Raquel’s Stage 4 Colorectal Cancer Story
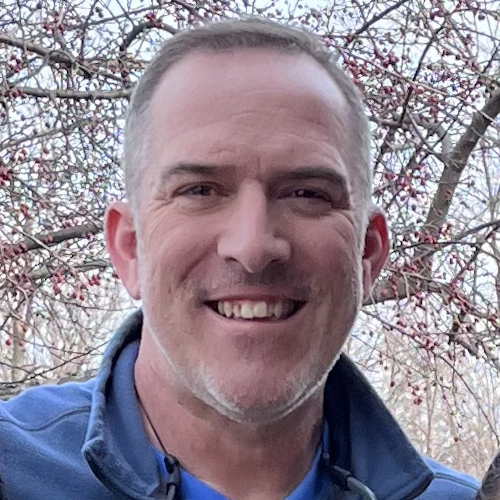
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Raquel first noticed symptoms in 2019, like pencil-thin stools, pain, bloating, and blood in her stool. She then started getting full quickly after eating.
When she finally went to the doctor after developing severe pain, she was dismissed and told, “It was just anxiety.” She then ended up in the emergency room and was later diagnosed with stage 4 colorectal cancer, which had spread to her liver, ovaries, and lungs.
In sharing her story, she aims to raise awareness about rising colorectal cancer rates in young people and the importance of listening to your body.
In addition to Raquel’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
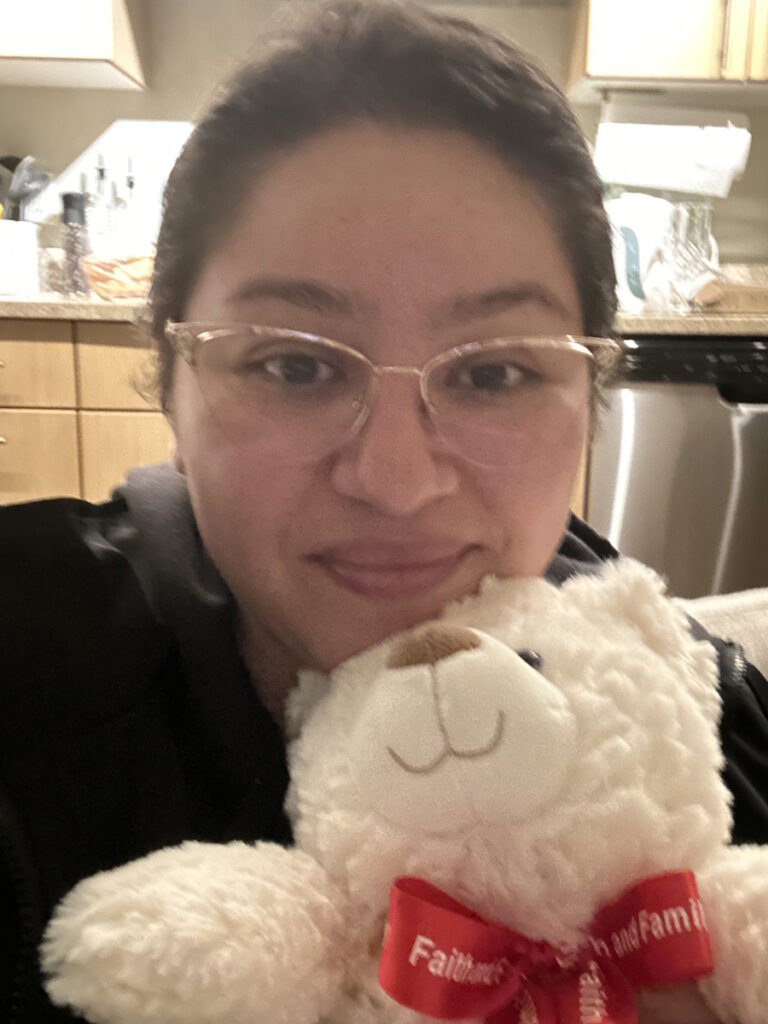
- Name: Raquel A.
- Diagnosis:
- Colorectal cancer
- Staging:
- 4
- Initial Symptoms:
- Frequent bowel movements
- Pin-thin stools
- Mild red blood in stool
- Treatment:
- Chemotherapy: oxaliplatin, 5-FU (5-fluorouracil), and irinotecan
I feel so confident that whether I can heal from this or not, I’m going to be able to handle it well. It’ll be okay. I’ve overcome other things in life and I hope that I can be an inspiration to people who are struggling.
Introduction
I’m 33 years old with terminal colorectal cancer. It has been such a huge part of my life that I have to remind myself that there are other parts outside of that.
I currently work in the tech industry and I’m very blessed to be able to do so.
In my spare time, I like reading and drawing. I’m very artistic and very recently, I’ve been posting more. I’ve been finding great connections on social media with other people who are going through the same thing as me.

I didn’t take my symptoms more seriously because they would come and go.
Pre-diagnosis
Initial Symptoms
I first started noticing symptoms in 2019. I was roommates with my best friend and she started to notice how often I was going to the bathroom. At the time, I was working in restaurant management so I figured I was probably eating too much of the food at work or eating too many processed foods.
I started changing my diet, trying to eat healthier and more protein but also using fiber supplements. I figured I wasn’t eating enough fiber and that’s one of the first things you read online about how to resolve diarrhea or bowel issues. That did help. The symptoms went away, but they would come back to plague me again.
Symptoms Worsened
In 2022, I was working as a contractor in the tech industry. I made really good friends with people on my team. One of them noticed how often I was going to the bathroom and she said, “Raquel, are you okay?” I said, “Yeah, I’m fine. Maybe it’s the dairy in my coffee. Maybe I have a gluten sensitivity.”
At the time, I wasn’t concerned and wrote myself off. I dismissed my symptoms. But knowing what I know now, I was having classic colorectal cancer symptoms.
I experienced frequent bowel movements and pin-thin stools. In addition, any kind of blood in your stool is a huge red flag. It means something is wrong. The color, whether it’s dark or mild red, pinpoints where exactly that bleed is located. Mine was mild red. I didn’t have heavy bleeding, which is why I thought there wasn’t something wrong.
But another classic sign is getting full quickly after eating and that was a huge red flag that something was wrong. That happened from 2022 until when I got diagnosed in May 2023. Every time I took a couple of bites of something, I immediately felt so bloated.
I was actively dieting before my diagnosis, but despite how healthy I was eating, I could not lose weight, which I thought was strange. My stomach was so round and hard. I would later find out that the cause of some of my bloating was ascites. When you have cancer that is as advanced as mine, especially with colorectal cancer, the tumors start secreting free fluid. I had about a gallon of fluid in my stomach that they had to drain. That immediately relieved so many symptoms I was having with eating.
I didn’t take my symptoms more seriously because they would come and go.
They’re not going to think of cancer when they see somebody who visually looks very healthy and young so I don’t necessarily blame her. At the same time, this dismissal of people who are like me is widespread because I know I’m not alone.
Symptoms Dismissed by Primary Care Doctor
It’s important to note that as a millennial—and I have statistically looked into this—half of us don’t have a primary care provider. That was the story of my 20s. I was blessed to land a permanent role in the tech industry where I had good healthcare and was able to schedule my first physical in 10 years back in May of 2023.
When you don’t go to the doctor for that long, there is a lot to talk about. I let my primary care physician know all of my symptoms, especially my bowel symptoms, and that I had severe abdominal pain somewhat recently. It wasn’t in one spot and felt very abnormal.
When I was talking to her about this, I could tell that she thought it was in my head. She scheduled me for a psychiatric appointment after my physical because she thought I had anxiety.
But now that I know so much about my disease, I know that they were classic colorectal cancer symptoms. Because I was so young, a woman, and a minority, statistically speaking, even just one of those categories is going to make you more likely to be dismissed in a medical setting and that is absolutely what I experienced.

It was maybe three weeks after that physical when my cancer was found to be completely metastatic and had spread all over. I know that she probably felt some guilt because, after my diagnosis, they sent the information to my primary care provider before I was assigned to an oncologist.
I’m sure once she saw how bad it was, she felt guilty at the same time. She’s not the only doctor who has done that, especially when you’re young. Medical doctors are taught these statistics of colorectal cancer being an older person’s disease. They’re not going to think of cancer when they see somebody who visually looks very healthy and young so I don’t necessarily blame her. At the same time, this dismissal of people who are like me is widespread because I know I’m not alone.
It wouldn’t be until I had a liver biopsy that they would find the primary source of my cancer, which was colorectal, and I wouldn’t find out until later how incredibly it had advanced.
Diagnosis
Getting the Cancer Diagnosis in the Emergency Room
I finally went to the ER. I remember that day so clearly.
I had severe abdominal pain that was migrating to my lower back and I almost fainted in my apartment. My intuition was saying that something was wrong so I went to the ER.
They did a full blood panel on me, which included the cancer markers CEA, CA 125, and CA 19. Mine were elevated. My CEA alone was in the 700s and anything above 30 is already a sign of cancer activity in your body. For mine to be that high means that my cancer was so advanced.
When I was in the ER, I felt that they took me seriously that’s why my cancer was found. The doctor knew something was wrong so she did that blood panel. I had an MRI, a CT scan, and an ultrasound. They did all those tests immediately.
The ER doctor told me that I had ovarian cancer because that’s where they found it initially. Based on the CT scan, the cancer was pretty advanced in my ovaries and my liver. It wouldn’t be until I had a liver biopsy that they would find the primary source of my cancer, which was colorectal, and I wouldn’t find out until later how incredibly it had advanced.
The metastases are in my colon, ovaries, liver, lungs, peritoneal cavity, and omentum. They found them through those tests within a week.
Everything happened so fast. I feel truly blessed that when I went to the ER, my cancer and the type of cancer was diagnosed so quickly. They ran all these tests, found my cancer, and immediately referred me to an oncologist. The next day, I was talking to an oncologist who then referred me to have a liver biopsy. A couple of days later, they found the primary source of my cancer.
Even though it’s very, very unfortunate how late my cancer was found, what an incredible experience for them to take me so seriously and find out what was going on. Kudos to the hospital that I went to. They took me very seriously.
Reaction to the Diagnosis
I don’t think I reacted like a normal person would have and that’s because I’ve had a lot of things happen in my life. I have a very calm demeanor. When things go wrong, I’m your go-to person to think logically and that’s how I processed my cancer diagnosis.
Even the doctor seemed really surprised that she said, “Raquel, you’re not even crying. I’m so sorry I’m not telling you good news.” I said, “You know what? It’s okay because no matter what happens, I’m going to get through it.”
I feel so confident that whether I can heal from this or not, I’m going to be able to handle it well. It’ll be okay. I’ve overcome other things in life and I hope that I can be an inspiration to people who are struggling. I feel like everything’s going to be okay. I told myself that even at the beginning of my diagnosis.

My liver and lung metastases aren’t responding to chemo, but the metastases in my ovaries and colon are responding moderately well. My oncologist and I are trying to see what combination could help with wherever else my cancer is.
Treatment
The treatment protocol and how they’re going to approach your diagnosis depends on your hospital. When I first got diagnosed, I was at a different hospital but for insurance purposes, I had to switch to a different one.
My treatments would have been a little bit different if I stayed with the first hospital because they wanted to start surgeries right away. They said, “You’re going to have a full hysterectomy. I’m going to be doing this in collaboration with one of our very renowned liver surgeons and we’re going to do this at the same time.”
But then when I switched to a different hospital, they told me, “We’re going to focus on chemotherapy. Let’s see how you react, shrink what we can, and then talk about surgery.” I understand the reasoning for that because they want to shrink as much as they can to lessen things going wrong during surgery or make it a little bit less risky.
Because I ended up switching hospitals, I’ve just been primarily I’ve been chemotherapy.
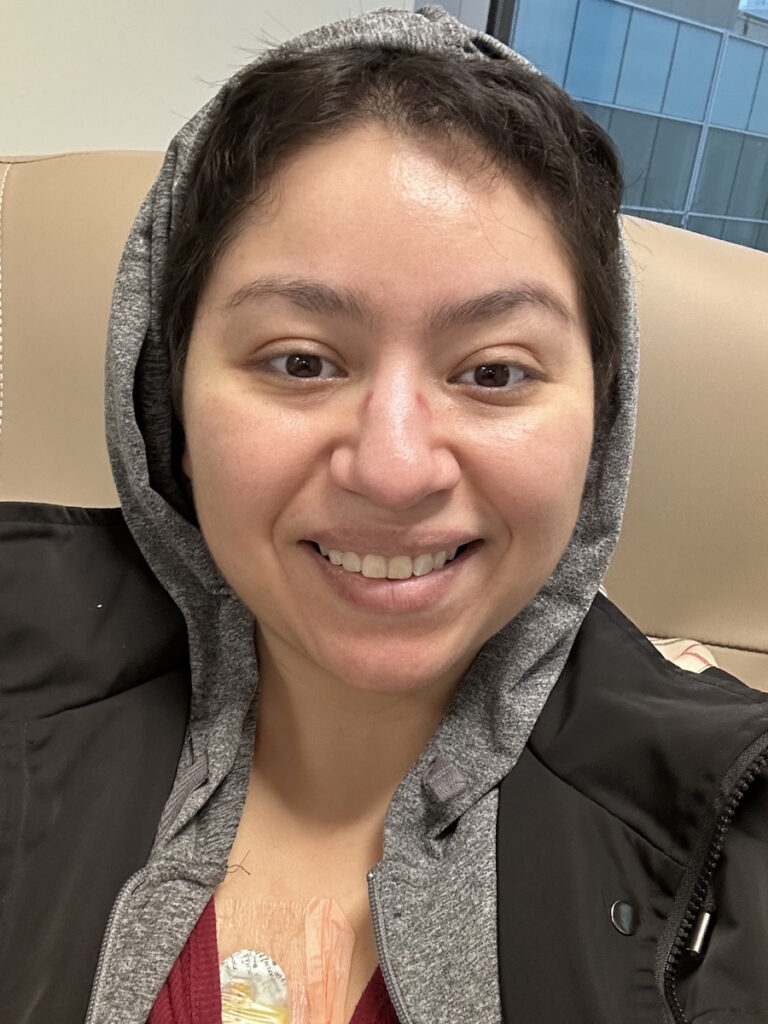
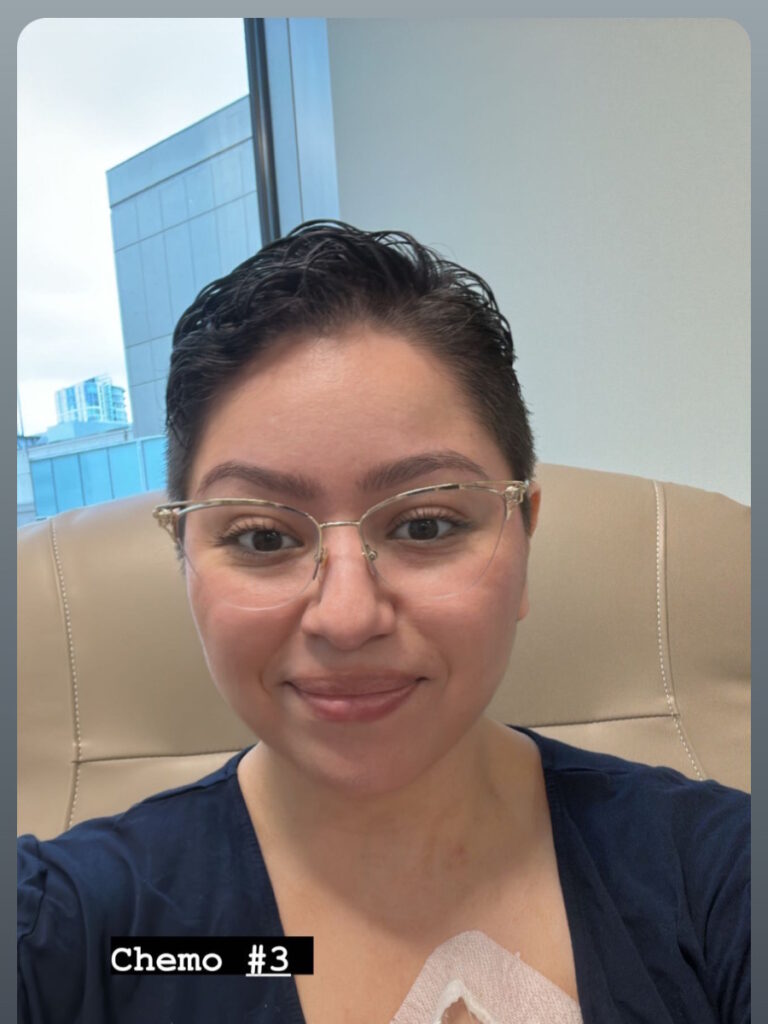
Being on Chemotherapy for Life
I first started with oxaliplatin. The side effects are not pleasant. It causes neuropathy. Fortunately for me, we stopped that in December. I was on it for six months until the side effects started affecting my quality of life too much.
I have switched to 5-FU (5-fluorouracil) and irinotecan. They introduced irinotecan to see if that’s going to help my liver metastases because so far, I’m having a mixed response to chemotherapy.
My liver and lung metastases aren’t responding to chemo, but the metastases in my ovaries and colon are responding moderately well. My oncologist and I are trying to see what combination could help with wherever else my cancer is.
I have chemotherapy bi-weekly and for Christmas, I pushed back my chemotherapy because I didn’t want to be sick during the holidays. My CEA, one of my cancer markers, jumped when I wasn’t strictly on my bi-weekly regimen. If I ever stopped chemotherapy, decided I didn’t want to continue, or changed my protocol at all, my cancer would jump at that opportunity to be aggressive.

I don’t have a choice as of right now. Chemotherapy is keeping me alive so I’m going to continue being on it bi-weekly. Fifty percent of people who have chemotherapy might need what’s called GRANIX shots.
The white blood cell count gets so low with chemotherapy that medications are needed to boost the white blood cell count to continue treatment. I, unfortunately, fall under that category so not only do I have my chemotherapy, but I have to have those shots to even have chemotherapy because my white blood cells get too low.
I’m very actively looking to find and get second opinions from hospitals that are willing to touch me and get some of this out because I know it would help me in the long run.
Looking for Other Opinions
As of now, they’re telling me that they don’t want to do surgery because of how incredibly advanced my cancer is. They’re saying that it might not be worth it.
However, I’ve read and seen from other people with colorectal cancer that they have better survivability with surgery because the more cancer is in your body, the more opportunities it has to spread and be aggressive.
I’m very actively looking to find and get second opinions from hospitals that are willing to touch me and get some of this out because I know it would help me in the long run. I will be traveling to MD Anderson and Memorial Sloan Kettering, hoping that they can do surgery on me, which will help extend my life. Even though I know it’s risky, I’m willing to do it because the alternative is being on chemo forever.
Getting Help & Support as a Cancer Patient
Having the support of family and friends has been such a huge help and I give so much thanks to the incredible people in my life who have helped me through this.
Some things have personally made it a little bit easier, like trying to buy foods that are pre-cut or pre-chopped. I like getting frozen oatmeal because I can just microwave it.
I’m sicker some days than others and I have found that it helps to have plastic utensils so that I’m not thinking about washing the dishes. To alleviate some of the guilt of buying disposables, I buy the biodegradable kind. You never think about how much something like that would make your life a little bit easier, but it does.
Give yourself grace and find the little things that you deserve to make your life easier.
If I had advocated for myself sooner, my cancer would have been found sooner… Listen to your intuition. You know your body more than anybody else.
Importance of Self-Advocacy
Self-advocacy has been such a big part of my cancer journey because if I had advocated for myself sooner, my cancer would have been found sooner. A lot of people who are as young as me or even younger don’t have a primary care provider.
Maybe they don’t have health insurance and I understand that there is a money barrier to getting treatment for a lot of people. That’s why I’ve been speaking to people who are younger than me and are getting diagnosed with advanced colorectal cancer because of those barriers.
One of the reasons why I started to be so outspoken about my diagnosis is to encourage people to go to the doctor. It’s never normal to have blood in your stool, even if it’s a little bit. Something’s wrong.
Unfortunately, if you’re young, a woman, or a person of color, you have to advocate for yourself so much more than people in different demographics. I hope to inspire people to get the medical help that they need for their symptoms because I was invalidating myself.

I went to my primary care provider and had my physical. I told her all of my digestive issues and bowel symptoms, and she said it was all in my head and that it was anxiety.
Other young people say in the comments on my social media, “This happened to me, too.” That’s one of the reasons why I’m trying to be so outspoken and raise awareness. I want people who have had the same experience to hear my story and say, “I need to take this seriously. Even if a medical professional says that I have nothing to worry about, I need a second opinion. I need to go to a GI specialist.” That is my goal in sharing my story. Don’t let anybody write you off. Get seen. Go to a GI specialist.
All it takes is one who will listen to you and help you. They’re out there. We just have to find them.

Words of Advice
Listen to your intuition. You know your body more than anybody else. A medical professional is diagnosing you based on generalities, but you know yourself better than anybody so if you are having these problems, you deserve to see a specialist and get a second opinion. Don’t listen to the first doctor. Get opinions from a second or a third, especially if your symptoms are persistent.
If your symptoms are persistent and aren’t going away, then something is wrong, especially if you have blood in your stool. That should never be written off. Any kind of blood in your stool is a huge red flag. Pay attention to it.
You deserve to be listened to and taken seriously in a medical setting. If the first doctor isn’t taking you seriously, all it takes is one who will listen to you and help you. They’re out there. We just have to find them.
If you have been invalidated about your bowel health or your symptoms, follow your intuition. As much as we want to completely trust that they have our best interests, that they went to medical school and they’re knowledgeable, that doesn’t mean that they aren’t sometimes wrong and don’t make mistakes or misdiagnoses.
Go out there and fight for yourself. Fight for your health. I hope everybody who hears my story feels very validated to go and seek help.

Inspired by Raquel's story?
Share your story, too!
More Colorectal Cancer Stories
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)
Nick S., Colorectal Cancer, Stage 4A
Symptoms: Change in bowel habits, size & consistency, blood in stool, abdominal pain, fatigue
Treatments: Surgery (sigmoid colectomy), chemotherapy (capecitabine, oxaliplatin), immunotherapy (bevacizumab, pembrolizumab)