Caroline’s Stage 3 Placental Cancer & Gestational Trophoblastic Neoplasia Story

I would probably say what that doctor said to me: “They’re going to kick your butt for a few months, but it’s going to be okay.” There are so many success stories. After being on the other side of it, I can tell you it really is going to be okay.
Caroline Chisolm
- Name: Caroline Chisolm
- Diagnosis: Placental cancer, gestational trophoblastic neoplasia at age 30
- Staging: 3
- 1st Symptoms:
- Morning sickness
- Positive pregnancy test
- Treatment:
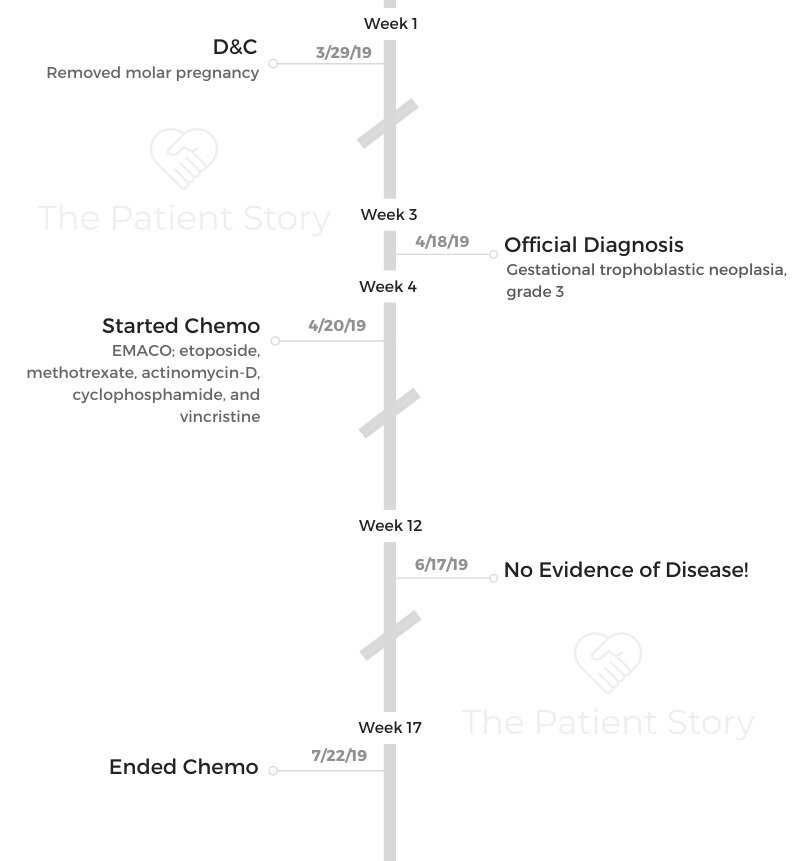
- D&C
- Chemotherapy
- EMACO, 14 weeks
- Etoposide
- Methotrexate
- Actinomycin-D
- Cyclophosphamide
- Vincristine
- EMACO, 14 weeks
- Diagnosis
- Treatment
- Reflections
- Did you have a fertility conversation?
- What is it like being a parent with cancer?
- Can you talk about hair loss?
- How did cancer affect the relationship with your husband?
- Can you talk about ways people were able to support you?
- What advice do you have on self-advocacy?
- What would you say to someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
When did you find out something was wrong?
I went to the doctor on March 22nd expecting to see a heartbeat. There was a mass instead, so they checked my beta hCG (human chorionic gonadotropin), which is the final determiner of whether it’s molar or not. A molar pregnancy is when two sperm penetrate one egg. It doesn’t ever form an actual baby. It forms a mass. I had that. My number on that day was 172,000, and normal would’ve been around 30,000.
A dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. We scheduled a D&C for the next week. There was no cancer found in the mole. My beta hCG went down to 40,000 a week later. Everything went back to normal. Of course, that sucked because I thought I was going to have a kid. That’s a shock in and of itself.
How did you find out it was cancer?
About two and a half weeks after the D&C, I went to the beach for a few days, and I started getting morning sickness again. My bleeding started picking up. I felt really bad.
I got back on a Sunday, and the earliest appointment I could get was Tuesday, so I saw my doctor that day before work. I said, “I think it’s back. I know you can bleed after a D&C, but I’m bleeding a lot.”
She said, “Okay. Let’s check your numbers. Hopefully it’s not.” She checked my numbers. I went to work. This is very female, but I was changing tampons every 15 minutes. I still worked. Then, around 1:00pm, she called. She said, “You’re right. You’re back at 220,000. You need to come to my office.”
I went to her office, and I called my husband. She said it didn’t mean it was cancer, but it meant that it was a recurrent mole, and that’s treated with a mild form of chemotherapy called methotrexate. Even though it wasn’t cancer, she said I still needed to see the gynecological oncologist because they administer the chemo.
She wanted to do a full body scan and make sure it hadn’t gone anywhere and that it wasn’t cancer. The initial CT scan results were no metastases. Since I work at the hospital I was treated at, I could see my results quickly. I was so relieved, but it wasn’t a final read yet.
The next day, my bleeding was so bad that I went through a super plus tampon in three minutes. I drove myself to the emergency department.
I told my husband to just stay at home with our son, who had just turned one. I said, “I just have to go have this thing taken out again. It’ll be okay.”
The resident came in and said they were going to call my gyno oncologist. She came in from home. I thought she was just being very courteous, but when she got there, she asked, “When did you see your CT results?” I told her I saw it probably right after it was posted.
She said, “There was an addendum. They found five lung metastases. This is cancer.”

She told me, “It’s aggressive, but it’s very susceptible to treatment. We’ll get you started on chemo tomorrow.” I asked about freezing eggs, and she said, “No. There’s no time.”
I sat there and cried to the point where I couldn’t breathe. I was trying to maintain some kind of composure though because I knew it was going to be harder on my husband than it was on me.
I called him at home. It was tough to call him and tell him that I had cancer over the phone.
I’m a doctor and didn’t even know what gestational trophoblastic neoplasia was. It starts out as a molar pregnancy. A molar pregnancy is when two sperm penetrate one egg. It doesn’t ever form an actual baby. It forms a mass. I had that.
A doctor came in the next day and said, “I’ve seen hundreds of women with what you have. I’ve never seen a single recurrence. You’re going to be okay, and you’ll hopefully be able to have more kids.” He told me, “We’re gonna kick your ass for three months, but then you’re going to be okay.” So I said, “Okay, if anyone can do three months, it’s me. I can do this.”
Treatment
What was your chemo regimen?
I had chemo weekly for 14 weeks. Because the EMACO regimen is so strong and the cancer is so aggressive, they really don’t want you to miss a dose or delay a dose. For that reason, I started on Neupogen my first week.
I had three drugs on Week 1 and two drugs on Week 2. I did that seven times. My first week was Etoposide, methotrexate and actinomycin-D. That was an overnight infusion, so I had to stay in the hospital for that. I checked in at 8:30am, got settled in, did my labs, and all that. I normally didn’t start on chemo until about 2pm. I would go from about 2pm to about 6am. I’d hang out and wait, and then I had another infusion for an hour and a half, and I’d go home in the mid-afternoon.

My husband stayed with me every time. My mom drove up from North Carolina and stayed with our son at home so my husband could be with me. They didn’t want me to have to be by myself.
The infusion center is across the street from the hospital, and I did my second week there. That was the cyclophosphamide and vincristine.
I would get there around 8 or 9am, and I’d start within about an hour and a half because there was a pharmacist specifically for dosing the chemotherapies. Most of the time, I’d be done by about noon or 1pm.
My husband would usually go to work, and I’d meet him afterwards for lunch.
I didn’t have any reactions to chemo during infusions, but I did react to the Neupogen. My hands would be really itchy after taking it.
I went to a campground with my family and hung out, so I thought maybe I had gotten into something. The steroids stopped it a little too.
It kept getting worse and worse, but I asked my doctor about it, and she said it was probably Neupogen. I was getting steroids every time with chemo, so that would help, but by the last time, my hands were so swollen.
I couldn’t bend my fingers, and I started getting rashes on my joints.
What side effects did you experience from chemo?
I had some nausea, but they gave me some anti-nausea medicine that lasts a week. That worked really well. I took a Zofran here and there. I just kinda felt like I did in the first trimester of pregnancy. I just wanted carbs.
My main thing was fatigue. Every round, it just got worse. For round 3 or 4, I fell asleep in an infusion because I couldn’t keep my eyes open anymore. The last two rounds they dropped Etoposide because it’s got a side effect of leukemia. Once I got to my last two cycles, I was cancer-free, so they dropped that just to be safe.
When I was still getting every drug, though, there were days I would sleep for about 20 hours a day. I would wake up for a few hours to play with my son each day, but that’s about it.
Did you get your numbers checked during treatment?
They checked my beta hCG, which is the tumor marker, because it’s placental cancer. It makes beta hCG just like a normal pregnancy would; it just makes a lot more of it. They checked that every two weeks.
It was 218,000 the day I started chemo. It dropped to 19,000 after two weeks. Then, it was 1,200. It slowly went down. For my fifth cycle, it was at 2.
It’s been undetectable ever since cycle 6 and 7. I get checked every month now, and it’s stayed undetectable.
They did an ultrasound of my uterus after everything was done just to make sure there was no dead tissue hanging out in there. They knew it was dead if it was there. They just wanted to make sure they didn’t need to go get it out.
This is kinda gory, but my tumor was the size of a football, and they didn’t do any surgery to remove anything, so it all just had to make its way out naturally. That was terrifying.
After cycle 2, around three weeks into chemo, I stood up off the couch, and it just hit the floor. They had told me that it would happen. It didn’t freak me out as much as it freaked my husband out.
They made the decision not to take it out surgically because my tumor was so vascular, and I was bleeding so much. They would’ve wound up having to take my whole uterus, and they knew I wanted more kids.
When did you find out you were NED?
They had said that once my beta hCG was 0, I would be considered no evidence of disease. I check it every month. There’s nothing for me to do that’s better than just checking the blood work.
Reflections
Did you have a fertility conversation?
Because this cancer only affects fertile females, the chemotherapy is designed to not be hard on your ovaries. That’s the reason why there’s so many drugs. They all work a little differently. None of them kill one thing, so it kind of preserves your ovaries.
My doctor said there’s no reason I can’t try again once I’m 6-12 months out of treatment, so I’m in the window now where we can start trying again now.
She had asked me the night I was diagnosed, “Do you want more kids?” I said, “Yes, I do.” She told me that if I didn’t stop bleeding, we’d have to have a serious conversation about taking my uterus.
Of course, I want more kids, but I told her, “I already have a kid at home. Don’t put my life in danger because of potential future kids that don’t exist yet. I have to be here for the one I already have.”
I refused to hemorrhage to death because of the possibility of more children in the future. If it was me or my uterus, I would choose me every time.

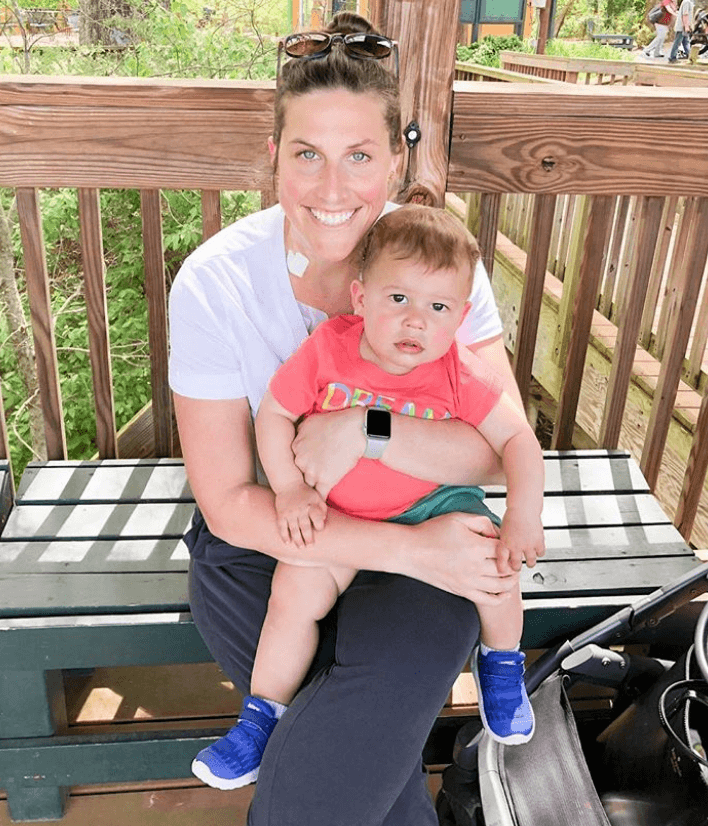
What is it like being a parent with cancer?
The second night we were in the hospital, I remember laying there while my husband was asleep. I thought, “I have a one-year-old. I can’t die.”
Everyone would be okay if I died. My husband could handle it. My son would be okay, but I really didn’t want him to grow up without me.
He’s supposed to be mine. That first little bit, I just really thought about him.
If you’re like me, you don’t ask for help. I’m very type A. If you’re like that, just accept the help when it comes. You need it. The people that love your child want to do just that. Let them love you and love your child and help.
Be okay with not being with your kid 24/7. He spent a lot of time with his grandma, and that’s okay. She’s his Nana, and they love each other. It still wasn’t me, though, and that was hard.
I felt guilty sometimes too because I had never put him in daycare on a day when I wasn’t working. I thought I was going to just keep him at home with me, but my body let me know that that wasn’t going to happen.
The thing is, I don’t think he noticed much of a difference because for the two hours I saw him in the morning and the two hours I saw him in the evening, I gave it every ounce of strength I had. It just seemed like a normal day of me going to work for him. The only difference was instead of me going to work while he was at daycare, I went to sleep.
Can you talk about hair loss?
It started falling out after the first week. We had a wedding to go to. I showered before that, and when I got out, it started coming out a little.
I curled my hair and made it so pretty. I cried getting ready, but I did it. We went to the wedding, and of course we had so much fun.
At week 3, it started coming out more. By week 5, I cut it short because long hair coming out was so annoying.
During week 8, I got out of the shower and had a big bald spot. My cousin came over and shaved my head.
I cried, but then by the next morning, I was okay.
I wish I had shaved it before I did. I dreaded showering. Had I shaved it, I wouldn’t have had to worry so much. People told me that, and I didn’t take their advice. Looking back, I wish I had shaved it earlier.
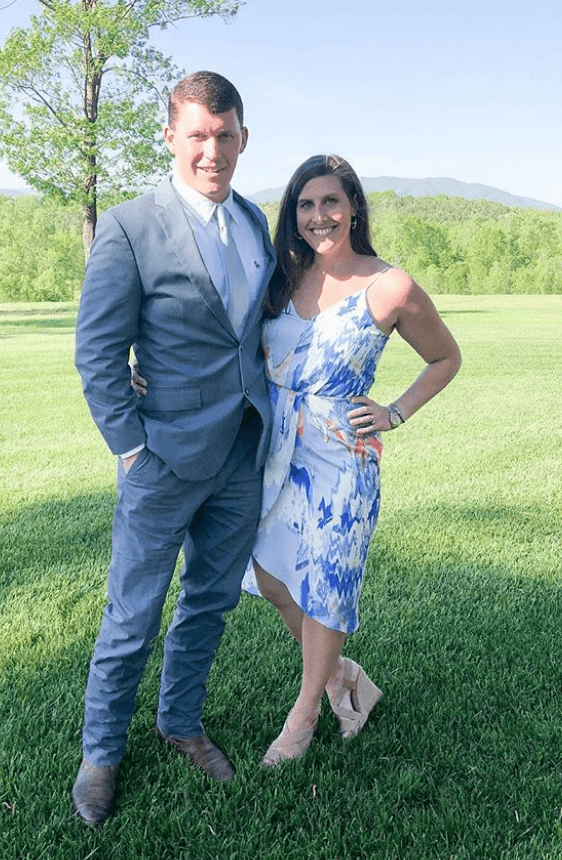
How did cancer affect the relationship with your husband?
My husband is one of the hardest working people I’ve ever met. I’m like that too. We go and do constantly. When I had to stop doing that, I think it was hard for him to watch. Not that it was hard on him, but that he just hated to see me that way.
There were days when he’d come in, and he wouldn’t be trying to be mean, but he would ask me, “Are you going to nap all day?” I’d say, “Yes, I am.” We’re just not normally like that. We’re a team, and on the weekends when we’re not working, we’re building something or doing something like that. It was hard for him to be on his own.
My husband has never had anyone close to him get diagnosed with cancer. He didn’t really know how to deal with it, I don’t think. It changed him though. It made him slow down and stop sweating the small stuff.

Can you talk about ways people were able to support you?
My mom was able to come up every other week for my long treatment. A bunch of people I work with helped me, of course, but also my family.
One person I work with brought a huge cooler full of food for my family to eat while they were visiting and left it on my porch.
One thing that was the most helpful was food for my son. There’s a company that delivers flash frozen organic meals for toddlers.
I was eating cereal all the time, so I didn’t want my son to be eating like me. My husband’s family paid for us to have that service.
As silly as it is, gift cards were helpful too. Luckily, I have insurance, but in the beginning, you don’t know how it’s going to go.
People would drop off gift cards to various restaurants. It made my life so much easier just being able to go pick something up.
When people would come just sit with me, that was nice. I didn’t have much energy, so it was great.
I didn’t want to be alone and get in my head, but I didn’t have the energy to get out, so them being willing to sit with me was so sweet.
What advice do you have on self-advocacy?
My cancer was very limited with options on what we could do. I pretty much just had to go with my protocol. A lot of cancers aren’t like that though. Fight for what you want. Be your own advocate.
Yes, I’m a doctor, but I don’t know what you look, act, and feel like before you got sick. As a doctor, you can only go off of so much. The patient knows their body better than you do.
What would you say to someone who has just been diagnosed?
I would probably say what that doctor said to me: “They’re going to kick your butt for a few months, but it’s going to be okay.” There are so many success stories. After being on the other side of it, I can tell you it really is going to be okay.
I still haven’t found an instance where someone died with this. It used to be a death sentence, but now with chemo and medical advances, it’s totally curable.
With a lot of cancers, there’s not a light at the end of the tunnel, but I had that hope. I could see my numbers going down, and that was so reassuring. Rest, know you’re going to be okay. Sleep. Sleep. Sleep.
It’s going to kick your butt, and then you’ll be okay. You’ll bounce back. It’s not going to kill you. Be thankful for that and make it through the hard 14 weeks or so of chemo. You can’t let it get you. You’ve just got to keep moving.
Figure out what keeps you going, and make that your mission. For me, it was needing to nap as hard as I could so I could see my son when he got home. It was to get through chemo and get some rest so I can go home and see my husband the next day. Do what you have to do to get through that next day or week.

Inspired by Caroline's story?
Share your story, too!
Gestational Trophoblastic Neoplastia Stories
Caroline C., Gestational Trophoblastic Neoplasia & Placental Cancer, Stage 3
Symptoms: Morning sickness & an unusually high beta hCG
Treatment: EMACO chemotherapy
...
Shannon W., Choriocarcinoma
Symptoms: Molar pregnancy, vaginal bleeding, overall feeling of unwell, cramping, weight loss, elevated HCG level, feeling bloated
Treatments: Chemotherapy, surgeries (D&C, total hysterectomy)
...


One reply on “Caroline’s Stage 3 Placental Cancer & Gestational Trophoblastic Neoplasia Story”
I’m so happy you were able to fight this. My best friend Jenny had a baby and they did not get all of the placenta out. By the time they found out that it was cancer it had gone into her lungs she fought for a year went into remission twice but did not survive her baby was just barely a year old when she died.