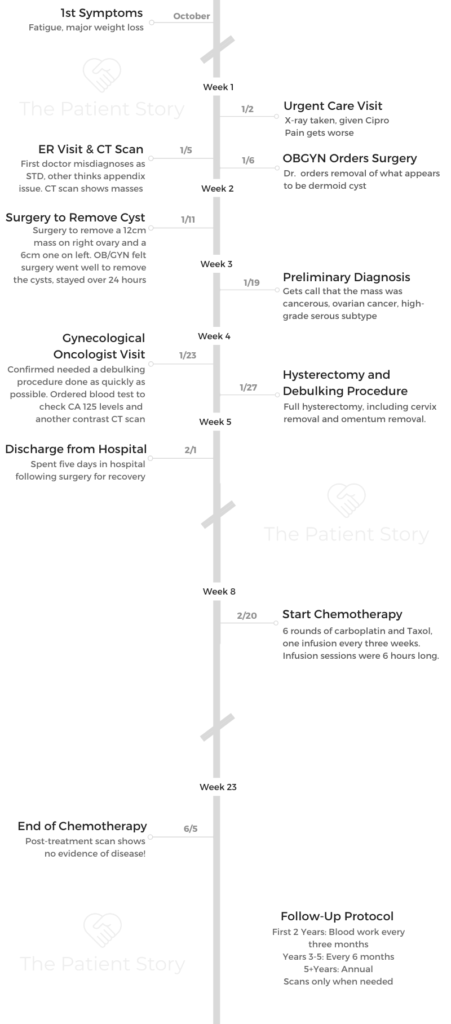
Randalynn’s Stage 1C High-Grade Serous Carcinoma Ovarian Cancer Story
In her story, she shares how it was undergoing treatment, both surgery and chemotherapy, tips on dealing with the hair loss, and how she advocated for herself as a patient. Thank you for sharing your story, Randalynn!
Randalynn has turned her cancer experience into a life of advocacy after getting diagnosed with stage 1C high-grade serous ovarian cancer.

- Name: Randalynn V.
- Diagnosis:
- Ovarian cancer
- High-grade serous
- Age at DX: 55
- Staging: 1C
- 1st Symptoms:
- Fatigue
- Weight loss
- Feeling of UTI
- Treatment:
- Surgery to remove mass (before it was determined to be cancerous)
- Hysterectomy, including cervix
- Chemotherapy
- Paclitaxel (Taxol) & carboplatin
- 6 rounds
- One infusion every three weeks
- Paclitaxel (Taxol) & carboplatin
It is going to feel like you are going through the worst possible thing ever, but if you can put one foot in front of the other, you will get to that finish line, whatever it is. Then you take the next steps.
You take each step at a time, and once you get a plan in place, things start to seem a whole lot easier because you figure out what to do. You focus on that.
Randalynn V.

- First Symptoms and Tests
- What were the first symptoms?
- Describe the visits to urgent care and the ER
- Dealing with doctors who won’t listen to the patient
- Describe the moment you learned about the masses
- What were the next steps when you got admitted to the hospital?
- The staff missed performing a key test
- How did they describe the mass?
- How did the initial surgery go?
- How was recovery from the surgery?
- Cancer Diagnosis
- How long did it take to hear the official cancer diagnosis?
- How were you able to process the diagnosis?
- How did you break the news to your kids?
- Deciding to inform the kids' schools about the cancer
- Any guidance for other parents on dealing with cancer around young children?
- How did you share the news of your cancer diagnosis with people outside of your mom?
- Treatment Decisions
- How did you decide where to go for cancer treatment?
- How quickly were you able to get an appointment?
- Describe the first appointment with the gynecological oncologist
- Advocating for yourself as a patient
- The importance of your doctor's bedside manners
- How was it having your parents come into the appointment?
- How did you decide what kind of surgery to pursue (laparoscopic or robotic)?
- Surgery and Recovery
- Chemotherapy (Carboplatin and Taxol)
- Hair Loss
- End of Treatment
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

First Symptoms and Tests
What were the first symptoms?
I was 36 years old. had an extremely stressful job. I am a part-time single mom of two children. Couple that with working 50-plus hours a week [and] having some events at the office go on. I was exhausted and fatigued. When I’m stressed out, I don’t eat. All of those things were norms for me.
That totally took over October. When I look back in photos, the weight loss was significant, like, “There’s something wrong with her.” You can start seeing that in July.
I have my children on Christmas Day, then they’ll go to one parent’s house from mid-day Christmas until New Year’s Day. It was my year to do the transition mid-day, and I decided to go on a trip.
I told one girlfriend that I was so tired that my workout routine must be stale. That’s what it is; it can’t be anything else going on. I just need to decompress. So I started doing a completely different workout.
In doing so, the doctors think what ended up happening was the tendons had wrapped themselves around the tumor, which was the size of a cantaloupe, and I only weighed 115 pounds. You couldn’t see it, which was the really weird thing.
The tendons started rubbing differently. I thought I was developing a UTI and called my nurse practitioner to ask for a prescription.
At that time, it was still fine. I don’t get them frequently, but I thought it was normal. I’d had them before, so maybe this was just caused from all the stress and everything else.
Describe the visits to urgent care and the ER
January 2nd was when I went to urgent care. They did an X-ray. Cysts like this don’t show up on X-rays, and they just wanted to make sure nothing else was going on.
I don’t know what they thought may have shown up on the X-ray, but they switched me to Cipro, which is supposed to knock everything out within 24 hours.
Then 24 hours later, it still hadn’t worked. It was probably me taking 10 or 20 steps and having to bend over because the pain was so significant. It felt like I was in labor. I was like, “This is just not normal.”
I went to the ER, and that was when — after me persuading that what they thought it was wasn’t what it was — we did a pelvic CT scan with contrast dye, and both masses showed up.
I had one on my left ovary and one on my right, but my right was the main culprit in what would come back as having ovarian cancer.
Dealing with doctors who won’t listen to the patient
I remember it was a male doctor who thought it was an STD when I first got to the ER. I remember pleading with him to believe me, and he didn’t.
A woman transported me from the ER to where the scan was taking place. I was in tears because of what he had said. She said, “He’s at the nurse’s station right now asking them if he overstepped and why you were in tears. They’re trying to explain to him, ‘You didn’t believe her. We don’t think she’s making this up, but you didn’t believe her.’”
The transporter herself said, “More times than that, I hear the ER doctors giving a diagnosis before they’ve run all the tests.”
They need to learn that whatever they’re assuming it is, they should not lay those things out until they know for a fact that that is what it is.
The female physician who was on call that night was the one who actually said, “I don’t think that’s what it is either. Her appendix is ready to rupture. Let’s go ahead and do a pelvic CT scan.”
It’s interesting how things play out and how physicians and the people around them interact, like, “You probably should have handled that a little differently.”
»MORE: How to be a self-advocate as a patient
Describe the moment you learned about the masses
[The doctor’s] face when she came in to tell me about the masses — it still didn’t click in my head. I was like, “Okay, well, people get ovarian cysts. I guess this explains it.”
I was supposed to go snow skiing with my kids in 10 days from then, and I was like, ‘Well, can we wait till after that?’
My mom was like, ‘You’re on morphine! It’s not working. No, we can’t wait.’

What were the next steps when you got admitted to the hospital?
The physician on call that night in the ER, it was about 1:30 a.m. when she came and told me, “We did the ultrasound as well. You have a mass on your right ovary.” She didn’t tell me I had two, nor how large they were. She asked, “Do you need to have an OB-GYN?”
I said, “Yes, I delivered in this hospital. She is on staff here, or at least has rights to be in the hospital in the OR (operating room) here.” They said, “Okay, we’ll give her a call, and we’ll see what she wants to do.”
They admitted me because the pain was [bad]. Morphine wasn’t managing it, and they ended up going to a Dilaudid drip. On top of that, they wanted to start a round of antibiotics.
My OB-GYN came in the next morning, and she said, “You look good. You look tired. How’s the pain?”
I said I was still in a ton of pain, and she said she thought there was a little bit of an infection and they’d keep me on the antibiotics. She said she was trying to get an OR, but she didn’t know how long it would be.
The staff missed performing a key test
I ended up staying over the weekend there. In the time I was there, I had my blood drawn at least twice a day.
Not one time did they ever draw a CA 125 test.
It’s not 100% foolproof, but for the type I had, it would have shown up as an elevated CA 125 level, which could have triggered in their minds, “Okay, we probably shouldn’t remove this. We should have her be with a gynecological oncologist to do the removal.”
How did they describe the mass?
What was explained to me was that I had a 12-centimeter, so the size of a cantaloupe, dermoid cyst. I’m not grossed out by them because I had cancer, but in the beginning I was like, “I’m not going to tell anybody that this is what I had.”
If you’re familiar with that, those are the kind that grows teeth and hair in this really kind of interesting way. It’s super lumpy.
That wouldn’t have triggered anything either. I ended up going home 24 hours before I had surgery, and my OB said, “So long as you stay in bed, let’s get you home so you can at least get some rest.”
I did and came back the next day, so it was about a four-day window between when I was admitted to the ER and when we actually had surgery.

How did the initial surgery go?
My OB-GYN wanted to try to do the surgery without having to do more than a C-section type of scar. They were able to get it out that way. In doing so, the surgery took quite a bit longer.
My tumor had been compromised. [If] it was compromised during surgery or whether it was compromised prior, we don’t know. She considered surgery to be a success.
I stayed over one night because they couldn’t get my blood pressure up and I was in a tremendous amount of pain, which was probably due to the fact that they had just removed a whole bunch of cancer, and there was other stuff going on.
She told me they’d have results in 24 hours and she didn’t expect for there to be any issues whatsoever.
How was recovery from the surgery?
I didn’t have any prep beforehand. It was supposed to take maybe 45 minutes but ended up closer to two hours because of the size and the way they were trying to get it out. They also had to remove the cyst on my left ovary.
They took my ovary, and it was attached to my fallopian tube on my right side. That was what was biopsied. Women who have C-sections, I have a lot more respect for you because it was pretty challenging afterwards.
I had never had an abdominal surgery before, so I hadn’t thought about the fact that even though it was lower, below the bikini line, having to try to move and get out of bed was challenging.
I was still tired because I had cancer, and I still really wasn’t able to eat because I had ovarian cancer, which is one of those symptoms, not feeling like you want to eat or feeling full quickly when you’ve taken a few bites.
»MORE: Read more patient experiences with surgery
Cancer Diagnosis
How long did it take to hear the official cancer diagnosis?
I left the hospital on a Friday, a holiday weekend. I hadn’t gotten the results by the end of Friday [and] knew I wouldn’t Monday because it was a holiday.
I had my OB-GYN’s cell phone number, so I texted her Tuesday and said, “Just checking in. Do you have those results? I just wanted to make sure everything was okay.”
She said she didn’t and that she would call the lab because it was weird she didn’t have them yet. Wednesday went by, and nothing. I thought I would give her till Thursday because I didn’t want to seem like that crazy patient who’s totally nagging. She had other things going on. She told me she didn’t think it was any big deal.
Thursday I had set in my mind that I was going to give her until 1:30 p.m. That allowed her through lunch, and then I would text message her again.
She beat me to the punch. Right around lunchtime on that Thursday, she called me. My mom was out. The call came in, and I was like, “Hey, how’s it going,” being my normal upbeat self. She said she was good and asked how I was feeling.
I said I was super tired and that it kind of hurt a lot. I should have recognized the tone in her voice, but I didn’t. She said she knew why my labs took longer to get back, and she wasn’t expecting this.
She said she had spent all morning thinking if she should call me to tell me to go into the office, but that I would know I was sick and would have to drive over, or to tell me over the phone.
She said she decided to tell me over the phone because she didn’t want me to have to get in the car, then have to drive out there, and drive back.
She said I had ovarian cancer, it’s high-grade, [and] that she’d have to get me to a gynecological oncologist very quickly.
How were you able to process the diagnosis?
I told her to give me a second, and I put the phone down. I had prepared myself. We were a week out.
I had actually talked to a friend who had had several cancer diagnoses. She said the further that you get out, the more chances it’s probably not good, especially when the lab is telling her they’re running more results.
In my head, I knew a dermoid cyst had a 1% chance of being ovarian cancer. Being my age, 36 at the time, I had 6.7% chance of being diagnosed with ovarian cancer. Put those things together and my odds were going to be very low of cancer happening, but I had still told myself at that point that it was very likely going to come back that way.
I remember I said I just needed a second, and I folded over in my bed, had a moment, sat up, took a deep breath, [and] said I was really sorry. She said no, she was really sorry.
I had two hours until my kids came home from school. In that two-hour time period, I had to find myself an oncologist [and] get an appointment. My mother was at my house at the time because I couldn’t take care of two kids by myself post-surgery.
She didn’t take the news so well when I told her, so I needed to get someone over to the house, one of her friends, to help her through this and to get her back up to normal speed before the kids came home as well.
I didn’t really have time to process it. The only time I had to really process it was at night. I didn’t sleep very much.
Honestly, once you find out you have cancer and you get into the flow of things, they have you going non-stop, one thing after another, and there’s really not time to think about it. I don’t think the whole processing you have cancer part happens — at least it didn’t for me — until treatment stopped.
That was when I had the time to process what the last six months looked like. I made it, but I didn’t even think about it one time more than what I was actually having to go through at the time.
»MORE: Processing a cancer diagnosis

How did you break the news to your kids?
My son was three, and my daughter was seven. My daughter knows what cancer is. She knew my mom’s dad was, at the time, dying from it. My son was three.
‘Mommy’s sick.’ That’s all he could really grasp. He didn’t understand what it would really mean or anything.
I did not tell them. I went through my debulking procedure and found out what stage it was. I told my kids the weekend before I started chemo just because I was going to lose my hair. That was one of the things I wanted to find out as well.
I decided it was in my best interest to tell them, to be open and honest about it.
I have an ex-husband and wanted to do it together, so he came over. We told them together because I wanted to use the words I was using so that he knew what exactly was said and that if there were any concerns, we were able to both know what those would have been and talk through them.
»MORE: Parents describe how they handled cancer with their kids
Deciding to inform the kids’ schools about the cancer
One kid was in first grade; one was still in a pre-K program. The kids’ schools both did really well with it. They had gone through adjusting through the change when we went through the divorce, and now I was saying, “Have another change we’re adding to the mix: I have ovarian cancer.” We worked as a team and combatted the whole thing.
Any guidance for other parents on dealing with cancer around young children?
For the kids’ side of things, the director of the school where my son was had just had a neighbor go through breast cancer. Her children are around the same age. They used a book.
I did not use the book with them. What I did was read the book to see what it said. There are a lot of books out there you can get that walk through “Mommy’s sick or Daddy’s sick” and break it down in those terms.

That initial part went okay. What I couldn’t prepare for was them actually see me go through everything. They got pretty tired of Mommy always being sick and not being able to be there.
My support system was great, so I got to everything, even if I thought I was going to be sick while I was there. I made sure that every child thing there was, I showed up for it. I think that’s really key, too, just so you can try to make things as normal as possible.
Everyone wanted to help. I said, “Let me get through a couple rounds and see what I’m dealing with. I don’t know what I’m going to feel like, and I don’t know where I need help.”
What I ended up coming up with was allowing for there to be meals, specifically for my mother and the children. I didn’t know if I was going to eat for the day and told them that. I didn’t want my mom to have to worry about feeding them and herself.
I told my supporters if they made sure my mom and kids had food, they wouldn’t have to worry about me. My mom would make sure I had food. That was super helpful.
How did you share the news of your cancer diagnosis with people outside of your mom?
I only told my inner circle and my family. I think my parents probably handled the whole telling my brother and all the grandparents. We were trying to hold off on telling my grandfather who wasn’t doing well; however, he was having chemo and labs at the same cancer center the day I had to go in to do my lab work and pre-op stuff, as well as CT scan.
My mom had gone to everything before that with him. What was she going to say? “Sorry, I can’t do this,” but then we run into each other in the lobby or something like that. That was the next day. So he was one of the first people I saw.
The rest I didn’t tell until I lost my hair. I needed to go through debulking surgery. I was in the hospital for five days following because it was major abdominal surgery. I needed to find out what stage I was and what my exact diagnosis was.
Then I had to start chemo, and I didn’t want all of the outpouring of support. I didn’t want everyone contacting me at once and having to deal with all of that.
The way I broke it was through a blog, because then I could tell people what I wanted to tell them, when I wanted to tell them. They were kept up-to-date without having to necessarily [come to me].
That was the easiest way I came up with, and it worked great. It caught a ton of people by surprise, but I don’t know that it was for everybody to know in the beginning.
It’s your turn to be selfish. I wasn’t a selfish person, and this was my time to focus on what I needed to do for myself and for my kids to get all of us through this. It doesn’t have to be a negative thing.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to go for cancer treatment?
I told my OB-GYN I wanted to be seen at Siteman Cancer Center, which is our main cancer center here in St. Louis. She said she knew someone at another hospital, but I told her I didn’t want to go that route.
I called my friend because she was on the patient advisory board at Siteman Cancer Center. I lucked out. At the time, one of the physicians who was on the board was actually a gynecological oncologist, and she’s now my lead oncologist.

How quickly were you able to get an appointment?
She got me in two business days later, so I asked what to do because normal protocol is not for you to call a cancer center, report you have ovarian cancer, [and] ask to get in.
It’s normally a doctor’s referral and you have to go up this chain. It takes two weeks, and that’s what happened.
I called. They said they had an appointment in two weeks and would call me back. Sometimes the oncologist takes people Monday afternoons.
I remember thinking, “I was just told I had high-grade ovarian cancer. I Googled it; it meant it grew quickly. Two more weeks in my body — what is this going to do?”
I lucked out. She opened up her schedule, probably due to my age because you don’t have a lot of 36-year-olds walking through your door.
She saw me that Monday morning. I went from knowing I had cancer to only having to really wait a weekend, which most people don’t.
Describe the first appointment with the gynecological oncologist
I walked in her office on that Monday afternoon, and we discussed what was going on. The only issue is that more times than not, you cannot diagnose ovarian cancer without actually doing a procedure. It’s normally a debulking procedure, or you’re going to do the biopsy.
They can normally do it on the table and be able to tell. Then they have to go through the rest of the debulking procedure if it comes back you have ovarian cancer.
But in my case, I knew I had ovarian cancer, and I knew the grade level that I have. What I didn’t know, which is the most important part, is what stage I was.
That was what we had to figure out at this point. We had to come up with a game plan to do that.
Advocating for yourself as a patient
My perspective on it changed. Now I’m very much, ‘Hey, what’s going on?’
My lead oncologist knows how I am, so as soon as anything [happens], even when I go through my check-ups now. She gets the alert. She pushes it straight to MyChart.
During all that was going on, I did not want to know all of that, so I didn’t sign up to have all of my records and everything being sent straight to me.
I didn’t sign up for that until 18 months ago, which is kind of backwards. She either releases it right away or text messages me and says, “Here’s what’s going on. Things look really good.”
That’s an important thing, too. If you have a medical team, your lead person should be able to figure out what is the best way for you to receive news and how you prefer to have it delivered.
A lot of people don’t like to do it until they’re in person. Me, I’m like, “Let’s rip the Band-Aid off. I want you to tell me now, and then we can discuss it when I come in. We still have my appointment, but let’s talk through this now since you have the information.”
»MORE: How to be a self-advocate as a patient
The importance of your doctor’s bedside manners
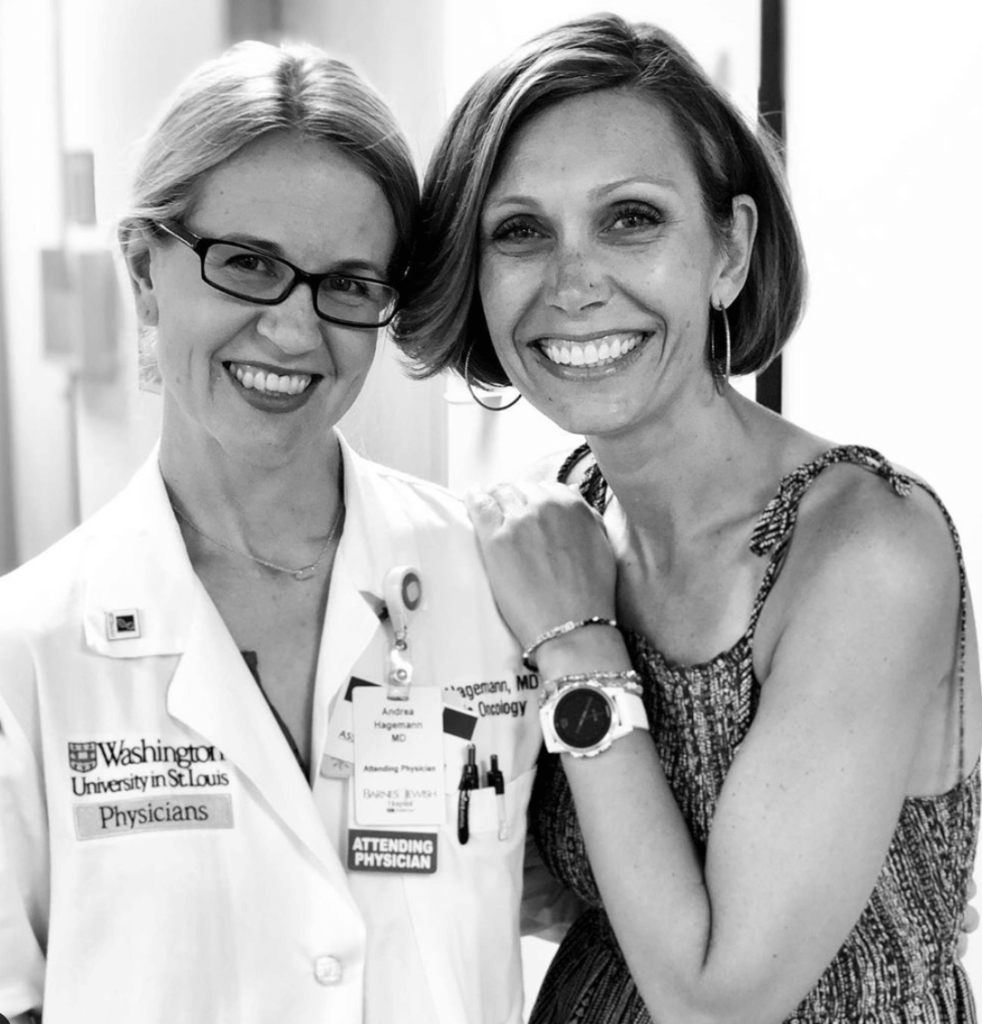
She does not introduce herself by doctor. She walked in the door and said, “Hi, my name is Andrea. I am so sorry that we’re having to meet under these circumstances,” and gave me a hug.
That speaks volumes for who she is as a person. This is how she treats everybody. She’s never introduced herself as Dr. Hagemann to any of my friends or family. It’s always Andrea, and if you ask any of her other patients, it’s the same.
I think in doing that, she tries to put herself at our same level. She’s not trying to elevate where she is. She wants to be at your level.
She spent two hours with me that day. I went back by myself — it was something I wanted to do by myself — and walked through what this looked like, what next steps would be, what that next surgery was going to look like, and what our hopes were.
Our hopes were that, from what the pathology (biopsy) report had shown, it looked to be like it would be the one ovary. The fallopian tube was clear, as was the other ovary.
From what they could tell from the cyst they removed, there was no cancer on that other side. She walked through all that. She listened. I cried.
How was it having your parents come into the appointment?
She asked if I had parents there, and I said yes, they were in the waiting room. She asked how I wanted to do this next part, and I said I needed her to talk to them. I would sit there, and if she could explain to them what she had just explained to me, that would be great.
She took her time and explained everything. She let them ask questions because they had a lot. It’s a lot for whoever will be your caregiver to take in.
Although I was 36 years old, I was single. The dad role takes over, and he was like, “I have to take care of my daughter [and] be fully involved in what’s going on.”
I could tell he had done his research and was asking the questions, like why not a robotic surgery? There are reasons why you do or don’t do a regular procedure, so we learned about all of that. The game plan was I would go in four days later to get surgery.
It was very quickly moving, and was really great. My relationship with Dr. Hagemann started off really great, and we still have a great relationship now.
How did you decide what kind of surgery to pursue (laparoscopic or robotic)?
[Editor’s Note: Always check with your doctor on medical information]
My goal was no matter what, I needed to stay alive for my children. My tumor had ruptured, which meant potentially there were microscopic “pieces” floating around my abdominal fluid. That means it could have attached to different organs, and that comes into play.
I had a full hysterectomy, including cervix. In a debulking procedure for ovarian cancer, I have a 13-inch incision. They checked my stomach wall to make sure nothing was there. They checked on all the other organs.
They take out your colon and intestines and go through it piece by piece. The stuff they’re looking for is granular, and the only way to find it is by touch.
In using the robotic procedure, you’re not able to do as thorough of a check. My omentum’s gone as well, and they consider that an organ. It’s a filter that catches everything. That’s usually the next place the cancer goes once the tumor ruptures. I was lucky and did not have it there either.
What we would find out, having my uterus removed, was I did have a focused group of endometrial cancer as well. That would have been done whether the hysterectomy was done laparoscopically or robotically.
My oncologist knew that my goal was whatever I had to do to be here the longest, that was what we needed to do. If that meant the measures were a little more extreme than me backing off and taking a lighter approach, then that’s what I was going to do.
Not knowing what stage it was and knowing the tumor had ruptured, we didn’t really have another option than a full, open procedure.
Surgery and Recovery
Was there prep leading to the surgery?
I had scans to make sure nothing else lit up that would be obvious, so they could try to eliminate that. We did that, my blood work, did the fasting after a certain time. They had me drink a bottle of Gatorade to try and hydrate a couple of hours before. I did that with two or three of the procedures I’ve had.
Then I went in for surgery. But [there is] one thing I would recommend. I have extremely low blood pressure. I was going through the pre-op. For the procedure I have, they usually do an epidural, so they have a block, and you can’t feel the significant amount of pain I was in.
The nurse’s assistant asked if there was anything the team should know about. I said, “Yes, please don’t worry. When I come out of surgery, I’m going to be 80 over 50.” She double-checked that I was talking about my blood pressure.
That was an important thing to tell them because an epidural lowers your blood pressure significantly more. In telling them that, I was not able to have the epidural, and they went a different route that they normally do not.
They put catheter pain bulbs in my abdomen in bags. They refilled them while I was at the hospital. You need to continually talk about things like that. A lot of times, people do not. That was key.
We went through everything. I was the first patient up. A pre-op room first thing in the morning is really hustle-bustle right before everything starts!
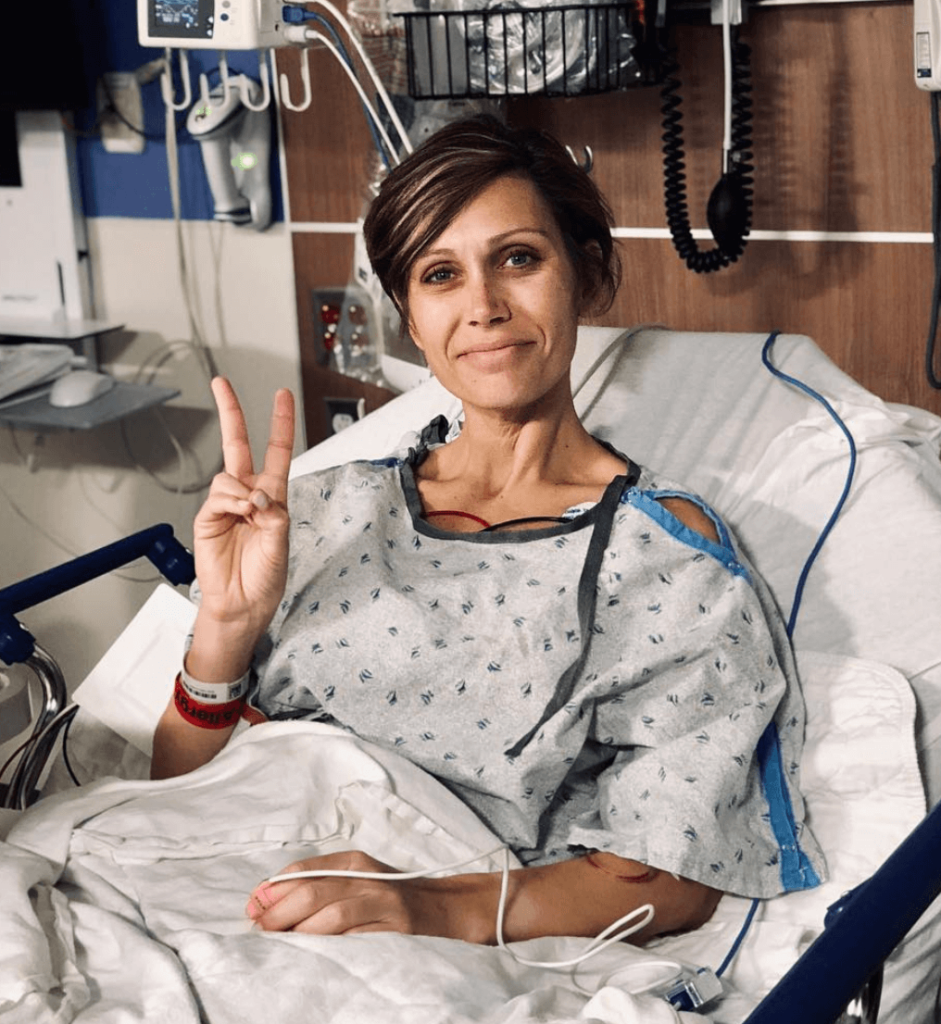
How were you feeling heading into surgery?
They give you the laughing gas to knock you out, and off we go. I didn’t have any nerves at all. To be honest, I wanted it out. You know you have cancer at that point. I just wanted it out. I didn’t care how you got it out; I wanted it out.
I wanted to know what stage I was because that is extremely important in ovarian cancer. The later the stage, the lower the chances are of being able to go into full no evidence of disease (NED) and the lower the chance I had of fighting this and being here the longest.
I was just like, ‘Let’s do this. I want to get this done.’
How long was the surgery?
It was five to six hours long. It was a pretty big deal. I think I woke up and recovered, saw my parents. I didn’t really remember anything until I got up to the floor that I was on, which was the gynecological oncology floor. I was the youngest person on the floor. It was pretty empty while I was there.
I remember coming around the corner, the nurses stations. I was elevated on the gurney, and the nurses said, “Is that her? There’s no way. She doesn’t look sick, and she’s so young.” I think that’s a lot of people’s reactions, and they probably didn’t think I would hear them or remember, and I did.
I shared a room with an older woman who was going through ovarian cancer. She said to my parents several times that she was sorry, that it wasn’t fair to me, that I shouldn’t be going through this.
The women there are either recovering for surgery or going through chemo. [They] aren’t used to seeing [young patients], and they don’t like it because they know the road you’re going to have ahead of you.
Describe the recovery at the hospital
I didn’t want to walk. That was the hardest part, walking and sitting in a chair with abdominal surgery. It was the worst. They usually want you to have a bowel movement (at the hospital). I had to get my blood pressure up to at least 90, and that took me a little while.
I was able to urinate. They pulled the catheter out within 24 hours of surgery. The only reason they could do it was because I didn’t have the epidural. I had the pain bulbs. Otherwise, I think they leave that block in for a couple or few days, which slows things down a bit.
I was up walking around maybe within 36 hours. You start slowly and eventually get faster. I don’t remember having a bowel movement, and that’s usually the number-one thing they make you do before they discharge you.
I think it’s because everything [inside you] was gone through, taken out, and put back in. It takes longer to heal.
Your body gets moving, and it’s better.
Describe the recovery at home
The recovery from the full debulking procedure was significantly easier pain-wise than the first surgery. It could have just been the post-care I had, the stuff they sent me home with.
I did go on blood thinners for at least two weeks, maybe three. It was very hard to get up and down.
Your best option is a recliner. That’s what I had because I was able to push myself up to the stage where I could put my arms out, not try to help, and have someone pull me up.
How did you learn the stage of your ovarian cancer?
Two weeks later, I would find out my staging. I went back again by myself. The resident came in first. I totally broke down and was like, “How bad is it?” She said she couldn’t give me that, that I’d be fine, and that I’d have to do chemo.
Andrea came in and said that we got the news we wanted, that the stage was 1C. However, I had thrown them for a loop because I had a focused group of endometrial cancer, which they didn’t see coming. Instead of having four rounds of chemo, I would definitely need the six rounds to combat that.
She also said I needed to do genetic testing because she needed to make sure I didn’t have Lynch syndrome. It’s pretty common for someone with Lynch syndrome to have both cancers at the same time. I did not have it.
Chemotherapy (Carboplatin and Taxol)
What was the treatment plan?
Hit the ground running again. We went through the drugs I would be in, which were carboplatin and Taxol. I would receive one treatment every three weeks of both. We knocked it out in six to seven hours, depending on how I could drip.
I met my nurses, and Andrea explained to my parents again because I couldn’t do it. They came back, and she explained everything again. We had my port placement done. The following week, I would start.
How was the port surgery (minor)?
It hurts and nobody prepares you for it, but I was super thin, so that might have been part of the problem. I think by surgery I was down to 105 pounds, and I’m 5’6. They didn’t have a lot of skin to get it under. There was a lot of poking happening.
I remember thinking if I might ever know what it would feel like to be in a bar fight, this is what it was like, because I couldn’t even move. It took five days for the pain to go away.
I told several people that, and they agreed people do not prepare you for how uncomfortable you feel after the [port surgery].
Maybe it was also because I was recovering from surgery. I had a power port so they could draw blood out of it. I could get chemo out of it. It was this little purple thing that went up and connected in the major vein, but I didn’t realize it was up here [on my chest].

Did you have to get labs before chemo infusions?
I lucked out and got to have all my labs the Friday before, and I was getting chemo infusions on Monday. But I did have pre-chemo bag of anti-nausea and steroids, so that adds some time.
Tips on getting through the actual chemo infusions
I am not normal when it comes to the chemo side of things. I slept the entire time. From the second it started dripping around 8 a.m. till about 1 p.m., I slept through the majority of the time.
There’s a lot of moving around. I had two nurses. I was at an eight-chair clinic, only gynecological oncology. We all had the same two nurses in this open square, with a couple seats in the middle. My mom, my dad, and usually a friend or two would come. They would entertain themselves because I was sleeping.
But I was prepared. I had a friend who’s amazing. She gave me all the tips and tricks, and I probably looked like a bag lady because on the off chance I felt good, I wanted to make sure I had things to do.
I had an iPad, my computer, books, all these other things they tell you to do, but I didn’t use one of them.
I brought snacks and didn’t eat them. But I did line my chemo chair with a blanket and had another blanket to put on top of me because it is cold in those clinics. I wanted to be as comfortable as I could be.
The nurses always laughed and thought it was so funny because I’d walk in, get everything situated, [and] then go to my doctor’s appointment and do my chemo.
I passed the time by sleeping. That’s all I can say. I know a lot of people will color or do crossword puzzles. I did drink a bottle of Gatorade while I was there for electrolytes. Water tasted awful to me, so I couldn’t do that.
Take things to entertain yourself. My dad went through chemo, too, right after I did. I don’t think he slept. He had friends who’d come in and out, so he just talked a lot while he was doing it. He’s not really a reader, so he’d just have people come and visit with him.



Describe the chemotherapy side effects
Day 1, I went into anaphylactic shock. I was allergic to Taxol. Normally you have an allergic reaction between the 10- or 13-minute mark. I was at the 15-minute mark. It came on. I got hot and was telling my mom. I tried to cough, but I couldn’t breathe.
On my first day, I thought that I was not going to be able to receive this drug, and now what would I do because this was my only chance of living? That’s not what happened. They gave me plenty of things to reverse the side effects.
I then got some fluids. Then they started it over again very slowly. A lot of it has to do with the speed at which you drip, too. I was a very slow dripper since I got sick from it.
The weird thing is with Taxol, the longer you take it, the less reaction you have to it. With carboplatin, the longer you take it, the more chance you will have an allergic reaction to it.
They were really worried that I was going to, toward the end of the rounds, start having a reaction to carboplatin, but I didn’t. I lucked out.
They also say that you’re going to get the steroid high after your chemo when they give you the steroids to take. I never got it. As soon as my chemo started dripping, I got extremely sick. I was in bed, nauseated, and whatever for at least five days straight.
I ended up back in the hospital after my fourth round to get a bag of fluids. That was the worst I’d ever been. That was the only time I was wheeled in and out of the hospital, other than my debulking surgery.
Outside of that, once I got through the five days afterwards, it was a lot of nausea until I got into the last four or five days before heading back into chemo. I felt pretty decent in those days.
Nausea is hard to explain, as well as the fatigue. I also had a heavy metal taste, which is common with the type of chemo I was given.
»MORE: Cancer patients share their treatment side effects
What helped with the chemo side effects?
I tried everything, and they told me they wanted me drinking about 100 ounces of water a day the first couple of days after the infusion. I choked that down. The only way I really got through the nausea part was I slept.
I had two different anti-nausea medications. I was able to somehow piggyback them. I knew Zofran wasn’t going to work because when I was pregnant I had nausea, and it didn’t work. I told them it isn’t going to work. They said it was really made for this nausea, not pregnancy, but it didn’t help.
I could time it to come up with a pattern to be able to stagger the medications; that was best. Don’t wait until you get sick. They tell you you will get sick, so just go ahead and start taking the anti-nausea pills because once you’re to that point, there’s no coming back. It just doesn’t work.
I was in surgically-induced menopause. I remember the night sweats from the chemo and the menopause, and how everything was, after the infusions, amplified so much.
Hair Loss
When did you start losing your hair?
They told me by the time I came back for my second round of chemo, all of my hair would be gone. I anticipated that it would start falling out two weeks later or that it would be gone two weeks later.
It wasn’t my choice on how to go about doing everything [after the diagnosis]. I was going to make sure this [hair situation] was my choice. You can tell me I have to do this, that I have to do that, but on the things that are my choice, I’m going to own them and make them my own.
I knew going from having hair to having none at all was going to be really difficult for the kids. In my mind, what could I do? Twelve days after my first round, I had decided to have a head-shaving party. My two kids and my friend’s daughter, who I call my niece — she was maybe one and a half. They shaved my head.

Describe the shaving party
Olivia, my daughter, got the first swipe at it. One of my girlfriends helped her. But the funny thing was I was trying to do everything to not have a nervous breakdown during all of this. There’s a video of this.
My son just kept saying, “Mom, Mom!” I was like, “What?!” I felt so terrible looking at the video. He’s like, “It’s black,” and I was like, “What are you talking about?” My hair was blonde, but I had dyed it blonde with highlights.
He had never seen me with dark hair, so when they went and took the first swipe and it was dark brown, it lightened the mood. I laughed and everything.
They did pretty well with all of that. Then one of my girlfriends went into my bathroom with me afterwards, and we took it down significantly to where it was just stubble. She said we should probably clean it up and get it a lot shorter. It’s going to fall out and be everywhere.
One of my other girlfriends had stayed the night with me that night because my kids weren’t there. They ended up going back to their dad’s place after we did the head shaving party. My friend stayed the night, and the next morning I woke up screaming for her in the shower.
The first three weeks, someone had always sat in my bedroom while I showered in case I needed help because of the surgery. She came running in and was like, “What’s wrong?”
I told her, “It’s all gone!” She was confused. But it was all of my hair, including my body hair and hair on top of my head, decided to fall out the day after I shaved it.
I lucked out and totally took control of it. All I had at that time was my eyelashes and eyebrows, and maybe a couple strands. But I used a towel to go around and try to get the rest of it to come off.
My dad lost his hair with his non-Hodgkin lymphoma. The hair was sensitive when it fell out. It hurt. It was this main front part that hurt the worst.
It was very unexpected and not something you would think of because your hairs are supposed to be dead, anyway, so you wouldn’t think there’d be feeling in your scalp, but that wasn’t the case. That threw me for a loop.

When did you lose your eyebrows and eyelashes?
After Round 4 is when my eyelashes and eyebrows became very few and far in between.
When I had my eyebrows but not my eyelashes, it still looked kind of okay. But when they eyebrows go, you have no idea how important they are until they’re not there.
The worst part for me was I kept them thinly until after my last round. They had warned me, “Three weeks after your last round, you’ll look your worst.” I just wanted to be done.
Not having to shave was the best thing ever, but then it was the first hair to grow back! I was like, “Why can’t the hairs on my head grow as fast as the hairs on my arms and legs?”
Tips on dealing with hair loss
I got a wig because I thought I was going to wear one. I did not know what I was going to look like without hair. I had no idea what my head looked like. I’d gotten a wig even before I started treatment, so I didn’t have to worry about it in case I was super sick.
I loved it. It was beautiful, long, [and] totally different. I still have it, but I wore it twice, maybe three times.
Olivia wanted me to have a wig. This is important on the kid issue. The first thing I wore it to was a school poetry night event. She wanted me to wear it.
But it was so hot, and being in menopause, all I wanted to do was throw it to the side somewhere. I wore it there, then within a week or two after, we were leaving to go on spring break.
I didn’t wear my wig much. I wore it to a friend’s wedding because that was her day, and I did not want my bald head sitting at the reception or during the ceremony to take away from her day. So I wore it there.
I was pretty cognizant of those types of things, because even though you don’t think people are looking, it’s distracting. I didn’t want to take away from her with a, “What’s wrong with you?”
»MORE: Dealing with hair loss during cancer treatment

Dealing with being bald and children’s concerns
We were going to be on an airplane, going down to Florida to the house, and I said, “Liv, I know that you really want Mommy to wear her wig, but I’m not going to because it’s going to get a lot of germs on the airplane. I’m not going to wear it in Florida; it’s too hot.”
She started to cry. I asked her why she was crying. She said, “Because people are going to make fun of you. I see the way they look at you.”
I asked her, “Do you think people don’t know that I’m sick? Because they all know the reason I don’t have hair. Mommy has this port here, they know I’m sick, and they’re not going to make fun of me because they know I have cancer.”
She said, “But you didn’t tell them.” I told her that for her, when she saw people like me, she knew they probably were undergoing some form of treatment that caused them to lose their hair.
It had never registered in my mind that she would be more concerned about that, and she didn’t want my feelings to be hurt.
She was afraid people would make fun of me and didn’t realize the reason they probably looking at me was because of my age, why at such a young age I didn’t have my hair.
But I got the wig because I wanted my kids to be more comfortable if we were in a setting. I did not realize she was asking me to wear it to protect me.
Her friends saw me with a wig and without a wig. The girls said nothing. The boys were the most intrigued with the whole thing. It was hysterical!
Jaxson was in pre-K at the time, and the little boys in his class didn’t know what to do. I would lean over so they could feel the wig. I said, “It’s okay. I’m the same person!” It was hard for them because I didn’t look like the same person.
When you’re three years old, you can’t figure out what’s going on. This woman is speaking, and it sounds exactly like Jaxson’s mom, but it doesn’t look like Jaxson’s mom. I don’t wear it different places, and they all got used to me having or not having it.
The kids at Olivia’s school were on a field trip, but it got hot that day. I was Hot Flash City, so I had it off and had a hat on by the end of the day. One of the girls was walking by and said, “Where’d your hair go!” Another girl said, “She has cancer, okay? She doesn’t have hair! That was a wig!”
I was just like, “Oh my gosh. I don’t know what these kids go home and tell their parents!”




End of Treatment
How did they track progress of the chemo on the cancer?
They didn’t do another scan until I finished the first-line treatment. I got done with that, and I remember leaving my sixth round of chemo. I had to have Neulasta [shots]. I hated it, but I didn’t think I had to have it after my sixth round.
We went through the end of the chemo treatment, and I asked not to do it because I didn’t feel like it mattered what my white blood cell count was. It would eventually come up.
My nurse told me that’s what they hoped for, but she had to prepare me that if my scans didn’t come back right, I’d have to do a few more chemo rounds.
That thought had never crossed my mind. I was like, whoa! It’s just not something you prepare for.
When did you learn you were in remission?
I had a scan afterwards, and on July 3rd was when I would get my results. I went from June 5th, Jaxson’s fourth birthday, my last day of chemo, to then coming back to do my scans, all my labs.
Then I went in and found out that I had no evidence of disease (NED), and we were able to move onto the three-month mark.
What was the follow-up protocol?
For the first two years, I had to do just blood draws. We would do scans as needed. Everyone talks about how you have anxiety around all of this, and so be prepared for your mind to play tricks on you.
It was every three months for my first two years, then years three until five I’ll go every six months. Then at the five-year mark, I’ll go in annually.

Reflections
How were you able to be your own advocate?
I went into that appointment on July 3rd and had the resident I had all the time. She was doing her rotation. She came in, and I said that I was going to tell her that this was all on my head, but I think there is a lump, or something is causing me to have to go to the bathroom frequently. I feel a bump right where the tumor was.
She felt around and said she’d grab the doctor. Ends up, I did have a bump, but it wasn’t cancer. It had shown up on the scan.
What I had was a pocket of lymphatic fluid that was filling up where the tumor would have been. It was pushing down on my bladder, mimicking the same symptoms I would have had.
Usually they don’t bring it up when it shows up on a scan, because most times, people don’t have a reaction to it. Unfortunately, I did. So I got a drain for it.
But I say this because even if you think you’re making something up in your head, just acknowledge you’re probably really nervous and that’s why you’re feeling these things.
Sometimes, it really could be something, so don’t downplay what you’re going through. Let them know. It’s normal for us to feel something. Go ahead and say it in case it really is something, which it was in my case.
»MORE: How to be a self-advocate as a patient
What’s your top advice for current patients?
I would tell anyone dealing with a diagnosis to decide yourself what is the best plan for you:
How you want to receive information, how you want to lose your hair, how you want treatment to go, [and] whom do you want to be a part of this? It’s all your choice.
You don’t have to do what everybody else is doing. We have those caretakers around us. Although they feel they are going through it with you, they are not going through it. It isn’t happening to them. That’s something that not only you have to remember, but they have to remember.
I don’t want to downplay their role at all, because I would never be able to repay my caretakers for all that they gave up in order to make sure I was okay.
It is going to feel like you are going through the worst possible thing ever, but if you can put one foot in front of the other, you will get to that finish line, whatever it is. Then you take the next steps.
You take each step at a time, and once you get a plan in place, things start to seem a whole lot easier because you figure out what to do. You focus on that.

Top message for others
For those of you who’ve just finished treatment and you are stuck at the edge of the cliff, where you feel your doctors are pushing you off the edge and you’re a baby bird with no idea on how to navigate all this, none of us do.
Your life is completely different. It’s not a bad thing. It takes a while to adjust. Figure out what works for you.
It’s not going to be the same as it was before. Maybe you don’t want it to be the same as it was before because you’re realizing things now that you wouldn’t have in the past. I know that’s how it is for me.
Do I miss the carefree, being naïve to all that is cancer? Absolutely, I do. If you read anything on my social media, you’ll see from time to time I’ll say my favorite place to have a breakdown is the shower floor because it’s quiet and nobody can hear me.
Even though I look upbeat and positive all the time, you’re still allowed to have our moments. Because it wasn’t fair; it shouldn’t have happened. My body still hurts, and I still have to go to these appointments. It’s exhausting. I get it. You’re going to be able to figure out how this works.
It just takes a little bit of time to navigate. It’s new, different, and as humans, we don’t like new and different.

Dealing with survivorship
I had a lot of pre-warning on not expecting things to go back full swing, but until you have the diagnosis of cancer and you’ve gone through chemo, you don’t realize that once the treatment stops, it’s not necessarily over. You still have the side effects — the fatigue, aches, and pains — for some time afterwards.
People around you expect things to go back to normal and it’s just going to be the way it was before, but unfortunately, that’s not how things work. It’s not a bad thing. It’s just the way it is.
New perspective on life
Some people are like, “You’re just saying that; you’re blowing smoke.” But I’m not.
I think I’m a better person, or at least a better version of myself, because I don’t feel like I have the time to say that I have time. The chance that you don’t have that time happens. You realize you should adjust some things and change for the better.
Inspired by Randalynn's story?
Share your story, too!
Ovarian Cancer High-Grade Serous Stories
Randalynn V., High-Grade Serous Carcinoma, Stage 1C
Symptoms: Pulling sensation when emptying bladder; abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), surgery
...
Shirley P., High-Grade Serous Carcinoma, Stage 3C, BRCA1+
Symptoms: Pulling sensation when emptying bladder; abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), de-bulking surgery, PARP inhibitors
...
Suzann B., High-Grade Serous Carcinoma, Stage 3C, BRCA1+
Symptoms: Inability to urinate
Treatments: Chemotherapy, de-bulking surgery, total hysterectomy
...
Susan R., High-Grade Serous Ovarian Cancer, Stage 4
Symptoms: Pulling sensation when emptying bladder, abdominal pain
Treatments: Chemotherapy (carboplatin & paclitaxel), surgery
...
Sara I., High-Grade Serous & Clear Cell Carcinoma, Stage 3A
Symptoms: Random sharp pains, unrelated scan showed ovarian cyst
Treatments: Debulking surgery, chemotherapy (carboplatin & paclitaxel), PARP inhibitors (clinical trial)
...




