Prostate Cancer Overview
Prostate cancer, is the second most common type of cancer amongst men after skin cancer, often responds well to treatment. If you or someone you know is facing prostate cancer, knowing what lies ahead can make the journey more manageable.
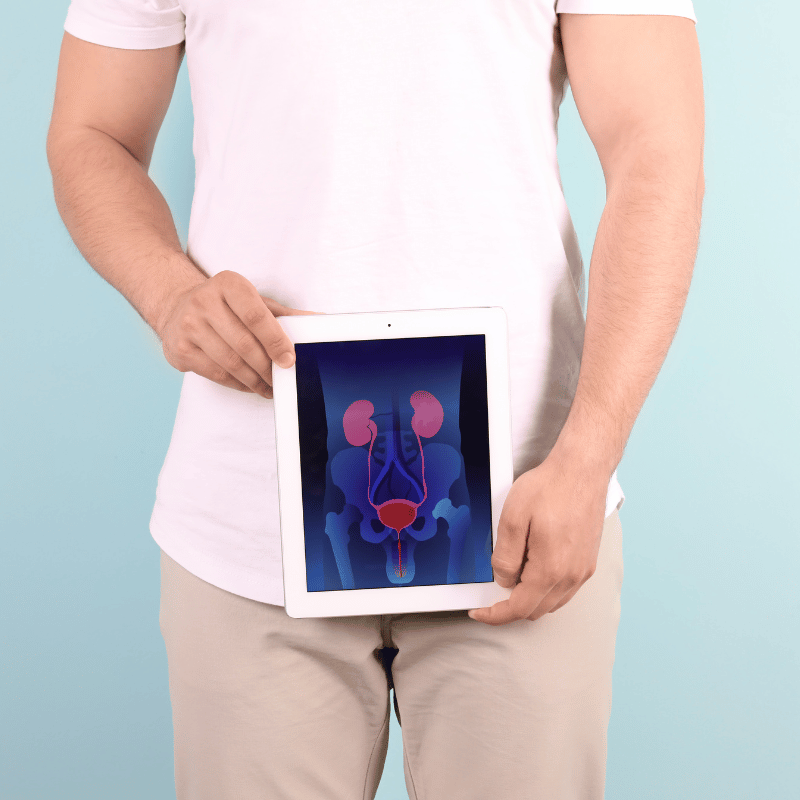
This cancer begins when the walnut-sized prostate gland’s cells start growing out of control. Located below the bladder and in front of the rectum, this little gland contributes to the fluid that’s part of semen.
What are common symptoms of prostate cancer?
Symptoms may vary depending on individuals, but here are some of the more commonly reported prostate cancer symptoms in men:
- Changes in urination (more frequency, slower or interrupted flow)
- Difficulty urinating
- Difficulty completely emptying the bladder
- Burning sensation or pain during urination
- Persistent pain in the hips, back, or pelvic region
- Blood in either urine or semen
- Pain during ejaculation
Note: These symptoms can represent a condition other than prostate cancer.
Who is most at risk for prostate cancer?
Every man has a risk for developing prostate cancer. In the U.S., about 13 of 100 men will get diagnosed with prostate cancer. Two-thirds of those diagnosed will die from prostate cancer1.
Age is the most common risk factor for prostate cancer. As a man gets older, his chance of getting prostate cancer grows.
There is heightened risk for African-American men or those with family history of prostate cancer.
How do you screen for prostate cancer?
There are two basic tests commonly used for screening:
pROSTATE sPECIFIC ANTIGEN (PSA) TEST
The PSA test is a blood test that measures the level of prostate specific antigen, or PSA, in the blood. The prostate creates the PSA. If the levels of PSA are higher in a man, it may be a sign of prostate cancer or another condition that impacts the prostate.
PSA levels may also be affected by other factors, including but not limited to:
- Specific medications
- Specific medical procedures
- Infected or enlarged prostate
If the PSA test shows a higher level, your doctor may suggest a biopsy as a next step.
Digital Rectal Examination (DRE)
In this case, digital refers to the finger. A digital rectal examination or DRE is when a health care worker puts a lubricated, gloved finger into a man’s rectum to try and feel for any signs of abnormalities, including cancer.
Pros and Cons of Screening
According to the U.S. Preventive Services Task Force (USPSTF, 2018), the recommendations include3:
- Men aged 55 to 69 years who may consider screening using a PSA test
- Every man should discuss the benefits and risks of screening, tests, and treatment with their doctors before making a decision
- Any man who is at least 70 years old should avoid being screened routinely for prostate cancer
- Men who are 70 years old and older should not be screened for prostate cancer routinely.
Gleason score
When there is a prostate cancer diagnosis, doctors will usually give a grade or Gleason score, to assess how aggressive the tumor is. The scoring is based on how aggressive or abnormal the cancer cells are (under a microscope lens).
The Gleason Score is the grading system used to determine the aggressiveness of prostate cancer. This grading system can be used to choose appropriate treatment options.
The score ranges from 1 to 5, and each patient is given two grades. There’s a primary grade to describe the largest area of cancerous cells, and a secondary grade to describe the next largest area of cancerous cells. The healthier the tissue, the lower that score o the 1 to 5 scale. That means the total score maxes out at 10.
One example is a Gleason score of 3+4=7. That would indicate that most of the tumor is given a grade of 3 and the next biggest section of the tumor has been described as grade 4. The total Gleason score would be 7.
gleason score 6 and below
A Gleason score 6 and below is considered “low grade,” or less aggressive. This means there’s less of a chance the cancer will grow and spread, compared to a higher Gleason score.
Most men who get a prostate diagnosed that is localized and low-grade will “die of something other than prostate cancer” (NCI).
gleason score 7 to 10
A Gleason score of 7 indicates an intermediate risk of the cancer being aggressive. Primary tumors that are scored 3 with a secondary score of 4 have a “fairly good outlook,” compared to the inverse of 4 then 3, which have evidence of being more likely to grow and spread to other areas4:
A Gleason score of 8 or higher indicates a cancer that is more likely to grow and spread more quickly. This can be described as “high grade” or “poorly differentiated.”
John B., Prostate Cancer, Gleason 9, Stage 4A
Symptoms: Nocturia (frequent urination at night), weak stream of urine
Treatments: Surgery (prostatectomy), hormone therapy (androgen deprivation therapy), radiation
Eve G., Prostate Cancer, Gleason 9
Symptom: None; elevated PSA levels detected during annual physicals
Treatments: Surgeries (robot-assisted laparoscopic prostatectomy & bilateral orchiectomy), radiation, hormone therapy
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Symptoms: Urinating more frequently middle of night, slower urine flow
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Active Surveillance
Leading organizations with prostate cancer strongly urge physicians to recommend active surveillance to patients with low-risk prostate cancer.
According to a cohort study published in the Journal of the American Medical Association (JAMA), that included more than 20,000 men who underwent or were undergoing treatment at almost 350 various urology clinics in the U.S., showed that the numbers of patients on active surveillance more than doubled in recent years – from 26.5% in 204 to 59.6% in 2021. (Cooperberg et al., 2023)
Study authors, led by Matthew R. Cooperberg, MD, MPH of Univeristy of California San Francisco (UCSF), wrote that the adoption of active surveillance (AS) in community practices nationally has been slow, with an increase in the last decade to an estimated less than 50%compared to less than 10% before 2010. Compare that against the “optimal rate of AS” reported by the US Veteran Affairs system and other healthcare systems to be greater than 80%. 2
Hear from prostate cancer patients
- Who Is at Risk for Prostate Cancer? (2023, July 17). Centers for Disease Control and Prevention. https://www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm#:~:text=Out%20of%20every%20100%20American,common%20risk%20factor%20is%20age. ↩︎
- Cooperberg, M. R., Meeks, W., Fang, R., Gaylis, F., Catàlona, W. J., & Makarov, D. V. (2023, March 2). Time Trends and Variation in the Use of Active Surveillance for Management of Low-risk Prostate Cancer in the US. JAMA Network Open. https://doi.org/10.1001/jamanetworkopen.2023.1439 ↩︎