Kristin’s Myelofibrosis Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

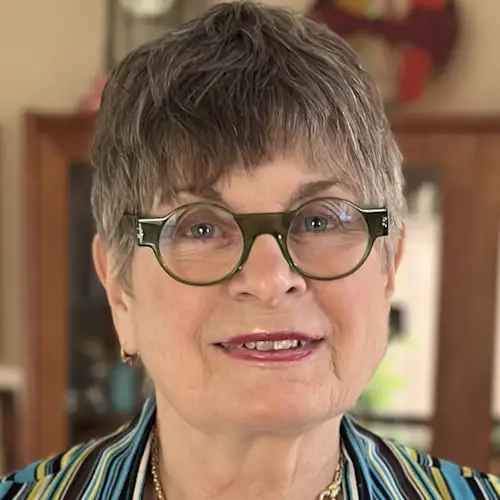
Kristin shares her experience of being diagnosed with myelofibrosis, a rare type of bone marrow cancer.
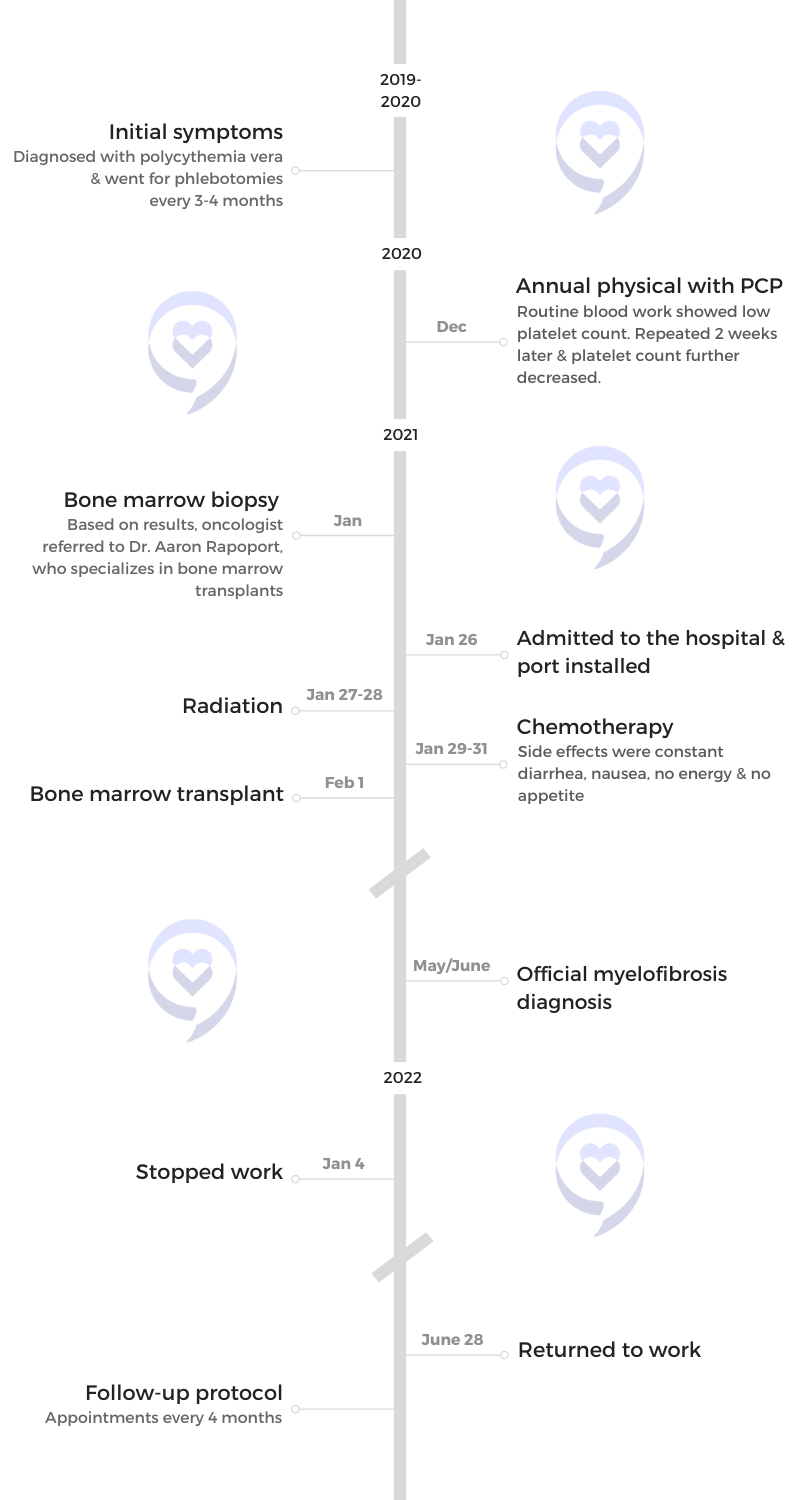
She was initially diagnosed with polycythemia vera (PV), a blood disorder wherein there is an increase in red blood cells. She would have phlebotomies done every three months as a treatment for about a year until she didn’t need to anymore.
Shortly after, a routine blood work showed very, very low platelets. After having a bone marrow biopsy done, she was referred to an oncologist.
The only treatment suggested was a stem cell transplant. Unable to match with a donor through Be The Match, she thankfully matched with her sister. She also shares how she dealt with her 25-year-old daughter’s Hodgkin lymphoma diagnosis.
Kristin shares her journey and the importance of finding positive people to surround you.
In addition to Kristin’s narrative, The Patient Story offers a diverse collection of myeloproliferative neoplasm (MPN) stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Kristin D.
- Diagnosis:
- Myelofibrosis
- Mutations:
- JAK2
- Initial Symptoms:
- None; caught at routine blood work
- Treatment:
- Stem cell transplant

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Introduction
I’ve been a flight attendant since ‘98, which has always been my dream job. I grew up in Chicago and went to college at the University of Illinois.
I’ve lived in a lot of interesting places. My favorite place in the world is where I live now in Annapolis, Maryland. My husband lived here so I moved here. We bought a house in 1996 and had a great life.
At the end of 2021, I was told I had myelofibrosis. I didn’t have many options. The treatment for it was a stem cell transplant.
It’s a very rare blood disease. I’ve never heard about it and I don’t know anybody who has. Luckily, I had a sister who helped me navigate through the whole process.

When I had routine blood work done, my platelets were very, very low so my general doctor wanted me to see an oncologist.

Pre-diagnosis
Initial Symptoms
During my annual blood work, they said my red count was so high. They said, “Don’t worry about anything. It’s easy to treat with phlebotomies.” They said it was not that uncommon.
I would go to the blood center every three months and pump out a couple of pints of blood. They would discard it because it wasn’t good blood. It was painless. I didn’t feel different going in or coming out.
I did that for a year. One time, my red blood cell count was good enough that I didn’t need it. I thought that was odd but a good sign.
Shortly after, when I had routine blood work done, my platelets were very, very low so my general doctor wanted me to see an oncologist. He did a bone marrow biopsy and turned me over to the University of Maryland.
I felt great. I wasn’t fatigued. I played a lot of tennis and nothing.
The only symptom was I bruised easily. There were bruises on my hands, legs, and arms. I would wake up with itchy arms.
I felt confident this wasn’t something I was going to die prematurely of because there was a treatment for it.

Diagnosis
Getting the Diagnosis
Nobody in my family ever had something like this. They said it’s not genetic.
My oncologist at the University of Maryland is fantastic. He’s a real rose-colored glasses kind of guy and non-alarmist. He said there was no explanation. It wasn’t environmental, genetic, or my lifestyle.
Before treatment, they thought it was related to working at altitude all the time, but they ruled that out.
Reaction to the Diagnosis
It was frightening, but I felt confident this wasn’t something I was going to die prematurely of because there was a treatment for it.
My sister’s a nurse. She’s my right hand when it comes to looking at my test results. She’s my interpreter because a lot of that’s so foreign to me. She was also my donor.
Getting a Second Opinion
I went for a second opinion at Hopkins. The doctor recommended a book about myelofibrosis, but I could never get my hands on it.
When people say, “What were you out with?” I say it’s a kind of blood disorder. I don’t say myelofibrosis because nobody knows what it is.

There was nothing else I could do, but it was up to me as to when to do it.

Treatment
Discussing the Treatment Plan
Other than the transplant, there was no other treatment suggested. It was the only solution. The only option I had was when to do it.
He said that since I felt so good, I could wait a year or two or three. He said it’s better to do it when you’re young. The way I am is I want to get it done.
He said, “You’re going to need a donor. You’re going to need to take a year off work,” and that shocked me. It turned out to be a year and a half.
I block out bad stuff and bad times, but I vaguely remember there was no other option than the transplant.
Bone Marrow Biopsy
They looked at my counts and my platelet counts were getting gradually worse. They said the next step was a biopsy, which was pretty much a no-brainer.
They got the diagnosis from the bone marrow biopsies. I’ve had probably at least 10 of them in my life.

Preparing for the Bone Marrow Transplant
Luckily, I have two children and that’s a good thing because they said the age of the donor is important to its success.
My son was living in Maui so he wasn’t an option. I didn’t want him to interrupt his life. My daughter stepped up to the plate and said she would do it. She started going for all the visits and tests.
I didn’t match with anyone in Be The Match. They said I was 1 in 1,000,000. My sister was a match so even though she was 61 at the time, there were advantages because we were full siblings.
I was in the hospital for five weeks. It was like being in a bubble.
Going Through Transplant
I went through radiation for two days for 15 minutes on each side.
I never knew how chemo worked. You get a port and it goes right in. You don’t feel a thing. They called it the eat, drink, and be merry days.
After the chemo went in, I felt really good. I couldn’t leave the floor so I would go on the treadmill.
My nurses predicted that by around day 10, I would feel sick and wouldn’t have any energy or appetite. They were right. Everything people say about chemo is true.
I had diarrhea pretty much for two months. It was a slow healing.
In my ward at the University of Maryland, I was the youngest person there. I was amazed that older bodies could go through that.


Recovering from Transplant
I was in the hospital for five weeks. It was like being in a bubble. You think it’s relaxing because you can read or watch a lot of TV or movies, but they’re constantly checking on you. They get your vitals every three hours. But I got a lot of support from them. I had my designated visitors so the five weeks went by fast.
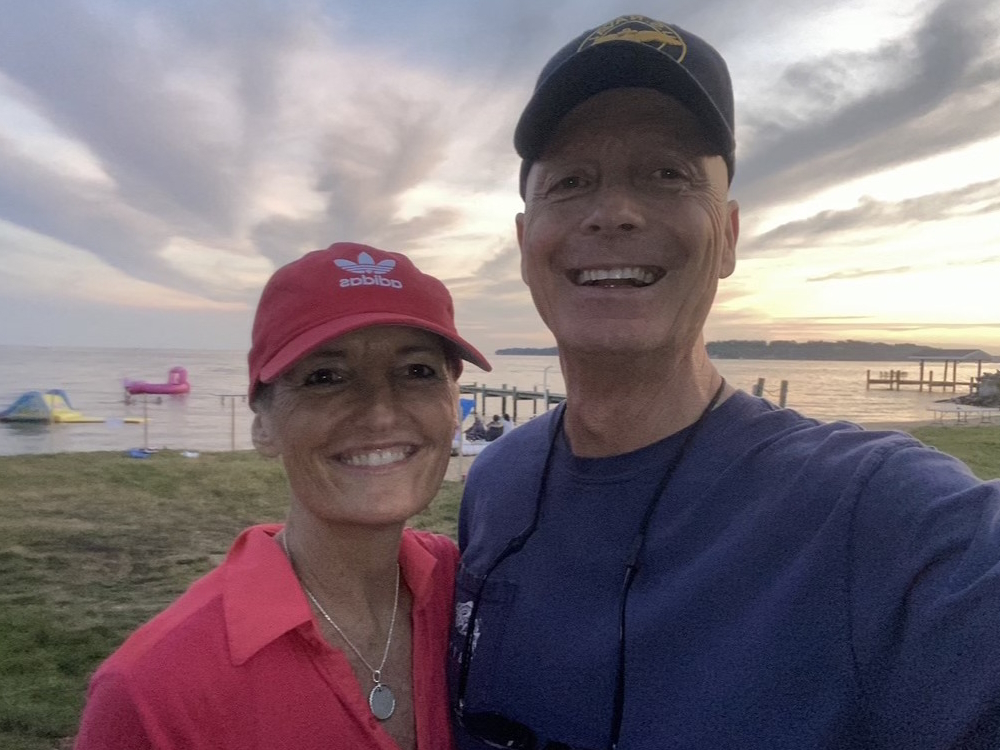
You need a caregiver. You need somebody to live with you in case you fall, to check your temperature, and to monitor you. My best friend from Indiana gave up three months of her life and came to live with me.
She was the perfect person for it. She took notes and took charge of my meds. She went with me to every appointment. She’s an incredible person.
If this comes back, when my numbers start to falter, I will do it again in a second.
Transplant Didn’t Work As Planned
When they found out I accepted only 2% of my sister’s cells, they looked at it as somewhat of a failure. I was so mad when a nurse said my transplant was a failure. I asked Dr. Rapoport, “Why did she call it a failure?” He said, “It was a bad choice of words. It didn’t work as planned. You still succeeded in getting rid of the JAK2 mutation.”
I was so upset about that because it meant my immune system was weak.
I was on VALTREX (valacyclovir). When my refill came up, I asked Dr. Rapoport, “Do I still need to be on this?” He said no. I’m in the process of getting vaccinated again.
They offered clinical trials to everybody on the floor. It required coming back to the hospital. I live an hour away and I didn’t want to do it.

Danielle is different than me. She investigated and talked to people who had been through it. She met a few people online who had myelofibrosis. She wanted to know where you were at this point, this point, and this point. I wanted to dive in and then forget about it.
Getting Another Transplant
They want to see me every four months. If this comes back, when my numbers start to falter, I will do it again in a second.
My best friend came with me to one of my appointments and said, “I don’t understand what’s going on with Kristin. Is she cancer-free?” A different said, “She’s never going to be cancer-free. It’s just the way it works.”
Hopkins had a way of doing things that I liked and didn’t like, but I would probably do it again there.
As far as finding another donor, I would probably go with my son because he’s young. It worked out well for my daughter and I’m sure he would do it. My sister’s 63 and if it comes back, she might be older.
My numbers have been stable. They’re not off-the-charts great, but they’re not getting worse.
Life Post-Transplant
I wasn’t allowed to vacuum. I wasn’t allowed to go anywhere without a mask. I wasn’t allowed in restaurants. I wasn’t allowed to eat anything that other people brought in.
They made me paranoid about germs, going outside, and eating anything that hadn’t been washed. No sushi, nothing undercooked, and no lunch meats. They put the fear in me. If I got sick with pneumonia or COVID, it could have been really bad because I didn’t have anything to fight that off, but I didn’t.
Follow-up
When I go to the doctor, I have a little fear, but Dr. Rapoport emphasizes that my numbers have been stable. They’re not off-the-charts great, but they’re not getting worse. He’s a great guy to deal with because he always looks on the bright side.

When she said, ‘I have a tumor in my chest. It’s big and it’s near my heart,’ we started crying.

Going Through Cancer with Her Daughter
Even though she’s got a wonderful guy, a mother’s instinct is to take care of her daughter, go to her treatments, and baby her and I couldn’t at those stages.
We all got through it. I thought she was going to have no energy and be chronically sick to her stomach and she didn’t. She didn’t feel great, but she was strong throughout it while I could barely get off the couch or go up and down the stairs. I don’t know if it was her age or if they did something differently with her.
She started going through all the tests that a donor needed to go through. They were confident she’d be great because she’s healthy, too.
It was Friday afternoon when she had her chest X-ray done. They took her in after the results came out and the doctor said, “You have a tumor,” and it was pretty sizable.
She called me as we were taxiing out. I wanted to know what was going on, but she said, “I’ll talk to you when you come back Sunday,” because she knew I would probably break down.
I thought she was going to tell me she couldn’t be my donor because we didn’t match. When she said, “I have a tumor in my chest. It’s big and it’s near my heart,” we started crying and saying, “This doesn’t make any sense.”
She went through the PET scan and the biopsy of the tumor. We clung on to the hope it would be benign and it wasn’t.
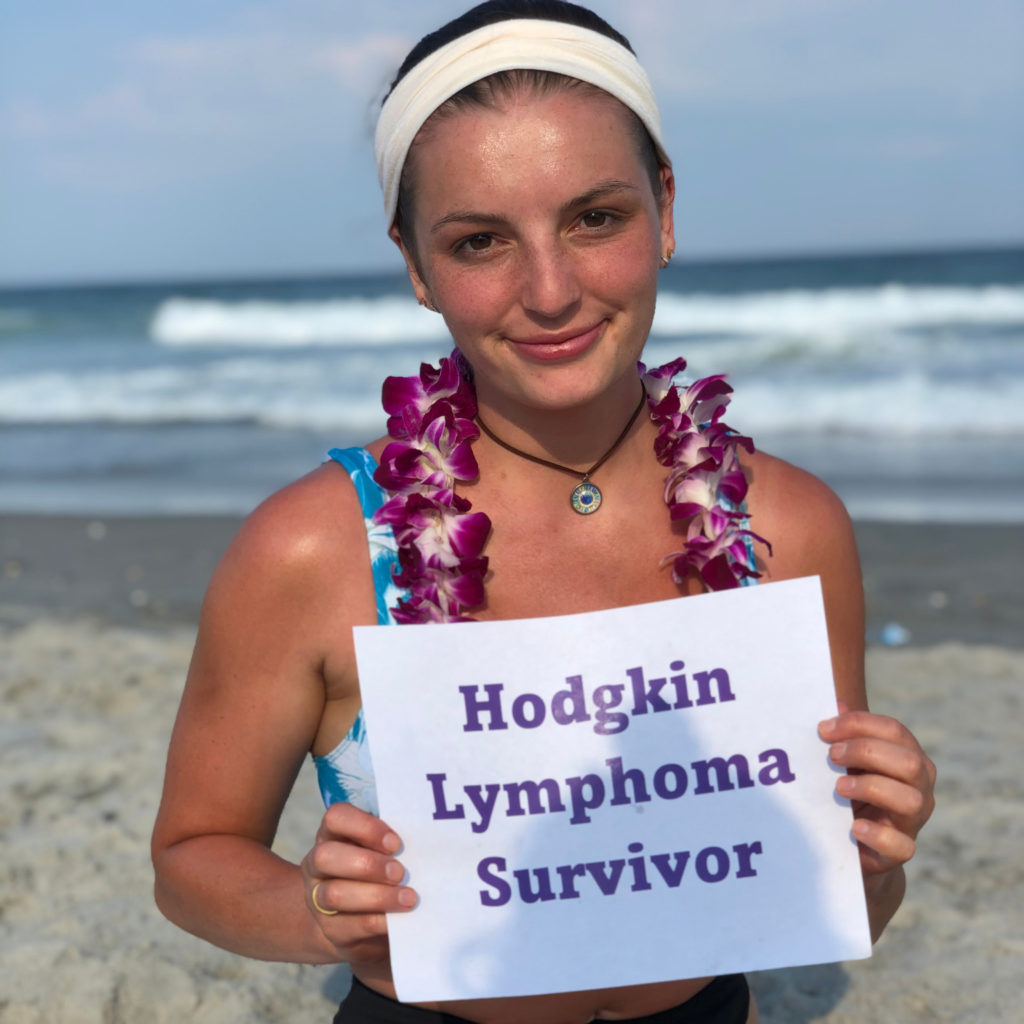
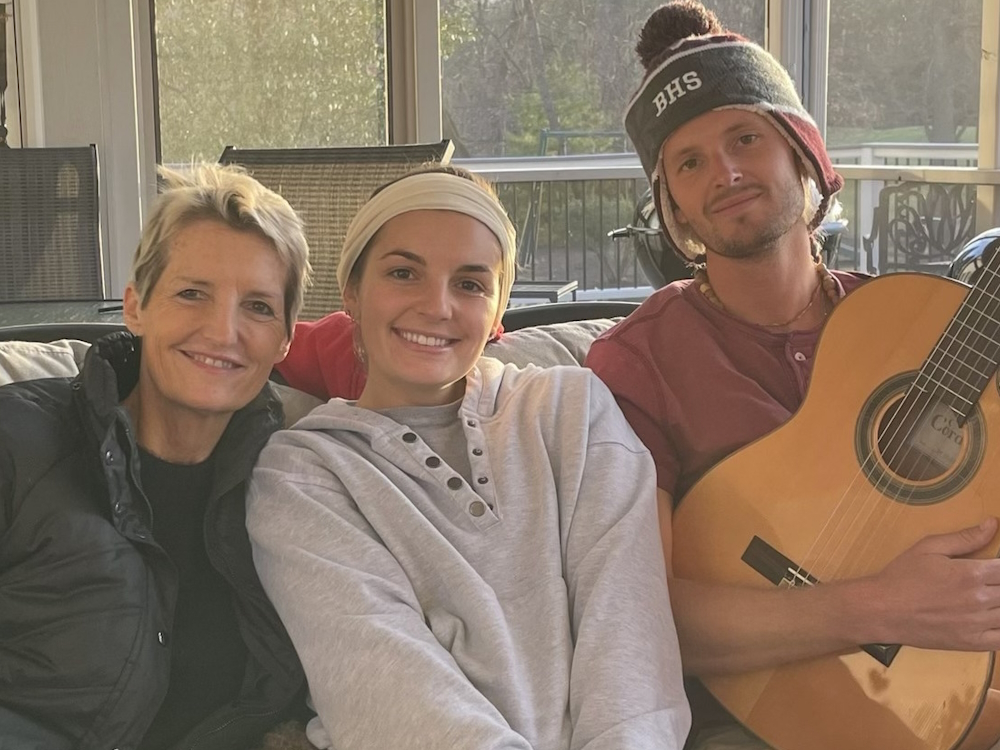
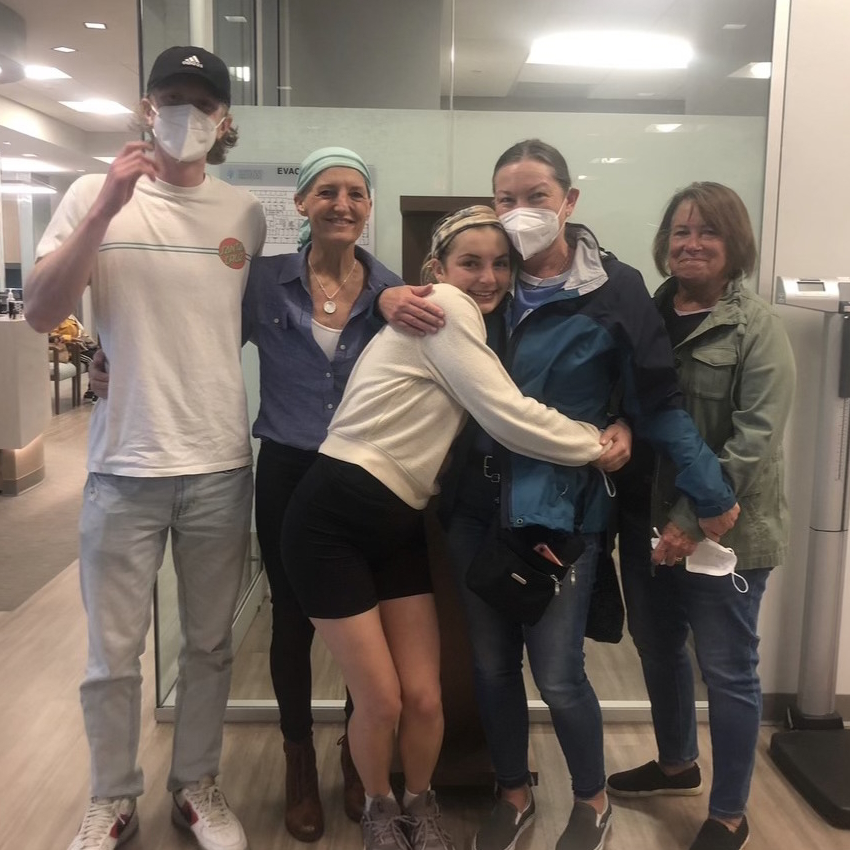
My daughter, who went to Hopkins, didn’t have it affect her as badly. They put her on chemo and she handled it well. She rang the bell and had a cancer-free celebration.


Four months after she stopped chemo, they found a lymph node. They called it hot. It showed up red on the PET scan. She was called refractory because she didn’t respond to chemo.
That was probably the worst part because I thought she was headed towards what I went through, which was hard. She’s 25. She’s supposed to be doing so many other things.
I wanted them to move in with me after she got out of the hospital and they said, “No. We’re adults. We’re going to figure this out our way.” I respect them. They didn’t need me as much as I wanted her to, but that’s a good thing.
She and her boyfriend have a great relationship. They laugh, enjoy themselves, and go for walks. They navigated their way through it. Now we’re in a state of relief. They have a great future ahead of them.
Words of Advice
I rave about Dr. Rapoport because he was positive, but there’s a lot of negativity.
You have to rely on other people to keep your spirits up. Take in all the positives. I had people come over and do puzzles with me. We’d watch Ted Lasso and I’d eat a lot of ice cream. To be without anybody that loved you or cared for you would be dark.
When I was in New York and started running a fever, I called the University of Maryland and said, “Can I come in tomorrow? Because I’m running a fever. I don’t feel that bad. I’m just running a fever and I know you don’t like that.” She said, “Get to an emergency room right now.”
I said, “Why? Why can’t I see you at eight tomorrow morning? I’ll catch the next flight.” She said, “Because the infection could go into your bloodstream.” She said this was an emergency.
I went to the emergency room and, as you know in New York, that took about six hours. They diagnosed me with pneumonia. I went on medication and got over it in a couple of weeks.
You deal with fatalistic people who are the glass is half empty. Find a positive person who points out the good things.


Inspired by Kristin's story?
Share your story, too!
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant