Kris’ Stage 4 Diffuse Large B-Cell Lymphoma Story
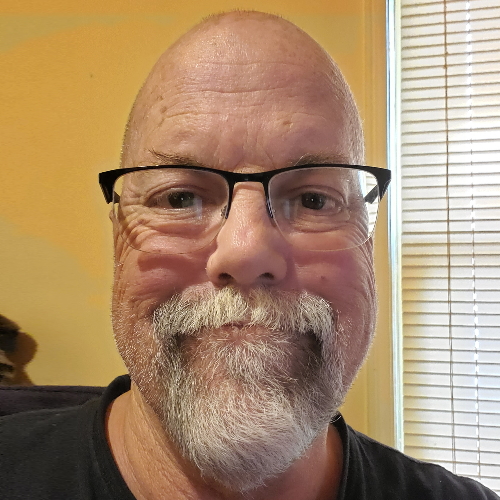
Kris was diagnosed with stage 4 Diffuse Large B-Cell Lymphoma.
He shares what it was like finding out his cancer diagnosis on his own, having to retire earlier than planned and learning his twin brother was diagnosed with cancer, too. He also shares his experience going through treatment alone, due to COVID restrictions, and what it was like dealing with isolation.
- Name: Kris W.
- Diagnosis:
- Diffuse Large B-Cell Lymphoma (DLBCL)
- Staging: 4
- Symptoms:
- Pain in the side of the abdomen
- Treatment:
- R-CHOP chemotherapy
If you even have just this remote idea that there could be something amiss inside your body, get it checked out. There’s no reason not to.
- Pre-diagnosis
- Diagnosis
- Treatment
- R-CHOP chemotherapy
- Being admitted into the hospital for treatment
- Side effects from chemotherapy
- What was it like undergoing cancer treatment during the pandemic?
- How was it like going through this experience alone due to COVID restrictions?
- How to deal with the feeling of isolation
- The impact of having to retire early
- Twin brother gets diagnosed with bladder cancer
- Getting a second opinion post-treatment
- Words of advice
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
There was pain that would keep me awake. I could sleep most nights but this one particular night, I woke up at about 3 o’clock in the morning and it just wasn’t feeling right.
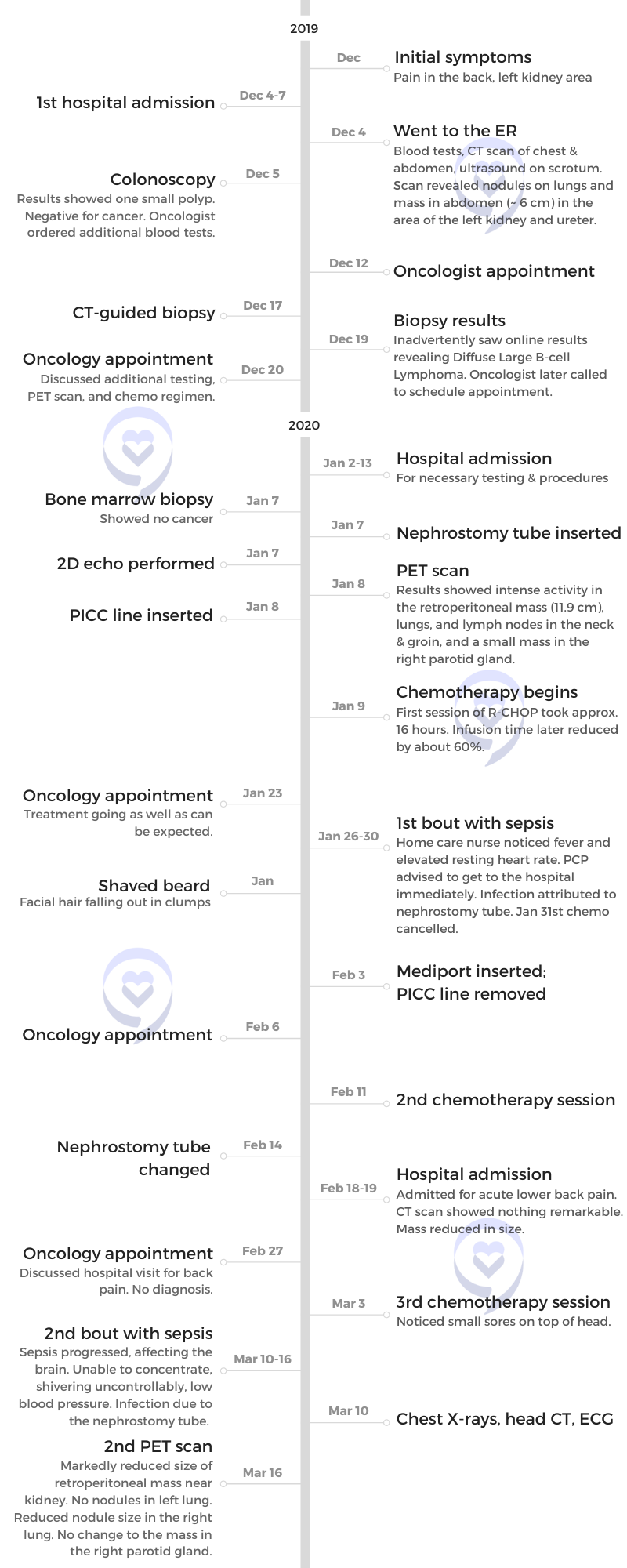
Pre-diagnosis
Share more about yourself
I was a senior developmental engineer in electronics for a total of about 40 years. Since the cancer diagnosis and the treatment, I’ve had to retire. But I really wish I hadn’t had to retire.
I have an identical twin brother and I have a sister that’s 10 years older. My brother really got me through the treatment and everything. He [drove] me to the hospital whenever I needed. I had a few infections and spent a lot of time in the hospital during the treatment. I just can’t thank him enough.
Initial symptoms
I noticed that [for] a few nights in a row, I had this pain in my abdomen and in my side. When I [lay] on that side, which I preferred to sleep on, there was pain that would keep me awake. I could sleep most nights but this one particular night, I woke up at about 3:00 in the morning and it just wasn’t feeling right.
There were some things that led up to this. Two months before, I had a blood clot in my leg and they told me, “You can’t take Ibuprofen anymore because of this blood clot. It’s going to make things much worse.”

What was going on in your head as they were performing all these tests?
When they did the CT scan, I thought, Well, that’s a little bit weird. I figured they should be able to see anything in the blood work that would have come up. But they went ahead and did as they saw fit.
We really didn’t come up with a lot other than there was a mass in there. [In] the first scan, the mass was about six centimeters in diameter or two and a half inches. They didn’t know what it was. They were thinking that they had done the surgery there, too, when I had the blood clot in my leg so it could just be a mass of blood… bleed out of the joint where they put the catheter in for my blood clot. They went ahead thinking that that’s what it was, that it was just some sort of a liquid mass and it was not pushing things around too much.
[They did additional blood work.] I think that’s where they started to think that the mass was more solid than just blood floating around.
The diagnosis was diffuse large B-cell lymphoma. That was a shock because I had heard of lymphoma before and it was never good. It was never in a good light.
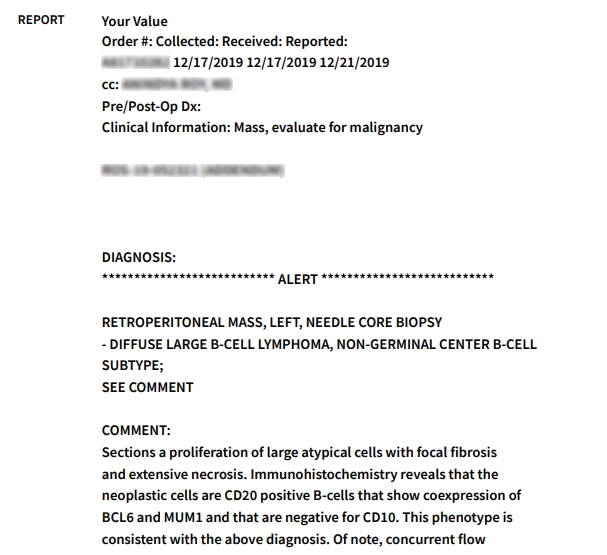
Diagnosis
Finding out the results of the CT-guided biopsy
There was a listing of what the biopsy found — a bunch of numbers, CD 20s, and all kinds of different things. The diagnosis was diffuse large B-cell lymphoma. I looked at that, went back up to the top, and said, “Wait a minute. Is this my file? Did I accidentally get in somebody else’s file?” That was a shock because I had heard of lymphoma before and it was never good. It was never in a good light.
[The] first thing I did was call my brother and go, “Dude, what’s this lymphoma thing?” He says, “What?” I said, “Well, it looks like I have cancer.” And he says, “Oh, come on now.” And of course, I was interpreting the chart so he was like, “Well, who are you? You’re not a doctor, you know.” And I said, “But it says pretty clearly: lymphoma.”
I had a doctor’s appointment the next day with the oncologist. I, of course, had a little trouble sleeping that night, but I didn’t really get sad about it. I was thinking, They’ll just tell me that it was a mistake and I’ll carry on. When I went to the doctor, they said, “Oh, no, that wasn’t a mistake. And we really do want to start treating you pretty soon.”
How cancer patients feel the moment they get their diagnosis »
I knew what my diagnosis was before they actually told me. I spent the rest of the day looking everything up online, but none of them made any sense to me.
They started to set up all of the appointments outpatient. It was going to be three to four weeks to start chemo and another five weeks to do the PET scan. I was going, “Oh, can’t they get me in any sooner? I mean, it seems like I need it.” Then they said, “No, you really do have this,” and I thought, “Okay, well, we’ll wait.” They were going to try and bump them up sooner and let me know. But at that point, they had already said, “You’re not working for a while.”
How did you feel when they said you’re not going to work for a while?
The feeling was, “When can I go back to work?” I had intended to work another 10 years if I could. At the company I retired from, I was going into 10 years total with them. I had worked with them in the early 2000s, then I left, and came back. I told them I was planning on working at least 10 years. I want to work for 20 years if I can. My brain will hold out. But obviously, that wasn’t going to be the case.
Working during cancer treatment: is it possible? »
Reaction to the cancer diagnosis
I knew what my diagnosis was before they actually told me. I told them, “Nice system you got where you find out just ad hoc online that you’ve got cancer,” but they talked their way around it pretty well. It doesn’t happen all the time, but they’re trying to figure out a way to make it different.
It was interesting. I spent the rest of the day looking everything up online, but none of them made any sense to me so I just carried on. “I’ll find out tomorrow what’s going on.”
There really wasn’t a lot of information that I got [on] the first visit. They handed me a folder that was probably about [an inch] thick and I didn’t read any of it. The last thing I wanted to do is dig into a bunch of medical jargon that I didn’t understand anyway.
I talked to friends that had been through similar things and that was a lot of help. My brother’s in-law’s family had just a bad few years with cancer.
I had intended to work another 10 years if I could. My brain will hold out. But obviously, that wasn’t going to be the case.
The importance of having someone with you during appointments
It was incredible. [My brother] was taking me to all my doctor’s appointments so he could be there as a witness. I’ve heard so many people on The Patient Story videos say [that] after they had said “cancer,” everything else was gone.
Learn how other cancer survivors went about breaking the news to their family and friends »
Treatment
R-CHOP chemotherapy
The doctors didn’t really go into much detail. They just said, “We’re going to do chemo and it’s going to be R-CHOP.” They told me what drugs they were and all that. They said that the first one that I get is going to be a weird one because they have to decide how long the treatment has to be.
The first chemo in the hospital was 16 hours. When they figured out how fast I could take that first drug, they cut it down to seven hours. All of my chemo treatments after that were seven hours.
Find answers to popular chemotherapy questions »
There really wasn’t a lot of information that I got [on] the first visit. They handed me a folder that was probably about [an inch] thick and I didn’t read any of it.
Being admitted into the hospital for treatment
They called me and said, “We’re admitting you to the hospital. We have a room for you on the oncology worked in. We’re going to do all of the initial stuff inpatient — the first chemo and the PET scan and so on — because we can get you in much sooner.” They didn’t really say why they wanted to do it so much sooner. I just assumed it was some trick that the doctors could use to get me in there quicker. I appreciated it because it was much sooner than planned.
It came as a surprise, but I was ready for it. They told me that that was going to probably happen. My brother was able to hang out with me while all of that was going on. He took me to the hospital and we got all settled in the room. I was only there a few days, I think four or five days, and he was there every day to visit me all the way until March when they closed down visiting.
My brother really got me through the treatment and everything. I just can’t thank him enough.
Side effects from chemotherapy
They never really did define the infection that became septic. They were very concerned about that. I spent a few days in the hospital with each of those. It pushed out my chemo treatments by about the amount of time that I was in the hospital, usually about a week or a week and a half.
I was really looking to get those over with and see what happened because otherwise, I had no real side effects from the chemo. I was a little tired the day of the chemo and maybe a little bit the next day. But then I had a lot of fatigue from other things going on, too. All the drugs that I have to take and so on.
They gave me Neulasta. I had to go to the infusion center again and get shots for three days.
Hear from other cancer patients on how they got through the different side effects of treatment. »
I’ve been shaving my head for so many years that I wouldn’t notice that. But I’ve always had a goatee or a full beard and it’s always been like Santa Claus in the natural sense, where the hair grows straight out and really thick. When I started growing my goatee back after the chemo was done, it was going sideways.
I heard that my dad, when he was going through chemo for his lung cancer many years ago, lost his hair. He had really white, perfectly straight hair. His hair grew back really curly. I thought, If I grew my hair out, it would probably be really curly because my hair was always really straight. Now it has this curl right down at the bottom and it all ends up over on the side. It’s not a big problem, but I just thought that was hilarious that it wouldn’t grow straight now.
I’ve never had heart issues, but I heard that it could have happened with the chemo, but I haven’t seen any of that come up.
How did you feel about losing your hair?
It didn’t bother me at all. I think I look funny without hair on my face, but everybody else said, “You look great!” I didn’t have eyebrows, eyelashes, or anything. The nice thing was I didn’t have to trim the hair sticking out of my ears or my nose. I didn’t have to shave and I thought that was really nice.
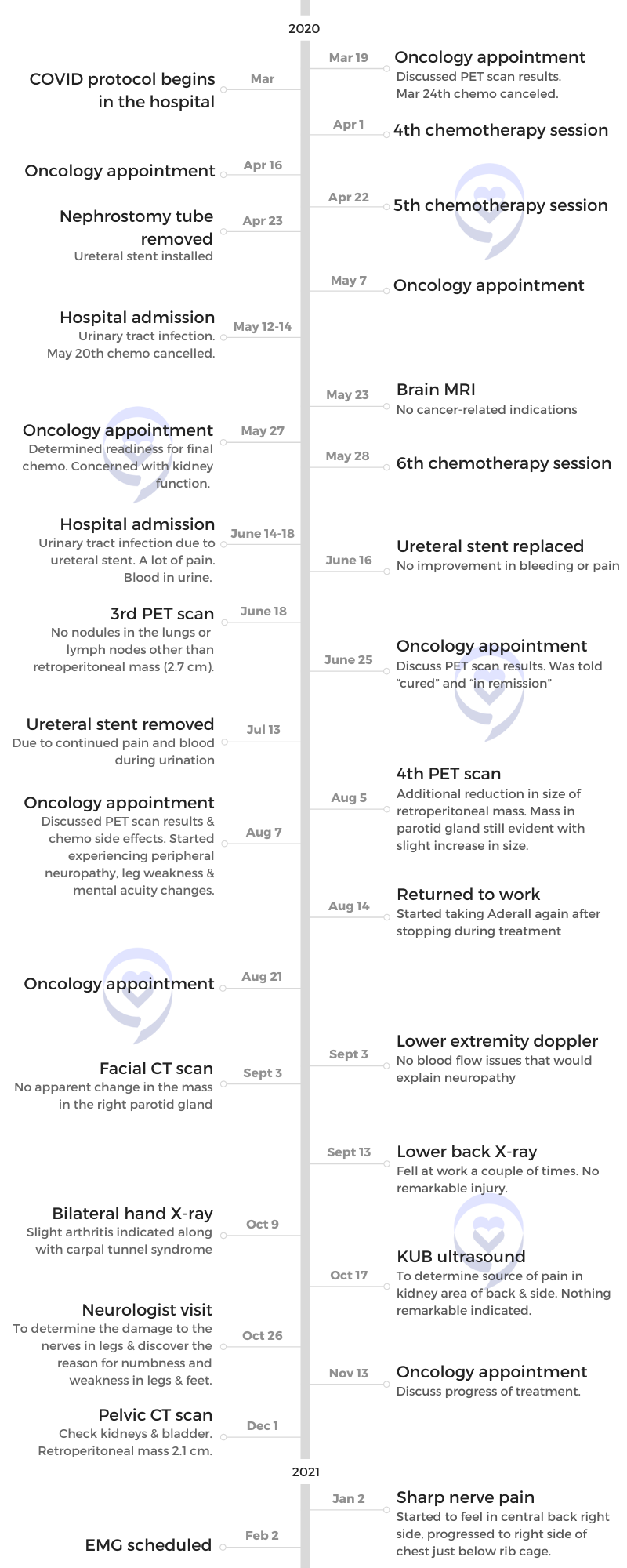
What was it like undergoing cancer treatment during the pandemic?
The hospital moved the infusion center to an easier place to get to so that most of us that were dealing with [infusions], which were mostly cancer patients, could just walk in a door and we’re in that area. That worked out really well but that was only one visit out of the six I had.
Then they moved it back to way down the hallway. It was strange because it seemed like there was doom at the end of this hallway. You couldn’t see all the way to the end. But when I got down to the [center], everybody was awesome to deal with. I used to show off my port and have the nurses all giggling.
My sons, I felt really, really bad for them. They were both in retail where they dealt with the public every day. Neither of them wanted to visit me because they just assumed that if they gave me COVID, I was going to die.
How was it like going through this experience alone due to COVID restrictions?
My brother found other ways to deal with it. When I wasn’t in the hospital, he would come meet me at my house and help me clean up. We’d have some takeout when they figured out how to do that with COVID. He probably took more time to come to my house to make me feel like there was somebody there.
I had a nurse that came to my house once a week to maintain the bandages and the surgical point for the nephrostomy tubes that I had to help with my kidney failure. I got to know her pretty well and she was a lot of fun.
My sons, I felt really, really bad for them. I knew they wanted to come and visit me but they were both in retail where they dealt with the public every day. There wasn’t any way they could [work from home] since they were dealing with the public every day. Neither of them wanted to visit me because they just assumed that if they gave me COVID, I was going to die. And they were probably right. I don’t know for sure.
There was always somebody that I could talk to though. There was no point where I was suicidal or anything like that. The doctors, at one point, were calling me every day.
How to deal with the feeling of isolation
I’ve always been a happy person, even though I was diagnosed in 2014 with ADHD. I guess I was just so used to being alone. It didn’t bother me. I didn’t let it bother me at all. I felt the same loneliness that I had before I had the disease.
Every once in a while, I’ll go out for drinks with my friends. I had both men and women that I could talk to about anything. I liked working so much [because] I was hanging out with 700 of my closest friends. I knew everybody in the plant. I may not have known their name, [but] I knew their face and what their family history was and everything. I could talk to anybody in that facility and feel better when I walked away.
We ran three shifts so there was always somebody in the plant to go talk to even if it was just about work. It was always good. I like being technical with people and teaching them things. So many of the people in that facility appreciated the fact that I would talk to them as somebody at their level or try to bring them up to my level of knowledge. They all appreciated that a lot.
I’d give anything to be there again, to be there right now.
How can you show support when a loved one has been diagnosed with cancer? »
I guess I was just so used to being alone. It didn’t bother me. I didn’t let it bother me at all.
The impact of having to retire early
I worked until January before my doctor finally said, “You’re done.” There were several things that led up to it. One of the drugs that I was on for ADHD kept me awake during meetings and also kept my brain working at a point where I could do my job as I felt that it needed to be done. Everybody said they didn’t notice that I was incapable of doing my job. I felt like I was incapable.
When my doctor asked me if I could do it without Adderall, I said, “No, I can’t. I’ve got to have the Adderall.” But I’ve been losing teeth from grinding my teeth so much and I felt stressed in my head even though there wasn’t anything to stress me out.
That drug was having a profound effect on my left kidney — that was the one that was struggling after cancer, even after the treatment. He said, “You’ve got to do something else.” I said, “We’ve tried everything else and nothing else worked like this.” He said, “Well, then you’re not working anymore.” “What?” He said, “Nope, we can’t do it. It’s going to completely destroy your kidney.” And I said, “Well, I got another one.” He said, “No, that’s not good enough. We don’t do that.”
I went out on medical again in January of ’21. By December of 2021, I finally decided I was going to retire.
It’s been a lot rougher because the medical leave, I knew that at the end of it, I was probably going back to work. And I was so excited to go back to work after the cancer treatment. My doctor said, “You really shouldn’t. You should just retire now.” But I don’t want to and we couldn’t come up with a really good reason to present to the Social Security Disability Board because my legs hurt and they’re weak. Why? We don’t know. And to this day, we still don’t know.
The thing that finally got me through all of it was chemo brain, which was really weird because I was an advanced-level engineer and I sat at a desk staring at a computer all day. I’d get up and walk around once in a while, but apparently, it was the best situation because I was approved for Social Security Disability two weeks after I applied. I’ve heard people that have gone for years trying to get disability insurance from Social Security with really obvious physical problems. I was really surprised by that.
What benefits are available for cancer patients? »
I’d give anything to be [at work] again, to be there right now.
Twin brother gets diagnosed with bladder cancer
He got cancer right as I was coming out of it and that was disturbing.
We were sitting and talking in my house. I said I had so many issues with [my] kidney even after all the treatment [and] the UTIs. I had stents in the ureter for a little while [and a] nephrostomy bag and everything on me for over six months. With all of that, he told me that he was having trouble going to the bathroom and I said, “Get your butt into the doctor right now and don’t sidestep it. Tell them exactly what’s going on.”
He went to our doctor and did a urinalysis. They said, “Wait, there’s cancer cells in there,” and discovered he had bladder cancer but it was really early. He went through one round of chemo, but they put it right in his bladder. Then he did immunotherapy for, I think, eight visits or something. It was almost every three weeks, almost like my chemo. Then they set up a maintenance plan for him after they told him that he was cancer free. We were celebrating that one, too, but mildly celebrating because it was still COVID.
He came out of it really well. I am just so happy that happened because there were a couple of scares where they thought it might have gone into the muscle tissue and I’ve heard that that’s not a good sign.
Getting a second opinion post-treatment
The last time I’d seen the doctors at Beaumont, at the Rose Cancer Center, in one sentence they told me I was cured and in another sentence told me I was in remission so I didn’t know what to believe. This was partially the reason that I went to Karmanos.
They also told me that Karmanos would be the next step if the cancer did come back, that Beaumont could no longer perform the treatments. They couldn’t do the stem cell transplant or anything if the cancer came back.
I set [it] up with Karmanos on my own. She had seen all of my records from Beaumont. They had access to my online chart. When I went into her office, I said, “I don’t want to have baby powder thrown up in the air and everything else to make me so welcome here. I want to know what’s really going on.”
It was humorous, the story. She said, “There’s a 65% chance that your cancer is going to come back.” I said, “Really?” She said, “That means there’s [a] 45% chance that it won’t.” And I said, “Well, I’m not as smart as most doctors, I don’t think, but there would be 35% that it won’t.” And she said, “Oh, yeah. You are an engineer, aren’t you?” And I said, “Well, yeah, but that one’s easy enough.” But so far, I’m good.
The other thing was that at Beaumont, they said that I was stage 3 to 4 and that they don’t really stage these things because there’s no real help in the treatment. I thought that was a little bit weird.
Then Dr. Sano at Karmanos said, “No, you are not stage 3 to 4. You are late stage four.” I said, “Oh. Well, what does that mean?” She said, “You are probably within a month of dying.” And I said, “Oh, I never even thought about that.” She wasn’t brutal about it or anything. I was thinking it was a quota they had to keep. She said, “That’s sometimes a quota thing. I’m not going to admit that any kind of a medical institution would do that.”
She was treating me as somebody on the same level, I’d like to think. She realized that before I had chemo brain, I was pretty smart. Since then, they’ve been pretty good. I’m afraid to say that she has left the hospital at Karmanos so I [will have to] see a new doctor next time. And I’m not looking forward to that because she was so awesome. She was really young, too. She was under 30. It was just nice talking to somebody that could tell it straight. I don’t want to sugarcoat it and that seemed to be what Beaumont was really good at.
Learn more about how chemo brain feels, how long it lasts, and how to combat it »
Words of advice
Why did you start watching The Patient Story videos?
I was looking for confirmation that I was going to make it through all this. I’m not the type of person to be scared of a lot of things and this one scared me a little bit. I’ve been riding a motorcycle for 50 years and this one scared me a lot more than getting out in traffic on a motorcycle.
The videos were quite helpful in how people managed it, especially the thought of it coming back. When I started watching The Patient Story videos, I had already been through my chemo and they told me that my cancer was gone. Of course, I was happy about that but they didn’t really tell me the rest of the story until I started seeing a different oncologist in a different cancer center. She was the one that told me, “You could be in deep trouble here, fella.” She was very nice about it. I’m not saying that she was brutal, but it was something I needed to hear because I had no idea what my chances were of making it through without cancer coming back.
[The] interviews, especially the young people, got me through a lot of the secondary side effects that I have from the chemo and just making sure that I’m not alone.
Learn more from our patient community »
I was looking for confirmation that I was going to make it through all this. I’m not the type of person to be scared of a lot of things and this one scared me a little bit.
How important was it to bring those moments of lightness?
It was important to me. I like to see everybody smiling. I’m the type of person [who] when I walk down the hallway at work and pass somebody, I always smiled at them. That was different after COVID hit, of course, but I still tried it and nobody responded.
I’ve always been that way, even [when] traveling. I always smile at everybody and people seem to smile back, even if they look like they were in a bad mood to start with. I just enjoy that. That’s something that I feel I need to do. And it helps. It helps me if nothing else.
Why men typically hesitate to go to the doctor
My brother is one of those tough guys. He’s really good with his hands, which was apparent in his avocation when he could still work. He was in printing and machine repair. He was an awesome mechanic. He was that kind of guy, very tough, and he wouldn’t wouldn’t admit to anything.
He was just like my dad. My dad, when he found out he had lung cancer, it was way too late. They just said, “Well, how long do you want to live?” He took the chemo treatments and everything. He lived for 15 months.
With Kurt, he would wait until it was killing him. He’s had two heart attacks and both of them were like, “Why didn’t you come in when you actually had the heart attack?” “Well, I just thought I needed an antacid or something.”
Don’t let it slide. If you have a pain that doesn’t feel like normal pain, have them look.
How to convince someone to go see a doctor
It was easy after all that I had been through. At that time, he probably heard me whimpering in the bathroom when I had to go because it hurt so bad.
For me, it was — my back hurts, yes, but not in this spot. In this spot, I’ve never felt that pain before. Don’t push it aside, especially as you start to get older.
Getting those infections that led to the sepsis, when the actual sepsis set in and my brain wouldn’t work, I was stumbling around the house and my brother’s trying to keep me from falling. I’m doing these calculations in my head that make absolutely no sense. It was like I was at work, but I wasn’t where I work. I would have probably just said, “I’m just weird, you know?” And my brother said, “No, I think we’re going to the hospital now.” He loaded me in the car and we got there. The nurse did all my vitals. My blood pressure was really low and my heart rate was really high. That was in the throes of it.
Don’t let it slide. If you have a pain that doesn’t feel like normal pain — because I know every man has some pain that he doesn’t admit to or that’s been around for 20 years. “It’ll be okay.” It probably won’t be, but if another one comes up, have them look at that one. It’s simple. It’s half an hour at a doctor’s office and you’re done with it or even a couple of hours at an E.R., if you have one that’s not too busy.
Most of us have medical insurance now. And even those of us that don’t, if you do find out you have cancer, I’m sure with a lot of the lymphoma societies, there are ways to get financial help. I haven’t needed it, thankfully. Just get it done.
Make sure you get diagnosed. If you even have just this remote idea that there could be something amiss inside your body, get it checked out. There’s no reason not to.

Inspired by Kris's story?
Share your story, too!
Diffuse Large B-Cell Lymphoma Stories
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy




One reply on “Kris’ Stage 4 Diffuse Large B-Cell Lymphoma Story”
Hello, I just finished RCHOP and radiation therapy for Large Diffused B Cell Lymphoma and was curious if anybody experienced severe side effects from the treatment. For myself, I lost a lot of weight, lost all my muscle mass, and developed neuropathy and upper and lower joint pains. Physically, I’m about 5% of what I used to be pre-cancer. Wondering if the effects eventually go away or if this is what it is moving forward. Thanks.