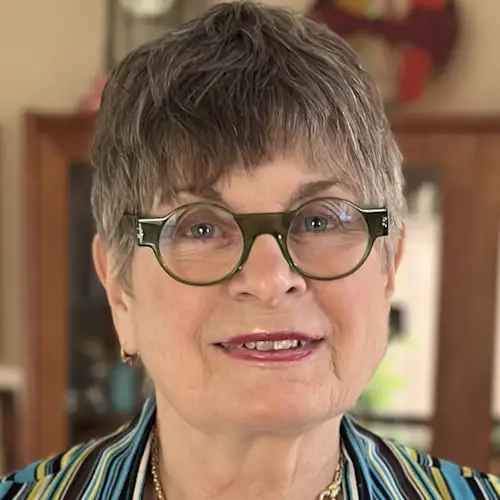
Natalia’s Myelofibrosis Story
Natalia shares her myelofibrosis story, a rare form of blood cancer that leads to scarring in bone marrow, anemia, and fatigue.
In her story, she discusses her misdiagnosis and the long road she faced before being correctly diagnosed with myelofibrosis.
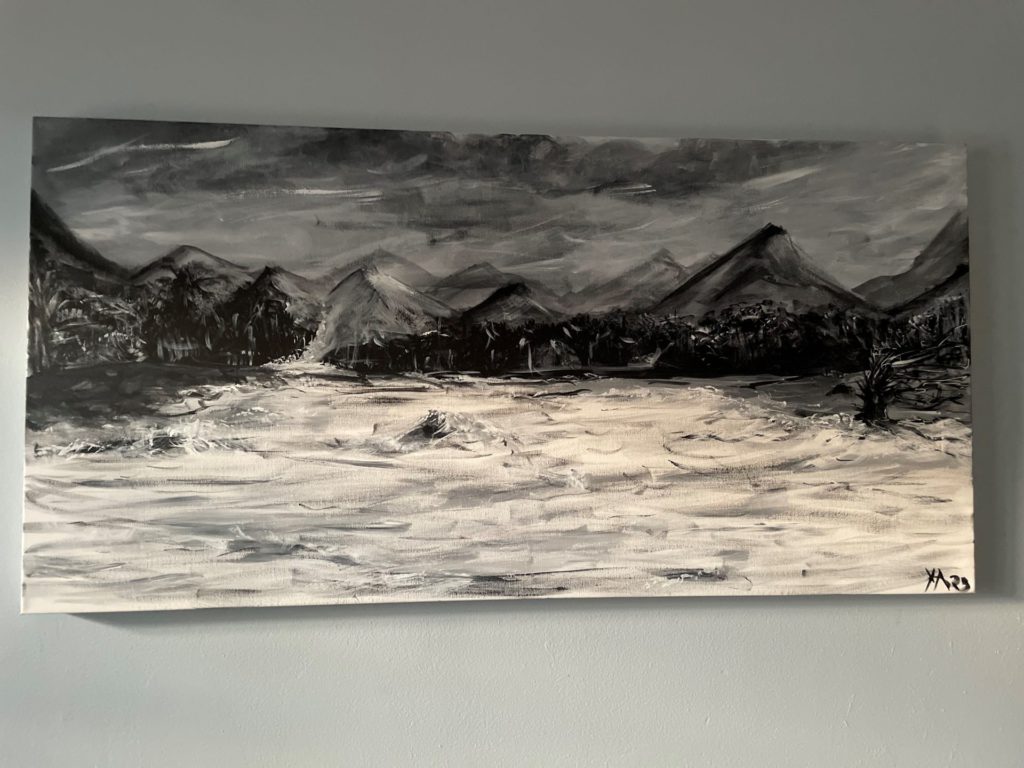
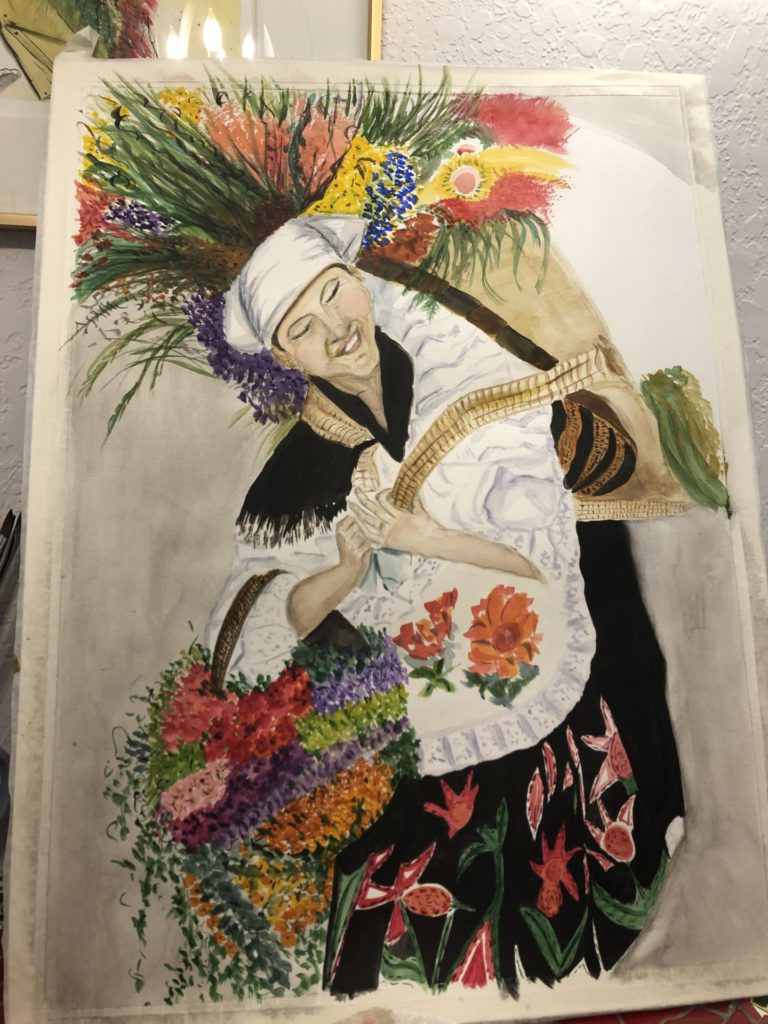
With a passion for painting, yoga, and Reiki healing, Natalia talks about how she coped with extreme fatigue and other symptoms. She explains why everyone should trust their gut and be a patient advocate, and what she’s doing to live life to the fullest.

- Name: Natalia A.
- Primary Diagnosis:
- Myelofibrosis
- Polycythemia Vera (PV) *Misdiagnosis
- Pericarditis
- Symptoms:
- Anemia
- Fatigue
- Weakness
- Shortness of breath
- Treatment:
- Phlebotomies
- Iron pills
- Blood transfusion
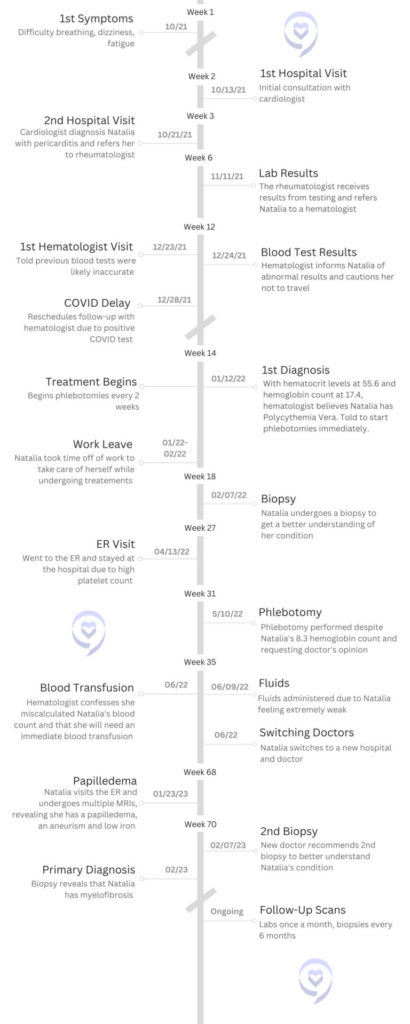
First Symptoms and Tests
Tell us about yourself
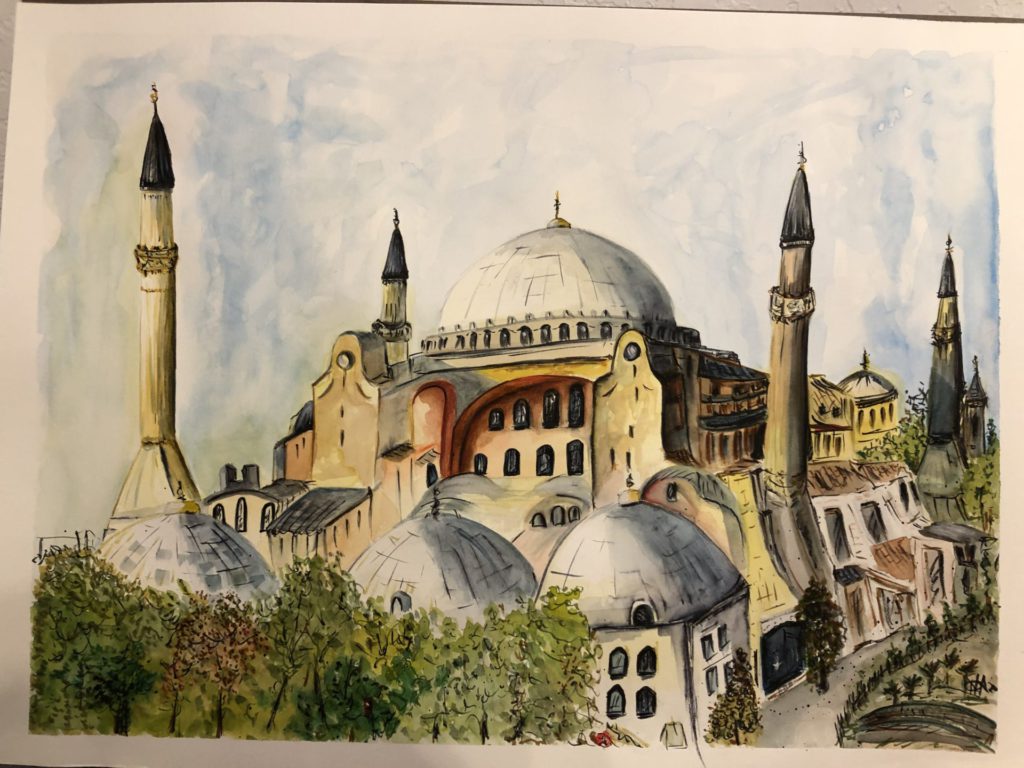
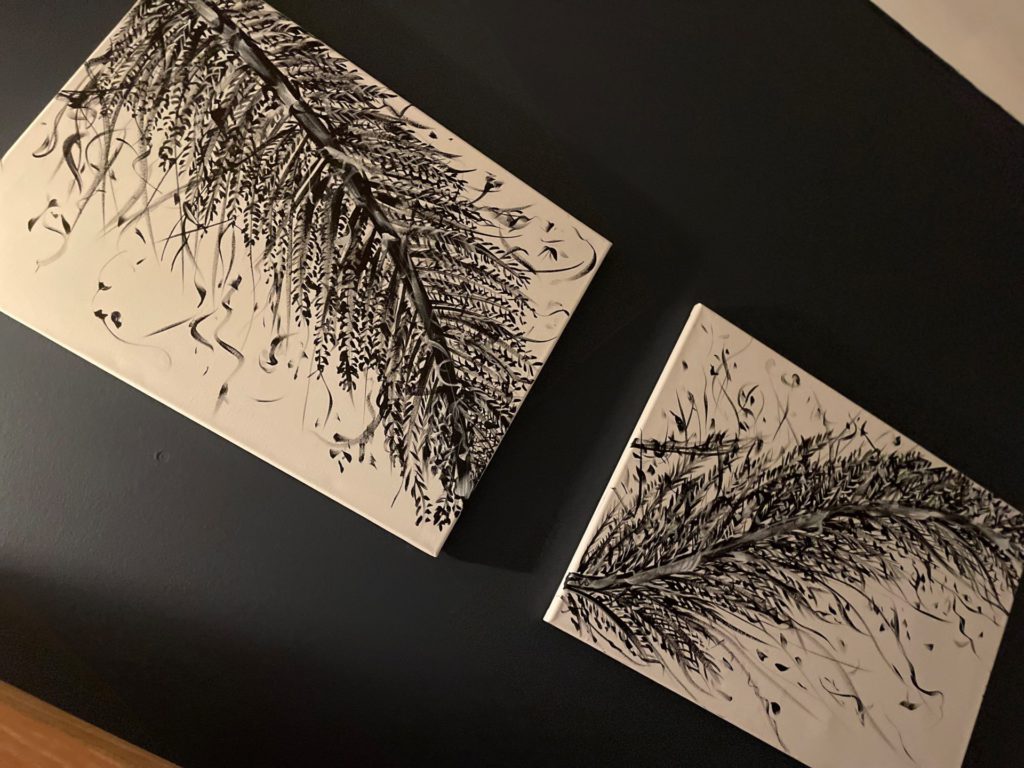
I am a mom of two adults, Gabriel and Ingrid. I’m an artist, so I paint. I’ve been painting since I was in high school – oils, watercolors, acrylics. I am also an executive. I work for an aviation company. I’m the head of administrative operations there, so it’s a big job. The painting kind of releases stress.

Aside from that, I love getting together with my family because I love to cook. My grandfather was a chef and my mom was a really good cook. She had several restaurants, so I think I’m genetically predisposed to that within my family. I love music. I’m a historian – that was my major in university.
The business side is the survival side, but I think my creativity has helped me in my executive career a lot. I’m the type of person that, whenever there’s a problem, people come to me to brainstorm. That’s helped me a lot.
What were your initial symptoms and diagnosis?
At the end of 2021, in the fall, my mother had passed away in August and I was going through a divorce. I started feeling shortness of breath. I always thought, “Maybe I’m just really stressed out.” But at one point, it got so bad that I couldn’t sleep lying down. I would have to sleep sitting up.
I knew it wasn’t an asthma attack because it was different – the pressure felt different in my lungs.
That’s when I decided to call my cardiologist, Dr. Mechanic. I called her and I said, “I’m having this problem. Can I come in?”
She did some tests, and then she told me that I was diagnosed with something called pericarditis. That was the first indication that there was something wrong.
Did you ask any questions after receiving your diagnosis?
She gave me a treatment plan for 2 weeks. I was supposed to take 25 100-mg of aspirin – some crazy stuff like that. Before I left her office, I looked at her and said, “What could cause this?” Because you don’t just randomly have something like that. That question saved me.
I’m still here because she immediately looked at me and said, “Well it could be an autoimmune disease.” So I said, “Who would I go to for that?” And she said, “Well, you could try a rheumatologist.” And that’s exactly what I did.
What if I just walked away and said, “Okay. I have this and now I have to treat it.” I think you need to go further and say, “What could cause that?”

I knew it wasn’t an asthma attack because it was different – the pressure felt different in my lungs.
It’s just very random. I mean, if they tell you it’s something genetic or caused by a medicine you’re taking or something like that. But for her, there was no other indication of that happening to me. So that kind of saved me.
I immediately thought, “I am going to go.” I made the appointment and I saw the rheumatologist and she ran about 7 different blood tests on me.
The importance of asking your doctor questions
I respect doctors very much. They have so many patients and such little time. And that’s why I believe that you need to ask the questions – to have your list.
I never go to a doctor, since then, without a list of questions because it’s easy to forget. They’re rushing and you feel like you’re imposing or you [consider] the waiting room is full of people.
That one question, “I need more information” could save your life.

I never go to a doctor, since then, without a list of questions because it’s easy to forget.
Describe your visit to the ER
I had a very funny day because I had to go in to get my results from hematology. I was living in my daughter’s apartment at the time, on the third-floor walk-up. I walked out, got very dizzy, and fell down the stairs. I had to call her to help me untangle myself.
At tje doctor’s office, and the first question they asked was, “Have you fallen? Have you been falling? Have you fainted recently?” I told the doctor that I fell down the stairs and she told me to go to the ER. I responded with, “No, I have to go to work and I have meetings.”



She was looking at me weirdly and then she told me ”Your hematocrit was something like 59 and your hemoglobin is 17 so you must not be feeling well.” She said, “I’m not a hematologist so I can’t give you any more details or tell you anything, but you need to see a hematologist immediately.”
I think her words didn’t really make any sense to me because I’ve never had to deal with hemoglobin or anything like that. She was looking at me like I was a ghost, like I wasn’t supposed to be standing. Their expression immediately felt like a cold sensation from my heart to my stomach.
I said, “Okay, I’ll make an appointment immediately.”
The hematologist suspected everything was fine
I went to a wedding in Columbia. I was with both of my kids. It was a hectic schedule. I started feeling like I couldn’t breathe, I couldn’t go up the stairs. I was thinking, “This is probably the altitude, I’m in the mountains.” Came back, and started getting very, very ill and extremely tired.

That one question, “I need more information” could save your life.
I came back [from Columbia] and I went in for my appointment. They drew blood and then the doctor came in and says, “We’ll have the results by tomorrow but I believe what I’m looking at right now is a mistake.” She was looking at the labs from the rheumatologist and she said, “I think they made a mistake. By tomorrow we’ll have our lab results and it’s probably going to be very different. I don’t think there’s anything wrong with you.”
Cancer Diagnosis
Was this the same doctor you’d made an appointment to see?
I showed up on the 23rd to see a specific doctor, and they told me, “You’re going to see a different doctor.” I said, “Well, that was not what I wanted.” And they said, “Well, that’s what we have available.”
You’re here and you feel very trapped in the sense that I had already waited for a whole month to see the specific doctor. Then you have a situation where they told you it’s urgent. Are you going to walk away? No. You’re just going to go in and see whoever so you can get some answers. But I knew I was not with the person, that I felt, had the knowledge.
How did you find the doctor you wanted?
I go on the hospital page and look at hematology. [The doctor I chose] was basically just taking care of hematology disorders, blood disorders. I had seen [the doctor I was assigned] because she was part of that group, but her expertise was gynecological hematology and I thought it was something to do with breast cancer. So she had several things, but he was a specialist on blood disorders and that’s why I picked him.
Then you go to Healthgrades, of course. You see the patient comments to make sure that people are being treated well. For me, that was the person that had great reviews and knew about what I was there to find out about.
COVID delaying information on lab results
I wasn’t worried because she said, “It’s probably a mistake.” I completely trusted her views and went home. Then the next day, which was December 24th, she called and said, “You need to come in and you need to see me next week.” I said, “Well, I have a trip on Monday. I have my ticket.” And she’s said, “You can’t travel, you can’t get on a plane.” That’s when she explained to me, “Your hemoglobin is so high that if you get on a plane right now, you could have a stroke.”
I immediately had to cancel all of my plans. My kids were devastated. My family had an Airbnb. Everything abandoned. I went in to see her on December 28th – that was her first available appointment. I arrived and the minute that I got to the floor before I left the elevator, I was escorted out by the management because she had done a COVID test on me the week prior and it had come back positive.

My daughter and I were kicked out of the premises. I had no idea. I usually keep the little tests at home. I was testing because I knew I was going into a cancer place. I told her I tested this morning and they said, “No, we did the blood test. You’re positive.” I needed to wait 2 weeks with minimal information.
“Yes, you have something very serious, but you can’t come near the hospital because you have COVID.” It was probably the worst Christmas of my life because my mother had just passed, my kids went on another trip with their dad because the whole Columbia thing was scrapped, and I was sitting there just not knowing what it was and had to wait until January 12th to see the doctor again.
What did you do following your cancer diagnosis?
The doctor said she thought I had Polycythemia Vera and the way that we can immediately attack it is by doing phlebotomies. She wanted to start doing phlebotomies every 2 weeks.
That was the first day that I ran from her office to the infusion center and had attempted to have my first phlebotomy. That didn’t work out very well. I had to leave and come back the next day.

That was the “it” day because then you go home and you start looking this up and go into a bit of a panic.
When I realized what was happening to me emotionally, I called one of my best friends, Bernice. Her mom is a pediatrician. I spoke to her and I said, “Hey, I just heard this. I’m very scared.” She called her friend, who was a hematologist in Venezuela and called me back and gave me the lifeline of words.
She told me, “You’re going to be fine. It’s controllable. I have a friend that has this.” I stopped searching and just said, “Okay, I’m going with what she’s saying.”
You have to look for the most positive energy source, and that was mine.
You have to look for the most positive energy source, and that was mine.

Were there any additional tests you had to do?
Yeah, especially genetic tests. They look for certain genetic mutations. She couldn’t give me anything definitive until I completed that.
From there on, I start having phlebotomies. I think we started every week. Because there was so much going on, I started getting weak, and very dehydrated.
I’m scheduled for a biopsy on February 7th, so she starts checking. We’re doing scans of the brain looking for any sign of strokes. She checked my entire body. We did scans of everything – MRIs, etcetera – just to make sure I wasn’t having any blood clots because that’s what the condition causes.
Getting a Biopsy and Treatment
How did your body react to phlebotomies?
On February 7th, I do my biopsy. Biopsy results usually take 2 to 3 weeks to come back. By that time and during that time – January 31st, actually – I had already called in because I was so weak from the phlebotomies that my doctor gave me a letter so I could get some short-term leave.
From the end of January to the end of February, I’m already on medical leave, trying to control this. At one point I started telling her, “Look, I don’t think I can do these things because I go home for 2 or 3 days, I’m useless. Could you give me some fluids?”
I started figuring out that the pain I was feeling was probably from being dehydrated. She changed the way we were doing it and she would ask them to do the phlebotomy and then give me 2 hours of fluids afterward.
How did you feel after receiving your biopsy results?

Then the results come in. Of course, we have a very different conversation, her and I. She tells me, “This is going to be a lifelong situation where you’re going to be taking blood out. I need you to be at a certain level where you’re kind of anemic. We need to lower your hemoglobin to at least 11 or 12.” And I said, “Okay, let’s do it.”
To me, it was like I was already there. She wasn’t going to go look for anything else because I felt overwhelmed. That’s why you should do the research before because once you’re in there and you get that diagnosis, your mindset is very different. You’re just in crisis, in shock mode.
It was tough because with it came the knowledge that because you’re making so many red blood cells, your bone marrow is overactive. Your bone marrow starts getting tired and it starts getting fibrosis, which is like scar tissue.
She tells me at one point, we might get to a level where the opposite happens and you stop making the red blood cells and we go into something like leukemia. This is terrifying news.
At the same time, she said something kind of weird. She said, “Well, of all the cancers you could get, this is the best one.” [I] didn’t agree with that, because I don’t think there’s anything that you could say to someone that would sound good at that moment.
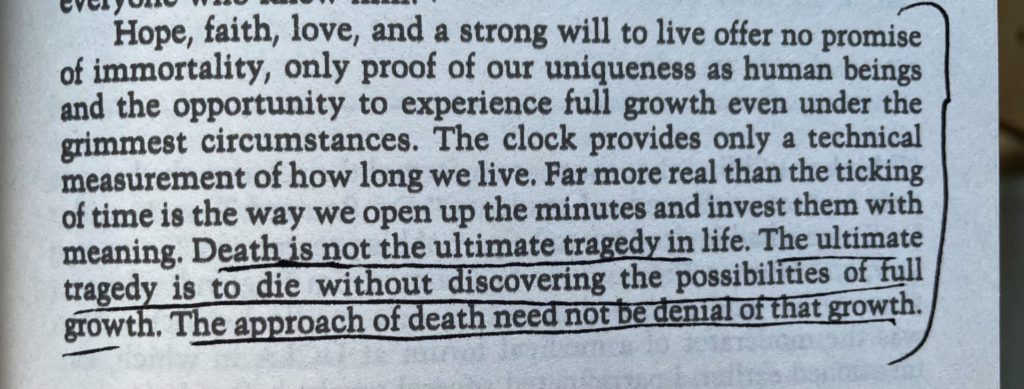
It was a knowledge that it was progressive, that there was absolutely no cure for this. I Googled, “Has anyone ever gone into remission?” and found one person in 1984. I kept it in one of my phone’s URLs. I kept it there until this year. I would look at it as if one person could get out of this, so can I.



What were some symptoms that arose with your treatments?
We start a process where they’re taking blood out. My veins are not easy to find, so that was another issue. I had one person that could find them [with] a special light.
You go home from the phlebotomies. I think it’s 500 cc’s that they take out every time you go. I had to drive myself because my entire family is working at this time. By the time I was getting home, my eyelids were getting heavy. I had to go up 3 floors and then and I could feel all my joints. It’s like a toothache in your bones.

Progressively, I started having pain in my hip, and then I couldn’t sleep at night because I started having night sweats. I had to purchase this little machine that is like a little air conditioner. Four times during the night I would have to put that on. I had the air conditioner going at home and had to put that on so I could come back to normal.
I started chewing ice. There’s a condition called pica that is caused by severe anemia, and then you get addicted to ice. I’d be chewing ice all day. Then at night, I would have to pee 7 times a night. My nights were horrible. I stopped exercising.
Quality of Life
What kept you going?
My life became very small. Then I had a conversation with my dad, and I told him, “I feel like I can’t do anything. I don’t have the strength to move around, to do the things that I normally do.” He said, “You have to move.” That voice stayed with me. Where I live, there was nowhere to walk around. He said, “Even if you go to the parking lot and you go 2, 3 times around the parking lot, you have to move.”
It’s true because it’s all about your circulation and the blood clot situation. You need to move and [my doctor] had told me that. But until I heard it from my dad, I was feeling like a victim.
I’m just taking in hits and I wasn’t coming out and doing anything about it. That gave me my first fighting punch. I was like, “Okay, let me move” and I started moving.
I would wake up every morning and I would do yoga in my room because I didn’t want to move around too much. I would do meditation, I would do yoga, then I would drive to this little park that I knew about. I would go around a few times. I would go to this organic store every day and buy the ingredients for the meal that I was going to have because that forced me to do something outside of the house.
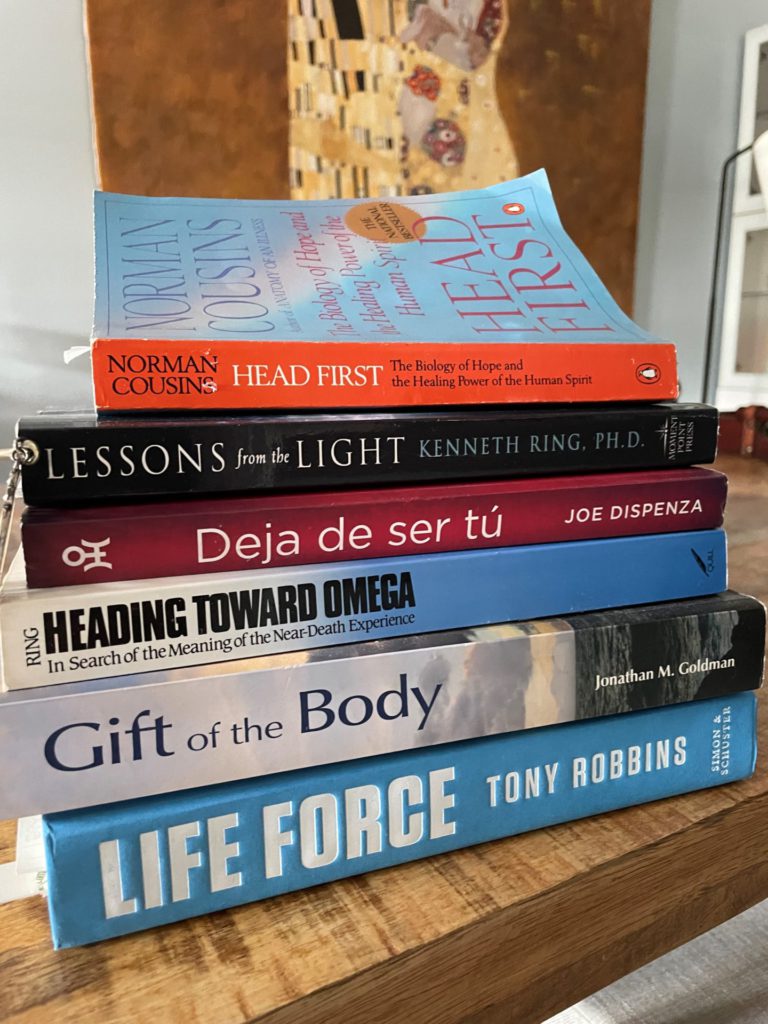
I did TikTok videos about my recipes and kept looking for things to keep me going. I started reading a lot about spiritual healing meditation and called one of my really good friends, Marianne, and asked her, “Hey, do you know someone that does Reiki healing?” And she’s like, “I’m a Reiki healer. I went to the best school.” I had no idea!
She goes, “Start coming.” I would go and see her once a week and that just changed the entire process for me.

No signs of improvement with treatment
I started feeling that we were just taking blood out over and over. I thought at one point I was going to feel better and kept asking her, “I have to go back to work. Am I going to feel better?” And she kept saying, “You need to adjust your lifestyle to the condition.” And I said, “But there has to be something.”
She suggested hydroxyurea and she said that my insurance had approved it if I wanted to go on it. I said, “No, I don’t. I don’t want to take that. I don’t feel that’s going to add to anything. I’ve studied it, I’ve seen the side effects and I don’t think that I’m at the level where I would be able to handle that. I want to feel better before I go to the next step like that.”
She was struggling with me. I could tell that she kept looking at my results and scratching her head, “What’s going on?” Because one day it was the platelets and then it was the white blood cells. And then she was getting a handle on it.
I went to do my phlebotomy on May 10 and the nurse told me, “You are a hemoglobin level of 8.” Anyone who was a nurse or a doctor knows you can’t take more blood from that person. I know that now, I didn’t know that then. She asked me, “Do you think we should take the blood out?” I looked at her and said, “I’m not a doctor. You need to talk to my doctor.” At that point, I didn’t know if she was dealing with platelets or red blood cells. She said, “Okay, we’ll talk to your doctor.”



I came back on May 19th for another phlebotomy. The answer, when asked “Did you talk to the doctor?” was “It’s still in the treatment plan.” They took blood out that day and then they took out blood again on June 7th. That’s 2 times after my hemoglobin level 8.
I came back on the 9th because the gentleman that was doing my phlebotomy that day refused to do the IV on me. He said, “I don’t have the right package, I’m not going to do it.” He took my blood out in 11 minutes. It would normally take 30 minutes. He just destroyed me after that, I was so sick.
My daughter started calling the doctor at night. She told me she was going to call 911. I’m like, no, because I was afraid of going to a hospital. This is a very rare disease and I knew no one would know what to do with me. So on the 9th, I came back. They gave me the fluids.
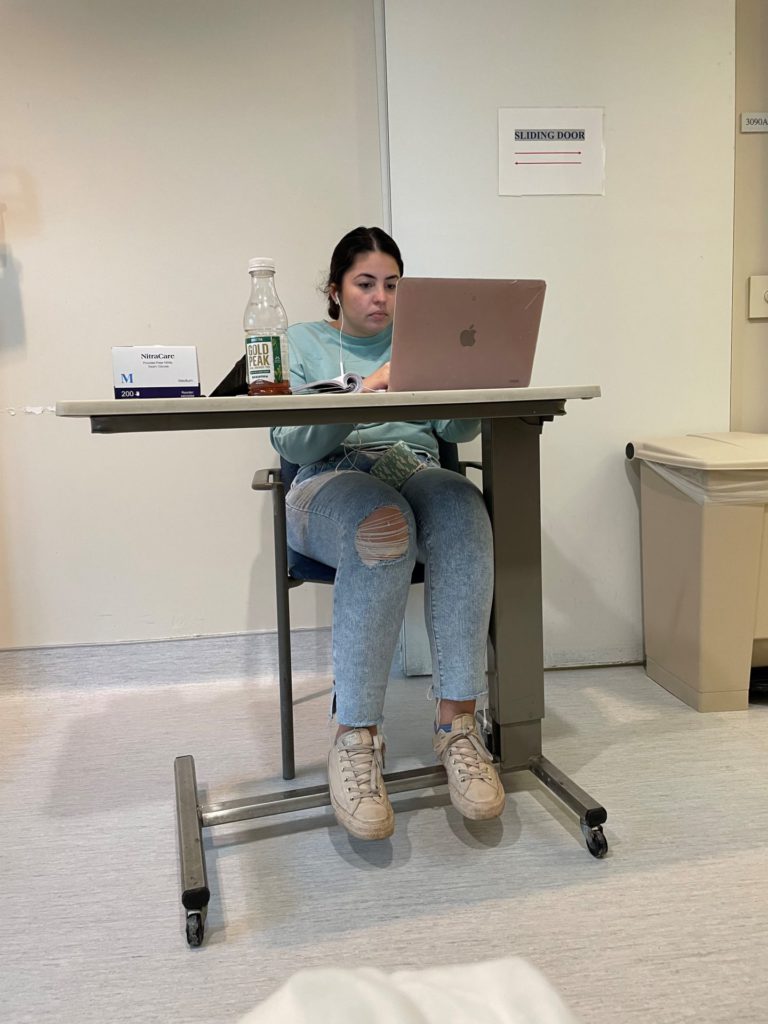
Describe working while still battling cancer
By that time, I’m still going to work. I would get to the office. I would call my security guard. Jason would come down and I told him the first day, I said, “I’m so sorry because I know this is not your job scope or anything, but I need a human favor. I can’t carry my laptop anymore.” So he would wait for me.
I would give him the laptop bag and all the stuff that we carry for work. I would go park, then I would walk and he would wait for me. He was a gentle giant. He would wait for me and walk me to my office. Then it would take me about 15 minutes to recover from walking up.
I would have this huge thing of ice that I had to eat. The ice had some sort of chemical reaction in the brain that gives you a little bit of oxygen, so it would make me feel better.
I couldn’t have rice and potatoes for lunch. I would have a carrot and a cucumber because if I had a normal lunch, I would fall asleep on my desk. That’s when I realized, this can’t be it. Like, how is this happening?
Incorrect Treatment Advice
The doctor had made an error
I went to my sister’s house on the weekend of Father’s Day. Saturday, I couldn’t talk. I sat there and I couldn’t talk. I couldn’t move around.
The next morning, which was Father’s Day, I drove myself to the ER and they told me, “Your hemoglobin is at 6. We need to do a blood transfusion immediately.” And I said no, because my doctor had already told me, you can’t get a blood transfusion because the red blood cells are going to just explode. So I refused it.
Then I waited maybe 2 more days to see her because she was coming back from vacation.
When she finally saw my labs, she said to me, “I am so sorry. I miscalculated your numbers and you will need a blood transfusion now.” I was furious.
I would fall asleep on my desk. That’s when I realized, this can’t be it. Like, how is this happening?
She said, “Once you get the blood transfusion, you’re going to start making blood like crazy and we’re going to be back to the level that you were in January.” Imagine going through this every 2 weeks – phlebotomies and all the pain. How am I going to go back to that? That didn’t make sense to me.
She said, “We need to go right now. We need to put you in the ER.” I said, “No, I need some time. This is a serious situation. A blood transfusion is something very serious. I need to talk to my family. I need to go home and I need to think about this.”
What was your doctor’s reaction to your refusing a transfusion?
She was not very happy with me saying no because I think she realized the responsibility of me just going home the way that I was. But I went home and I called Bernice’s mom again. She called her friend, the hematologist and we waited until the next day because he’s in Venezuela. And he said, “She’s wrong. You’re not going to start making red blood cells like crazy. Your hemoglobin with the blood transfusion is only going to go up 2 points and that’s it. [For] the rest, you would need iron.” That’s another story.
So that’s when I called her back, on a Thursday. I spoke to her and I said, “I’m going to go through with the blood transfusion.” She said, “I’m going to have my office call you and schedule it immediately.” They never call me back, to this day, not even to find out if I’m still alive.
Did you still get a blood transfusion?
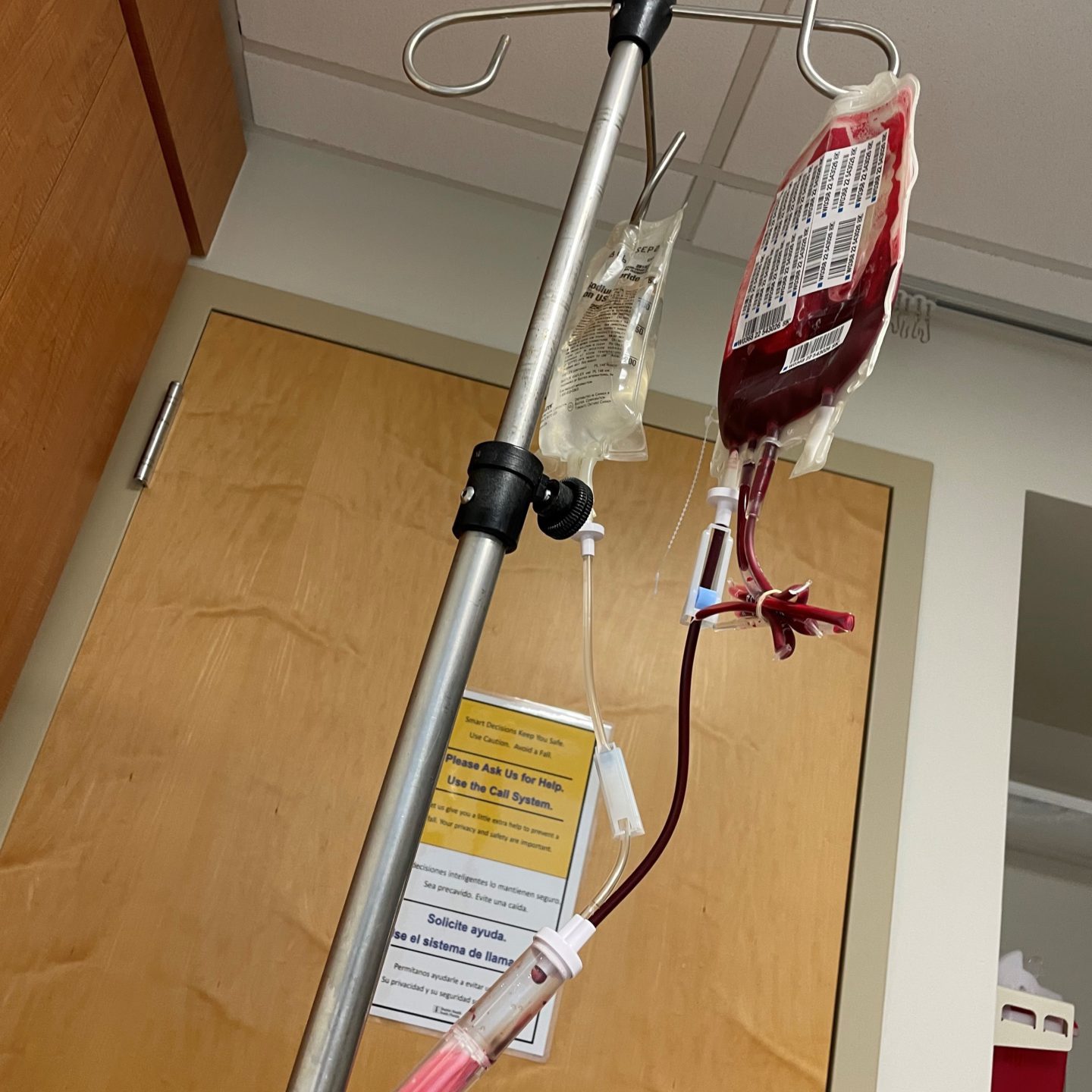
I waited until Saturday because my friend Lizzie works at the hospital. She told me, “You need to go into the hospital on a Saturday around 7 to 9 a.m. There won’t be anyone if you’re going through the emergency room.”
I started researching who had the best hematology group for my condition. I found South Miami Hospital. I found Dr. Kim, who was in charge of blood disorders. I went to her hospital but went through the emergency and then I was assigned to her.
From there, I got my blood transfusion. I think it was June 24th. My hemoglobin went from 6 to 8 within a few days. Then I was with the new hospital, a new doctor, and went from there.
How did your first doctor explain their miscalculation?
I said, “Well, how do you mean? Your team has been telling me that [my hemoglobin was level] 8 and I shouldn’t be taking blood out. Did they reach out to you?” And she said, “Yeah, but I thought that because you have Polycythemia Vera, you would make so much more blood, so I wasn’t concerned with that. I figured we were following the right pace, so you were making blood at the same speed that was taking out. I don’t think it should have been a problem.” That was the explanation I got.
Switching Hospitals and Doctors
Beginning treatments for anemia
I was with Dr. Kim from June until last month. In February, she started giving me iron pills because now we’re trying to get me out of very aggressive anemia where I have zero iron deposits.
She starts giving me the pills, she tells me there’s no more phlebotomies for a long time, you can now fly because you have blood! [She] started treating it in a very positive way, but I was still very weak. Without the phlebotomies, I start feeling a little bit stronger. I go back to work. I realized that I couldn’t do a lot of physical activity, but I tried to walk a little, maybe like 20 minutes a day just to help me out.
Everything was going fine but we kept doing labs and my hemoglobin numbers were not moving and my iron. I think all of last year, we were able to get it up to 9. That’s it. We’ll be stuck at 9 or even a little lower or go up to 9.5, but never more than 10. It was like 9-point-something always.
When I left on vacation in December, she told me “When you return, we might have to give you iron infusions because I’m not getting anywhere with the pills.”
Developing a papilledema
I come back from vacation, I start working. January 21st, I’m sitting here with my family having dinner, and I start seeing something very strange in my eye. The next morning, I wake up and I see I have a floater, a dark spot. I got very tired. My limbs felt tired. I stayed in bed all Sunday. Monday I call my ophthalmologist. They gave me an appointment for that morning.
At the time, one of my cousins sent a video in our chat about what it feels like to have a stroke, and in the video, there’s a picture of a person seeing what I was seeing. I panicked.
Dr. Kim and her team would answer phone, email, everything within 2 minutes. I tell her what’s going on. She said, “Don’t go to the ophthalmologist, go to the ER.” I went to the ER and she was already there, she came in immediately. I had MRIs done on my brain. I had something called papilledema, which is an edema of the brain, which affected the eye.
Getting a second biopsy and diagnosis
What happened (it’s probably because of all the anemia) they checked my numbers and my platelets were very high. They were 740. That’s when she realized, “This isn’t right. Her numbers are not responding and I need to do something.”
She told me “I’m going to have to do another biopsy,” which I was terrified of. She goes, “It just doesn’t make sense to me. I’ve been giving you iron for months and nothing changes, and now I see your platelets are up. This doesn’t make sense.”
February 7th, I go through another biopsy and she calls me 2 weeks later and says, “You have primary myelofibrosis, not Polycythemia Vera. It makes sense because in myelofibrosis sometimes you’re making a lot of red blood cells, and sometimes you’re making zero. Sometimes the problem is the platelets or the white blood cells.”
I had MRIs done on my brain. I had something called papilledema, which is an edema of the brain, which affected the eye.
Not having access to medical records from the previous doctor
Whatever she was reading, because she had the other doctor’s diagnosis and notes, was not what is happening.
The only thing that she’s able to see from my former hospital is what I have in my chart. She’s never able to get my official medical records, even though I sent 2 letters to the hospital and I called the hospital and spoke to, I don’t know how many people. So they never got my records.
They don’t answer anything. [I] kept sending the letters, because at one point, I called and they said, “Send a letter.” I did that during the fall of last year, but nothing happened.
[My doctor] said, “I don’t have anything to compare, but the notes that are on there. I need to see the actual pathology exam that was done.” She was under the assumption that whatever [my previous] doctor had put on her notes was what was happening.
How did you react to being diagnosed with myelofibrosis?
That was a very difficult week, a very dark week. I was so happy to know that there was a path. Now things made sense to me.
I was told immediately that I wasn’t going to stay with Dr. Kim anymore because she’s a benign hematologist. I needed to go to another hospital and go to malignancies. That was difficult because I was already very attached to Maria and Dr. Kim because they were awesome.

I was traumatized. I thought, “I don’t want another doctor. I’m good here.” You met someone you could trust, now I have to find someone.
But they were so sweet. They said, “We’re going to be with you until everything’s done.” The first thing they did is an iron infusion immediately, so I got an iron infusion. They gave me the options that are available in this situation.
They have an amazing new medicine. I believe it’s Jakafi. They also said, “Miami has an excellent cancer center in Baptiste’s, a brand-new building and it is just truly amazing what they’re doing there.” They told me “You have the option of getting a bone marrow transplant. They have a team there that does it.” That’s also another point that you feel great. “We’re going to refer you to this new doctor at this location.”
Changes in Lifestyle and Outlook
Finding hope by reading about patient’s experiences with myelofibrosis
Of course, the next morning, and the next 3 days are terrible because I, again, am looking at everything possible about myelofibrosis. It is terrifying until I found [The Patient Story].
I found Mary’s story. I had spent 3 days where I couldn’t move. I would cry 7 times a day. I live by myself, so it’s not a good environment for someone that’s going through this because I’m not hungry because of the anemia. I wasn’t sleeping well. I was just in a very dark place.
I see her story and the first thing she says about fatigue (I was feeling really tired), if you’re fatigued, you need to move. Don’t go take a nap – move.
»MORE: Mary’s Myelofibrosis Story
I see her story and the first thing she says about fatigue (I was feeling really tired), if you’re fatigued, you need to move. Don’t go take a nap – move.
I immediately started thinking, “Yes, I’ve been at home for months with all the stuff that was going in my brain and taking this medicine that they had put me on, then they gave me this very difficult news.” I’m just going into that little world from last year. I immediately thought, “I need to call someone.” I knew that one person that would have the time to wake me up every morning and get me out of the house.
Getting back into an exercise routine
I called a [family friend] and said, “Hey, can you be here every day next week at 9 a.m. and get me out of the house?” I love biking outdoors. Walking is very difficult because it’s hot here in Miami. The heat is not good. But when you’re biking, you’re getting air and it’s just easier for me. He agreed, and for an entire week last week, he would come in and we would walk.
I mean, [at] first, we walked, but it didn’t work out. So I’m like, “No, biking” and we would bike [for] 12 minutes. I would have to sit down and catch my breath for the return. And then he would help me prep food. We went [with the] Mediterranean diet because the new hospital sent me a Zoom meeting where they told us food is medicine. That week, I was able to bike 4 times.
What’s your outlook on living with myelofibrosis?
You’re here to get your children through difficult situations. You’re not here just to live and breathe. You’re here to affect other people.
I decided my spiritual beliefs are, you have to fight for every inch of life that you can get. Even if it is less than normal and if it is painful sometimes.
Most of the time you are here to inspire, you are here to love. You’re here to get your children through difficult situations. You’re not here just to live and breathe. You’re here to affect other people. All of us affect each other. I mean, [The Patient Story] affected my life in such a positive way. This is what we do. So I said, “Whatever it is I need to do, I’m going to do it.” I stopped reading all the horrible stories that you find on Google.
[I] got my appointment with the specialist. I saw her on Monday. This week, I’m going to see the transplant specialist on the 8th. [I] got amazing news because they have a resident in that hospital that was able to obliterate or get rid of the graft versus host disease, which is one of the biggest problems after a transplant. I have my sister and my 2 kids as possible donors. I’ve had a crazy amount of people being brave enough to even say “I will do it.” I was like, “Wow, that’s amazing.”
Did biking improve your quality of life?

[Biking] makes a complete difference because your circulation is hindered by how thick your blood is with this condition. Once you start moving, you realize when you come back from it, you have 3 or 4 hours of high energy which you don’t have if you sit around. You don’t get the tingling in your hands or your feet.
Psychologically, you’re out, you’re getting some fresh sunlight. I think the worst thing you can do is lie down and close your shades because you just really need that vitamin D.
We human beings need everything around us that’s been created for us. Water, sunlight, other people. That’s the best medicine.
The biggest thing that helps is exercise because it helps with joint pain.
What are some other things that improved your quality of life?
Once I got the infusions, I stopped eating ice. I’m excited. That helps me sleep through the night a lot better.
If you’re having hot flashes, which you will have with these conditions, they sell these covers for your mattress that are cold and a pillow. The items that I bought helped me so much. You just put it on here. They sell them on Amazon for maybe 20 bucks. If you wake up in the middle of the night, you turn it on and you’re able to cool down enough to go to sleep.
In case you’re in a situation like I was where the anemia was so terrible and you need to work, having that lunch that I would have, carrots and cucumbers, would get me through the day so that I could come home, have a regular meal and be able to digest it and get sleepy on my couch, not at work.
I think the ice did help a lot during that time because it helped me breathe better.
Reflections
Have you spoken to your first doctor again?
No, I’m writing her a letter. A lot of people have told me, “Why don’t you do something about it?” I don’t want to do anything with litigation or anything like that, because I need positive energy in my life right now.
Trusting your gut
I believe you have to look at how things make you feel. It is difficult to say to a doctor, “You don’t make me feel right.” It’s not a fact, it’s just feelings. But feelings are very important, especially when you’re going through this.
When people are paying attention to you, pay attention. If they’re making eye contact, pay attention. If they’re looking at their watch and they’re in a hurry, you can fire your doctors. I learned this and it is the best thing to learn.
If you go to someone and they make you feel inaccurate, they discard your symptoms as not important…
I had gone to a cardiologist, different from Dr. Mechanic that year, and he had told me there was nothing wrong with me. When people are paying attention to you, pay attention. If they’re making eye contact, pay attention. If they’re looking at their watch and they’re in a hurry, you can fire your doctors. I learned this and it is the best thing to learn.
When she told me, for example, about the drug, I felt in my heart that I would rather go through the symptoms that I was having than take that medicine. I went and I studied it and I went into the blogs and I saw what people were going through and I said, “No, I don’t want this.” I, told her, “If you see that I’m close to dying, then I have to take it. I will. But at this point, do you feel that I’m at that stage?” She said, “Well, it would be great.”
Remember, they’re advocating for medicine. I’m not saying that’s [always] the case, but sometimes they are because they’re selling something they’re trying out too. Sometimes we’re guinea pigs. They’re trying stuff on you.
If it makes you feel weird, it doesn’t feel right, walk away. Say no, respectfully. I told her, “I’m sorry. I know you got it approved, but I’m not interested in that right now. I need time to process this, and I don’t feel like I want those side effects.” I think it’s kind of like chemotherapy medicine, so it’s a serious medicine that you can’t just be offering to people. Do your homework, read.

Also, if you are told to take something and it has to be that way, don’t believe the worst-case scenarios. We’re all different, we all react to things differently. Just focus on how you feel.
How does that energy of that person make you feel, in the case of a doctor, when they offer you things? She told me, “Let’s go for the blood transfusion right now.” I said, “No, I need time” and give yourself that time because there will come a time when you say, “I’m ready.”
Whatever it is, don’t let anyone rush you into anything. It’s your body, it’s your life.
I would have been on that medicine for a year and I would have been on the wrong medicine because right now they’re like, “No, we’re not going to give you that.” So imagine.
We’re all made of energy, so it’s the most important thing [to] be around people who present that energy. There are people that are going to come and look at you and you’re going to tell them what you’re going through. But because you look fine and you have hair, you don’t look like you’re very ill, they’re going to just tell you, “So and so has this disease and they’re fine.” Do not listen to that. You are a unique human being and only you know how you feel.

Communicating your needs to people
The other thing is work. We’re indispensable and we have to be there. That was my first struggle – I need to go back to work. I need to go back to work even though we have remote work. That’s helped me so much – my company gives us 2 days of remote work a week.
I’ve been able to keep my job because of that opportunity. Talk to the people around you, talk to your boss, talk to your assistants, talk to your co-workers. You don’t have to give them details, you just need to let them know.
I told my boss, “Hey, there’s certain things that I’m not very good at right now” like events. I was the life of the party. Now I’m not. [I’m] kind of sitting in a corner, but I told him that. He’s an amazing boss. He’s just so understanding. He’s like, “Okay,” because he didn’t know that. So you let them know.
Also, you can’t expect people to assume and know. You need to let people know if you’re not feeling well, because people are worried about their life.
Many times, I would not tell my boss or people in my family how I was feeling and I kept treading on. Then you get to a point where you get upset, and it’s not their fault. They’re fine, they’re not in your shoes. You’re the one that needs to communicate, “Hey, today I’m not going to be able to go to that party because I can’t stay up after 9 p.m.”
My lifestyle has changed completely. You can’t drink alcohol. I can’t do certain activities in the sun, for example, I can’t take sunlight. I changed a little bit of my lifestyle, but I let people know. I let them know I’m a little different now. I’m still me, but we’re going to have to do things a little different.
What’s your top advice to others?
I got so much support after I started speaking up. If you stay silent, it’s not going to help you. At the beginning, I was like, I’m not going to bother. Then you’re the one that is going home hurt and sad, and they’re not to blame. They don’t know what you’re feeling. So speak up. Let people know. Find a buddy if you need to. My husband’s my buddy. I call him, “Carlos, I know you’re a health nut, so you need to help me now.”
In this case, for example, you ask for help and sometimes you’re going to get help that is not what you thought you needed or the person. Take what they’re giving you. My friend gave me this mug, it says “Mindset Is Everything.” I read a book called “The Biology Of Belief.”
They focus on the placebo effect and the fact that 30% of people just heal without taking medicine. Focus on that. I mean, how amazing is it that just by believing that you’re taking something your own body will heal?

Special thanks again to AbbVie for its support of our independent patient education content. The Patient Story retains full editorial control.
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant