Madi’s Stage 1B Nodular Sclerosis Hodgkin’s Lymphoma Story
Madi was diagnosed with stage 1B Hodgkin’s lymphoma at just 24 years old. Explore her story on how she used self-advocacy to get diagnosed and underwent ABVD chemo to get into remission.
Madi also shares how she navigated the hair loss, the support that meant the most, and the impact of cancer on her relationship.

- Name: Madi J.
- Diagnosis:
- Hodgkin’s lymphoma
- Classical: nodular sclerosis
- Staging: 1B
- 1st Symptoms:
- Shortness of breath
- Difficulty breathing
- Treatment:
- Chemotherapy
- ABVD, once every other week for a total of 6 infusions
- Chemotherapy
If you don’t feel inspired or led to be the ‘inspiring cancer warrior,’ then don’t. Not everyone feels like it.
People always say, ‘Use your story for good!’ Well, yeah, but only if you feel like it.
There’s so much pressure on cancer patients to be strong through treatment and use their story for some greater purpose. I don’t think you need to feel pressured into that. Do what you feel is right.
Madi J.
- Diagnosis
- What were your 1st symptoms?
- First doctor's appointment, tests and scans
- How did you get news of the mass?
- You had to advocate for yourself
- Describe the moment you got the cancer diagnosis
- How did you process the Hodgkin's lymphoma diagnosis?
- Describe the first oncologist appointment
- How did you approach the issue of fertility preservation?
- ABVD Chemotherapy
- Remission
- Hair Loss
- Reflections
- What was the lowest point for you?
- What helped you during those moments?
- What’s your advice for people who want to help but don’t know how?
- Can you talk about self-advocacy?
- Do you have any advice for someone who is nervous to self-advocate?
- How did the cancer affect your relationship?
- Financial toxicity: paying for cancer treatment
- Message for patients
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your 1st symptoms?
I really just couldn’t breathe. That was the only symptom I really had. I was going to the gym 5 or 6 days out of the week.
I was biking 10 miles a day, and all of a sudden, I was calling my mom after my workouts. I was super fit, so I was telling her it was getting harder, and it was weird. She said I was probably just working out too hard.
I took it a little easier and it wasn’t getting any better. Then it got to the point where it was just sporadic. I would be driving in the car, and I’d feel like an elephant was sitting on my chest.
First doctor’s appointment, tests and scans
I went to my doctor, and they did pulmonary function tests, EKGs, EEGs and every test under the sun to see what was going on. Then they did a CT scan, and that’s when they saw a little mass in the center of my chest.
I started going to the doctor on August 8th, and I wasn’t diagnosed until October 1st. The placement of the tumor was really weird. It was on my phrenic nerve. It was in my mediastinum.
It was right in between my heart and my lungs, so they kept sending me to specialist after specialist to see what it was without actually going in and biopsying it.
How did you get news of the mass?
At first, they said, “Well, it’s probably just anxiety.” Then they did the pulmonary functions test. My O2 stats were all really abnormal.
They sent me to a cardiologist, who told me everything was fine with my heart. From there, they checked for blood clots. Then the CT found the mass.
You had to advocate for yourself
I went to a pulmonologist who really pissed me off. I was his last appointment of the day, and it was a Friday. I walked in, and he said, “I’ve already reviewed everything. Your mass isn’t concerning to me at all. Let’s just do an asthma test.”
I was like, “Okay? I’m 22? Isn’t childhood asthma a thing? Would I just be getting it?” We did it anyway, and everything came back normal.
He said it was probably just anxiety. He said the mass looked like it was my thymus gland, and I was like, “Aren’t those usually gone by the time you’re 17 or 18?”
He said we could biopsy the mass if it would make me feel better, so he called around to some of his surgeon friends to see what we could do. He called me back within a few days and said no one there would be comfortable biopsying it because of the placement.
He said there was one doctor who would consider it, but I’d have to sign a release form. They were going to cut me open like open heart surgery.
They told me it wasn’t advisable because it was most likely just my thymus gland, and I’d have to undergo a major surgery in order to biopsy it.
I said, “Okay. That’s a risk I’m willing to take, but I don’t want open heart surgery, so I want you to send me somewhere else.”
About a week later, the lady at the desk called me and said she got me in at Emory. I was set up with a cardiothoracic surgeon, and then the surgery.

Describe the moment you got the cancer diagnosis
He came in after the surgery, and he was holding my hand. He said, “We were able to take the tumor and some surrounding lymph nodes. We got your pathology back. Preliminary results show that it’s Hodgkin’s lymphoma.”
I didn’t know what was going on or what that meant since I was so groggy. My mom was just crying, and I was out of it.
He came in the next day and explained everything. I think I was in denial because so many different doctors had told me it was nothing to worry about. I tried to argue with him and told him his preliminary results were incorrect.
I said, ‘Unless you know without a shadow of a doubt that I am walking out of here as a cancer patient, I don’t want to hear it.’
On October 1st, he called me and said I definitely needed to see an oncologist as soon as possible. He was going to get me set up with one there.
He said, “Good news, it hasn’t spread to any of the surrounding tissue we took, so I’m pretty sure that means you’ll be staged pretty low.”
How did you process the Hodgkin’s lymphoma diagnosis?
I was just kind of in shock. I was confused. We had a cruise scheduled on October 8th. That helped me keep my mind off of it. I got to go on that vacation, not be on chemo, and not really have to think about it yet.
I don’t know when the reality of it all set in. It wasn’t right away. When I talked to my mom, I was like, “Okay. This is going to be something new. We’re just going to have to figure it out.”
I had lost my grandmother to cancer a few years prior, so I knew we had to do whatever it took. I hadn’t had time to research any survival rates or anything. I wanted to go into the first appointment without any fear that the internet put in my head and just do what she said.
The only thing I really researched beforehand was freezing eggs. With me being so young, I asked her what I needed to do there. That was really the only thing I looked up before going in.
»MORE: Patients share how they processed a cancer diagnosis
Describe the first oncologist appointment
It went well. She kept pausing as she was explaining things and looking at me. I was like, “Keep going,” and she said, “Well, it’s just that this is normally when people start crying.”
I said, “No, the reality has come and gone. I’m not going to cry about it.” She said we were super understanding, and she was super appreciative of our openness about everything.
How did you approach the issue of fertility preservation?
As far as freezing eggs, she said that wasn’t necessary since I was 1B and only needed 3 rounds of chemo. I had a total of 6 infusions.
She said, “Since you have an IUD in, we don’t need to freeze eggs. If you just want to, we can, but it’s going to delay treatment.”
I wanted to just get it over with, so we opted out of that.
She said I should be pretty responsive to the chemo. She told me about the ABVD. She told me I’d do every other Thursday, and as long as my PET scan showed that everything was going the way it should, I wouldn’t have to do radiation.
»MORE: Fertility preservation and cancer treatment

ABVD Chemotherapy
Can you talk about getting the port inserted?
It was terrifying. They explained that the ABVD chemo regimen is one of the more vicious chemo regimens to have. Plus, I’m such a tough stick, so they said it would collapse my veins if I didn’t get it.
It was outpatient. I was in and out the same day. It hurt a lot. I still have a ton of discoloration from it. My body just didn’t react to it very well. It was sore. It was scary because of the way they had to go up through the vein through my neck.
My blood pressure kept bottoming out when they were putting it in. Of course, the whole time I was thinking, “This is going to be what kills me because I’m gonna bleed out my port.”
Lidocaine cream is something I would suggest for anyone who has to take the port route.
The way your skin is stretched makes it so sensitive, and you have this big marble underneath your skin.
Also, the needle is so long and has to be thick for the chemo to go through it. It’s just a mess. I would highly recommend the cream and maybe some Xanax before you get it accessed.
My nerves are so shot still. To this day, I’ll rub the area sometimes. It itches and hurts sometimes. It’s good when you have it, but it sucks getting it and sucks when you get it out.
How long were the infusions?
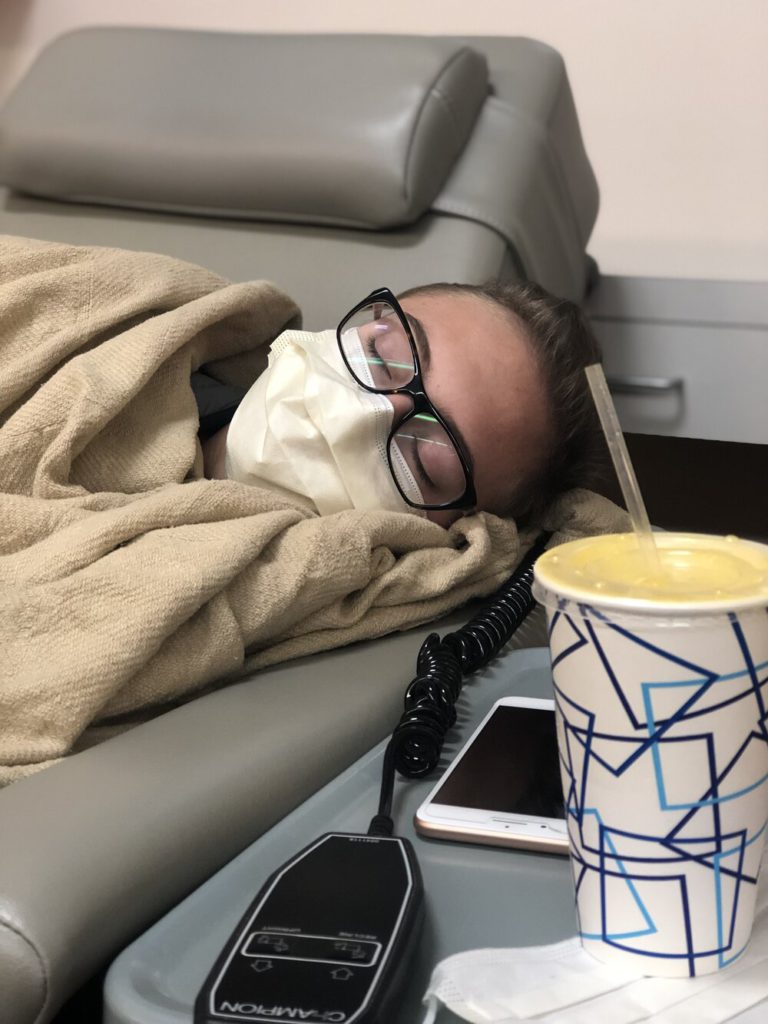
Infusions were once every other week, and they were outpatient. I just went into the infusion bay. It probably took 6 hours, give or take.
Describe the ABVD side effect cycles
The “red devil” was push chemo. That typically went by pretty fast. That one didn’t do a whole lot to me during the infusions. I only had 2 infusions of the bleomycin because it was destroying my lung function so bad. They had to cut it out.
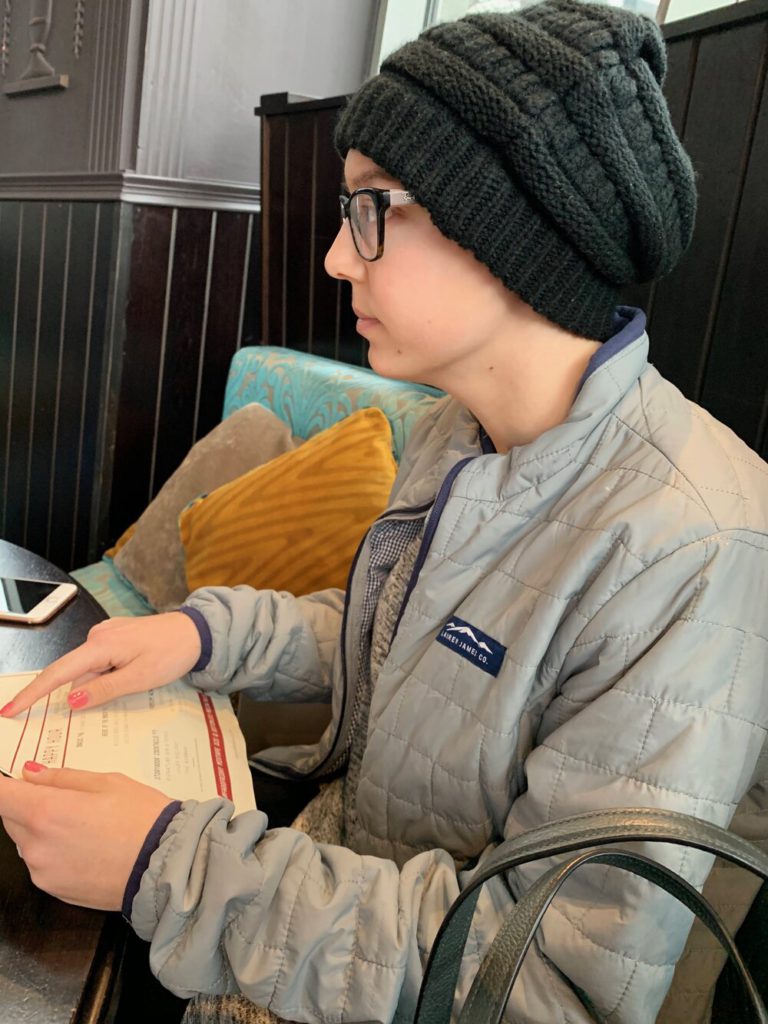
Once I got to the vinblastine, I was just so exhausted. I pretty much slept through that and had the dacarbazine. That was light sensitive, and it was wintertime thankfully. Any time I would go out in the sun, it was so sensitive. I had to wear long sleeves and hats.
It was rough. I had to take a bunch of different medicines, and my body had to get used to it. I had 14-day cycles. The first 5 days, I pretty much just slept. Those were absolutely the worst times of my life.
The next 5 days were okay. I could get up and take a shower or make myself something to eat. I couldn’t usually get out of the house, but I could get out of bed. I’d have a little bit of an appetite.
The last few days before my infusion, I had a little bit more energy. If I had to get out and do anything, I could.
I would respond to text messages that people had sent in the previous 10 days because I finally felt good enough to give a genuine response.
There was only one time during the chemo that I felt miserable enough to think, “This is it.”
Everyone told me that the survival rate with Hodgkin’s was so high, but typically people that die from it actually die because of complications with treatment, like a secondary infection.
I got severely neutropenic. I was passing out. I couldn’t stay hydrated. I went from almost 140 pounds to 103. I went to my local ER.
They didn’t have a hematologist or anything. I had a person who didn’t know what she was doing trying to start my port. I kept passing in and out. I think I slept for 72 hours, and I kept pulling my beanie over my head because the light was hurting my head. I just felt so bad.
The ER called an ambulance for me to take me back to Emory. I had a 2-hour ride. I was hospitalized for 6 days. My counts just wouldn’t come back up. I had to be on the bone marrow transplant floor. Everyone had to scrub in before they came into my room and wear scrubs and stuff.
That being said, infusions were rough. I never really knew what to expect.

What were the other ABVD chemo side effects?
The nausea was really intense. The doctor gave me 3 different anti-nausea medicines. I would take those pretty religiously post-chemo (infusion) as a precaution.
Have someone that makes you eat and drink something. I don’t know how I would’ve made it through chemo without a support system.
If I didn’t have someone who came home to check on me and say, ‘Hey, this is the same bottle of water I put next to you before I left,’ I don’t know what I would’ve done.
I didn’t really have an appetite at all. Everything tasted terrible. That was a really big side effect.
There was also really bad fatigue. I have 2 big dogs. One is almost 100 pounds, and the other is 52 pounds. I couldn’t walk them or take them to the dog park. I had muscle weakness, too. I had to call my mom or my fiancé to come over on their lunch break and come do it because I couldn’t.
»MORE: Read our comprehensive ABVD chemotherapy info page
Mental impacts of chemo
I never got put on antidepressants during chemo because I’d been on them before, and I just never like the way they made me feel. I told my doctor I didn’t want to be put on them.
I said, “I’ll take something for acute anxiety or panic attacks during this, but do not put me on something long-term.”
I experienced isolation, loneliness and all that. It definitely took a toll on me mentally, but that’s what having a support system is for.
Throughout the holidays, I’m that person that annoys you with their excitement. We always have Friendsgiving. We squeezed 20 people in our apartment.
I had hand sanitizer at the door, I wore a mask, and I got the food before anyone else touched anything. They were all so understanding, and I was so grateful that that was one of my good days where I could get up and move around.
A big mental thing is feeling helpless and useless, but if you try your best to stick to any kind of normalcy, it gives you something to look forward to and get out of bed. We always do a big Santa Swap around Christmas, so looking forward to things like that really helped.
Mentally, it takes a huge toll on you while it’s happening, but also after you’re done. I finished treatment on December 27th, and I think I’ve had 4 CT scans as of September because I get so anxious.
I don’t have the luxury of brushing something off anymore. I don’t get to say, “Oh, it’s probably just a bug going around.”
The long-lasting anxiety is definitely there. I started going to therapy recently because it got to the point where it was getting too heavy.
I wanted to talk about my experience, but I didn’t want to word vomit cancer stuff all over everyone. Therapy has really helped me talk about everything.
Survivor’s guilt sucks so bad. All these people come up to you and say things like, “Oh, my grandma died from that.” I think, “Why didn’t these people make it when we did the exact same thing?” That weighs pretty heavily on my mind.
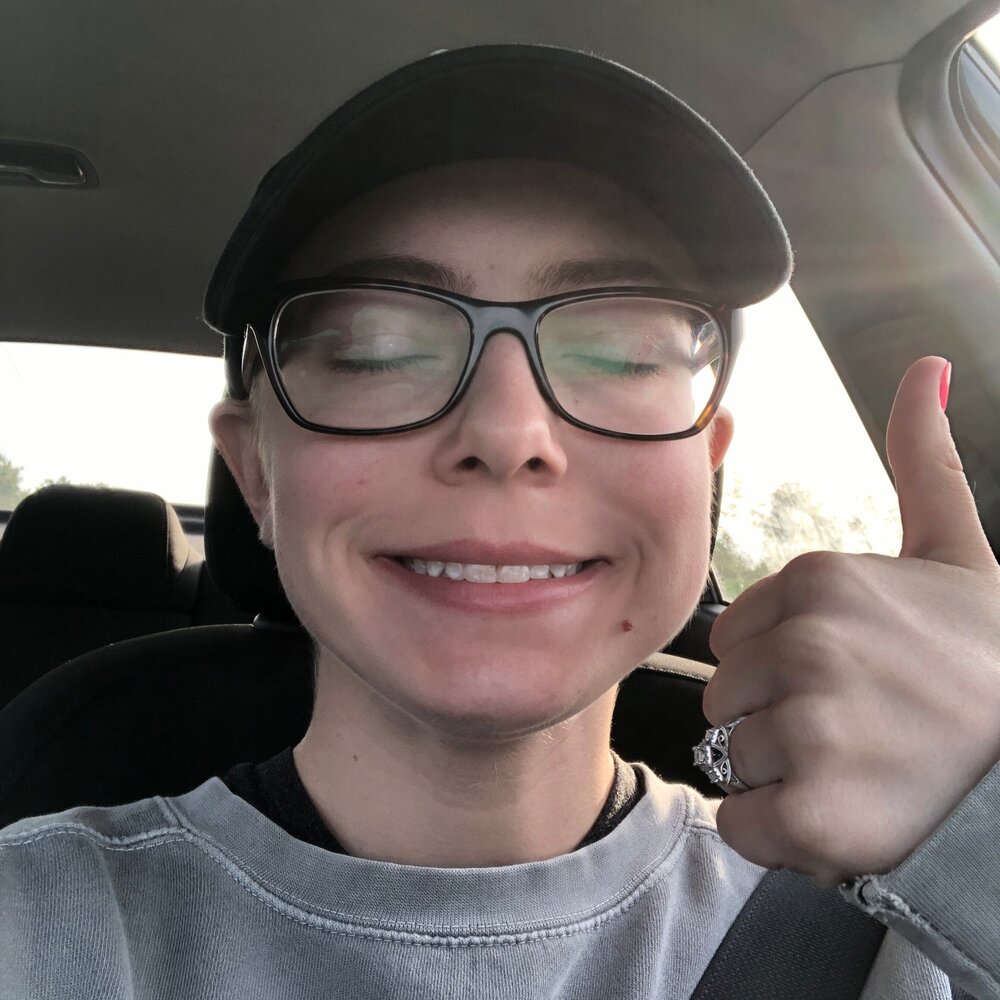
Remission
News of “no evidence of disease” (NED)
January 9th is when I had my PET scan. January 10th is the day they told me I was all clear. I was excited, relieved, anxious, and I was like, “Okay. It’s done. How do I progress?”
Everyone preaches to you about the new normal. I don’t do well with change. My entire life had just been flipped upside down, and now I was needing to create a new normal for myself?
There was also anxiety because I would be seeing my doctor less. I didn’t want my team to be out of the loop.

The bottom line, though, is that I was overjoyed. My fiancé actually proposed to me at the end of my last chemo. I was excited to be healthy. I was excited to know that we were going to be able to start a life together.
I don’t know how people maintain relationships during chemo, especially new ones. If you don’t live together, the rare times you get to see them, your communication is crap. You feel sick, tired, and you don’t have anything positive to bring to the table.
Luckily, I found a guy who stuck through it. He understood. He had his own things going on to help distract him if he needed them. That really helped us.
He had his friends and own support system he could talk to. All that history between us and the engagement gave me so much more to be happy about when I got the clear PET scan.
Has cancer changed your life perspectives?
Yes and no. It’s definitely made me more thankful for the present. It has made me seek out opportunities more, especially things I would’ve been hesitant about before. It’s given me a push.
My new normal is not settling anymore. If I’m unhappy with something, I no longer reason with myself about why I should just stick it out.
If I’m not happy with something, there’s no reason to continue being unhappy.
I recently quit my job. I was miserable. I hated it. They were not understanding at all when I was finishing treatment.
They expected me back to work and ready to go the Monday after I finished treatment. They treated me like I had been on vacation for 3 months. I toughed it out for several months. I felt like I owed it to them.
I finally came to the realization that I don’t actually owe them a thing. I worked my butt off for them for 2 years before I was diagnosed and gave it my all. They maintained my job through treatment because I was a good employee.
My new normal includes a lot of self-love and appreciation.
There was extreme weight loss and gain. It didn’t all come back the way I lost it. My hair fell out and grew back.
I’ve learned that people who are worth being around care about what’s on the inside and what you have to say. Before I got diagnosed, I didn’t tell anyone what was going on except my parents and my fiancé’s parents. I didn’t want all the pity. Now, I don’t really care.
If someone wants to give me false pity or post something on Facebook to make them look better to their followers, whatever.
At least they’re sharing the fact that someone they know is going through cancer, and maybe someone will see it and reach out because they’re going through something similar.
Is there anything you wish you’d known at the beginning of all this?
I wish someone would’ve told me to document it.
It sounds weird, but I wish I would’ve known to be more appreciative of what I was going through, so I could use it.
My mom always tried to take pictures when I was at appointment, and I was always so mean. I did not feel like taking pictures. Looking back on it, I wish I had those memories so I could look back on it and reflect.
No one told me to journal. I wish I had done it, though, because it would’ve been useful.
Humans, what we do when we go through something traumatizing is we block it out. It’s a blank or blurry space in our memories. That’s what that 3 months is for me.
I can tell you I had to stay in bed a lot. I can tell you I lost my hair. I can tell you my infusions sucked, but I don’t know what the actual emotions I was feeling or thoughts I was having were.
That’s a big piece of advice I have for people going through cancer. Document, document, document.
Even if everything you document is negative, and you’re mad at the world every day, document it so that you reflect back on it when you’re on the other side of it.
After cancer, when you’ve locked your keys in the car and think it’s the worst day, you can look back and really ground yourself in the moment. Is locking your keys in the car the worst thing that’s happened?
When your friends want to come see you, and your doctor says it’s okay, let them. Don’t assume that everyone has an ulterior motive. That’s kind of the outlook I had, and I wish I hadn’t thought that way.

I thought, ‘People only want to come see me so they can take a picture with the cancer girl and post it on social media.’
That’s not always true. It might be sometimes, but I wish I hadn’t thought that way.
Hair Loss
Can you talk about the hair loss?
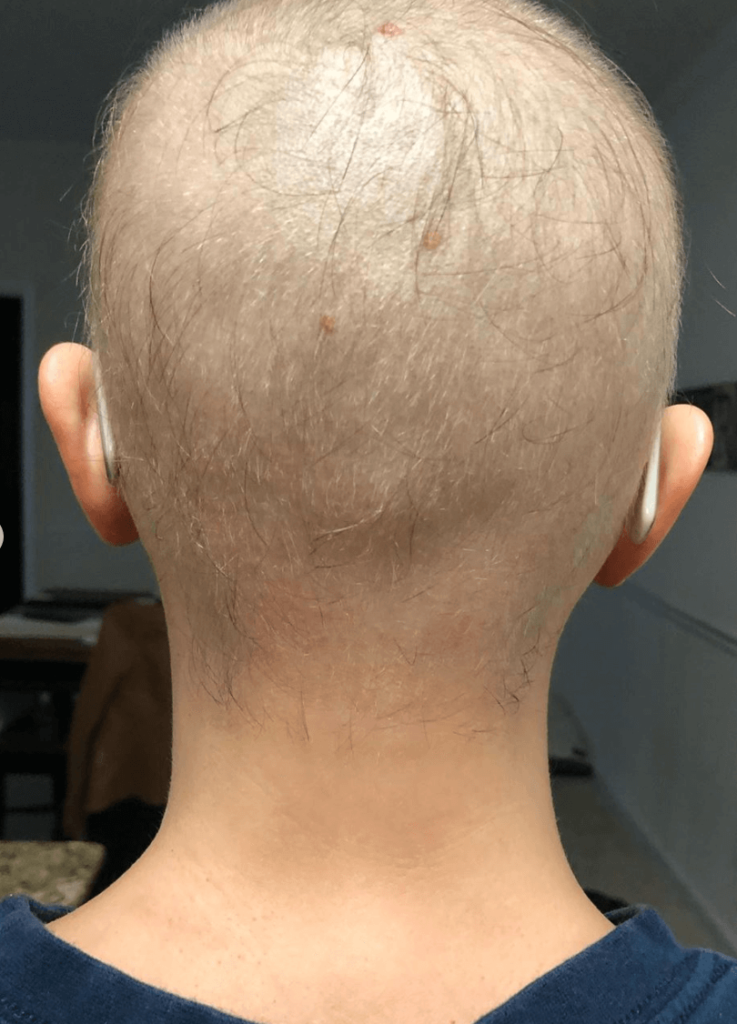
My hair started coming out after the second infusion. That’s when I got hospitalized.
When it started falling out, my hair follicles felt like they were burning. They feel like little sticks in your head poking you.
Hospital beds suck enough as it is. I was trying to get comfortable, but my head was sweating so much. It hurt. It itched. I asked the nurse if I could have some shampoo because I really just wanted to wash my hair.
I can hardly get out of bed at this point, so it’s not like I was checking myself out in the mirror. I had no idea what condition I was in.
I took a shower, and I got back in the bed. I asked my mom if she would brush my hair. It felt so fragile and burned. I needed some kind of relief, so she started brushing it.
Then she said, “Hey, stay right where you are. I don’t want you to fall off the bed, so don’t move.” I hear her drag the trash can across the floor, and I realized what was happening.
She was brushing it, and this sad feeling came over me. I didn’t turn around. I didn’t look. She took the trash can outside of the room when she was done and asked them to take the bag out because she didn’t want me to see it. She called my hairdresser and scheduled an appointment for her to come to my apartment the day I went home.
I could tell it was a lot thinner when I left the hospital, but she cut it so short that it felt like I still have a lot of hair. From there, it just fell out in bigger and bigger clumps. I couldn’t tell what was dog hairs or my hairs. I would wake up every morning with hair on my pillow, and that was emotional.

Did you shave it?
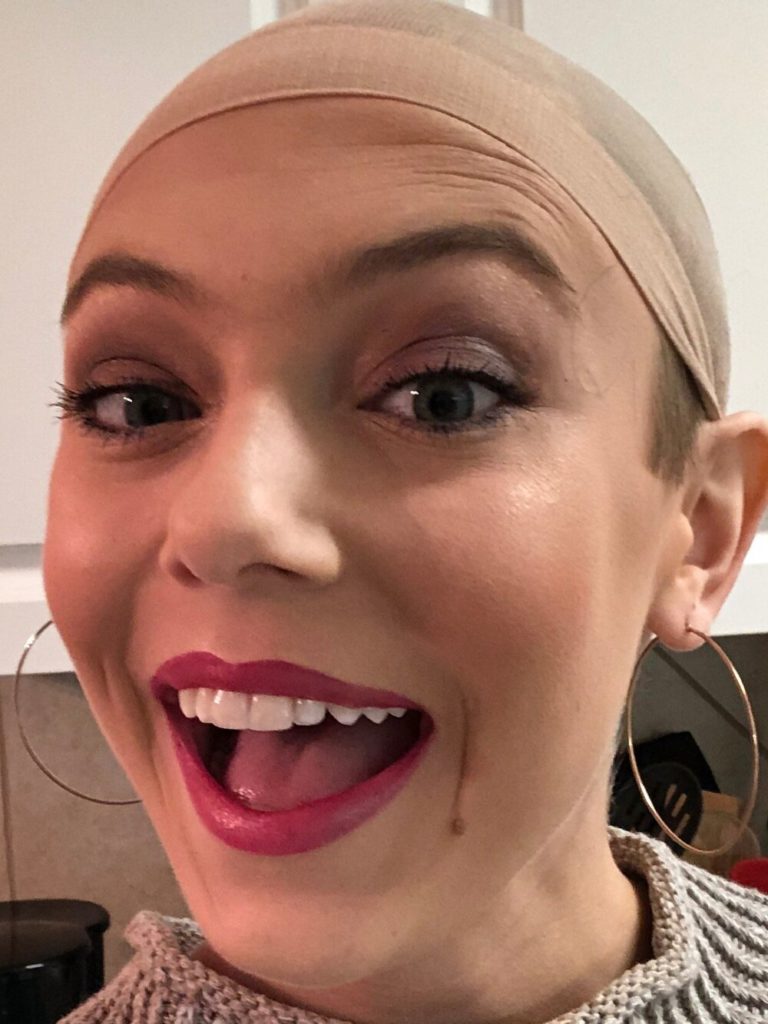
I never shaved it. I cut it to about an inch. I had a love/hate relationship with my wig. When I went wig shopping, I hated everything. It wasn’t my hair, and I didn’t like it.
I didn’t want to shave my hair because even though it was short, I still had some. I was holding out hope that it would just thin out and not all fall out.
It all fell out, though. It thinned the whole time, but the worst was right after the last infusion. That’s when my eyebrows and eyelashes fell out. It kept falling out after I was in remission for about 2 months.
When it started growing back, everything grew back so thick. I’ve never had to shave my armpits so much in my life.
»MORE: Dealing with hair loss during cancer treatment


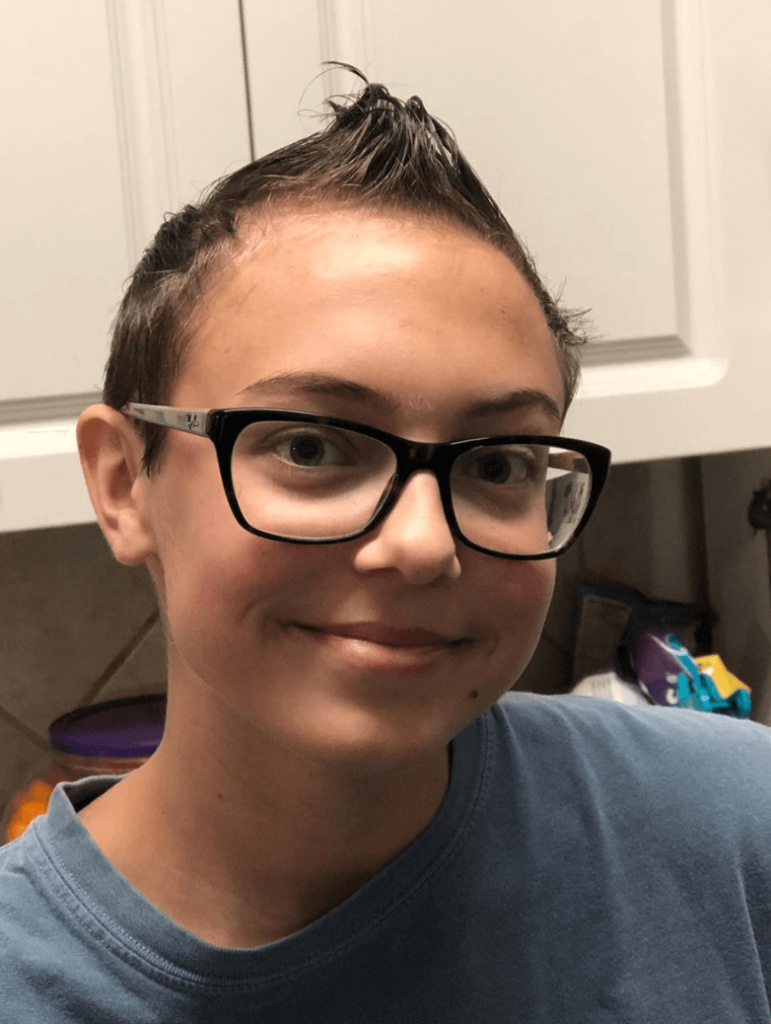
How did the hair loss affect you emotionally?
I lost all control of my life at that point. Your hair is one thing you can control.
You can get up and style it in the morning. It kinda sets the tone for the day. You can curl it, put it in a bun, or whatever you want. It kinda goes along with “look good; feel good.”
When I started losing my hair, I felt like there was nothing left that I could do to not look sick. Losing my hair made the reality set in.
Of course, the infusions sucked, but I tricked myself into just acting like they were a bad course of antibiotics. It was fine. I could get over it.
When all the hair started falling out, I told myself, “Okay, this is not strep, Madison. This is your life.” It was the last straw for me.
A lot of people say shaving it is empowering and helps take some of that control back, but I didn’t want to shave it.
Reflections
What was the lowest point for you?
When I was neutropenic and hospitalized. I thought I was going to die. I didn’t want to be at the hospital. Sick people are at the hospital, and I was neutropenic. That was the scariest point.
My fiancé’s dad came in and prayed over me. I was like, ‘Oh, wow. I’m about to die.’
The fact that I kept passing out and didn’t know what was going on didn’t help. I couldn’t stay awake long enough to ask questions or try to understand what was going on.
Trying to have support while being severely neutropenic is so hard because no one can be around you. I felt more isolated than I already did.
If my friends texted me or wanted to call and check on me, I usually didn’t have the energy to talk. I just handed the phone to my mom.
Part of the isolation I did to myself, but what else was I supposed to do? I could hardly even walk myself to the bathroom.

What helped you during those moments?
Knowing that I only had a total of 6 infusions. Seeing the light at the end of the tunnel and being able to stay positive was crucial.
It also helped to have people understand that I didn’t want pity. I used a lot of dark humor to get through it, and people who understood that and joined in helped keep my spirits up.
Joking around gave me a sense of normalcy. There were little positive moments sprinkled through everything. That helped.
One of my friends knew I couldn’t be around sick people or people who had been around sick people, but she wanted to help, so she dropped a care package off on my porch. It had coloring books, a blanket and some other fun stuff. She left it outside my door, and she didn’t even tell me it was there.
My little brother went outside later and said, “Uh, I think there’s something here for you.” He came over to me carrying this big basket of stuff. Little things like that were so nice.
What’s your advice for people who want to help but don’t know how?
Just be there. I was terrible about texting back because I felt so crappy all the time. If they don’t text you back, don’t take it personally. Text again the next day. Ask if they’re hungry. Tell them you’ll bring food.
My biggest pet peeve is that ominous phrase, ‘Let me know if I can do anything.’
That is the biggest cop out ever. Initiate something. Make a plan. Say, ‘Hey, I’m out and about. What can I bring you?’
I was so sick that I couldn’t walk my dogs. If someone had texted me and said, “Hey, do you mind if I come walk your dogs for a bit,” that would’ve been so helpful.
Be there. Have a real conversation with whoever is going through it and find out what their idea of “being there” looks like. Everyone is different. Some people need a lot of constant reassurance. Some people just want to be left alone and just know that if they need you, you’ll be there.
I wanted genuine people who were actually there if I needed them. The generic “let me know if I can do anything” people drove me crazy. That’s the emptiest statement ever.
It’s like when someone’s family member dies. If you say that to them, what does that person want to say back? “Let me know if you can do anything? Well, can you bring my loved one back to life?”
When someone leaves it that far open for you, it’s hard. “Anything” is very broad. You want to pay my medical bills? My rent? There are a lot of things I could say in response to that question, so it makes it really hard.
If you want to help, that’s why I say initiate something specific. Whether the person suffering chooses to accept or not doesn’t really matter. At least they know how much you’re willing to give of your time and energy. It helps to feel genuineness in an offer.
Monetary gifts are great, but time is worth so much more. If you want to come over and watch a show with me, awesome. Be there. Be genuine. That’s my advice.
»MORE: What kind of support cancer patients say helped the most

Can you talk about self-advocacy?
I had to advocate for myself to get diagnosed. My doctor was great and was willing to run any test I asked her to, but I don’t have a medical degree.
I didn’t know what to ask. All I knew to say was, “It’s not anxiety. I know what that feels like. I know it’s not anxiety. I’m not scared. I can’t breathe.”
I had to push that a lot. With me being so young and healthy, cancer was the last thing on anyone’s mind. You have to advocate for yourself if you feel something going on.
Doctors have gone to school and everything, but they’re also taught not to scare patients with cancer unless they absolutely have to.
My medical team was amazing. It just took a lot of pushing to get there and get diagnosed.
Do you have any advice for someone who is nervous to self-advocate?
Have a support system. Have people who are looking out for you. You wouldn’t have gone to the doctor unless something was wrong in the first place. At the end of the day, realize that your health and sanity are your responsibility. You owe it to yourself.
Don’t psych yourself out. Don’t let anyone convince you that something’s not wrong until there’s proof. You know your body.
Know yourself. Know your body. It’s your life on the line. It’s your well-being that you have to stand up for. Confronting someone about your own body is something that you just have to suck it up and do.
You need to have a support system standing behind you and reassuring you. They need to be able to say, “No, we’ve seen a difference in her from point A to point B. She’s right. Something is off.”
»MORE: How to be a self-advocate as a patient
How did the cancer affect your relationship?
I don’t know that it affected a whole lot. Getting diagnosed had the biggest negative effect on us.
He doesn’t ever get sick. I’m always sick. When I started having this shortness of breath, he said, “You’re just being a hypochondriac.” I disagreed, and we went round and round like that.
It caused a lot of tension. He told me I was wasting my time. I knew that something was wrong, though. When I did get diagnosed, we didn’t argue, but we did have “what if” conversations.
Thankfully, we’ve always had an open channel of communication. We were super prepared for worst-case scenario.
After I got diagnosed, he was unfailing. He was so supportive. I had surgery the day before his birthday. He found out I had cancer, and he left work. He drove through rush hour traffic to be there when I woke up.
If anything, I think it strengthened us. Any situation we go through now, we think, “We got through me almost dying. We can do this.”
One thing that crossed my mind a lot was guilt. I felt like I owed him so much because he stayed with me and took care of me through it.
The more I got my footing back, I realized I don’t owe him anything. He chose to stay. I would’ve done the same.
I don’t need to go out of my way to make sure everything is perfect. Our relationship is stronger, sure, but everything doesn’t have to be perfect.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

Financial toxicity: paying for cancer treatment
I was still on my parents’ insurance. It was at the end of the year, so we had already met our deductible. It’s still expensive, of course, but we only had to pay 10% of everything basically.
I was also proactive and bought a cancer policy at work the year before getting diagnosed. That offered a lot of assistance, too. They paid a percentage of everything.
While going through it, the financial stuff wasn’t really on our minds. My parents are stable and were able to help provide for us. Between my fiancé and I, we were able to pay our bills. The cancer policy helped a lot. I was definitely lucky.
Once the year started over and the deductible wasn’t met, that’s a different story. The PET scan I had was almost $6,000.
Message for patients
Find your community. There’s a group on Instagram of a bunch of young women called “Chemo Queens.” They’ve all been through some kind of cancer. Somehow, we all just connected.
We’ve grown tremendously over a few months. They are who I can talk to. I was having trouble breathing the other day, so I went to the doctor and had to have a scan. Not everyone truly understands what that’s like.
Don’t be afraid to talk about things. If you’re having a bad day and want to tell the world, post it. You can get little words of encouragement from people on your Facebook if you need it. It’s okay. Put it out there. People will receive it how they want to.
Don’t worry so much about running yourself ragged to maintain friendships. If there’s one thing I learned, it’s that you will have so many people be your friend while you’re going through treatment who will not be there after you get your NED report.
Don’t exhaust yourself. People who want to maintain friendships will understand it’s their turn to put in the work for that time period.
You do the work to keep yourself healthy and feeling good. Use your energy to make sure you’re eating and things like that. If there’s ever a time to put yourself first, it’s after a cancer diagnosis.
If you don’t feel inspired or led to be the “inspiring cancer warrior,” then don’t. Not everyone feels like it.
People always say, “Use your story for good!” Well, yes, but only if you feel like it.
There’s so much pressure on cancer patients to be strong through treatment and use their story for some greater purpose. I don’t think you need to feel pressured into that. Do what you feel is right.
Inspired by Madi's story?
Share your story, too!
Classical Hodgkin’s Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta






