, exercise, and good mental health, as well as having hope for the future of treating MPNs.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

It’s a wake-up call for you to adjust your life. You should take advantage of that because you can get too focused on all the things going on inside your body.
Jeremy Smith
Diagnosis:
Myeloproliferative Neoplasm (MPN), Polycythemia vera (PV) and Chronic Lymphocytic Leukemia (CLL).
Introduction to Jeremy Smith
Andrew Schorr, The Patient Story: Hello and welcome to Cancer Friends. Andrew Schorr, here in San Diego and living with myelofibrosis and chronic lymphocytic leukemia (CLL). Joining us on this program is someone else who’s living with myelofibrosis and CLL, and that’s Jeremy Smith, who’s in West Linn, Oregon, right near Portland. Jeremy, thanks for being with us.
Jeremy: It’s a pleasure. Thanks for inviting me on. It’s been quite a journey for me over the years. I’ve always known who you are but didn’t get a chance to really talk to you until recently, so it’s been a welcome pleasure.
Andrew, TPS: Thank you for sharing some time with us. As you said, it’s been a long journey. Jeremy, you’ve been living with an MPN, starting with PV (polycythemia vera), for 33 years. You were part of one of the original, I would say, internet patient communication pioneers, where patients started talking to patients.
As you’ve told me, these other founders of this early listserv — actually, even before we had more sophisticated tools on the Internet — they passed away. Thank God you have not.

Why is sharing your voice important?
Andrew, TPS: You’ve really been dedicated to sharing your voice. Why is that so important?
Jeremy: I think that one of the things that I learned about my diagnosis is it’s very difficult for anyone who doesn’t have cancer to understand how you truly feel. As soon as you talk to another MPN patient, there’s a bond that happens and an understanding that you don’t get from your friends or your family, as hard as they try.

I think it’s important for all of us to keep talking and learning and sharing what we know between each other, because I think it builds strength and knowledge. As rare a disease as an MPN is, it’s a very tight community, and I think that’s related to the social media connections and the ability to converse with each other.
As you start to talk to people, they do feel lonely at times. It brings people together. It’s a real learning experience for everybody, no matter how knowledgeable or what level you’re at. There’s always a big difference between the person who just got diagnosed and someone who’s been on a 10-year-plus journey.
MPN Forum Live
Andrew, TPS: That’s what you’ve been helping facilitate for others. You’ve been part of the MPNforum, which has more than 10,000 followers. You started about a year ago, after thinking about it for a long time, MPN Forum Live as a podcast. What does it give you?


Jeremy: I love telling stories, so I feel like it’s a digital book that I’m writing and helping guide people to express themselves more openly about where they’re going. For me, it feels good, because everybody’s nervous.
I would say, because of the average age of MPM patients … when you [tell] them, “We use Zoom,” they’re like, “What’s that?” Some only have 25 megabyte internet broadband. They’re not as technology-savvy as some other groups.
I’ve enjoyed the conversation and getting to know other patients more in depth than I would otherwise. If I can help them in any way understand things [or] find different doctors, then it’s rewarding to me. I feel like we have an obligation as educated patients to pass on things that we’ve learned to other patients to help them find the answers to their questions.
Importance of diet and exercise
Andrew, TPS: Let’s talk a little bit about your personal journey. Your treatment now is with an interferon. You have your highs and lows, but you’re doing okay. You’re a big believer in diet and exercise.
I think all of us want to know what we can do to strengthen ourselves for a higher quality of life. Talk about what you do and what you talk to others about related to diet and exercise and that being part of your role as a patient.

Jeremy: When I was first diagnosed, I had never heard of the disease. I was scared. As I started doing research, I found at the time — this was 1989 — there wasn’t a lot of access to information specifically on exercise and diet for MPN patients at all on the web.
There weren’t any studies. There was no fatigue study that was done later with Dr. Mesa. What I started doing was going to other cancer forums and finding out what these cancer patients were doing with really bad cancers that was different than what we were doing as MPN patients. The constant theme that came through from everything I read was diet and exercise.
At the time when I had polycythemia, I said, “I got this thick blood. What can I do to help my body recover and fight this disease?” I came up with a whole business plan that I wrote [of] these things I was going to do. For diet, the first thing I started doing was consuming large quantities of garlic because it has properties to thin the blood.
I knew that I was getting fatigued and that exercise can thwart some of that and definitely depression. Everyone goes through a phase where there is some depression — some worse, some very mild. Then you also get fatigue.
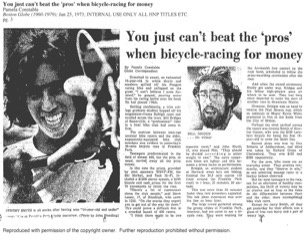
I felt that I really needed to change my program, lose weight, [and] get in shape. Then I brought exercise in, where I’d go out on 30-, 40-, 50-mile bike rides. I want to say, first of all, that I didn’t just do this all on my own. I sat down with my doctors, because you should never start any changes to your diet or exercise without consulting with your doctor so that they know what’s going on.
One of the things I didn’t know until I spoke to my doctor is that he asked me to always let him know when we did CBCs if I had exercised before or a day before. In many cases, exercise increases your white cell counts.
It’s important to know that because my white cells might bump up, and that’s either a sign of an infection or something else. There were a couple of times where my white cells went way up, and it was because I had been on a 100-mile bike ride the day before.
I combined all of those things, and all of a sudden, the fatigue was gone. I was just feeling better. I will say, one of the things that I’m most proud about is that I’ve never missed a day of work in 34 years because of my MPN.

I’ve flown probably — I know I got the 1-million mile certificate, but I’m around 1.7 million miles on planes. Although, once COVID hit, my doctor said, “You’re not flying anymore.”
I paid for a lot of my own CDC testing so that I could see if I switch to this type of diet or I moderate this, what are the results that I’m getting? I was able to track some of that stuff and share it with my doctor. Now, it’s still unscientific. I’d go to him, and he’d say, “There’s no data to support that.”

I don’t believe you should create a diet for yourself that makes you miserable.
The way they look at data is very different than the way I do or you do. For them, they’re more suspicious of what they don’t know. I did learn along the way that the younger doctors seem to be more behind the exercise, although I have to give Dr. Silver credit. He was a runner himself, so he was always behind that.
Andrew, TPS: And he’s in his 90s, right?
Jeremy: Yeah. A few of the other doctors were kind of, “Well, if you can do it and it helps, that’s awesome. Now, let’s move on.”
What do you eat now?
Andrew, TPS: Jeremy, let me ask you. I’m sure our viewers are hanging on this and saying, “Okay, so what does Jeremy eat now?”
Jeremy: I’ve had one rule, so I’m going to say this now. One day a week, I can eat anything I want, and that includes McDonald’s. I don’t believe you should create a diet for yourself that makes you miserable. If you love food, you shouldn’t start hating it. I’m more on the Mediterranean diet than anything else.
Another lesson I learned along the way is that it may not be your disease that kills you. It may be something else because of the stress on the body and how the diseases morph. I’ve had cardiovascular issues and things like that.
The head of cardiology [at the Mayo Clinic] recommended the Mediterranean diet, and that’s pretty much where I am today. It’s a diet anybody can be on and get great benefits out of it. It’s not one of those diets where you have to just eat beans. It has a very good balance, and it gives you flexibility.
I still eat a Kit-Kat bar. There’s certain things I’m not willing to eliminate. The diet to me that I would go on if I was an MPN patient — and, again, always check with your doctor — is more the Mediterranean diet or some variation of that.

Andrew, TPS: You and I both know Dr. Angela Fleischman, who’s a researcher and a clinician at UC Irvine, up the road for me. She is a big believer in the Mediterranean diet. It’s all connected in her mind — and some of the others say this, too — that what we have is an inflammatory condition.
Jeremy: Right.
Andrew, TPS: This diet can lower inflammation. Again, check with your doctor, but someone who is a very highly regarded MPN specialist, Dr. Fleischman, is doing a lot of research on this. It’s not just conjecture. There’s some thought about it, too.

Jeremy: There was a seminar back in May up at the Hutch (Fred Hutchinson Cancer Center) with a bunch of doctors that Dr. Scott led, and Dr. Mesa was there. There was an interesting doctor from Arizona who is focused on nutrition. We’re really starting to see things change. I think 10 years from now, nutrition and exercise will be a major part of MPN patient treatment.
At this seminar, she was talking about the importance of diet and exercise. I used to go to ASH (American Society of Hematology) every once in a while, and early on, there wasn’t any real discussion of diet and exercise. Every once in a while, someone would talk about it for 15 minutes.
It’s really starting to change now. I think doctors realize now that it has to be a comprehensive treatment and that food does heal the human body. The right foods, as you said earlier, are critical to reducing inflammation.
Inflammation drives almost every cancer or disease in the human body. As well as part of my diet and exercise, something I focused on is to get my inflammation down to as low as possible. I’ve done a pretty good job with that.
Importance of mental health
Andrew, TPS: We’ll all, I think, need this. I know I’m working on my diet now, and I think we all want to know what we can do on our end? Beyond the medications or shots, what can we do to put ourselves in the strongest possible position?
Jeremy: I also think — and we don’t talk about this enough — mental health awareness and treatment is very important. I saw a big shift in my attitude when I went to a therapist. I had a person that I could actually talk to about how I felt about possibly dying or my life being impacted.
I think everybody needs to have that option and consider it. I was driving my doctors nuts at one point because it was very hard to tell when I’d get sick, was it related to my polycythemia vera at the time, or was it related to something else?
I needed to calm down, and so my therapist got me to start meditating. Although, I have to say, Dr. Schrier was big on meditation. Those things are really helpful. It’s not just about diet and exercise; it’s about healing the body overall.

All of those things contribute to that and are very important aspects that all MPN patients should explore. Today versus 1989, a lot more patients dabble in some sort of meditation and alternative treatments that they take in consultation with their doctors. You have to be really careful in going off into the la la land of supplements.
»MORE: Read other patient experiences on yoga and meditation



Do you believe this happened for a reason?
Andrew, TPS: Jeremy, 33 years. Many of the people you first met in the very earliest days of the internet are no longer with us. Thank God you are. I don’t know if you’re religious or spiritual at all. Do you ever think there’s a reason? You’re a voice now. You’re a pioneer who’s still with us. It gives you purpose.
Jeremy: Yeah, definitely. I think that priorities shifted in my life. It didn’t happen overnight. It took me about 10 years to get into a state of mind where I was thinking more about things besides work, because I was an A-plus personality. My career was everything. I was missing out on a lot, but I did not know that.

I always say that an MPN is both a curse and a blessing. The blessing part is that it reminds you how short life can be. It doesn’t mean that you won’t live for 30 or 40 years with the disease, which is a huge advancement compared to 20 or 30 years ago.
At the same time, it’s a wake-up call for you to adjust your life. You should take advantage of that because you can get too focused on all the things going on inside your body.
The doctor appointments, I would say, in my mind are the most draining [because of] all the time of having to see the doctors. I kind of created my own mess by having 3 hematologists. I’m to blame for part of the problem.
Again, this is the blessing part. I think the quality of my life is better today than it was 25, 30 years ago, because I’m more spiritually in tune. I’m not a religious person. The Jewish religion is we’re always wrestling with concepts and ideas.
I wrestle with a lot of concepts. I have had some issues that I’ve dealt with my therapists on about feeling guilty. Why me? Why, out of all these other people, am I still walking upright? I think some of those things are normal day-to-day stuff that sometimes creep into the crazy mind.


Looking toward the future
Andrew, TPS: I’ve gone through the same thing. I fortunately have a wife of 37 years, who’s a great supporter. Exercise is a bit of my therapy as well. I can imagine you on that 100-mile bike ride and the cadence of it. Thoughts can be with you there, too. How do you feel about the future?
30-some-odd years. You’re doing your podcasting now, but certainly there’s an uncertainty both with the MPN, and then you have this other condition like I do, CLL. How do you think of tomorrow, next week, next month, next year?
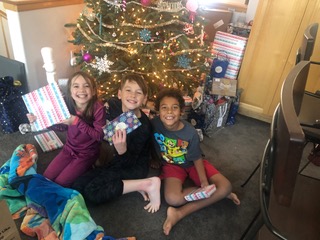
Jeremy: I do sometimes. I don’t know that it’s that productive. One of the things Dr. Schrier had me do was set up goals and write them down. I was going through a divorce at the same time I was diagnosed, and I won custody. My kids were 5, 3 and 1.5. My first goal was to see them graduate high school.
Then as we passed these goals, Dr. Schrier would have me reset them. Then we kept developing them. My goal of today is to make it to 70. My number-one goal is to have the best quality of life that I can have for whatever time remaining that I have.

I was on a 767 that almost went down over Dallas several years ago. It makes you think about, “Wow, the disease isn’t going to get me. The plane will.” I just try and stay positive. Everybody has their dark moments when you’re alone, and you’re like, “Oh, man, I got that bone pain.”
It’s not going to go away, but all you can do is give yourself the best opportunities, stay educated, [and] have good doctors, which is very critical. The top doctors have access to some of the drug development that’s going on. As an MPN patient, it’s hard not to be positive these days versus 20 years ago, because there’s so many new drugs being developed.

I don’t know — other than a stem cell transplant, which sometimes works, sometimes don’t work — whether there’ll be a cure, but I think there’ll be drugs that will allow us to live even with myelofibrosis, at some point over the next 5 to 10 years, that will allow us to live like you have PV or something for a 30- or 40-year lifespan.
I believe interferon is an important drug that can allow you to at least slow the progression of the disease down. Anything you can do that means there’s more time for you and your life, hopefully. None of us know what’s going to happen in the future. That’s a hard challenge.
You bring up a really good question. You can get sucked into the negativity of all of it, and it is exhausting. I take more pills than I ever thought I would. Then there’s the fact that I’m much older now than I was when I was first diagnosed. There’s the normal bumps in the body that you get from just being older and the aches and the pains that you would have whether you had this disease or not.
With all of those things compiled together, you have to get a reflection and just kind of take it with a grain of salt. Whatever happens, happens. I never thought I would be alive to see 5 grandchildren born into this world. I’m very blessed by that.
COVID scared the crap out of me, and I’ve made it through that, knock on wood, thanks to Evusheld. Life’s a crapshoot no matter what, whether you have a disease or you don’t. Anything can happen at any time.
I think it is important to have a positive attitude going into this. The more negative you are, I definitely believe that there is some karma out there that can make things worse if you go all dark.

Conclusion
Andrew, TPS: I just love your wisdom, Jeremy. I got to really pay attention to that Mediterranean diet. I used to exercise all the time. I’ve sometimes been tired, but maybe I’d be less tired if I was exercising. I got to work on that, and I think looking to the future.
You’ve told me you’re 63. You’re shooting for 70 now, and I wish you all the best with that. How about 75 or 80? Wherever you get, though, it’ll be a blessing. I want to thank you, Jeremy, for really being a leading voice over time and now with your MPN Forum Live podcast, which I hope people will look up, and just being almost like a catalyst or a ringmaster for our discussions.

As you said, there are all these things we can do with our doctors and our diet or exercise, but there’s also great strength in community. I know you foster that, and I’ve tried to foster that, too. So thank you. I just want to thank you on behalf of the community, Jeremy Smith. Thanks for doing that and for being with us today.
Jeremy: Thank you. It’s been a real pleasure. I appreciate you bringing me on.
Andrew, TPS: Andrew Schorr in San Diego, Jeremy near Portland. Both of us [have] myelofibrosis, are living with MPNs, and are devoted to the community so we can all do better.

Inspired by Jeremy's story?
Share your story, too!