Doug’s Myelofibrosis Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal
Doug shares his myelofibrosis journey after being diagnosed in 2016. He initially experienced fatigue, leading to a series of tests, which included a bone marrow biopsy that led to his diagnosis.
After following a watchful waiting approach, he started treatment with ruxolitinib. However, he continued to experience fatigue and platelet issues.
After extensive reading, he discovered a clinical trial for selinexor. Despite initial hesitation from his local doctor, he joined the trial in November 2019, experiencing positive results. Despite some side effects, like loss of appetite and weight as well as temporarily feeling off, the overall impact on his health has been significant.
Doug, now well beyond the initial life expectancy range, maintains a stable condition, visiting the Huntsman Cancer Institute every three months for follow-up. He emphasizes the importance of being proactive in exploring new treatments and encourages others to explore clinical trials for potential advancements in cancer care.
In addition to Doug’s narrative, The Patient Story offers a diverse collection of myeloproliferative neoplasm (MPN) stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.

Thank you to Karyopharm Therapeutics for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
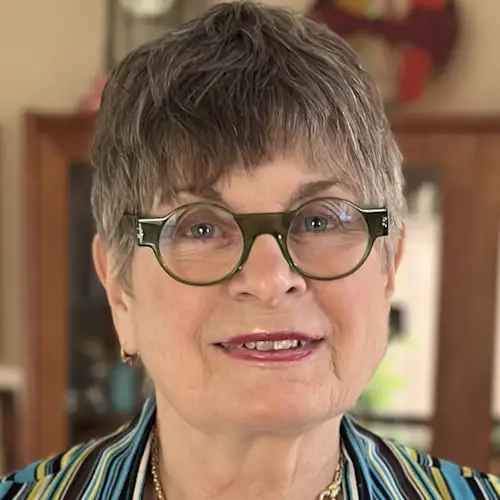
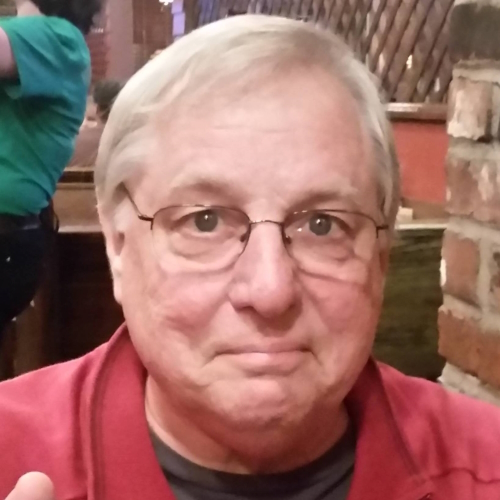
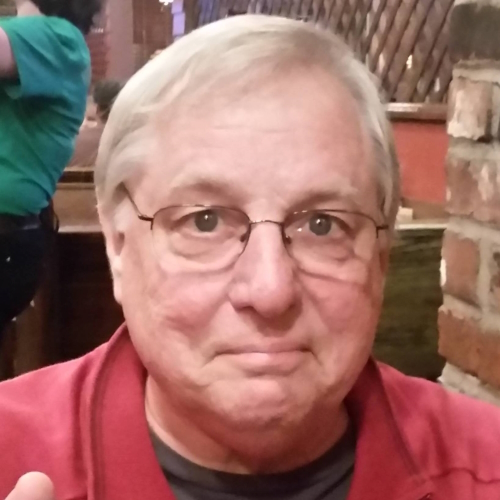
- Name: Doug A.
- Diagnosis:
- Myelofibrosis
- Initial Symptoms:
- Fatigue
- Treatment:
- Ruxolitinib
- Clinical trial: selinexor
Introduction
I was born and raised in Illinois and moved to Idaho for work in the early ‘70s. I love living in Idaho. Before I retired, I was working in Eastern Washington. My wife and I moved back to Idaho to be with family and we live outside of Boise.
I was having trouble with fatigue… When I mowed the lawn, I had to stop and rest because I was getting exhausted.
Pre-diagnosis
Initial Symptoms
I mentioned to my doctor that I was having trouble with fatigue. I noticed that when I mowed the lawn, I had to stop and rest because I was getting exhausted. At first, I didn’t notice it, but it got to a point where I was doing that every time.
I can’t remember what steps he went through with me, but after two or three different tries, he ended up referring me to a hematologist.
Diagnosis
Seeing a Hematologist
When I went to a hematologist in Washington, we went through a series of tests, including a bone marrow biopsy. That’s how I got my diagnosis in May 2016.
It was a shock. It was made doubly so because my wife was diagnosed with breast cancer a couple of weeks away from my diagnosis.
Learning About Myelofibrosis
I knew absolutely nothing. It took me a while to remember the name. They call it a rare disease. You don’t know people who have myelofibrosis. It’s not like breast cancer. Everybody knows somebody who had breast cancer so that’s familiar.
Reaction to the Diagnosis
It was a shock. It was made doubly so because my wife was diagnosed with breast cancer a couple of weeks away from my diagnosis. We were a year into my retirement and getting going with traveling when all of a sudden, both of us had cancer.
Her breast cancer was treatable. It was one of the less aggressive ones so after she had two surgeries and radiation treatment, she hasn’t had to do anything since. She’s clean every time she goes in for an examination.
Learning to live with the idea that I had cancer took a while. Through my reading and thinking about it, somehow your mind comes to terms with it. You can’t have a big open issue like that. You resolve it a little bit at a time. It comes down to it’ll be what it’ll be, but it isn’t necessarily what I would like it to be.
I was not doing that well on ruxolitinib. I had a lot of fatigue. I felt like I was going downhill.
Treatment
Watch and Wait
My disease wasn’t that far along so we decided to do what he called watchful waiting. At the time, there was only one medication, ruxolitinib, and it was not a cure. As long as I didn’t have symptoms that we were going to try to treat, we would wait.
That went on for the better part of a year. In the middle of all that, we moved back to Boise. When I found a new hematologist in town, he prescribed ruxolitinib right away.
Starting Treatment on Ruxolitinib
I was a fairly typical patient. I went through a period where I had very low platelet counts. We had to keep adjusting my dosage because at one point, I went well below 50 and I was having trouble with it. I also had anemia and it had gotten worse. I was on ruxolitinib for probably a year and a half, no more than two years.
I was not doing that well on ruxolitinib. I had a lot of fatigue. I felt like I was going downhill and my platelet counts continued to be a problem.
I wanted to find a clinical trial that I could buy into the idea of what the drug was.
Learning About a Selinexor Clinical Trial
Early on after my diagnosis, I started doing a lot of reading. I subscribed to Google Alerts where you provide keywords and it sends you links to articles with those keywords.
An article showed up from The Salt Lake Tribune and it was from the Huntsman Cancer Institute at the University of Utah. The doctor in the article had a new FDA study that he and his team were initiating. The drug was called selinexor and they saw good results in their clinical studies so they were ready to start a human trial. They described in layman’s terms how the drug worked and what it did.
It was interesting because it was unique and completely different from ruxolitinib. It had been FDA-approved and was used as a treatment for multiple myeloma. It was just a matter of trying to see if it had efficacy with myelofibrosis.
I’ve been grateful for the good fortune I had to read that article. It was a shot in the dark. Something I say to anybody is you don’t know where the answers will come from.
It always amazes me that myelofibrosis is a rare disease. Not many people have it, but it amazes me the amount of effort that the pharmaceutical community is putting into developing treatments. I don’t see how they can come out ahead financially, but I’m grateful for it. I’m all for it. If they’re willing to go for it, I’m willing.
I had gotten familiar enough with my reading. I knew there was only one approved drug that I could have prescribed for me. Now, there are four, but they’re all somewhat similar. They have different characteristics, but they’re all JAK inhibitors. If you’re going to get anything different, it’s going to have to go through a clinical trial first. I wanted to find a clinical trial that I could buy into the idea of what the drug was.
There was another drug in the trial phase with a very different mode of operation. I went to Oregon Health & Science University and interviewed with them at the same time as the selinexor clinical trial. I was considering it, but at that point, I had some issues going on with my kidneys and they wouldn’t accept me because of my kidney function.
As far as trials are concerned, if you want to get the latest and greatest technology, it’s probably the best way to do it. You have to accept that there’s a certain amount of risk. With selinexor, after you’ve been on the drug for a year, nobody knows what the effects are. That’s what they’re trying to find out.
My doctor wasn’t enthusiastic about the idea (of a clinical trial) so that put me in a quandary because I didn’t want to get in a situation where I was running contrary to my doctor’s advice.
Joining the Selinexor Clinical Trial
There was a name and a phone number so I contacted them. They invited me to Salt Lake, which was a six-hour drive. One of the problems I had when I was doing my reading was every time I came across a new drug that was in a trial, it was always in some place like Los Angeles, Houston, or New York. Travel was always a big bugaboo for me, but Salt Lake was doable. I could do a six-hour drive or a one-hour plane flight and be there.
They evaluated me and extended an offer. The doctor said that he could tell that my spleen was large. I didn’t have that much information about my spleen at that point, but his take on the whole thing was that ruxolitinib was not effective for me and the outward evidence was my enlarged spleen.
Oftentimes, we hear people say you need to be your own advocate. It’s not just up to the doctor. It’s up to you to take care of things.
I went back to my doctor and said, “There’s this drug trial that they’re starting at Huntsman and I’ve been invited. What do you think?” He wasn’t enthusiastic about the idea so that put me in a quandary because I didn’t want to get in a situation where I was running contrary to my doctor’s advice.
After a week or two, I got a call from the doctor in Salt Lake and he said, “Doug, are you going to come on the program or not?” I explained to him about my doctor being reluctant about it and he said, “Let me talk to him.” They talked on the phone and after their conversation, my doctor was enthusiastic about it so I said, “Let’s go do it.”
This was in November 2019. I had to get off of ruxolitinib for a couple of weeks before I started. That was an ordeal for me because I quit cold turkey and it was like the worst flu I ever had. I felt bad for a couple of weeks. I felt like I was sinking, but I got through that.
I was feeling the results of the drug and it was all good.
Effects of Selinexor
Within a month or two after starting selinexor, I was feeling the results of the drug and it was all good. I wasn’t keeping a journal but over time, my platelet counts started stabilizing and went up.
My hemoglobin was increasing. I was at 7.8 and my doctor told me that when a patient is 7.5 or less, they start doing transfusions. A lot of myelofibrosis patients live on transfusions. I was steadily getting closer to the territory where I would have to get transfusions.
My blood count took off from 8.7 and after a year or two, my blood count is now 12.5. It’s almost at the low end of the normal range. My platelets are in the 250 range. My hemoglobin varies somewhere between 12 and 12.5.
My white blood cell count was one of the early indicators at the very beginning. The counts were high and in the normal range, but they were at the high end of the range. The doctor noticed that they were consistently high.
White blood cell counts vary quite a bit in normal people, but mine were always at the high end of the range. I never go out of the range, but the white blood cell counts for me are high.
My anemia has been solved in the last two years that I’ve been on the drug. When I do monthly blood draws, my hemoglobin and my red blood cell counts are in the normal range, my white blood cell counts are at the high end of the normal range, and my platelet counts are in the middle of the normal range.
Before I started the selinexor clinical trial, I bought a walker because I was having so much trouble with fatigue that I wasn’t taking walks. I didn’t want to go on a walk somewhere and be exhausted. She suggested I get a walker with a seat. That way, I could park myself for a time and get my energy back.
I haven’t used that walker ever since I started the selinexor clinical trial. I’ve loaned it out to friends a couple of times. I can’t say that my energy level is the same as it was before I received my diagnosis. It’s not quite the same, but I still can go out to take a half-hour walk and it’s not a big deal for me to do that.
Because the anemia went down, my energy levels have gone up. I take selinexor once a week. We’ve adjusted the dosage. When I first was on the selinexor clinical trial, I was taking 80 mg. Now that the initial trial period is over, the doctor adjusted my dosage to 40 mg.
What’s different about being on a trial is you don’t know what to expect over time.
Side Effects of Selinexor
The problem I have gotten into with selinexor is my appetite and maintaining my weight. I’ve lost 85 or 90 lbs. It was over a year or two, but it was still a significant weight loss. It was due almost entirely to the fact that selinexor took away my appetite.
The doctor gave me different medicines to try to counteract that problem. I still take one pill daily. Food doesn’t appeal to me like it used to. When I sit down at dinner, I invariably look at my plate of food and think I don’t want to eat, but once I get started, I can finish my meal. This comes from my experience and dealing with the change.
That’s been the only hard part of being on selinexor. My doctor tried to find a dose where I would quit losing weight and maintain a stable weight. I’ve been at this dosage level for a long time. I seem to be in a place where it’s still effective but I’ve stopped losing weight and can better maintain it.
I weigh myself every day. I have heart failure and they want me to weigh myself every morning. They’re looking for weight loss as an indicator of an event, but that’s been pretty stable for a long time.
Another thing that I have to put up with is selinexor puts me in a mode where I feel off. I take the drug on a Wednesday and it’s not until Saturday or Sunday before I feel completely right again. Sometimes it’s like having the blues. Sometimes it’s not feeling quite right, but it’s never intolerable. It isn’t like I lay around and writhe. No pain goes along with it, but it’s part of what I have to put up with.
What’s different about being on a trial is not knowing what to expect over time. The doctor and I have talked a couple of times about that. I was the fourth person on the selinexor clinical trial so nobody with my disease has been on the drug for that long. The doctor said at the end of the day, maybe the main thing that comes out of this is that we’ll have a drug that will arrest the progress of the disease.
I got something that works and it doesn’t seem to be fading out on me.
Current Status
I don’t feel like I’m gaining or losing. I know that my status has improved greatly. I don’t seem to be going any further up but neither am I going down. I’m maintaining a good normal.
There’s not a lot you can do. I was first diagnosed in 2016. I’m already beyond the range of what they say the life expectancies are, which is often a mid-range of about 5 to 5 1/2 years. I’m already beyond that and I feel good.
I know that a lot of cancer treatments only last for a time. Somehow, the cancer adjusts to them and they lose their efficacy. I had a sister-in-law who had breast cancer. She came in and moved in with us in her final year. They were constantly coming up with a new treatment. But 3 or 4 months later, she’s right back where she was again until she finally got to the point where she said no more and she passed.
Cancer treatments tend to have a limited period of effectiveness. But this one, because it has such a unique method of operating, doesn’t seem to have that same life expectancy so I’m grateful for that. I got something that works and it doesn’t seem to be fading out on me.
It was my good fortune that the selinexor clinical trial worked out well for me and was doable from the standpoint of the travel.
Traveling to Clinical Trials
The biggest bugaboo in the clinical trial process is the fact that it’s such an isolated condition. There are a handful of hospitals, most of which are associated with a university. It logically makes sense that that’s where these trials would be centered, but it sure leaves a lot of people out.
I’ve talked to a number of people over time. Somebody who lives in Idaho, Montana, or somewhere similar doesn’t have any way to commit to the travel. I know people who get on a plane to go to Los Angeles because that’s where the trial is.
I get a certain amount of reimbursement for travel down to Huntsman from the University of Utah. As I recall, their accounting people figured out a rate per mile. I get a check for a little over $200. But all of that is predicated on the fact that Salt Lake is relatively close to where I live.
For me, driving down to Salt Lake was doable. One way or another, I was going to make it happen. It’s a few hundred bucks to go down there, spend the night, and come back the next day. I’ve since found that it costs me about the same to take a plane because I can go in the morning, come back in the afternoon, and I don’t have to stay overnight.
They reimburse me based on the mileage of driving back and whether I drove or not. Flying is a little more expensive. But at the end of the day, it’s a difference of a couple hundred bucks. It’s not that big of a deal. It was my good fortune that the selinexor clinical trial worked out well for me and was doable from the standpoint of the travel that was required over three months.
Follow-up Protocol
I go once every three months. I do blood tests and sampling. They take a certain amount of blood for research and a certain amount for monitoring my health. I visit with a nurse and doctor. They’ve been good people to work with.
I encourage people to be open and moderately aggressive in looking for new things that are out there.
Words of Advice
Cancer is a nasty animal. We’re learning more and more about it all the time. It’s more and more getting to be a condition that can be solved. I look at selinexor knowing that it’s not a cure, but it seems to be holding me steady enough that over time, maybe there will be a cure.
I would expect there will be one at some point in time. Somebody will figure something out. If I die two months before that gets decided, it doesn’t do me any good, but this way, at least I give myself a chance to take advantage of new developments.
I encourage people to be open and moderately aggressive in looking for new things that are out there. There are new trials that are starting all the time.
There’s a new selinexor clinical trial that’s going into phase 3, I think, which means it’s well on its way to being an approved drug. They’re doing it in combination with ruxolitinib. I’m on selinexor alone. I don’t know what ruxolitinib adds to it, but if it works, it works.
Based on my experience, there’s a lot of safety built into the process. I had the benefit of selinexor being tested for other cancers before it came to me. Some questions on safety had already been answered with other drug trials. It made it a little bit easier for me to make a decision.
Don’t think that it’s dangerous and you’re out there all by yourself. There’s a whole network of knowledgeable people who are supporting and running these programs. They don’t want to have a failure in me any more than I want one.

Special thanks again to Karyopharm Therapeutics for its support of our independent patient education content. The Patient Story retains full editorial control.
Inspired by Doug's story?
Share your story, too!
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant