Michele’s Chronic Myeloid Leukemia Story

Michele, an active dancer and traveler, brushed off her symptoms until she received a surprise CML diagnosis.
Michele shares her journey, including first symptoms, researching treatment options and regularly draining fluid from her lungs.
A huge advocate for other CML patients, Michele also discusses creating a blog to share her story, living life to the fullest with chronic cancer, and the importance of advocating for herself.
Thank you for sharing your story, Michele!
- Name: Michele T.
- 1st Symptoms:
- Bruising
- Struggling to breathe
- Rash
- Diagnosis:
- Chronic Myeloid Leukemia (CML), Ph+
- Treatment:
- Tyrosine kinase inhibitors (TKIs)
- Sprycel
- Bosulif
- Tyrosine kinase inhibitors (TKIs)
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
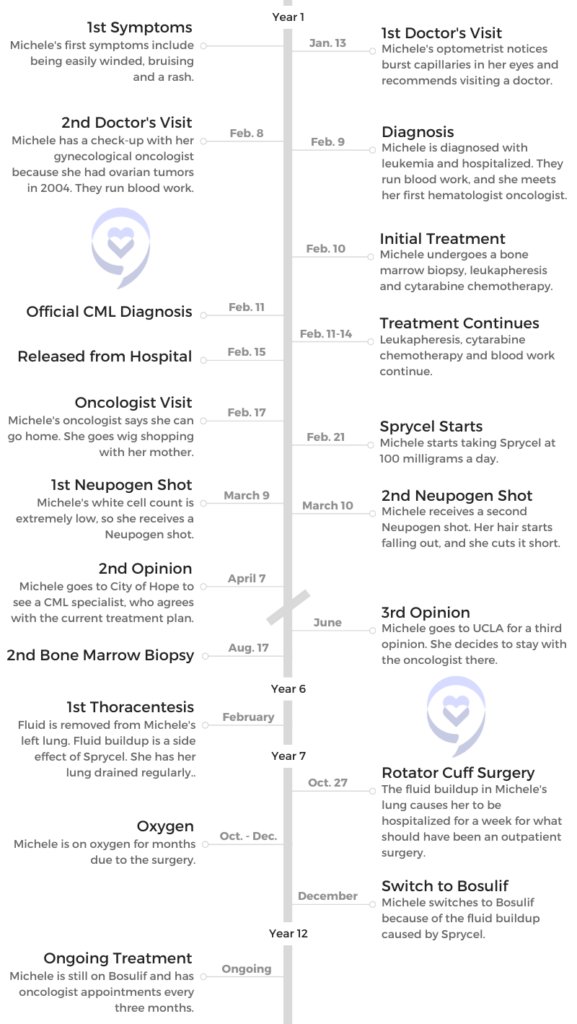
1st Symptoms and CML Diagnosis
Introduction
Tell us about yourself
I’m a wife, a mother and a grandmother. I love all of those roles, and I love my kids and grandkids.
My husband and I have hobbies. I write, knit, and crochet. We dance and we like to travel. We do ballroom, country, two-step, waltz and cha-cha. As a matter of fact, I was dancing two weeks before I was diagnosed with leukemia.
I just love to enjoy life and I love my family and my friends. Helping other CML patients is another passion of mine.

What were your first CML symptoms?
Honestly, I had probably every symptom of leukemia and I explained away every single one.
I was dancing in Nashville at the world competition in January. I was winded and tired, and I kept asking what the elevation was, why couldn’t I breathe and why was I so tired?
That was a symptom, but I didn’t realize it was because I had leukemia. I just assumed it was because we had worked so hard to get there.

I had bruising, but I thought, “Oh, you’re clumsy. Stop running into things.” I had these massive bruises. I didn’t think anything of it. I had spots, kind of like a rash, all over my body. I checked for bedbugs, washed the sheets and changed my laundry.
I did all of these things. While every single symptom that I had was a symptom of leukemia, it just seemed like it was a common thing that could be happening.
The night sweats got me a little concerned because I would wake up soaking wet. I had already been through that ‘time’ in life and I thought maybe my hormones are wacky.
He says, ‘Your white count’s over 385,000. Normal is 4 to 10. I need you to go straight to the emergency room.’
Probably the biggest [symptom] I had was an uncomfortable feeling under my left rib cage. When I was reading at night, I kept telling my husband, “Oh my God, things just don’t feel like they fit the same in here anymore. I don’t know why I’m so uncomfortable.”
I began to get a little concerned and still didn’t really think something was wrong.
Why did you go to the doctor?
I had an eye appointment for glasses, and my optometrist started asking me these questions.
He was like, “Do you have high blood pressure?”
“No, I have low blood pressure.”
“Do you have anemia?”
“No. What’s wrong? Why are you asking these questions?”
Basically, he said that there were capillaries that had burst inside my eyes, so he was concerned.
I was like, “What does that mean? Am I going to go blind?”
He said, “No, you’re not going to go blind, but you should have it checked out.” That was just another one of those things.

I got through the [dance] competition, and I got home. I had my regular checkup with my gynecological hematologist. Years before, I had borderline ovarian tumors. In the back of my mind, I was thinking that maybe this uncomfortable feeling in my abdomen might have been those tumors coming back.
They’ve always said they could grow back, so that is where my mind went. I went and explained all of these symptoms. He was like, “Well, let’s do some blood work and do a CT scan tomorrow.” That’s how it all began.
The CML Diagnosis
Blood work results
I ran across the hall and I got blood work. It was actually after 5 p.m. It’s kind of a funny story.
I got in the elevator. This doctor got in behind me, took one look at me, and said, “You okay?”
“Yeah, I’m fine.”
“Are you sure you’re okay?”
“Yes, I’m fine.”

He got out, I got out and I went to my parents’ house to spend the night. I got up in the morning. The phone rang at 8 a.m., and it was my oncologist.
He said, “Michele, I don’t know how to tell you this, but you have leukemia. I need you to go to the emergency room. I have a doctor waiting there for you.”
“Wait, what? No. What do you mean?” I was brushing my teeth in the bathroom. I was standing there, looking in the mirror with the phone in my hands and going, “How do you know?” That was my first question. “How do you know?”
He said, “Your white count is high.”
“How high?”
“Astronomically high.”
“What does that mean?”
“Your white count’s over 385,000. Normal is 4 to 10. I need you to go straight to the emergency room.”
“Well, can I drive myself there?”
He said, “I really would like you to get a ride. We’re afraid your brain’s going to start to bleed.”
About this time, I was thinking to myself, “Better get dressed. You better just get up.” I went and asked my dad to give me a ride to the hospital. I was like, “Apparently I have leukemia.”
What happened at the hospital?
I got there and they were waiting for me. They put me right into the ER, and I was in there for about an hour. They ran some blood work and the curtain opened up. Who’s standing there? That doctor from the elevator.
I said, “It’s you.”
He said, “It’s you. I didn’t think you looked okay.”
I said, “What was it about me?”
He said I was very pale and just looked sick.
It’s in those wee hours of the morning when nobody else is around that the gravity of the situation actually hits you.

At that time, I didn’t know there were many different types of leukemia. I knew nothing about leukemia. I knew it was a blood cancer
and that was it. This was 11 years ago, so I didn’t have a smartphone, an iPad, or a laptop. I had nothing.
I kept bugging the nurses. I was like, “I know you can print this stuff off for me.” Fortunately, it was right across from their little station there, and they just kept printing off information for me for leukemia.
I started reading all this stuff. I was thinking, “What do I do? Am I going to live? Am I going to die? What next?”

When did you start processing that you had leukemia?
It probably wasn’t until I was in my room and left alone. You just look in the mirror and you just kind of go, “Cancer. I have leukemia.” I probably did that. I probably still do that to be perfectly honest with you.
It wasn’t until I had to tell my children and make that phone call that the gravity of the situation actually hit me. At first, it was just like, “What do I need to do? This is where we are. This is what I have. Now I need to fix this.” You kind of stay on autopilot for a while.
I did the bone marrow biopsy and the different tests. They got the complete diagnosis of what type of leukemia and I was starting to feel really sick. It’s in those wee hours of the morning when nobody else is around that the gravity of the situation actually hits you.
What is your advice for someone undergoing a bone marrow biopsy?
Do not let them do it without sedation under any circumstances. My first one was without sedation. I balked a little, but not loud enough. In my opinion, it was pretty brutal. For my second bone marrow biopsy, my doctor was like, “Of course, we’ll lightly sedate you.” He felt it was barbaric to do it otherwise.
A big guy and a little guy came in, and I was like, “That one’s to hold me down and you’re the one to do the thing.”
He was like, “Pretty much.” Had I known what I knew, I would have just said no.
It’s easier for them to just do it, as opposed to having an anesthesiologist or somebody else there to monitor you more closely.
It’s easier for them, but we have to remember we have rights and we can stand up for ourselves. That made me go, “I’m standing up for myself from here on out. I am never going to let that happen again.”

Can you explain the leukapheresis process?
I made them explain every step of that process long before I let them touch me. They put it into your jugular vein. They follow it through an ultrasound as they’re putting it in. It’s more uncomfortable than painful.
It’s probably similar to getting a port that many people get when they have cancer. The tube sticks out of your neck where they connect that to and they take the blood out and return it.
Like I said, it was uncomfortable more than anything. It actually goes right into your heart. Having to think about that is just a little freaky.
I asked lots of questions and made them explain everything very thoroughly before they started.

It’s a little daunting thinking you’re going to have cancer the rest of your life, and some people will refer to it as ‘good cancer.’ I don’t think any cancer is good.
I had the catheter for almost 5 days. They took it out after they finished the treatment. I had the leukapheresis for 4 days in a row. It takes hours. You’re pretty much hooked up to this machine and somebody sits and watches it. I guess it centrifuges out the white blood cells.
You’re there, and you’re just kind of stuck there in the bed. They do it for several hours a day. Then they come back and do it again, because it has to be done more slowly. It can’t be done all at once.
Receiving the full CML diagnosis
Now I had something I could actually read and understand. I knew exactly [what it was]. Instead of it being vague leukemia, I knew it was this type of leukemia, so I researched that.
At that point, my husband had come over to Palm Springs and brought my computer, so I was able to sit up, read and try to understand what it was that I had, what it meant, what the treatment was, and what the complications could be. Knowing that was helpful, actually.
The type of leukemia I had was chronic, meaning I would have it the rest of my life, versus, “Okay, I have cancer. I’m going to have treatment, I’m going to ring the bell, I’m going to go home and I’m going to be done.”
It’s a little daunting thinking you’re going to have cancer the rest of your life, and some people will refer to it as “good cancer.” I don’t think any cancer is good. I was like, “Fine, you think it’s so great? You take it. I’ll just not have it.” They don’t realize the gravity of it.
You’ll see people 5 years later and they’ll be like, “Oh, you’re doing so well.” You’ll be like, “I still have leukemia.” They’ll be like, “What?”
They’re confused because cancer is not supposed to last forever. That was a little bit of a hard pill to swallow. Forever’s a long time. You hope it’s a long time, anyway.

Medication and Next Steps
Taking lifelong medication for CML
One of my biggest concerns was, “I’m going to be on these strong medications.” It’s an oral daily chemotherapy that you take every day for the rest of your life.
I was like, “What’s that going to do to my heart? What’s it going to do to my liver? What’s it going to do to my kidney? What’s it going to do to the rest of my body? Am I now at greater risk of other cancers? Is it going to damage my heart muscle?”
Chances are I might not die from CML, but I might die from the treatment, which also happens with other cancers. A lot of times, it’s the treatment.
How did your doctor discuss the next phase of treatment?
He basically said that he was using the leukapheresis and the cytarabine to bring down the white cell count quickly. There was concern [about] the third stage of CML, called blast crisis, which in many cases in the past meant a bone marrow transplant.
Now they have come up with certain different TKIs that seem to get people out of blast crisis and back into a more chronic phase.
At that time, he said, “Are you going to need a TKI, which is the oral medication, or are you going to need a bone marrow transplant?” His main concern and goal was to get me to a stable position before trying the medications.
Why did you decide to get a second and third opinion?
I realized that there were hematological blood cancer doctors that specialized in different types of leukemia. I quickly became aware that there were people that specifically worked with CML patients.
My thought process at the time was, “I want to see someone who sees other CML patients so they will have something to compare to, versus someone that only sees it once.” There’s a really good chance that a hematologist-oncologist will never see a case of CML.
At the time, there were 10,000 people living with CML. It was rare because 10 years prior to that, people died quickly. Now we have a much larger community. I think it’s maybe 100,000 people. It’s a rare cancer.
City of Hope
I called City of Hope, they had CML specialists. I was living in the LA area, so it was closer to home. “Maybe I should go here,” I thought.
I went there and I was mesmerized by the size. It is huge. It is run like a well-oiled machine. You go in, you meet this person, you get the badge, you get the blood work and you get sent over here. They do this. They do that. It felt very methodical.
The doctor was very thorough and she was on board with the treatment from the doctor that diagnosed me.

Nobody knows your body more than you. They see you for a short period of time. You live with you every day.
She said, “We just want to do weekly blood draws and make sure. This will be for several months. Then come back and see me in a month.”
I saw her a second time, but I just didn’t feel like we had a connection that I wanted for the rest of my life. With CML, it’s the rest of your life.
I felt I needed somebody that I could talk to — somebody that would listen to me, somebody that would answer my questions, somebody that wouldn’t get impatient, and somebody I could reach when I was scared or had a question. I needed all of those things.
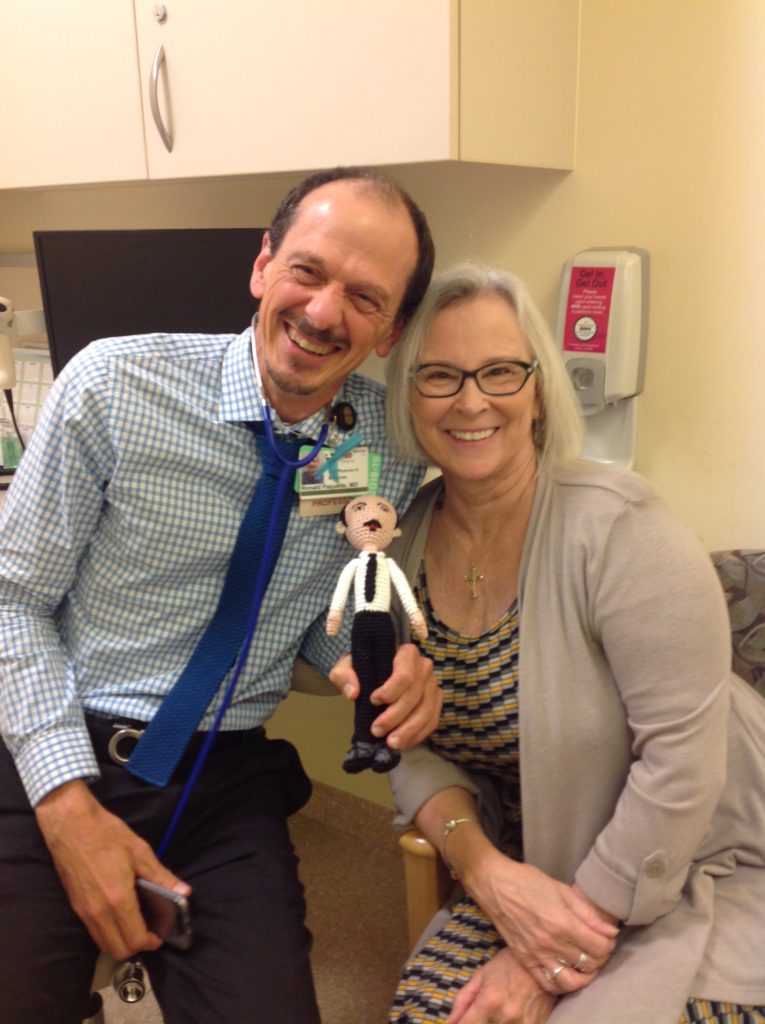
Having a personal connection with your doctor
I made another appointment and I ended up at UCLA. Then two minutes into that conversation, I was like, “Okay, this works for me.” I went in for a third opinion, and he was very conscientious of not trying to say, “You should come and be my patient.”
He looked at it as a third opinion and pretty much agreed with the treatment. It was a connection for me, so I switched doctors to go to him.
I think it was just bedside manner. He was comfortable, and he was like a human being. He wasn’t like the person that most people think of as a doctor.
Doctors are human beings. They are no different than you and I. They have a degree. They’re practicing medicine. They call it “practicing” for a reason.
They don’t know everything. Doctors can’t predict everything. They are human beings and different people work and connect better with some people than others.
Other people need different types of communication and I needed somebody to meet me on a personal level. I needed somebody to consider what I was saying was important. Whether it was silly or not, it was important to me.
He didn’t make me feel like it was frivolous or stupid. He met me on a personal level. For me, that’s important. I don’t want to feel like my doctor is this person on a pedestal.
Nobody knows your body more than you. They see you for a short period of time. You live with you every day.

TKI Treatments for CML
What treatment options were presented to you?
I was still in the hospital. I was getting close to 100,000 white cells, which meant I could be going home shortly. My doctor actually came and told me that I would be leaving and that I would be on a medication.
Pretty much what he said is, “You will be on a pill for the rest of your life. It’s a very small pill, but it costs a lot of money.”
I said, “What’s the name of that pill?”
He told me, “Gleevec.”
I said, “Is it the only option for CML?”
He said, “No, there’s 3, but this is the one that people usually start with.”
I said, “Could you tell me what all 3 of them are, please?” He told me and rattled off the names. I didn’t understand, so I was like, “Write them down.”
He wrote them down. At this point, he was a little exasperated and maybe a little bit annoyed that I was questioning him. I didn’t really care.
Researching Options
I wrote them down and I looked them all up that night. What I found was Gleevec was the first TKI. It was invented, for lack of a better word, by Dr. Druker. It saved so many lives. It was great in that regard.
They came out with the second one. I was like, “They came up with the second one, so it may be better.” I started researching that one, and that’s called Tasigna. Twice a day, you had to fast an hour before and two hours after. I was like, “That probably won’t work for me.”
It also had a black box warning. When I looked that up, it was cardiac issues. I take black box warnings on medications extremely seriously. I had a really bad reaction to an antibiotic with a black box warning that no one told me about.
Then Sprycel was the third one. The data on it seemed to say that people reach expected CML milestones for the best long-term outcome quicker than on Tasigna or Gleevec.
I was like, “Why wouldn’t I want to start there?” Sprycel seemed to have better data regarding reaching milestones and long-term success. That’s the one that I wanted to start on.
»MORE: Targeted Therapy
Starting Sprycel
When my doctor came in the morning, I told him that. He said that people usually started with Gleevec. I said, “What do we need to do? I want to start on this one.”
He somehow sent in his assistant and she got a 7-day free trial at the pharmacy. They got me on the patient assistance program and I started on Sprycel.
It was once a day. Typically you start at 140 milligrams. I guess 100 is also fairly normal. I questioned the dosage based on my thinking, which was, “At 110 pounds, why would I take the same medication as somebody that’s 300 pounds? Shouldn’t it be geared more toward body size?”
I was opting for a lower dosage to see if it would work, because of the longevity of having to be on a medication that could potentially damage the rest of my body. We agreed on 100 milligrams and that’s what I started on.
Taking the first pill
I took the first pill when I got home to LA. You read all of the possible side effects and things that could happen in adverse reactions. It’s just scary. I literally looked at that pill and I was like, “Oh man, what do I do?”
I took it and just sat there, waiting to call 911 in case something horrible happened. It did not.
You want somebody with actual, true experience.
It gave me a terrible headache. I felt like I had the flu. I had to go to bed. It took me weeks and weeks to adjust to it. It was like, “Is this the pill? Is it still just the leukemia?” You just don’t know in the beginning.
I just had to say to myself, “Self, you have cancer. You have leukemia. You are sick. Be kind to yourself. Rest when you need to rest, and do whatever it is you need to do. Do your weekly blood draws. Take your medication.”
White cell count dropping
What ended up happening — and often happens in the beginning — is that it will absolutely tank your white cells. Your white cells are what fight infection. I went from 385,000 to 900 and I couldn’t figure out why I felt so sick. I felt so sick because I had 900 white cells. They called me once again, and they were like, “Come to the emergency room.”
They gave me a shot of Neupogen, which stimulates the growth of white blood cells. It also causes more bone pain than you already have. I had to have several injections of those to get it stabilized.
Then they hung at about 3,000 for probably 3 years. They’re currently around 5, so that’s good.
I did not get other illnesses and I didn’t get sick. Of course, I didn’t go anywhere, so I wasn’t really exposed to germs. All in all, I am a pretty healthy cancer patient. I’m fortunate for that.
Importance of seeing a CML specialist
I feel like it’s really important to see a CML specialist if you have CML. What I mean by that is somebody who sees more than just you. You want somebody who sees lots of CML patients. They can say, “Okay, this happened to this person. This is common. I saw their white cells dropping below 4,000 and this is what I did. This is the result I had.”

You want somebody who has knowledge and experience with things like that. They know what to do and they’re not just going to the internet. You want somebody with actual, true experience.
Side effects of Sprycel
I was on Sprycel for 6 years. In about year 5, I started developing a small pleural effusion in my left lung.
In the beginning, Sprycel clearly gave me headaches, which I took Tylenol for. They felt that was the most compatible with the Sprycel. Sprycel can also cause your blood to become thinner, and ibuprofen can make that happen even more. Tylenol was the drug of choice for headaches.
I had terrible bone pain. I had pain in my hands. Everything I picked up, I dropped. My hands would burn at night. They ended up saying it was neuropathy. They kept saying it wasn’t from leukemia, and it wasn’t from the Sprycel. I kept saying it absolutely had to be. I didn’t believe that it was anything else.
»MORE: Side Effects of Cancer Treatment

Dealing with side effects
They sent me to a neurologist. They did all the tests. All the tests were negative. They were absolutely convinced I had carpal tunnel. I did not.
They finally agreed that it was the Sprycel. I would try Voltaren gel at night for inflammation. That didn’t really help.
I tried those compression drugs. That didn’t really help. I tried Claritin for bone pain. That helped somewhat.
I had back muscle spasms or musculoskeletal pain. I used heating pads, I used Voltaren gel, and I used ice.
There were some times that I was literally down 2 or 3 months, and I just couldn’t get up. Everything hurt so bad.
Talk about boredom! You just get sick of your own self. You really couldn’t watch TV because you couldn’t focus. You couldn’t read a book because you couldn’t focus. What do you do?
I ended up teaching myself to crochet all these cute little animals for my grandkids, which aggravated my hands. It was like there was just no way to win.
With the neuropathy in my feet, I could hardly walk. That went on for the better part of 3 years, off and on.
CML treatment’s impact on quality of life
It drastically changed my life. I could not just say, “Next Tuesday, let’s go to a movie.” Never. Maybe I could go and maybe I couldn’t. They stopped inviting me because half the time I had to say I couldn’t go. I did not know from moment to moment.
Because CML is forever, you just hope that eventually it will level out, your body will adjust, and you will get to a better place.
Lot number correlation
I started writing down my symptoms daily. What I found was that my side effects correlated 100% with the lot number of the drugs that I took. With different bottles, every 30 days I felt different side effects. If I got a good bottle, it was a great month. I could do more things.
Because my drugs came from mail order, it had to come from a specialty oncology pharmacy. When I got a good one, I would ask the person filling my order, “Could you look for this lot number?”
I had one person who would do it, and it was the best 6 months of my life during that time. For 6 months, I felt great, and then I got a crappy bottle and went back down.
I held out hope that eventually they would come up with a better drug or maybe a cure.
They call it a new normal. It’s just a new normal. It’s hard because I was always flew by the seat of my pants and did whatever I wanted, whenever I wanted. I never, ever considered I might not feel good enough to do that.

It never entered my consciousness that I would have to live with, “How do I feel today and can I do it? I’m going to suffer if I do it.” I would go dancing on occasion when I felt good. I was wiped out for two days, but it was worth it.
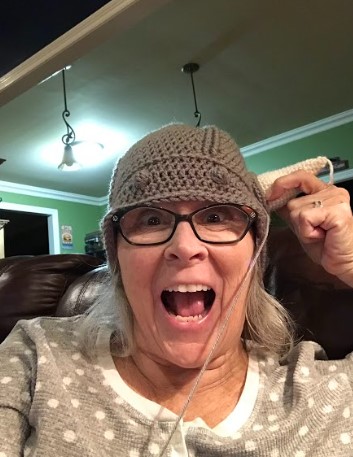
What helped you through the physical, mental and emotional strain?
I started crocheting little things for the kids to keep my hands busy, to keep my mind focused and to learn something new. I started watercolor. They were just different things than what I used to do. They were different ways to fill the time and the space and they didn’t take a lot of energy. I can see how it would be very easy to become depressed.
My hair just grew out. I looked ridiculous. I didn’t care. I had cancer. Who cares? All of a sudden, you really just don’t care.

Michele’s blog
I started writing a blog to keep my friends and family informed as I learned about CML, what that meant, what my treatments were and what I was doing.
I put it on a blog because when you get sick, people start calling. It’s exhausting. My poor husband had to deal with all the calls because I didn’t have the energy or the emotional stability to keep saying, “I have cancer.” It was so hard. I told my children, and it was the hardest thing I’ve ever done.
I started writing this blog because as I learned, I wrote it down. My friends and family could read it, and they could understand what I was going through and how I was feeling at the time. That was really, really helpful.
Back then, there weren’t so many Facebook groups. There was very little on the web about CML at the time. People died, people got diagnosed older, or they weren’t on the computer.
I started hearing from people all around the world. They were saying how helpful it was. On my bad days, I wrote about my bad days; on my good days, I wrote about my good days.
I started sharing what living with CML was like. That gave me an outlet. The people who reached out didn’t have access to good care, or they were afraid to stand up for themselves. It helped me to help them.
I never in a million years would have dreamed my life would become an open book. If anybody wants to know anything about me, just go read my blog. It’s all there: the good, the bad and the ugly.
»MORE: Breaking the news
Dealing with hair loss
My hair was just falling out in buckets. It is so thin right now. Even still, I barely have that much hair on my head.
The other very interesting thing with Sprycel is that all of a sudden, my hair was completely white. I had dark hair. My skin was extremely white as well.
I went to my oncologist, and I was like, “What’s up with this?”
He was like, “It’s the Sprycel. It takes the color out of your skin and your hair.”
I was like, “Oh my God, can I dye my hair?”
He was like, “Well, you already have cancer. It’s a bunch of chemicals. I guess you could if you wanted to.”
I thought about that, and I just let it grow out. I looked ridiculous, but I didn’t care. I had cancer. Who cares? All of a sudden, you really just don’t care. My hair grew out; my skin was white.
»MORE: Hair Loss and Regrowth

Heat and sun exposure
We were in Europe. There was a transportation strike in Rome, and we walked miles to get back to where we were staying. When I looked down, my legs looked like hamburger. All of the blood vessels in my legs were bright, splotchy red. I was mortified.
I took pictures and sent an email to my oncologist, asking, “Do I need to come home?”
He was like, “No, just try and stay off them for the next couple of days. It should be okay. If it gets like that again, just try and stay off of them.”



We were getting on a cruise, so I was in a wheelchair for like 4 days. I got better and walked around. They were fine, but it happened again. Interestingly enough, I had 3 people come up to me and ask me if had cancer. I was like, “Yeah, why did you ask me that?”
They were like, “Your legs. My husband has cancer, and his legs are doing the same thing.”
It was the heat. I couldn’t be in the heat at all on Sprycel. I couldn’t be in the sun. Apparently, all the capillaries would burst close to the skin from walking, so that was fun.
I had a chilipad. Those things are so fabulous. You wet them and put them around your neck, and they stay cool for hours. I’ve got a personal fan that goes around my neck because I’m very sensitive now. It’s not as bad on the Bosulif as it was on the Sprycel.
Pleural effusion
Probably the most dangerous side effect was the pleural effusion, which is where the sac around your lung fills with fluid. The first time I had it drained, they took 2 liters out of my lung. I walked out, and I was like, “Oh my God, I can breathe.”
That sadness gets you. It’s just that emotion. It’s just something that I miss within myself.
I didn’t really know at first. I kind of had a cough, and it was just annoying. It was like a dry cough. It did seem like if I tried to take a really deep breath, I just couldn’t quite get a deep breath.
For the first year or so, it was controlled by going on Sprycel breaks. My doctor was like, “Let’s take you off for 10 days, until the pleural effusion begins to clear. Then we’ll try you on a lower dose.” I was on so many doses of Sprycel.
Losing a spark of yourself
The very first time I was off the Sprycel for 10 days, on the third day I felt like me for the first time. It was this little spark.
My husband came home from work, and he was like, “What’s up with you?” I was literally giddy. I was happy. It’s not that I’m a sad person or a depressed person. It’s not that I’m a pessimistic person. I didn’t think any of those things.
I didn’t even realize I was missing this little spark of joy. I called it Sprycel sadness. It was like a dark cloud. It was like it just dampened who I was. I never realized it. I didn’t know that it made me feel duller, but it absolutely did that kind of stuff. The Sprycel breaks were pretty great.

Living life
It’s hard to explain if you haven’t been there. It’s just a little tiny spark that’s missing. It takes something away that you didn’t even know you were missing until you have an opportunity to revisit it. It’s not like I sit around and mope [or like] I’ve canceled the rest of my life.
I try to live my life to the best of my ability every day. That’s why I take the medication — because I love life. I love my life. I’m fortunate. I’m blessed. I’m grateful, but there’s a tiny little spark that’s just missing. I can’t even explain it.
If you think about it, it can make you a lot sadder than just a moment of sadness. It just makes me teary.
My mother’s passed away, and I love my mother. If I think about my mother too much, that sadness gets me.
It’s just that emotion. It’s just something that I miss within myself. You wouldn’t know if you didn’t know. Nobody around me would know.
Switching Treatment and Doctors
My doctor probably told me that I could switch for a year. For a year, I was like, “No, I’m good. I’ll just get my lung drained every couple of months”
You get comfortable with something. At that point, I felt pretty good otherwise — or so I thought. I’d adjusted. The hand stuff was sporadic. The headaches had kind of gone away. I felt like I had more energy than I had in the beginning. I felt like I had adjusted pretty well to Sprycel, and it was keeping my leukemia at bay.
It wasn’t the greatest PCR results, but it was good. My doctor had said that it was good enough and that he thought my prognosis was good long-term.
I was comfortable with it, and I understood Sprycel. I knew Sprycel. If I switched, I had to make a choice between Tasigna and Gleevec. Neither one of those sounded better than what I was already on.
Plus, if I gave up on that one, then I’d only have 2 more choices if my leukemia became out of control. Every 3 months, you have to be tested because it can become uncontrollable at any point in time. I kept sticking with Sprycel.
Draining fluid from lung
I even went to a pulmonologist. They said there’s a procedure to put powder between your lung and the pleural sac. It causes scarring, and it causes the sac to stick to the lung. Then the pleural effusion can’t happen anymore.
My thoughts went to, “The fluid doesn’t go there. Where does it go? You have a sac around your heart. Oh, great. If I have to get a pleural effusion, I don’t want it around my heart.”
This went on and on, and I just started getting my lung drained on a fairly regular basis. I was like, “Can they just put in a drain, and I can just drain it out every day? I’m good with that.” They were like, “That is an option if this continues.”



Fast-forward another year, and I had to have rotator cuff surgery. I had to have it drained the day before surgery. They checked me with an X-ray right before surgery. They had to drain it again that morning.
What was supposed to be an outpatient surgery — they were already going to keep me overnight because of the CML — ended up being a week in the hospital on oxygen. I went home on oxygen for several months.
Switching to Bosulif
I was like, “Okay, I think now’s the time to change.” At that time, Bosulif was an option.
Its biggest side effect for people seems to be massive diarrhea. I travel. I like to go places, and I like to fly. I was like, “I can’t have that. I don’t want to be homebound constantly.”
I was like, “Okay, I’ll try it.” Bosulif is known for that and nausea, so we pre-medicated with Zofran.
Being a CML specialist, my oncologist said, “Start on 100 milligrams. 400 milligrams is the desired dose. Start at 100 milligrams for a week. If you tolerate that well, go up to 200 milligrams. Give your body time to adjust. This drug is one of the hardest to start.”
It’s rough. It is difficult. By the time I got to 300 milligrams, I couldn’t tolerate it. The nausea was so bad. I asked, “Can I split it to 200 and 200?”
“Yes.”
All doctors that aren’t CML specialists will say no. They will give you a 500 milligram pill and start you out on that, and they can’t figure out why people fail the drug. It’s because they’re setting them up for failure.
»MORE: Managing Nausea and Vomiting
Alleviating side effects
I use Preggie Pops. My friend sent me those off of Amazon. They’re little sucker things. They use them for pregnant women.
I did the pressure things for the motion sickness. I tried Zofran.
What works the best for me is CBD drops. No THC, just CBD drops. If I start getting nauseous. I put 3 drops under my tongue. At first, I rolled my eyes and went, “There’s no way this is going to work.”
It works every time. It’s crazy. I cannot believe it. Another cancer patient gave me her drugs when she finished her chemotherapy. I was like, “I’ll try anything.”
For me, it wasn’t the diarrhea, which is a good thing. It was the nausea. I have way more energy on Bosulif once I adjusted. I can go out in the sun. My hair’s getting a little darker. It’s not as white. I have a little color in my skin. All of those things are good.
At one point, Bosulif had to be your second TKI. I don’t know if they will yet start people on it. I think they might, but I’m not sure about that. It was at the end of 2017, I believe, and my oncologist had 5 other patients who were on it and doing really well.

The importance of preserving treatment options
It’s a little hard.
- You get comfortable with what you’re taking.
- You know you have these options. There’s always a chance that it might stop working altogether. At that point, you have to go to another option.
Fortunately for CML, they seem to keep researching and coming up with new options. They also have another one called ponatinib for people that have a mutation in their CML. They’re also coming up with trying treatment-free people.
You have to take all of these things into consideration when you’re choosing what is best at this moment, at this point in time. It is helpful to talk to other people. I have a Facebook group and my blog. I hear from other people and hear what their experiences are. Some are helpful. Some are just downright terrifying.

People think, “You have CML. You’ll be fine.” Unfortunately, that’s not always the case. I’ve lost many people that I’ve met over the years with CML. They have gone into blast crisis, had bone marrow transplants, second bone marrow transplants, and they don’t live.
A lot of people do get diagnosed routinely through routine blood work. If they’re going for a new job and want to have a physical for whatever reason, they get diagnosed very early. They get treated very early. Their CML is non-detectable within 6 months. It’s great.
There’s plenty of people who don’t. For me, they pretty much said it’s never going to be an option for me to be treatment-free. It’s probably because I explained away all my symptoms in the beginning, and I was diagnosed further into the disease than many other people.
Why are you working with 2 doctors?
I was happy with my doctor in Los Angeles. My husband retired, and we moved to Boise, Idaho. When we were in Boise, we went to a dance event in Portland, Oregon.
Portland, Oregon, happens to be where Dr. Druker, who developed Gleevec, practices medicine. I was like, “Why wouldn’t I go see him?” He is like the Grand Poobah of CML. I made an appointment with him and loved him as well.
I would see him once or twice a year. Then I’d see my doctor in Southern California once or twice a year. I fly once and do virtual once usually, but it works out for me because I have family there. I just use it as an excuse to go. Fortunately, I’m retired and can.
If you need to fly to see a specialist, specialists will see you. They will establish you as a patient, and they will work with your local oncologist. It’s so worth it.
I just want every single person who has CML to see a specialist, and it doesn’t happen. Those are the people that seem to not do well and actually have passed away.
I see Dr. Druker. He sends me a blood kit. I have it drawn here. They ship it back to Portland. Then I’ll do a virtual doctor’s appointment with him.
Lessons learned
What advice do you have for others in your situation?
Honestly, I don’t think it necessarily ever gets easier. Somewhere along the line, there came a time when I didn’t think about it every single day.
Then the other problem with having cancer for the rest of your life is with every ache and pain, you’re like, “Uh-oh, what’s that? I hope that’s nothing.” That is not great.

The one thing that I’ve learned more than anything is that you need to be your own self-advocate.
That’s not much fun, especially in the middle of the night. I’ll say to my husband, “If I die tonight, it’s probably a brain tumor. It’s right here, because it hurts right here.”
Lingering anxiety
It puts you on edge. My logical self says, “Stop it.” My brain is like, “Uh-uh.” It’s that little guy sitting on your shoulder.
There are days I go through a whole day and don’t remember that I have cancer. Then I know I have to get blood work.
I get my blood drawn. We do a happy dance over it; we do good juju. Then they send it off. I have to wait a week or 2, and then I see the test result pop up.
I want to look, but I don’t want to look. Sometimes it’s gone up, and I’m like, “Okay, it’s only gone up a little.” Then you’ve got to stress for the next 3 months — is it going to go up, stay the same, or go down?
Then I had a great one. I was so excited. It was just the best. I put off getting my next 3 months for like 3 weeks. I was like, “I just want to live on that really good one for just a little longer.”
I finally did it 3 weeks late. It got compromised in the mail. I had to redo it, so I’m still waiting for that result. I don’t know that it ever really gets easier. Unfortunately, you just don’t know, but nobody knows.
The importance of self-advocacy
The one thing that I’ve learned more than anything is that you need to be your own self-advocate. You need to stick up for yourself. It’s important to understand what’s going on in your body. It may be scary, but I truly believe that not knowing is probably scarier.
If you’re in the hospital, have an advocate with you. You’re too sick even to stand up for yourself. I feel like every single person that’s in the hospital needs somebody there standing by their side and trying to do what’s best for you.
Don’t be afraid to stand up for yourself. Learn about your diagnosis, learn what your options are, and fight for you. You know you better than anybody else ever, ever will. You just need to do that. It’ll make you feel good, and it’ll help.
»MORE: Advocating for yourself


Inspired by Michele's story?
Share your story, too!