Courtney’s Stage 3A Colorectal Cancer Story
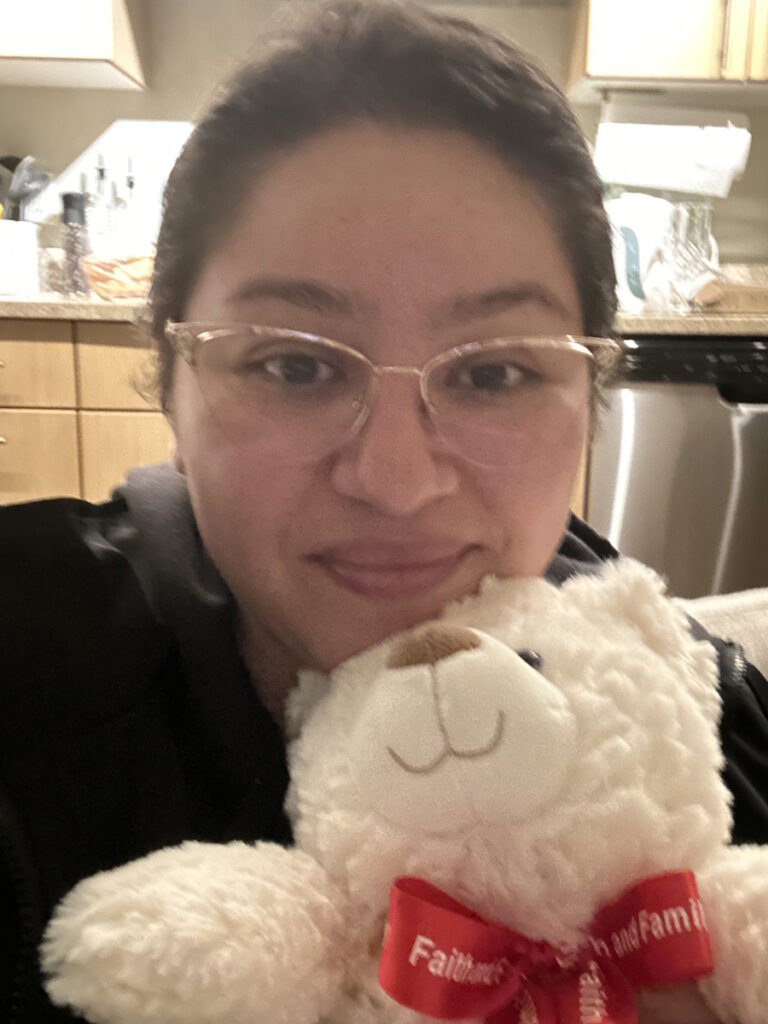
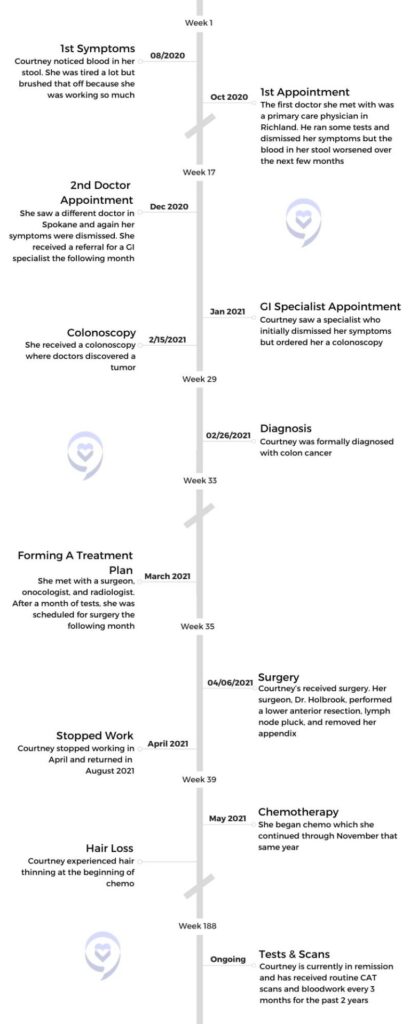
Courtney, a high school English teacher from Spokane, experienced symptoms such as fatigue and blood in her stool that led her to suspect she had colon cancer. Despite initial dismissals from multiple doctors due to her age and lack of family history, Courtney persisted in advocating for herself, ultimately undergoing a series of tests, including colonoscopies and scans, which confirmed her suspicions. Diagnosed with stage 3A colorectal cancer, Courtney underwent surgery to remove the tumor and lymph nodes, followed by chemotherapy as a precautionary measure.
Throughout her treatment journey, Courtney faced various challenges, including side effects from chemotherapy such as hand-foot-and-mouth sores and neuropathy. Despite these obstacles, she pushed forward, continuing to teach full-time and engaging in physical therapy to regain her strength. Three years into remission, Courtney emphasizes the importance of self-advocacy, listening to one’s body, and pushing for answers, especially when faced with medical dismissals or ambiguity. She encourages others to trust their instincts, seek support from loved ones, and persevere in navigating the healthcare system to ensure proper diagnosis and treatment.

- Name: Courtney H.
- Diagnosis (DX):
- Colon Cancer
- Staging:
- 3A
- Symptoms:
- Blood in stool
- Fatigue
- Treatments:
- Surgery
- Chemotherapy
- Capecitabine
- Oxaliplatin
Advocate for yourself, know your body, listen to your body, and keep pushing until you find answers.
Courtney H.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself
My name is Courtney. I am a teacher. I teach high school English – specifically honors 9 English and mythology. I am a big lover of reading. I like to play outdoor volleyball, garden, and explore. I live in Spokane, in the Pacific Northwest. It’s so beautiful. We have four seasons and lots of activities and different things to do. I like to spend time with my niece and nephew.

What were your first symptoms?
I took an anatomy and physiology class in college, and one of the only things I remember from that was that the professor said, “Most often when you have internal bleeding of some sort, it is your body’s inability to heal itself, and that usually comes in the form of a tumor.”
What had happened was I had gotten a teaching job in Othello, where I grew up, and I moved down there. This was August of 2020. I was a very busy new teacher. I was the head cheer coach for a cheer program. I worked a lot of jobs in grad school, and so I just was very used to being on the go all the time and having a busy and packed schedule.
I knew I was sick. I knew I had colon cancer, so I just kept pushing.
When I moved to Othello, I started showing one symptom – I had blood in my stool, and I instantly knew. I knew instantly that I had colon cancer. Moving down to Othello, I had to get all of my records and everything transferred down there, including all my medical stuff. So I wasn’t able to go in and see a doctor until October. My symptoms kept progressing, and I just knew when that started happening. I was trying to find somebody that could help me find the exact diagnosis. The answer.
Did you have any additional symptoms?
Just blood in the stool and fatigue. My friend’s mom, who’s a nurse, did a blood test on me and she said I was very anemic. What we ended up finding out when they had taken the tumor out is the blood flow was feeding the tumor, and that’s why I was so anemic.

Colonoscopy
Experiencing medical gaslighting
The first general practitioner doctor I went to, he dismissed all my symptoms and said, “There’s nothing wrong with you. You’re thin, you don’t have a family history. You just need to make some dietary changes.” I was like, “Well, I’m going to keep trying to find answers.” It was in the middle of COVID, so everything was pushed back. Then symptoms kept getting worse. When I came home for Christmas break – home was Spokane – I saw a different doctor and it was the same thing. He spent about an hour with me, ran some tests, dismissed all my symptoms, but I knew I was sick. I knew I had colon cancer, so I just kept pushing.
The first doctor in Richland, he actually had put in a referral for me to see a GI specialist. I was able to see a GI in January of 2021 and [experienced] the same thing. She dismissed all my symptoms. Finally I said, “Listen, this isn’t about you being right or me being right. This is about figuring out what’s wrong. You’re speculating and I’m speculating.” They were all saying, “We think you have Crohn’s or diverticulitis, diverticulosis, or a bleeding hemorrhoid.”

One of the greatest skills that my parents ever taught me was the ability to advocate for myself and to know your body.
I said, “No, I think that I’m sick. What can we do?” She said, “Well, we can give you a colonoscopy. You’re too young and they’re very expensive.” I said, “Well, I’m a teacher. I have great health insurance. We need to do this. I think it’ll give me peace of mind knowing that we have tried everything.”
Receiving a colonoscopy
Months later, she did a colonoscopy and found the tumor. That was February of 2021. That whole month and a half that I went through 9 different tests. I did 3 colonoscopies, a sigmoidoscopy, 2 CAT scans, a PET scan, and an MRI. There’s another one I did but I can’t remember the name of it. All of those tests brought me to the diagnosis. Now what are we going to do? What’s the plan of action going to be? I got a team together.
What tests did the first doctors do?
He did a blood test and some general stuff. He felt my stomach to see if I had any lumps or bumps. Then he went through and looked at family history. Obviously, I don’t have a family history of it. He said, “You’re thin, you’re not pre-diabetic.” I was in Richland, Spokane, and then I went to Kennewick. So three different cities, three different doctors. The doctor in Spokane pretty much did the same thing. They didn’t do anything extensive because you can’t really diagnose it unless you actually get a colonoscopy.
The problem was, neither one of those two doctors could perform that. Then they just dismissed my symptoms. They said, “Well, we’re not going to put in a referral for you to have a colonoscopy because we don’t think, from our experience, that you have it. I really had to beg the GI specialist to give me one.
We did a blood test with the first doctor and he didn’t see anything abnormal. Then the doctor in Spokane didn’t really see anything abnormal. But my friend’s mom, who’s a nurse, knew what to look out for because I told her what was going on. She did her own test and said, “You are severely anemic. Something’s going on.”
Did your insurance cover the cost of the colonoscopy?
I paid a little bit out of pocket, but it was mostly covered. The problem was, and this is something that I think a lot of people run into when they’re getting tests done, especially a colonoscopy or sigmoidoscopy. My insurance company did not want to pay for the right type of drugs. I didn’t know that. I didn’t hear the confirmation. They actually had to tell my parents, and it took 8 hours for the drugs that they gave me to wear off. So I actually didn’t find out about the tumor until the next day. My parents waited to call because they tried to talk to me after the procedure and I was just bonkers.
Surgery
The importance of advocating for yourself
They dismissed the symptoms because I didn’t fit the profile, but one of the greatest skills that my parents ever taught me was the ability to advocate for myself and to know your body. I just knew I was sick. I had that feeling in my stomach. Sometimes science can only go so far, and sometimes you have to put it in your own hands and keep pushing for it. It was a unique set of circumstances, because when I did my colonoscopy, COVID cases were very light, so I was able to go in and get a colonoscopy. When I had my surgery, COVID cases were really light, so they didn’t push my surgery back. These were just perfect little windows where things ended up really working out in my favor.
Formulating a treatment plan
Because I didn’t have the right drugs, she couldn’t finish the colonoscopy. I would have to come back 4 days later and do another one. I came back that Friday. I had [the first one] done on a Monday, came back that Friday, and everything else looked clear. She said, “I’m 98% sure that this is a cancerous tumor. We’re going to send it off to have it biopsied.”
It took two weeks to get back. The next conversation, I said, “I know a surgeon who saved my dad’s best friend’s life. He had stage 4 rectal cancer and he’s been in remission for 20 years. I want that guy.” She was going to put in a referral for somebody else. I said, “No, I want this guy.” Then everything started to move, all the tests.
After all of the tests came back – because the original plan was to do some radiation, 6 weeks of chemo, and then do surgery after the MRI, – the radiologist called me and said, “This is miraculous, but your tumor is a lot smaller than we thought, so we’re going to operate. Nothing else is lining up in your body, so we’re just going to go for it and operate.” So they did.

Describe your surgery
Dr. Holbrook went in and did a lower anterior resection and took out part of my colon, 21 lymph nodes, and my appendix. He said, “I had a stage 4 appendectomy patient who’s 17 years old last week. I just thought I’d take your appendix out.” He spent about 4 hours in surgery. He just retired last year, but he’s one of the best in Spokane. I trusted him.
»MORE: Cancer Surgery Treatments
Did you have to prepare for your surgery?
The prep work was I had to go onto a liquid diet about 48 hours before. They gave me some things that they wanted me to take prior. After I was in the hospital for about 4 days, I had a series of things that I had to go through to get out of there. I had round the clock bloodwork. They would come in at 2 a.m., they’d come in at 6 a.m.. They were checking fluids and different things like that.
As far as the procedure, he just went in. He didn’t tell me how much of my colon he took out, but he took out the sigmoid region of the colon. That’s the end. He took that part out and did the lymph node pluck. After that, I was on a liquid diet for about 3 weeks, giving my bowels a break and allowing things to heal. He was able to go in and do it minimally. The incision where he went in was about this big. He was able to go in right underneath my stomach and do it.
Chemotherapy
What stage were you in?
We got a really good prognosis back. I had a stage one tumor. There were just a few little cancer cells that had broken off and gone into one lymph node, so I had a really good prognosis.
Preserving fertility before starting chemo
I had my 3 week clearance from surgery, and then I actually harvested my eggs, and then I did chemo. It was boom, boom, boom. My body had been through some things. Harvesting your eggs is quite an interesting process. I didn’t know this. When you go through and you do all the things, they monitor you, they take your temperature, they do all the things.
The day before my procedure, they did a COVID test on me and it came back positive. I didn’t know I was asymptomatic. Seattle Reproductive had to fight with Seattle to advocate to harvest my eggs because it’s a $15,000 procedure. They ended up saying, we’re going to suck it up, risk it, and do her procedure. Then I started chemo right after I was cleared from COVID.
»MORE: Fertility After Cancer Diagnosis
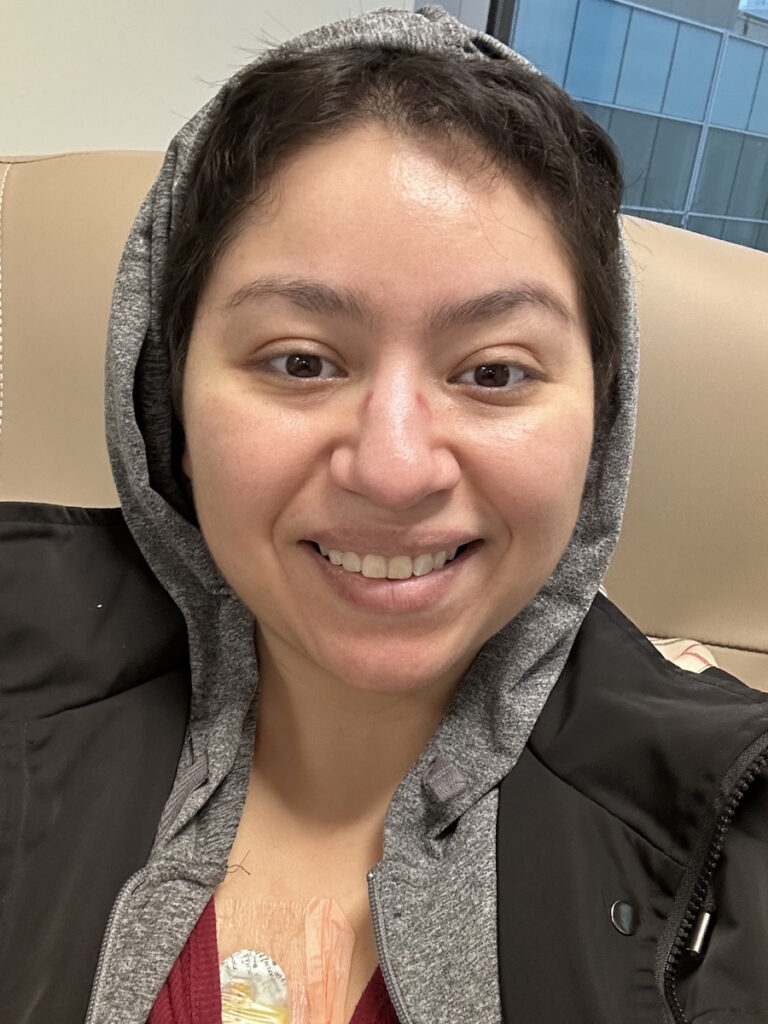
Beginning chemotherapy
I didn’t have to do chemo because of my prognosis, but my surgeon and team recommended that I do it as an insurance policy. I was prescribed 2 different types. I had an infusion chemo which entered through a port and a pill chemo. I would do one infusion every 3 weeks. Then I was on pill chemo for 2 weeks at a time and I’d get a break at the end of it.
»MORE: Chemotherapy FAQs & Patient Stories
Chemo Side Effects
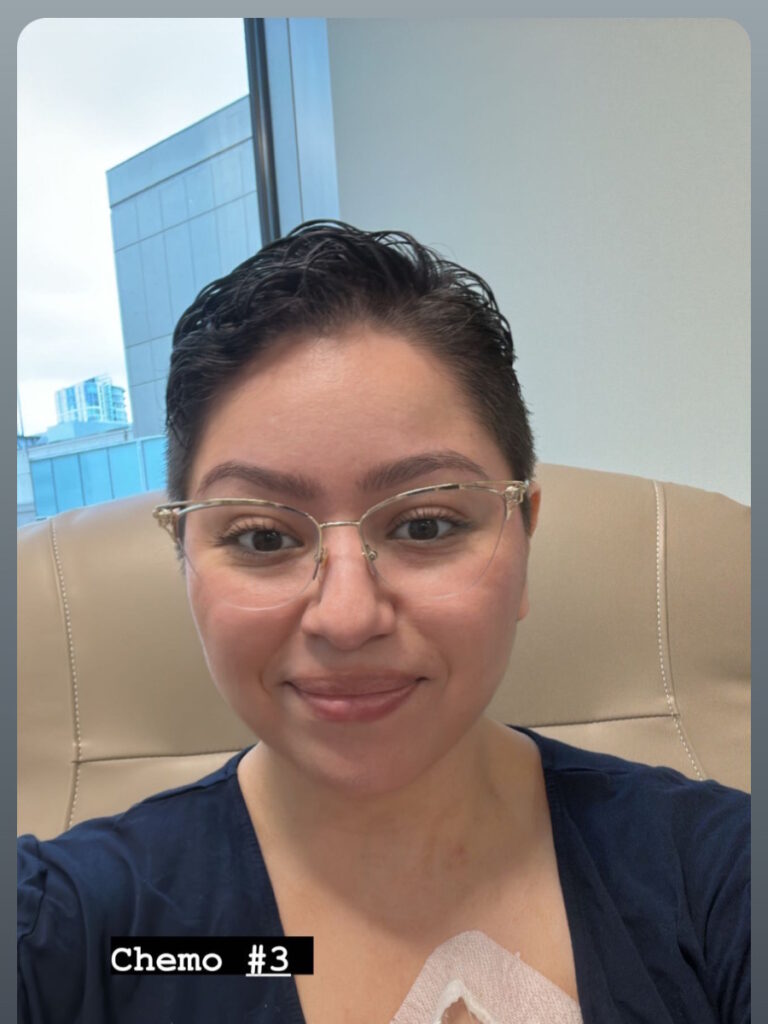
Which chemos were you on and did you have side effects?
Capecitabine. The infusion chemo was called oxaliplatin. I had side effects with each. With capecitabine, I had hand-foot-and-mouth, where you get really bad sores everywhere. The other chemo was oxaliplatin. It’s a platinum chemo. It had some really strange side effects. You couldn’t touch anything cold. You couldn’t ingest anything cold. I couldn’t drive in my car with the AC on or it could close my throat. Everything had to be room temperature or hot.

It was in the middle of the summer, so one of the biggest issues I ran into was I was dehydrated a lot. I was hospitalized 2 different times for dehydration which was scary. I lost a lot of weight. I think I lost about 25 pounds. I tried to eat when I wasn’t hungry. I had to watch what I ate. They tell you you can’t have raw fruits and vegetables while you’re on chemo, which is so weird because you should be eating healthy foods, and they said to eat what I could.
The first two days after infusion chemo and pill chemo, you’re the sickest, you’re nauseous. It’s really, really hard to get up and move around. With oxaliplatin, like I said, it’s a platinum chemo so it causes neuropathy. You have a lot of tingling going on in your body. It got to the point where my eyes were affected by it. I could taste it in my mouth. It was very all-consuming throughout my body.
Stopping oxaliplatin
I did my own research about my particular prognosis and I decided to stop oxaliplatin after 4 rounds. That’s the infusion chemo. A lot of patients push past that, and there are some patients that end up disabled from doing that chemo. I did not want to do that. I didn’t want to risk that. It was making me so sick that I could barely eat.
Did anything help alleviate your chemo symptoms?
When I was dehydrated, I would go in and get pumped with fluids. That helped. I did take Zofran to help with the nausea. You can’t be in the sun either when you’re on chemo. You have all these things that you can’t do.
The best thing that helped with the side effects was to get my mind off of it.
I think for me, the best thing that helped with the side effects was to get my mind off of it. I taught full time while I was on it. That was my choice. I didn’t want to lay in bed every day and dwell on it. That’s just my personality so I decided that I was going to work and let that be the thing that would help get my mind off of it. I did oxaliplatin for 3 months and capecitabine for 6 months.
When I went back to school to teach, I did physical therapy and that helped a lot. It helped me build up strength because I had lost so much muscle mass and lost so much weight and it helped with getting through those days.

Reflections
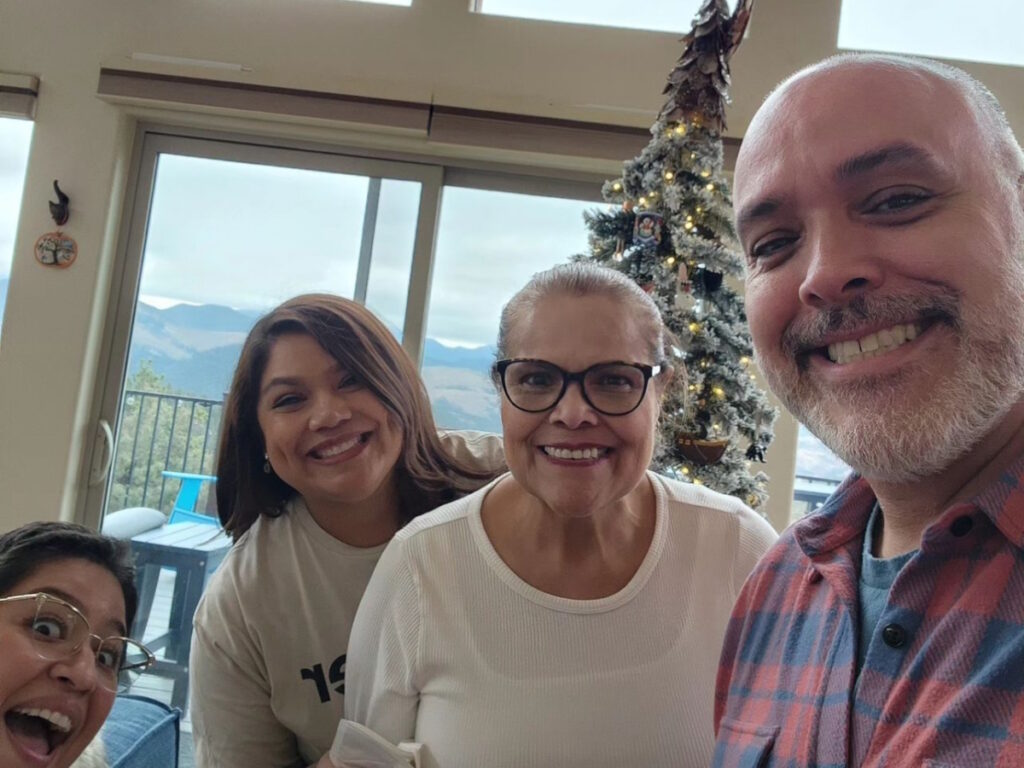
How long have you been in remission?
I am almost at the 3 year mark of being in remission. I count it as April. My oncologist counts it as November because that’s when I finished chemo, but I think that the surgeon got everything.
How often do you get scans and do you experience scanxiety?
I don’t think that it ever really leaves you. I think that it stays with you.
I just hit the 2.5 year mark, so now I go every 6 months. I think that’s one of the hardest parts. I was joking with a friend that I’m a part of an exclusive club now because it doesn’t really ever leave you. With scanxiety, I just do my best to just try and stay positive. It’s always quite exhausting because it’s a 4-day process – blood work, scan, and meet with your doctor.
My aunt is a phlebotomist, so she’s always encouraging, giving me tips on how to stay positive and hydrate, make sure you’re ready to go. But it is a real thing, and I honestly don’t think that it ever gets any better. I think that you learn how to manage, how to live with it. The farther out that you get, you feel better. But I don’t think that it ever really leaves you. I think that it stays with you.
What advice do you want to share with cancer patients?

Advocate for yourself, know your body, listen to your body, and keep pushing until you find answers.
You need to advocate for yourself and you need to be able to listen to your own body. Science only goes so far. Knowing, understanding, and listening to your body is really important. Because if you’re sitting in front of this doctor that doesn’t know you, you’re just a statistic. They’re trying to see where you fit, and if you don’t fit the category, you don’t fit the profile, of course they’re not going to suspect anything.
I also think that you have to hold on to your faith and keep pushing through roadblocks and things that are in your way. You just have to keep going until you find the answers that you really desire to have. For me, that was, I’m sick of hanging out in ambiguity. I know I have it. You are speculating, but that’s why we have science. That’s why we have these things. We shouldn’t be profiling people based on their age or the way that they look. We should be listening to the patient and to their concerns.
Advocate for yourself, know your body, listen to your body, and keep pushing until you find answers. That’s why I’m alive and well today, because I advocated, and I continued to push until I got the answers that I needed. I don’t blame any of them. They’re doctors, they’re human, but I do think that they need to listen to patients better. I think that they need to listen to their patients, listen to the concerns that they have, and really do a better job of putting something in place that is going to help. Help eliminate this ambiguity. For people that may not feel as comfortable to advocate, you just have to remember that you know your body. So even if it’s something that’s totally foreign, talk to somebody about it and try and find those answers that you are desiring to look for.
More Colorectal Cancer Stories
Cora V., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, unintentional weight loss, blood and mucus in stool
Treatments: Chemotherapy, chemoradiation, surgeries (temporary ileostomy and reversal, liver surgeries and ablation)
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)