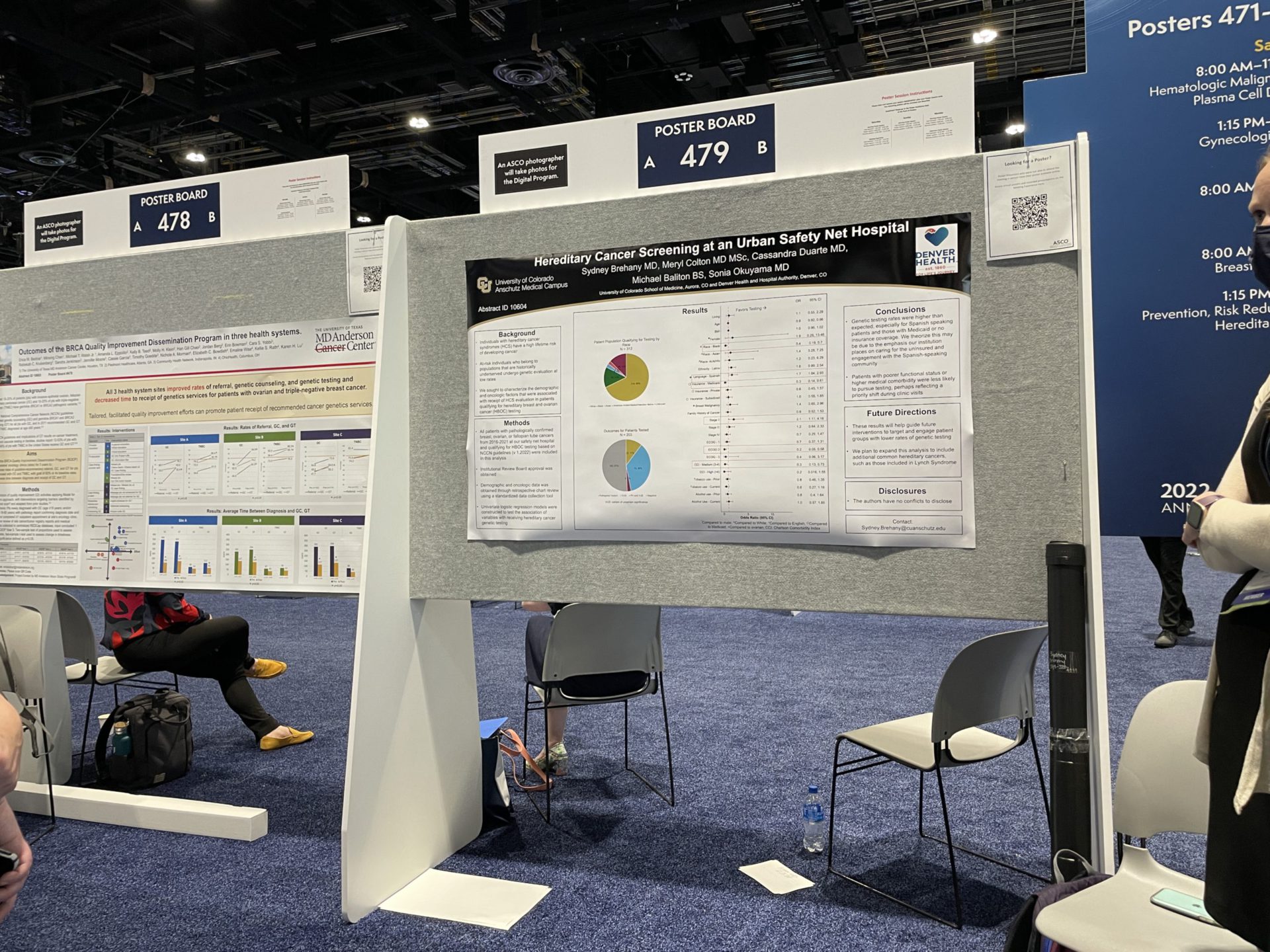
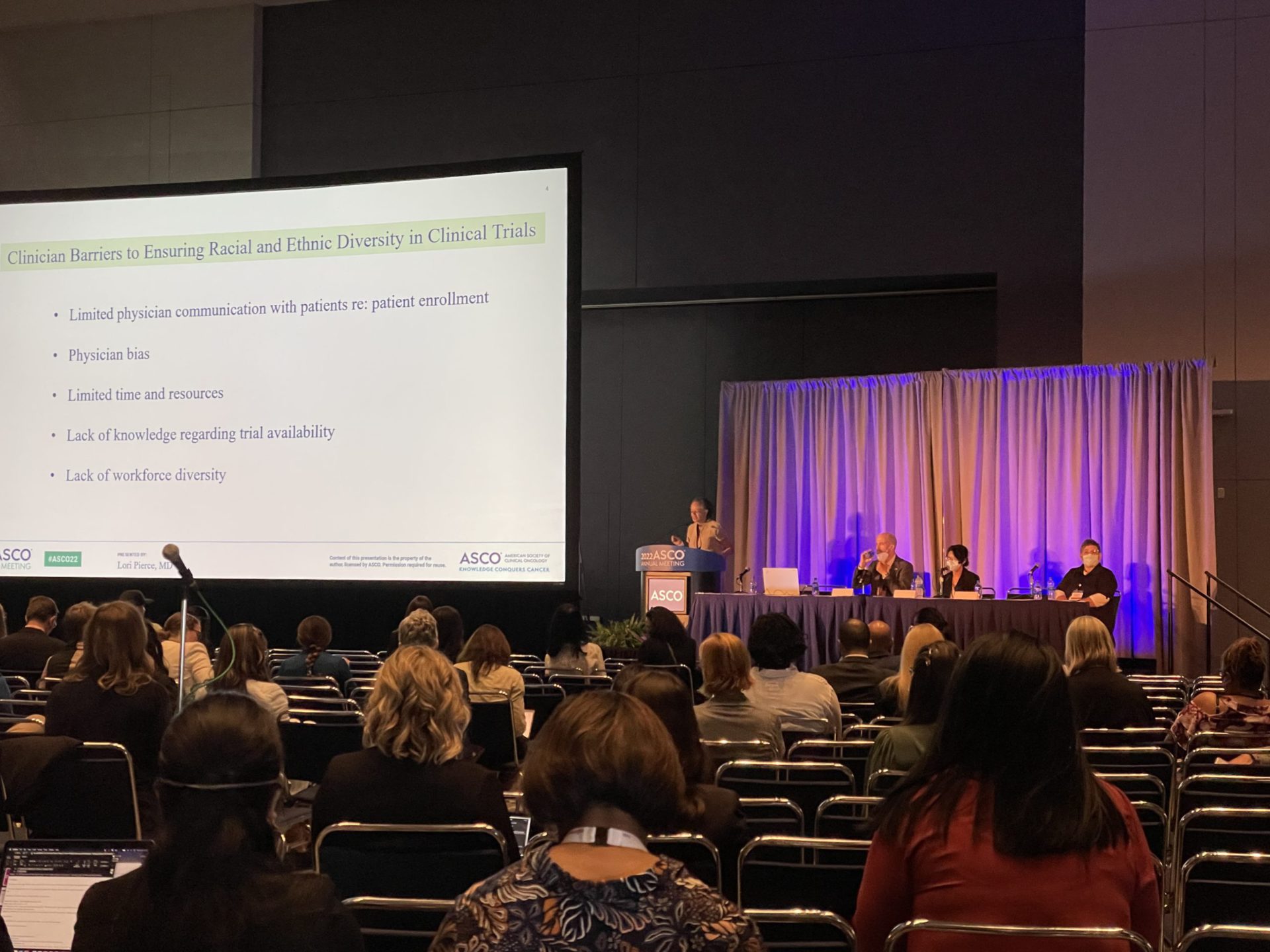
Trends in Cancer Research (ASCO Conference 2022)
Top Specialists at ASCO 2022
The annual American Society of Clinical Oncology (ASCO) meeting is where top minds in oncology gather every year to share progress and cover the the top cancer treatment and research trends today. The Patient Story spoke with three of the top cancer specialists, covering precision medicine, myeloproliferative neoplasms (MPNs) and chronic lymphocytic leukemia (CLL) studies.
There are 35,000 people here talking about cancer, but more importantly, talking about progress.
Dr. Mark Lewis
Dr. Mark Lewis

Dr. Mark Lewis, a cancer survivor, is a hematologist-oncologist at Intermountain Healthcare and an expert in precision medicine.
Dr. Ruben Mesa
Dr. Ruben Mesa is the director of UT Health San Antonio MD Anderson Cancer Center, and a top MPNs specialist.
Dr. Kerry Rogers
Dr. Kerry Rogers is a hematologist-oncologist at The Ohio State University’s Comprehensive Cancer Center and a top CLL specialist.
Dr. Mark Lewis: Precision Medicine
Personalized medicine
Patients should know the theme of ASCO, which is like the Super Bowl for oncology. There are 35,000 people here talking about cancer, but more importantly, talking about progress.
I think the biggest theme has been personalized medicine. That’s a phrase that sometimes is used almost to the point of overuse, but I think authentically means individualizing treatment.
First of all, defining a cancer as specifically as possible. For instance, rather than saying colon cancer, which side of the colon that it started on? That matters. Then what molecular or genetic characteristics does the cancer have that can refine the patient’s treatment?

Actually, a lot of the meeting has been about doing less, not more. What I mean by less is intensifying treatments, which means fewer side effects, but arguably no decrease in outcome, meaning that the cancer related outcomes like survival don’t get worse, and the patient was spared side effects.

The most unbelievable study happened. In fact, it was so important it got coverage in the New York Times. Patients with a relatively advanced but not yet metastatic rectal cancer had a vulnerability to immunotherapy. With just immunotherapy, all 12 patients — which I know sounds like a small study — had a complete response to the cancer.
Not only did they not need surgery, but they didn’t need chemo. They didn’t need radiation. It was such a big deal that it actually got covered in The New York Times in addition to getting, of course, a lot of publicity here at ASCO.
Those are the kind of things that are happening. You can see the spillover into popular media and popular culture when something of that magnitude happens. Traditionally, we have thought every patient with a cancer like that would require chemo, radiation and a big operation. Now it turns out, again, it’s exceptional that a certain group of patients can “only” get immunotherapy, which is amazing.
Patient access
We do walk this tightrope of hope and hype. I don’t think it’s hype, because the science is there. I think the difficulty is in overpromising logistically. It’s okay for patients to ask their oncologists about the progress that they’ve heard about here, but I do think there has to be a little bit of realization that it will take a little bit of time to implement.
Now, having said that, the really groundbreaking changes will almost immediately change the guidelines by which doctors — and let’s be honest, insurance companies — decide how to arbitrate care. You actually should not have to wait very long. The FDA monitors a lot of this activity and is pretty quick these days to approve new drugs and new indications when they see evidence of benefit.
Precision in oncology and what that means to care
To be honest with you, oncology has this not-proud history of indiscriminate toxicity. Quite famously, people know that people on chemo tend to be very sick. They tend to lose their hair. They can have permanent damage.
We really are trying to be more targeted in the treatments we get, and so less really is more. It’s interesting. I actually had a patient reach out to me and say, “Don’t say ‘less’ because patients don’t want to feel like they’re being treated to a lesser degree.”

There’s a difference there. It is quantitatively less. It is not qualitatively lesser. We’re not actually treating you in an inferior manner. I would actually argue that we’re having it both ways. We’re having an equal outcome in regard to your cancer, while we’re preserving you and your quality of life.
For people that don’t get to attend, I think it’s actually really important that you know that there’s gatherings like this. ASCO is a massive, massive event. Again, I think what’s so exciting is we’re all pulling in the same direction. We’re all trying to make things better for patients. Regardless of what specific cancer you might be interested in, there is research being done. We are slowly but surely, in some cases very quickly, moving in the right direction.
Dr. Ruben Mesa: Myeloproliferative Neoplasms (MPN)
Developments in treatment
For MPN patients, I think there should really be a tremendous sense of hope. There are many, many new therapies in development, some that are really having some very positive results.



I’m at this meeting. I’ve got this 20-year member badge here, and I’ve been a member here for about 25 years. But I saw my first MPN patient now almost 30 years ago.
The first 15 of those 30 years, we did not understand the diseases to a great degree. This is before we had discovered the JAK2 mutation and many other associated mutations that are very important in the biology of why MPNs develop and why patients are afflicted.
Sometimes we learn even from diseases as different as lung cancer or breast cancer, and they learn from us.
Dr. Ruben Mesa
During that time, it was very hard to develop treatments that were effective against the disease, because we didn’t know that much about them. The last 15 years have really been unprecedented.
We now have several approved drugs for MPN, three in myelofibrosis, ruxolitinib, fedratinib and pacritinib. The recent approval of ropegylated interferon alfa-2b, or Besremi, for individuals with polycythemia vera. There is an unprecedented number of new medicines that are in development. That may have implications, whether you have MF or PV or ET. It’s really a tremendous time to be hopeful.

What are the top focus areas trending for oncologists?
I think there are several things. One, a meeting like this, there’s a lot of innovation in terms of how we care for patients. If we’re using telemedicine, how do we do that best? How do we help to care for everyone in society, and how do we help to improve diagnostics? How do we help better monitor patients in a way that’s more convenient, whether through their device or their cell phone or other things?
Second, there are real innovations in different ways that we’re treating cancer. They have started more in other types of cancer, particularly around the treatment of the immune system, with either ways that are vaccines against cancer or even treatments that we call cellular treatments that, again, use the body’s immune system.
There are things that are called CAR T or CAR NK. These are treatments where these cells are programmed to go after the disease itself. They have not yet started in MPNs, but we’re learning a lot about them from other diseases and then really hoping to apply those things in the future.
I think, again, the treatments that we’re going to have are going to continue to evolve, but we learn from other blood diseases. We learn from the diseases that are cousins of MPN, diseases like myelodysplastic syndrome or even acute leukemia. Sometimes we learn even from diseases as different as lung cancer or breast cancer, and they learn from us.
I just came from a meeting with a colleague. She is looking at using a medicine we use in MPNs, ruxolitinib, but combined with a different type of medicine to treat patients with advanced lung cancer. The combination with an inhibitor against her protein called AXL may have a benefit against treating lung cancer. We learn from them, but they learn from us.
Dr. Kerry Rogers: Chronic Lymphocytic Leukemia (CLL)
Larger studies follow-up
This year, I think the theme is kind of follow-up on larger studies, and I was really excited to present some work that we did. We have a study at Ohio State that’s a combination of obinutuzumab, ibrutinib and venetoclax for people with CLL given for just a little over a year.
We’re seeing longer remissions off treatment for patients.
Dr. Kerry Rogers
We’ve now looked out to 4 years with the first 50 people treated with this regimen in our phase 2 study. The big question is, “How long do people stay in remission after only one year of treatment?” It looks like people are staying in remission.
For people that took this as a first treatment, it looked like 96% of them were alive and without leukemia returning at this follow-up. For people who took it after another treatment, 85% were alive and without the leukemia recurring. That’s really outstanding for something where you get treated for one year and you can remain in remission.
That is kind of a theme we’re seeing in CLL now, because we did these really great studies to combine non-chemotherapy drugs to get really deep remissions for our patients, and then they could be off treatment, back in observation, living their lives and not have to deal with taking treatments every day or chronic side effects.
»MORE: Read more patient stories about CLL


CAPTIVATE
There is a study called CAPTIVATE, which had a group of 159 people with CLL treated with just ibrutinib and venetoclax for a little more than a year. They received similar results for our 3-drug regimen. For the extended follow-up, they’re at 3 years. 88% of those folks are alive and without their leukemia returning. 88% might not sound awesome, but this is really awesome when you consider people aren’t taking treatment.
At the European Hematology Association meeting, which is coming up in a couple weeks, we expect to see a follow-up on a study called CLL 14, which is the venetoclax and obinutuzumab study. This is really just kind of a theme we’re seeing, where we’re seeing longer remissions off treatment for patients.
It might not seem brief for a year, but that’s brief considering the alternative is taking BTK inhibitors every day. People can just remain healthy and in remission.
Other Medical Experts
Dr. Christopher Weight, M.D.
Role: Center Director Urologic Oncology
Focus: Urological oncology, including kidney, prostate, bladder cancers
Provider: Cleveland Clinic
...
Doug Blayney, MD
Oncologist: Specializing in breast cancer | HER2, Estrogen+, Triple Negative, Lumpectomy vs. Mastectomy
Experience: 30+ years
Institution: Stanford Medical
...
Dr. Kenneth Biehl, M.D.
Role: Radiation oncologist
Focus: Specializing in radiation therapy treatment for all cancers | Brachytherapy, External Beam Radiation Treatment, IMRT
Provider: Salinas Valley Memorial Health
...
James Berenson, MD
Oncologist: Specializing in myeloma and other blood and bone disorders
Experience: 35+ years
Institution: Berenson Cancer Center
...





