Maria’s Stage 3C Adenocarcinoma Rectal Cancer Story
Maria shares her stage 3C rectal cancer story and undergoing treatment, including chemotherapy, radiation, and surgery. In her story, Maria highlights navigating quality-of-life issues, including losing her hair, the impact of her rectal cancer diagnosis on her marriage, and the support that was most helpful.

- Name: Maria A.
- Diagnosis: Rectal cancer
- Staging: 3C
- 1st Symptoms:
- Fatigue
- Weight loss
- Fast heart rate
- Bladder infection
- Treatment:
- Chemotherapy
- Every other week for 6 weeks
- Radiation therapy
- Weekdays for 7 weeks
- Targeted to the pelvic area
- Surgery
- Tumor removal
- Chemotherapy
Be positive. Don’t get caught up in the negative what ifs. That doesn’t help anything. It’s better to look at the bright side.
The thing that helped me the most was a positive attitude. If you go into it with a good mindset, shit tends to just work out.
Maria A.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
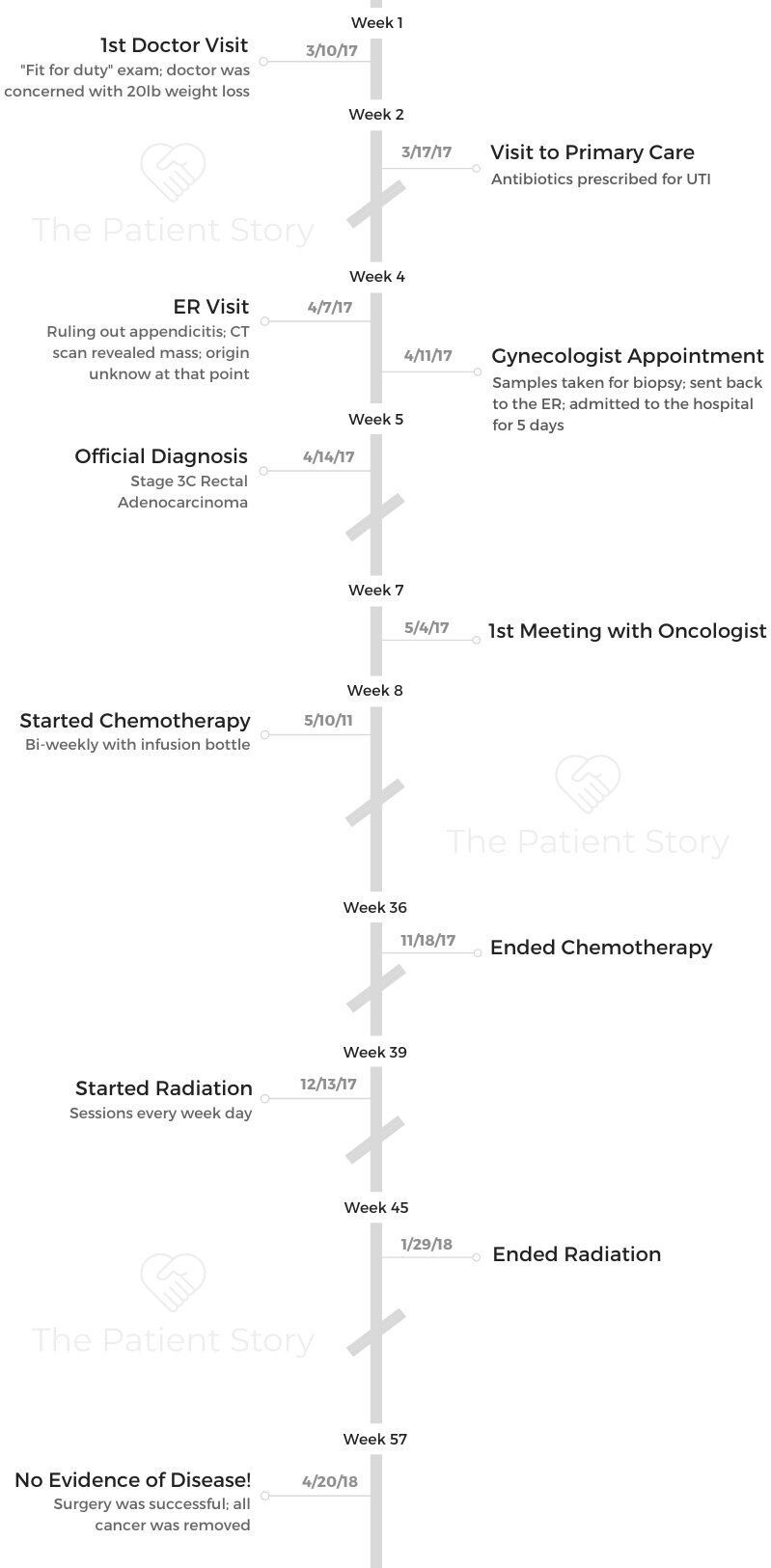
I was tired a lot. I lost a lot of weight. I’m a maritime marine. Before I can get on a ship, I have to pass a physical. I got the job, went to the doctor, and he noticed that I had lost like 20 pounds. My pulse was also really high. He didn’t want me to get on the ship.
He told me to go to the emergency room to see if they could handle it. I also have a thyroid problem, so he thought it might be that. They found a bladder infection that wouldn’t go away no matter how much medicine they gave me.
I worked as an equipment engineer for a medical technology company for a while, so I saw how broken the system is on that side of things. I stopped going to the doctor. I just didn’t trust it much anymore. Because of this, though, I had to get a general practitioner.
She sent me to the emergency room again about a week after. She thought it was appendicitis because I had pain. They did a sonogram and found a lump.
From there, it escalated. I saw an oncologist. She did an MRI. They found a 7 cm mass that was pushing on my bladder.
They thought it was uterine cancer at first, but the gynecologist said it wasn’t. The gynecologist was going to do a Pap smear, but she couldn’t because I started bleeding, so I went back to the emergency room for a third time.
They kept me there to monitor me because of the bleeding. They did scans and tests, and they found out that it was colorectal cancer pushing on my bladder. That was causing the infection.
How did you get the diagnosis?
I was just going to let it run its course. To me, cancer was a death sentence, so when I got it, I thought I should just prepare my family members for my passing.
My husband and sister talked me into getting treatment. I told them I would try anything once.
I’m pretty familiar with the medical industry, and I just thought it was a scam. They make money out of people’s suffering, especially if you have insurance. They fix the symptom instead of the problem a lot of times.
My initial thought was, “I don’t think we can dig ourselves out of this financially.” With my job, I only have insurance for 6 months after getting off a ship, so I was running out.
Luckily, the union I’m a part of covers cancer as an emergency, so we didn’t walk away destroyed.
I was also trying to figure out where I got it from. It doesn’t run in my family, so I was trying to see how I got it and how I could have avoided it, but I don’t think it could’ve been avoided, honestly.
How was the first appointment with the oncologist?
She told me the treatment plan. I did 7 months of chemo, 7 weeks of radiation, and then surgery. They took everything that the tumor touched. I had a hysterectomy, colectomy, and they had to rebuild the vaginal wall.
Treatment
Did you experience side effects during chemo?
I had no strength. I was so weak. All I did was lay down. I had no appetite. I was prescribed morphine for the pain and marijuana to help. I had body aches pretty bad.
I couldn’t eat a lot of the stuff I used to eat. I had taste changes, and that would make me want to throw up. I had nausea a lot. I had some tingling in my extremities as well. My nails got brittle and wouldn’t grow back.
What got you through chemo?
When you’re questioning whether or not you’re going to die, how are you supposed to deal with that? You really can’t.
I just tried to be optimistic. I knew the best- and worst-case scenarios. I tried to just stay positive and spend time with my family. I just tried to trust the chemo and hope that it would work.
I thought about the fact that I was going through this for a reason. That reason could be that I could help someone in the future. I tried to focus on that rather than whether or not I would live or how much it was hurting.
Attitude was a big part of it for me. Everything starts in your mind and then manifests elsewhere. Staying positive is really important. I would always be smiling at my infusions, because what good does being depressed about it do? I just tried to accept the role that life threw at me.

What was radiation like?
It was every day Monday through Friday for 7 weeks. During that time, they tested my white blood cells to make sure they were high enough. They would skip if my count was too low.
Each session took about an hour. My skin was really pretty raw for a while. They targeted the pelvic area, and it hurt quite a bit.
It was hard to walk and put clothes on, so I laid around a lot. They told me to use Aquaphor, and that helped a lot. It made the cracked skin not so dry. It helped.
After radiation, you had surgery. What was the preparation for that like?
They had me do a cleanse to clean out my intestines. That was about it. It was just the night before the surgery. I had to drink this nasty stuff they gave me. I puked it out instead of it doing its job, so we told the doctor. She just worked around it, I guess.
After we checked into the hospital, I changed. I had 3 surgeons, so I met with them. The gynecologist did the hysterectomy, there was another one who did the colectomy, and the third did all the rebuilding of the vaginal wall and everything else. Then they gave me some medicine, and I guess I was loopy because I don’t really remember anything else.
Do you have any lasting effects from treatment?
Right now, I’m going through what they call surgical menopause. I have hot flashes and all that good stuff. I’m finding out that I’m still recovering. I can’t trust my own thermostat, so I have to ask my husband if it’s just me or if it really is hot. I’m still figuring out how to get used to my new body.
I’m not cancer-free until 5 years, so I still get blood tests every 6 months. My white blood cell count is still not as high as it was before I started treatment, but it’s getting there. I still experience neuropathy sometimes.
I wear an ostomy bag now, so before I get on a ship, I have to make sure I have supplies. The last ship I was on, it was 120 degrees in the engine room. The adhesive comes off at temperatures that high, so that irritates my skin.

Reflections
How did your experience affect your relationship with your husband?
It brought us closer. We’ve been married 20 years. This experience just cemented the whole thing. It felt like we were building our relationship up for years leading up to this, and to have him be there for me and care for me has been really nice.
I don’t ask for help. I’m stupid that way. My husband would see me stumbling and just help me. I wouldn’t have to ask. He never left my side.
If I had to use the bathroom, he would walk me. He was just always there. I didn’t have to ask for help because he just offered.
We would walk to Walgreens sometimes during treatment. I would be too tired to walk back, so we would just Uber, or he would walk the rest of the way home and get the car.
Can you talk about hair loss?
I’d be in the shower, and a clump would come out. Or I would run my hand through my hair or scratch my scalp, and it would come out. My husband saw a look on my face one day, and he said, “Let’s just shave it off.”
We didn’t need a reminder every time my hair came out. The less reminders and triggers there were, the better I did coping with it.
We just tried to eliminate the traumatic stuff. Shaving my head was a great way to do that. It was better to tackle it head-on than let it happen to me.
How important was it for you to have a support system?
It was one of the key things that kept me positive. If they weren’t there, I would’ve probably been too depressed to do anything. They reacted to my optimism, which made me even more optimistic. If they hadn’t been there, I wouldn’t have been able to keep myself positive.
My older brother and I didn’t really get along very well, but when I got cancer, he really stepped up. It brought us closer. When it came down to it, my family had my back. That was really nice to have.
It’s one of those things that you don’t really think about until you go through it. I always had someone with me in the hospital. Because of that, I didn’t have to be alone with my thoughts and really focus on the fact that I was in the hospital.
The nurses were surprised that I was walking around 3 days after surgery. Because I always had support and positivity surrounding me at the hospital, I felt better. They made me want to get better.
»MORE: What kind of support cancer patients say helped the most
How were you feeling when you found out you had no evidence of disease?
The PET scan came back clear. When I got the results, I was anxious. Of course, I was happy, but I just didn’t want to go through it again.
There’s always a fear of it coming back, but you can’t focus on that. You have to keep your quality of life in mind. It’s no way to live when you’re tormented by the anxiety of recurrence.
Getting the screenings done every 6 months brings back the anxiety. It’s really only during the scans and tests. I remember the anxiety, and I just talk it out with my husband. We reassure each other that it’s not coming back.
What advice would you give to someone who has just been diagnosed?
Be positive. Don’t get caught up in the negative what ifs. That doesn’t help anything. It’s better to look at the bright side.
The thing that helped me the most was a positive attitude. If you go into it with a good mindset, shit tends to just work out.

Inspired by Maria's story?
Share your story, too!
Rectal Cancer Stories
Kalei M., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Presence of mucus and tissue-like substance and blood in stool, stomach cramping
Treatment: Radiation therapy, chemotherapy, surgeries (two lung resections)
Jessica A., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Changes in bowel movements, blood in stool, abdominal pain, back pain, difficulty sitting comfortably, constipation, feeling of incomplete evacuation (as if some stool remained after bowel movements), mucus-like stool consistency, bloating
Treatment: Immunotherapy under a clinical trial
Shiva S., Rectal Cancer, T2, and Renal Cancer, T3
Symptoms: Pressure and urgency of bowels, back pain
Treatments: Chemoradiation (for rectal cancer), surgery (ileostomy, combined bowel and kidney surgery), immunotherapy (for kidney cancer)
Jeanine B., Rectal Cancer, Stage 3 (T3bN0M0)
Symptoms: Long history of bleeding that was blamed on hemorrhoids, pain in the tailbone, urgent need to use the restroom, unusually narrow stools, presence of mucus in stools, fatigue
Treatments: Chemotherapy, radiation therapy
Devon B., Rectal Cancer, Stage 4
Symptoms: Pain when trying to move bowels, increased frequency of bowel movements alternating with periods of constipation, passing mucus instead of feces, narrow stools
Treatments: Surgery (ostomy surgery), radiation therapy, chemotherapy
James K., Rectal Cancer, Stage 3C/4
Symptoms: Occasional rectal bleeding, increasing fatigue
Treatments: Chemoradiation, surgeries (coloanal pull-through, temporary ileostomy, ileostomy reversal, permanent colostomy), adjuvant chemotherapy






One reply on “Maria’s Stage 3C Adenocarcinoma Rectal Cancer Story”
The stories of these brave survivors from rectal cancer are really heartening.They have shown that with knowledge, careful study and patience, cancer can be controlled and perhaps won.I was left wondering why only women have come forward to tell their stories. Where are the male survivors? I am a male,90 years, diagnosed with rectal cancer one month back. Tentatively stage 3c.Thanks.