Stage 4 Stomach Cancer Surgery at 28-Weeks Pregnant: Arelly’s Surprising Story
When Arelly received her stomach cancer diagnosis, a look back at her experience revealed just how critical awareness and advocacy are for patients navigating troubling symptoms. Her life as a mother and wife was upended in early 2024, moments after surgery exposed a malignant tumor. Her case underscores the urgent need for better screening and listening to every patient’s voice, particularly for symptoms like fatigue and persistent pain in individuals who are often told they’re “too young.”
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Initially overlooked by medical providers, Arelly’s symptoms, including pain after gallbladder removal and unusual exhaustion, were attributed to routine postpartum changes. Yet, a growing mass during her third pregnancy drove multiple ER visits and eventually life-saving surgery. The path to her stomach cancer diagnosis was marked by self-advocacy, perseverance, and partnership with her husband, who documented her symptoms and supported her emotionally through critical hospital stays.

Family remains Arelly’s anchor and inspiration. Her experience balancing motherhood and cancer treatment highlights the unique challenges facing patients with young children. She describes learning to cherish “sunshine hour” visits, communicate openly with her kids, and plan family time around her treatment cycles, showing that quality of life is built on routine moments together. Online communities and peer support have helped her process grief and find solidarity with other patients.
Arelly now advocates for early screening and self-kindness, urging others to use their time well and embrace lessons learned. Her words, “Time is your biggest asset,” aim to empower those facing gastric cancer to prioritize courage, connection, and compassion in redefining their experience.
Watch Arelly’s video above and read through the edited version of her interview transcript below for more on how:
- Listening to one’s body and advocating for answers is vital when symptoms are overlooked or dismissed
- Family support, routine, and open communication are crucial in balancing treatment and parenting
- Community connections with other patients provide essential emotional support and solidarity
- Time spent with loved ones is the most valuable asset for any patient
- The experience transformed Arelly into a stronger advocate, teaching her to value mindfulness and kindness in daily life
- Name: Arelly R.
- Diagnosis:
- Stomach Cancer (Gastric Adenocarcinoma)
- Age at Diagnosis:
- 38
- Staging:
- Stage 4
- Symptoms:
- Nausea
- Blood in stool
- Side pain
- Extreme fatigue
- Excessive burping
- Treatments:
- Surgeries: gastrectomy, port placement
- Chemotherapy
- Immunotherapy
- Targeted therapy: antibody-drug conjugate
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Arelly
- First red flags during my pregnancy and postpartum
- Symptoms that were overlooked or misattributed
- Feeling dismissed by doctors, and taking the H. pylori test
- Why early screening and advocacy matter so much
- Advocating for myself in the emergency room
- My husband’s support and documenting the tumor
- Hearing “cancer” while pregnant
- How I knew something was wrong before I got diagnosed
- Motherhood, hospitalization, and protecting my kids emotionally
- How cancer affected my identity and personality
- Quality of life, treatment cycles, and everyday joys
- Hair loss, body changes, and rediscovering myself
- Holding on to small happy moments
- Finding stomach cancer community and online support
- Time, identity, and redefining what matters
- My final message: forgiveness, kindness, and changing the world
My name is Arelly
I was diagnosed in late February of 2024 with gastric adenocarcinoma.
I grew up in Orange County and had a pretty happy childhood. My parents made it a point to go on vacation to Mexico every year, which is where my family is from, so I have really good, embedded roots there. I have three kids, and I am married. We just had our fourth anniversary last week.
I love to scrapbook. We love nature and visiting national parks. That is kind of our hobby, or was our hobby before I got diagnosed. We love music and going to concerts, and we spend a lot of time doing that as a family. Family is really important to me, and so is spending time doing things that I love, like music and the arts.
We saw Bruno Mars, and that was an amazing experience. We have seen Alicia Keys, Coldplay, and others. That was all pre‑diagnosis, and post‑diagnosis, I am like, okay, we have to see this person and that person. Bruno Mars is the number one.
I love shows that don’t allow recording because they make you be in the moment. We are on our phones all the time.
First red flags during my pregnancy and postpartum
The beginning for me really starts with my middle child’s pregnancy, my toddler, who is going to be four in May. I had a CT scan that was normal, and that pregnancy looked normal on paper. I had a lot of pain during it, but overall, everything was considered fine.
After I gave birth, I went through all the postpartum things. I ended up having my gallbladder removed about a year after he was born. It was via C‑section, and I was having a lot of pain on my right side. They removed my gallbladder, but after the removal, I was still having pain. I kept saying, “I am still having pain on the right side,” over and over. They would answer, “That is normal because you just had surgery.” Anytime I brought up a concern, it was, “That is normal.” Stomach issues were explained away as part of learning to function again without that organ.
My husband and I wanted to grow our family, so we decided to try for another baby. I had a miscarriage and then got pregnant again. Everything seemed to be flowing. I was not feeling anything out of the ordinary, just tired. I had a toddler, and I was pregnant. Then, out of nowhere, I had a mass protruding out of my umbilical area.
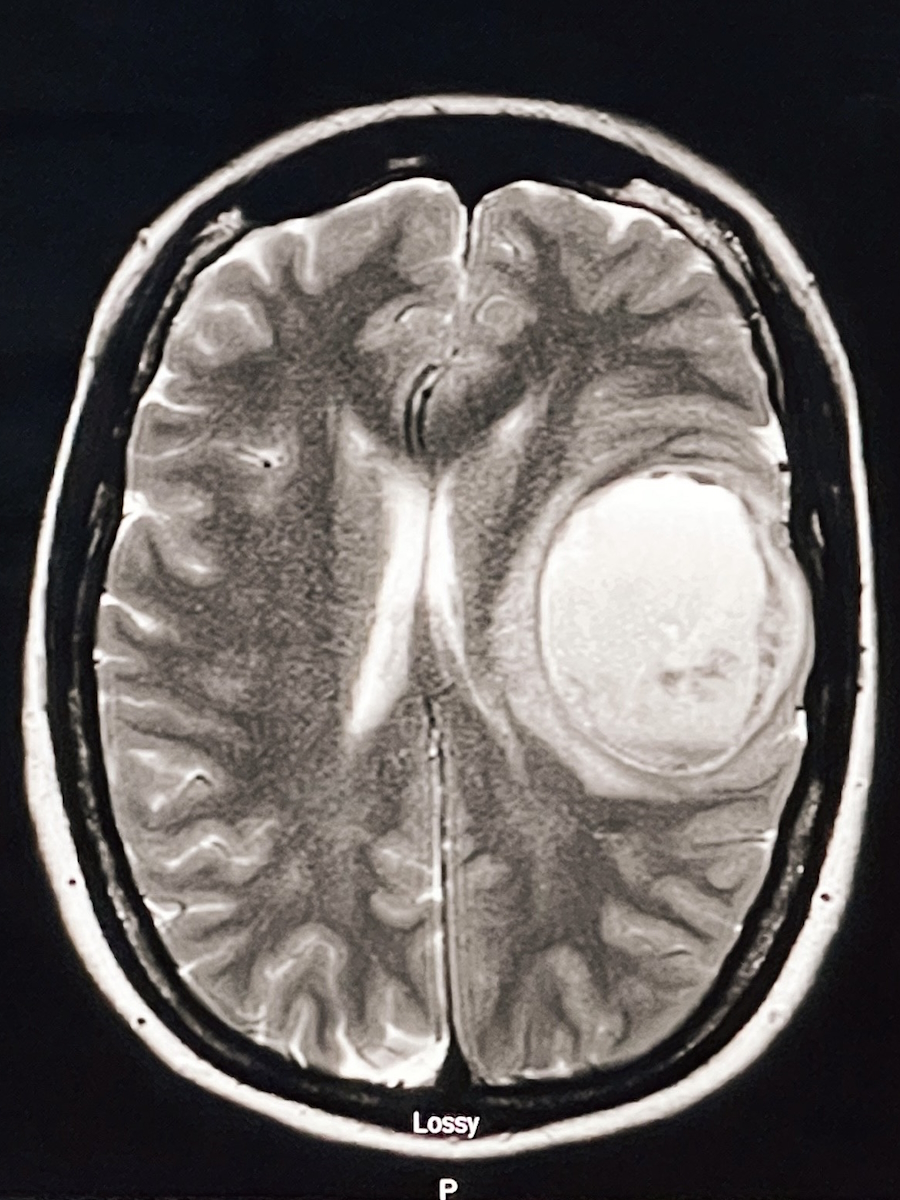
I kept bringing it up at my OB appointments. They said it might be a hernia, but they were not sure. They would just check it and send me on my way. As my stomach continued to grow, the growth pushed the tumor out more, to the point where I had two ER visits. On the last ER visit, there was leakage from the mass. That leakage concerned the surgeon enough to say, “We have to take this mass out. We do not know what it is. Your baby is going to be fine, but we need to remove it.” I was about 28 weeks pregnant in 2024.
The next day, they removed around a 15 cm mass. They told us it was a malignant tumor. That was when my OB recommended transferring my care to another hospital that could handle both the high‑risk pregnancy and the new cancer diagnosis. Hearing the word “cancer” and then “stage four,” and then phrases like “three to six months to live,” was devastating. I had pregnancy, postpartum, symptoms that mimicked postpartum, and a recent gallbladder surgery, all happening around the same time. It is all masked within everything you are already going through. It felt like we hit a wall, everything slowed down for a second, and then everything picked back up again. We have just been running with it since.
Symptoms that were overlooked or misattributed
The most prominent symptom was fatigue — extreme, extreme fatigue. There was one time when I had blood in my stool. I assumed it was hemorrhoids because I was pregnant, so that is what I told myself. Besides that, I cannot pinpoint anything dramatic. I did not have constant headaches, and if I did, I would think it was something like high blood pressure from pregnancy.
Mostly, I was just always exhausted, physically and mentally. Later, the symptoms became more visual. I could feel and see something strange in my belly. Looking back, I would also include the right‑sided pain, which I had treated as “normal” because I had been told it was normal after gallbladder removal. Now, when I talk about it, I can see that pain is a symptom too.
Feeling dismissed by doctors, and taking the H. pylori test
I do feel like I was dismissed at times, although there were also moments that made me think, “Why are they ordering this?” After my gallbladder removal, I kept going back to my regular doctor, saying, “I am feeling these things again. What is going on?” After I complained three or four times, he finally said, “Let me give you this H. pylori test.” I did the test before I got pregnant with my third, and it came back negative.
I know H. pylori can be a cause of some gastric cancers, but I do not really sit and wonder what caused mine or what I could have done differently. I do not ponder that because there is no point. That is the one thing he did, ordering that test.
Around the same time, my best friend had just gone through her own journey with breast cancer while pregnant, so I was very cancer‑aware. She is a survivor now, but back then, it was very fresh. I told my doctor, “My friend just had breast cancer. When should I get checked?” Instead of something like, “You should start at this age,” he said, “You know cancer is not contagious, right?” I remember freezing and thinking, “That is not what you are supposed to say to me.” I do not know if he realized he said it like that.
It was during COVID, and many appointments were by phone or in rushed in‑person visits. I do not want to say I lost trust in doctors, because there are amazing care teams out there, like the team I have now; but they are human, and sometimes they just do not see things or think about them. That comment and the repeated dismissal of my symptoms made me step back and lose trust in some of the medical staff at that time.
Why early screening and advocacy matter so much
That whole experience ties into how I feel about screenings, especially for gastric cancers. Screenings are so important. Right now, I am very passionate about advocating for earlier screening, because we are seeing cancer in younger people so often. That is one reason I do things like this: to create awareness that you are never too young to get cancer. Children get cancer. So why do we have these strict age protocols telling us when we “qualify” for colonoscopies, endoscopies, mammograms, and so on?
We need to take into account people’s histories and symptoms and what patients are actually saying. If someone keeps saying, “This does not feel right. I feel this and this,” that should matter. Doctors have the expertise; we do not. We are the patients. They are there to help us and to listen.
Advocating for myself in the emergency room
By the time I was going to the ER repeatedly, my advocacy became very simple and direct. It was like, “I am here now. I was here two days ago. You sent me home. I cannot be sent home today. Please, what is going on? Please take a look at this.”
It is important to be able to say, “I know my body. I know what is normal and what is not. Please listen.” The sad part is, I have heard many stories from people I have met in the stomach cancer community who said all those things and still were not heard.
So a lot of it becomes repetition: “This is not right. This is not right. Please look into this. What tests can I take? This is not my normal.” At one point, I was literally saying, “Look at this. This is not normal,” because sometimes they would not even physically examine me, just listen and move on. It was crazy.
My husband’s support and documenting the tumor
My husband has been such a key part of this. In the beginning, he took a lot of pictures of the tumor. It is funny because we have different sets of photos. I have certain pictures in my phone, and he has others in his. He took pictures of the tumor as it progressed. I did not want to look at them; I did not want to even see my own belly button with the tumor pushing out.
He did it so that when we went to the ER and doctors needed context, he could say, “This is what it looked like a week ago, and this is what it looks like now.” That helped us show that things were not improving; they were getting worse.
The last time we were at the hospital before they removed the 15 cm mass, the mass looked red. In the report I read later, they said it was infected. It had gotten to the point where the surgeon on call around 7 p.m. was worried about sepsis. He said, “Whatever it is, we have to take it out, because you can die of sepsis.” Hearing “sepsis” before hearing “cancer” out loud was very scary.
My husband has always been there, especially when I could not articulate or face certain realities. When I had blood clots, he would take pictures to track whether they were getting better or worse. He tried not to panic, because if he panics, I panic. He is the calm, and I am the “That does not look right” person. We really balance each other out in that way.
Hearing “cancer” while pregnant
By the time I officially heard “This is cancer,” I had already had major abdominal surgery while pregnant. I was barely moving and barely conscious in a small hospital room. I already had a feeling it was cancer. My OB called me because he was not at the hospital. He said he needed to come talk to me. I said, “I already know. Can you just tell me?” He did not want to tell me over the phone, but I insisted, and he finally said it looked like cancer and that he wanted to transfer me to UCI.
Once I was transferred, it became a night‑and‑day difference in care. They monitored me around the clock because they had two lives to keep stable: me and the baby. At UCI, there was a team of about ten people involved: baby specialists, oncology teams, and people focused on post‑surgery recovery. They were constantly checking me and checking the baby, trying to figure out exactly what type of cancer it was.
It was overwhelming. Sometimes there would be ten to fifteen people in the room in white coats talking to me at once. Even now, my husband and I sometimes sit in the quiet when the kids are asleep and ask, “Is this life even real?” It still does not feel real sometimes. I can picture myself in that hospital bed, in pain, with everyone talking, and I am half-listening, half-tuning them out because it is too much to process.
How I knew something was wrong before I got diagnosed
I had a sense that something was going on with me even before the big tumor showed up. Because I am over 35, I had NIPT testing during my pregnancies. It is genetic testing for the baby, and everyone thinks of it as a gender test, but it looks at more than that. With my third son, Benjamin, I had to do the test twice, and both times it came back inconclusive.
When I spoke with the genetic counselor and looked back at the report, there was a note at the bottom saying they could not get genetic information for the baby because something in the mother’s DNA was impeding it. Of course, I went online and started researching why other people’s NIPT results were inconclusive. I went down that rabbit hole and started wondering if something was going on with me.
I was also dealing with a lot postpartum with my middle child and was already in counseling. A lot of my biggest fears centered around not being able to take care of my children and something happening to me so that I would not be there for them. Looking back, I feel like my subconscious was preparing me, telling me this might be my reality.
The fact that the NIPT had been normal for my toddler but not for the baby also gives me a rough timeline. I know that in one year, I likely did not have cancer, and by the next, I did. That shows how quickly this type of cancer can progress. The type I have is rare and spreads like fire.
Motherhood, hospitalization, and protecting my kids emotionally
When I first got my diagnosis, I did not worry about my unborn son’s safety as much as you might expect. I felt deep down that he would be okay. I did not even focus much on myself. I just had this feeling, pregnancy‑wise, that he would be fine.
What crushed me more was being away from my older two kids for those two weeks in the hospital. My oldest was around seven, and my son was about one and about to be two. They did not really know what was going on. All they knew was that Mommy and Daddy had disappeared to the hospital for a long time. My parents and family stepped in and cared for them.
There were lots of video calls. We would tell them, “Mommy is at the hospital,” but I did not say, “Mommy has cancer.” They do not know what that is. We just tried to reassure them that I would come home soon.
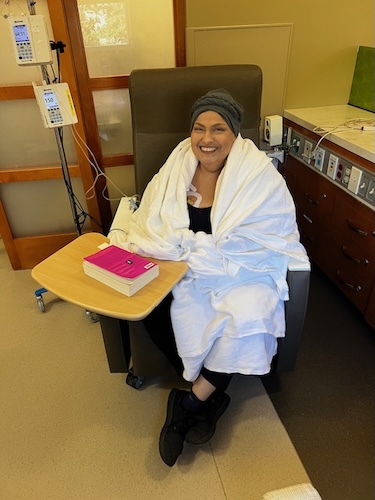
When I started feeling better, the hospital had a “sunshine hour” where I could go outside for an hour, even while hospitalized. I would be hooked up to my IV while my husband wheeled me outside in a wheelchair. The kids would visit, and we would sit together and have something like a little picnic or cafeteria time as a family. I was still pregnant and recovering from surgery, but those visits meant a lot.
Eventually, I came home, and we focused on spending as much time together as we could before chemotherapy started while I was pregnant. I had a port placed, went through endoscopies, colonoscopies, and other testing. I got to be with my kids before Arthur was born.
After that, life became chaotic. There is the cancer itself and being a cancer patient; there is also being a mom of three, with two of them being two and under. That balance is what has kept me going. They are my motivation. I still deal with a lot of mental battles, but they keep me grounded.
How cancer affected my identity and personality
Cancer does not just attack your body; it attacks your personality and who you thought you were. I am in the middle of figuring out who I am now, accepting that I am a mother of three and also a terminally ill person who has to think about leaving all these things behind. That is something no one prepares you for. Almost as soon as you get a serious diagnosis, people start asking about your “dying wishes.” I have not confronted all of that. I process it in small pieces.
People who are not in this situation will say, “Take lots of videos. Take lots of pictures. Live your best life.” And I do try to do those things, but I am also so tired. So I focus on quality time. I want my kids to remember that when I felt okay, I was present with them. I know there are many days when I am knocked out after treatment and just have to rest, but when I do feel okay, I make an effort to say to my husband, “Let’s do something with the kids this weekend,” even if it is just the zoo or the aquarium.
I also had to tell my oldest daughter the truth at some point. She is going to be ten, and she is very aware. I was diagnosed in late February, but I waited until school was out around May or June. I wanted her to finish the school year without that weight. Over the summer, I told her, “Mommy has cancer,” so we had time to talk and for her to process it. Just yesterday she said, “Mom, I wish you did not have cancer,” and I told her, “Me too, baby.” I am glad she knows. I do not want her to feel, later on, that I hid it from her. With the little ones, it is different. My three‑year‑old just knows I am sick and that I go to the doctor, and that I have a port he can touch. He does not understand cancer.
Quality of life, treatment cycles, and everyday joys
Quality of life has become central to how I navigate treatment. Over time, you become an expert in your own body. I know my regimen: I get treatment every three weeks. The first week tends to be okay, the second is usually the worst, and then I get a few better days. We plan our lives, and especially family outings, around those better days.
On days when I am present, I try not to overthink it. We just do normal things: read a book together, work on my son’s preschool projects, or scrapbook with my daughter. I have always loved scrapbooking, and now I am teaching her how. Communication with my husband is key. I will say, “These are the days I think I’ll feel okay; let’s try to do something then.” Sometimes it does not work out, and the day is worse than expected. In those cases, I try to give myself grace and accept that it is okay not to feel well.
My husband has also been a 100% caregiver through this, and I admire him so much. He potty‑trained our toddler, handles diaper changes, and takes care of both the kids and his wife with a terminal illness. I try to remember to ask him, “How are you feeling?” because he rarely gets a break. When he does get a break, I am thinking, “Who takes care of the kids then?” Our parents help as much as they can, but they are older, and we try to save that help for when it is really necessary.
We also try to carve out time for our marriage, not just parenting. On good days, we might go to a concert or try to do something just for us. When I am feeling okay, I will say, “You take a break,” and I will be the supervising adult once the kids are asleep, hoping my body cooperates and there are no emergencies.
Hair loss, body changes, and rediscovering myself
My first year of treatment was strange in that I did not lose any hair. I did not look like what people imagine a cancer patient looks like. There is no one “look,” but society tends to picture someone thin, frail, and bald. I am a heavyset woman, and I still had my hair then, so I did not fit that picture. Then I started a new treatment, and with the very first infusion, I lost all my hair. That was when it really hit me.
Hair is wrapped up with identity. You think you will not care that much, but you do. Chemo also makes you exhausted and changes your skin. I will look back at a picture of me when I was pregnant and see this glow. Then I look at myself now, and I look different. I often put on makeup, and my husband will ask why. I tell him, “I do not want to feel like I am dead.”
It is not just physical. A heavy diagnosis brings heavy thoughts. You have to confront things like death and how it might happen. I was preoccupied with that in the beginning. Now I try to avoid overly dwelling on it. When I feel myself going down a bad spiral, I let myself feel it fully for a day. I ask, “What else have I been holding back? What else do I need to feel?” I let it all out. The next day, I say, “That was yesterday. Today is not going to be that day,” and I try to start over with better energy.
Holding on to small happy moments
Happy moments now are usually small things that might be easy to miss. I used to love cooking. That was my love language. If my husband liked noodles, I would think, “Let me make this noodle dish,” and it made me happy. Earlier this year, I had ascites so badly that I needed to be drained twice a week. I could not walk or even shower on my own sometimes, let alone cook. Cooking was just not possible.
When I do have a day where I can cook, it feels huge. I notice it, and my daughter notices it. She will say, “Mom, thank you for this food,” and I recognize that I did something important just by making a meal. Those are the happy moments now: sitting at a table, eating together, and being able to participate.
Sometimes our evenings are staggered. My daughter comes home from school, and we are immediately in night‑routine mode with the younger ones. We do not all sit and eat together. On the days we do manage to eat at the same time, we notice it. We say, “We are all here together,” and that becomes the memory we hold onto.
Finding stomach cancer community and online support
At first, having this diagnosis is very isolating. You do not know where to go. My best friend was my first lifeline because she had gone through breast cancer. We talked almost every day. Outside of her, I started finding online support in stomach cancer‑specific groups and foundations. I joined groups where people have gastric cancer like me, including younger parents.
We have lost many people from those groups, and it hurts because they become like family. It is powerful, though, to connect with people who share similar circumstances; not just the same cancer, but also being young parents, dealing with caregiving, finances, fear, and all of it. Sometimes we talk about cancer; other times we talk about normal things just to feel human.
November is a heavy month in the stomach cancer world because it is Stomach Cancer Awareness Month, and also when we tend to remember and lose many friends. There was a woman named Rita whose situation really resonated with me. My kids are half Cantonese, and her kids were half Cantonese too. She left behind very young children. Those similarities hit you hard.
We also have regular support calls every couple of weeks. Recently, we found out that one of our sisters is going into hospice because there is no more treatment left. Knowing I am headed to that reality, too, at some point, makes it all feel very close. We cry together, pray for each other, and try to lift each other up while still respecting that no two people experience this the same way.
Time, identity, and redefining what matters
One big lesson from all of this is about time. Time is your biggest asset. I am very careful with where I give mine now. Texting someone back takes time. Taking a call takes time. If I am giving you my time, it means you matter to me. I tell my friends and support sisters that, and they understand, because they are living it too.
I also realized how easy it is to let cancer become your entire identity. In the beginning, I think I fell into that. You are searching for information and community, and everything in your life becomes about cancer. Recently, I have been trying to pull away from that mindset and remind myself that I was more than cancer before this, and I still am. I am funny, I am creative, I am a mom, a wife, a daughter, a friend. I am not just a patient.
When I am in the hospital three times a week, I allow myself to be “the patient” in that space. But when I go home, I sometimes tell my sister or my friends, “I do not want to talk about cancer today,” and that is okay. I step back from social media if it gets too triggering. I try to read, do something small that feels normal, or just rest.
Ultimately, it is about redefining who I am and what I want the rest of my life to look like, however long that is. That is true for anyone, with or without cancer. If you are not happy with your life, you can ask yourself why and start taking small steps. Things do not change overnight, but small wins matter. I celebrate the small wins.
My final message: forgiveness, kindness, and changing the world
If there is one thing that sums up what cancer has taught me, it is that you have one life to live and time is precious. Spend it on what and who truly matters. Try to be forgiving of yourself. When I look back at my life, I do not see mistakes as just mistakes; I see them as learning. I learned, I grew, I changed. Holding onto self‑blame does not help.
The most beautiful thing you can do is be kind and spread love. That starts with being kind to yourself. Many people are not kind to themselves, and that makes it hard to be kind to others. You do not have to change the whole world with some huge gesture or have millions of dollars. If you work on yourself and try to be a good person, that is how you change the world: one small act at a time.

Inspired by Arelly's story?
Share your story, too!
More Stomach Cancer Stories
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...