Velcade Side Effects & Patient Stories
Velcade (bortezomib) is a chemotherapy drug approved for use in the treatment of multiple myeloma and mantle cell lymphoma.
Velcade is also considered a targeted therapy in the class of drugs that is sometimes referred to as proteasome inhibitors.

What Is Velcade’s Mechanism of Action?
The mechanism of action for bortezomib is that it slows down or blocks the action of proteasome in both cancerous and healthy cells. Proteasome plays a major role in cellular processes.
How Is Velcade Given?
Velcade (bortezomib) treatment is administered via injection into a vein. A special port or line is not necessary, but you can use those if you already have one in for another cancer treatment.
What to Expect After Velcade Treatment
If an oncologist or other healthcare provider has recommended Velcade for multiple myeloma, mantle cell lymphoma (MCL), or other cancer for you or a loved one, you may wonder about bortezomib side effects.
Velcade’s manufacturer lists the following as possible side effects:
- fatigue
- peripheral neuropathy
- low blood pressure (hypotension)
- heart problems
- lung disorders or problems
- liver disease or problems
- hematologic disease (thrombotic microangiopathy, [TMA])
- posterior reversible encephalopathy syndrome (PRES)
- gastrointestinal problems (nausea, vomiting, constipation, and diarrhea)
- low levels of neutrophils and leukocytes, which are types of white blood cells (neutropenia and leukopenia), and low levels of platelets (thrombocytopenia)
- tumor lysis syndrome (TLS)
- low level of red blood cells (anemia)
- rash
- fever (pyrexia)
- decreased appetite (anorexia)
Velcade Patient Stories
Here’s what some cancer patients have to share about their Velcade treatment experiences:
The next treatment, which was three weeks later, Dr. Greenberg came in and said there was a Phase 3 trial of adding Velcade to Rituxan, that monoclonal antibody.
Velcade has been very effective for multiple myeloma and there are some similarities between multiple myeloma and mantle cell lymphoma, so they wanted to see if it would help.
So on the intervening two Mondays, I went in for four hours. I’d get an infusion of Rituxan and Velcade. They had an infusion for the Rituxan and then injected the Velcade into the line, and that was it. That was usually just a four-hour thing.
I’d go in the morning, then went home, and after I had some lunch, then went to work. So overall, Monday I’d have R-CHOP, then the next two Mondays I’d have Rituxan with Velcade, and then the R-CHOP again all over again (for six cycles).
No. I went to work everyday except for the all-day chemo. For R-CHOP I was there for close to eight hours each time. Then I’d go home and take a nap. That Benadryl just made me sleepy.
I really didn’t have any other effects. On the weekends I went biking with my bike club. I didn’t know any different so I just did what I felt like I could do.
Shari B. (Mantle Cell Lymphoma, Stage 4, Non-Hodgkin’s Lymphoma)

The steroid is just a pill. It’s dexamethasone. Velcade is the (targeted therapy) chemo, and it’s an infusion. I didn’t need a port or PICC line
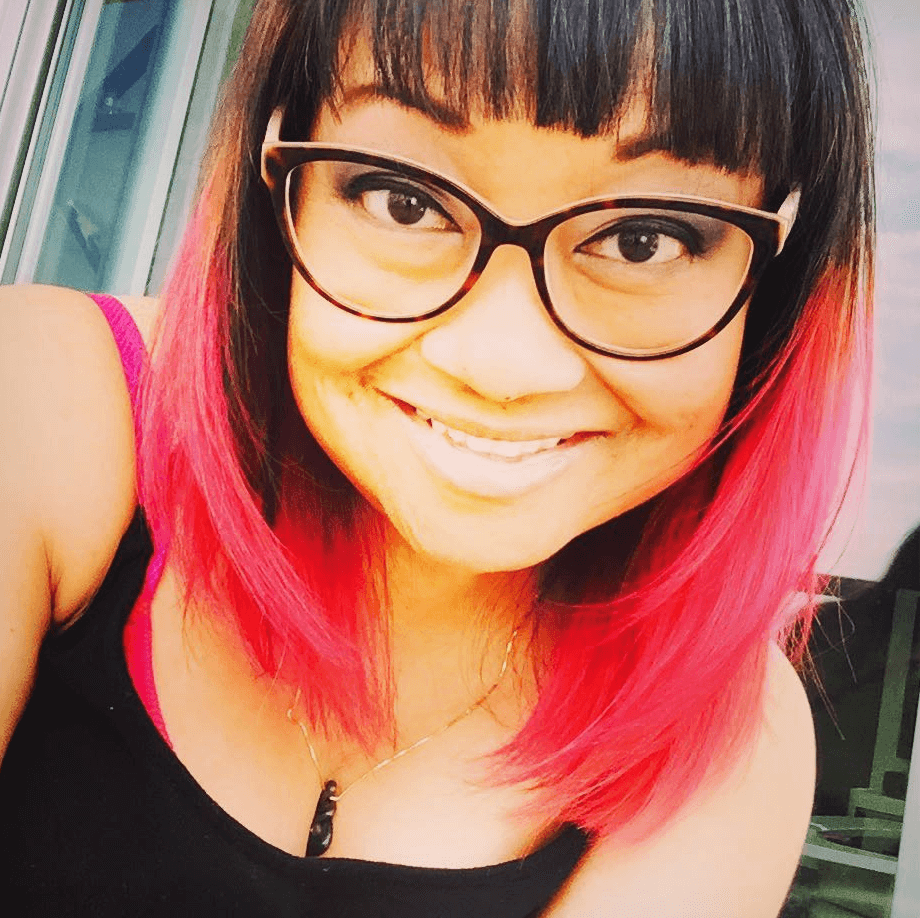
I was on a high dose of Velcade, so I would go in twice a week to get infusions. I would take Revlimid every day, and I would take the steroid the day of the infusion and the day after. I did that for three weeks, and then I would have a full week off from treatment. I was in the hospital for about five hours every time I went in.
Exercise was something that I’ve always done, thank goodness. Going into treatment, it wasn’t as hard for me to do it. I would just walk a lot.
The night of my infusions, I would be really sick and nauseous. I would take some Zofran to help with that. There was really just no helping it though. Nausea was a big problem.
A lot of people in the myeloma community say they gain a lot of weight during treatment. It was kind of a balance of being nauseous and craving things. When I was nauseous there wasn’t really much to help it except maybe bananas. I ate a lot of bananas.
Melissa V. (Multiple Myeloma, Active Myeloma, Stage 3)
I was scheduled for my second, and that’s when I had the fever. I didn’t have my second round until I got to the third hospital. He put me on a different cocktail. It was Darzalex, Velcade, and dexamethasone.
I hated the Velcade because it was subcutaneous, so I had a lot of bruising with that.
If there were four things that I could tell people to do, that would be: eat, hydrate, exercise and sleep.
Your body needs fuel to fight. I always had a big breakfast. I numbered my cups of water to ensure I was drinking enough.
I forced myself to get out of bed and walk. I had to do PT as well for the thigh surgery. They wanted me to exercise and walk. I walked around the nurses’ station.
It was hard to sleep being hooked up to so much stuff, but I tried my best to sleep.
Juda A. (Multiple Myeloma, Stage 3, Surgery & Chemotherapy)
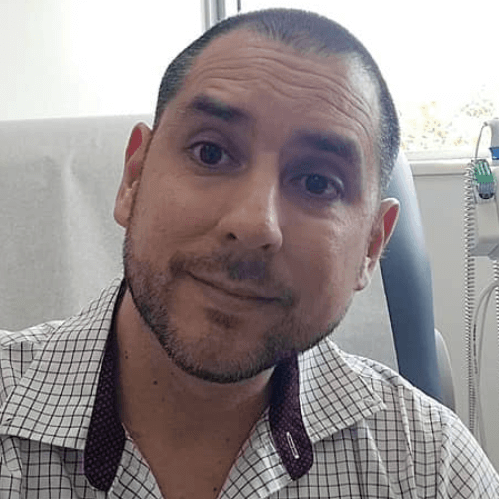
The doctor chose RVD, or Revlimid, Velcade and dexamethasone. That’s immunotherapy, targeted therapy, and one steroid.
Velcade was two times a week for two weeks and two weeks off. It’s an injection they give you at the hospital and it goes into your stomach. That was definitely not fun. They inject it very slowly. It burns a lot.
A side effect that I would get the day after my Velcade was the hiccups. The first time I got them, I tried the usual known remedies like holding my breath and drinking water quickly.
After turning blue and drinking two liters of water with no results, I researched online and found that some hiccups may be caused by stomach indigestion. I took a TUMS and problem solved.
I am a firm believer in eating well and by that I mean eating for nutrition. Lots of organic vegetables, eggs, green juices, along with some fruits.
In addition, I do intermittent fasting. That’s when I eat two times a day, once at 1 pm and once at 7pm, [which I read] help your cells clean out damaged cells, a process called autophagy.
Apple cider vinegar really helped me with any intestinal issues or heartburn. I took all types of different teas. I was already on enough pills, so I gave the alternative medicine thing a try.
In general, it really did help. Eating well and exercising even if it was just a little bit every single day was a big deal.
I would go outside and walk to get some vitamin D, which is extremely important for your bones and immune system. I believe all those things really helped to not feel as much from the side effects.
Carlos C. (Multiple Myeloma, Light Chain, Stage 2)
All Velcade Patient Stories
Laura E., Multiple Myeloma, IgG kappa
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
...
Valarie T.
Symptoms: Nose bleeds, fatigue, back pain
Treatment: Chemotherapy, stem cell transplant
...