What Myelofibrosis Taught Demetria About Showing Up for Herself
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal
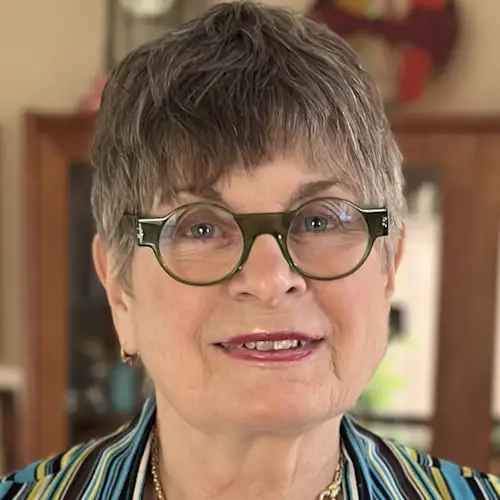
In a heartfelt and powerful conversation, Demetria, a resilient businesswoman, opens up about her experience with myelofibrosis, a rare blood cancer, and how it reshaped her life in the most unexpected ways.
From the outside, she was the glue — supportive, successful, always encouraging others. But behind the scenes, a wave of unrelenting fatigue had crept into her life, something deeper than just being “tired.” It took persistence and self-advocacy for her concerns to be taken seriously by her doctor, and soon, she found herself face-to-face with an oncologist and an unfamiliar word: myeloproliferative neoplasm.
Initially diagnosed with essential thrombocythemia (ET) due to the JAK2 mutation, she navigated treatment with courage, resilience, and a lot of unanswered questions. Her mental strength carried her through the confusion, and her spiritual grounding gave her clarity when facts didn’t. Despite feeling isolated in her diagnosis, she remained inquisitive and proactive, seeking second opinions and trusting her instincts.

As her condition progressed into myelofibrosis, the reality hit harder. Her body stopped producing blood cells. She found herself in complete bone marrow failure and urgently needed a bone marrow transplant. What followed was a deeply emotional and spiritual experience marked by weekly blood transfusions, a life-changing phone call from a donor registry, and a renewed sense of purpose.
What stands out is not just her diagnosis, but the quiet power with which she faced it. She never let fear define her. Instead, she leaned into her faith, stayed curious, and used the waiting period to advocate for more African Americans to join the donor registry — a crucial step, as she learned how underrepresented Black patients are in the system.
Demetria’s story isn’t just about myelofibrosis; it’s about mental wellness, feeling seen, and finding peace even in uncertainty. She openly shares the importance of prioritizing health, listening to your body, and staying grounded in what truly matters — family, purpose, and presence.
Now thriving post-transplant, she’s working on launching a nonprofit that supports awareness and self-care for entrepreneurs and communities impacted by myeloproliferative neoplasms. She’s proof that healing is as much about inner peace and support systems as it is about medical treatment.
Watch Demetria’s video to find out more about her story:
- What happened when a mystery illness was something she never expected?
- How she turned a cancer diagnosis into a platform for life-saving advocacy.
- From weekly transfusions to spiritual clarity, how she shifted her perspective.
- Learn how one woman brought her daughter into her healing process in the most touching way.
- Why she says “feeling good” means more than “looking good” and how she got there.
- Name: Demetria J.
- Age at Diagnosis:
- 41
- Diagnosis:
- Essential thrombocythemia (ET), later progressing to myelofibrosis (MF)
- Mutation:
- JAK2
- Symptoms:
- Extreme fatigue
- Stomach pain (later identified as due to an enlarged spleen)
- Dizziness
- Shortness of breath
- Treatments:
- Spleen-shrinking medication
- Regular blood transfusions
- Bone marrow transplant

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
- Introduction
- Red Flags I Noticed Before My Diagnosis
- Meeting My First Oncologist
- Getting a Second Opinion
- My Reaction to the Essential Thrombocythemia Diagnosis
- Educating Myself on Treatment Options
- Possibility of Disease Progression
- When I Started Feeling Symptoms Again
- Feeling Worsening Symptoms
- Going to the Emergency Room
- Finding Out I Have Myelofibrosis
- My Reaction to a New Cancer Diagnosis
- My Thoughts on Needing a Bone Marrow Transplant
- Finding a Match
- Undergoing Regular Blood Transfusions
- Preparing Myself for the Bone Marrow Transplant
- My Life After Transplant
- Educating People About Myeloproliferative Neoplasms (MPNs)
- My Advice About Paying Attention to Your Body
- My Advice About the Mental and Emotional Side of a Cancer Diagnosis
I started experiencing extreme fatigue. When I would get home… I wanted to go straight to bed.
Introduction
Those closest to me would probably say that I’m their biggest cheerleader. I have been gifted with the ability to encourage people and give them a little extra boost when they may feel like they can’t do something or are going through a certain situation. I have a unique ability to give a different perspective on things. A lot of times, I’ve heard people even describe me as a silent strength. Even though I can speak to people, I’m not very vocal. I may not talk a lot, but when I do talk, I use my words in a meaningful way.


Red Flags I Noticed Before My Diagnosis
I have been a business owner for over 15 years. I was also working with an organization that works with kids, trying to get them into high school. On top of those, I was doing a lot of traveling. I was busy all the time.
I started experiencing extreme fatigue. When I would get home, I would normally tend to our daughter, who was very young at the time. I would fix dinner and hang out around the house. Instead, I wanted to go straight to bed, and that’s why I knew this was a different kind of tired. I didn’t even have the energy to do anything except go straight to bed.
When it was time for my routine check-up with my physician, I mentioned to him that I’ve been tired. At first, he brushed it off. He said, “Well, you do a lot.” I told him it was a different kind of tired. He said, “We’ll run some extra blood work to check your nutrient levels. Maybe you’re low in B12 or something,” but that was not the case.
After a couple of days, while I was driving, the doctor’s office called. The nurse said, “Your blood work came back, and your doctor is sending you to an oncologist.” I said, “Wait. Hold on. Let me pull over.”
I pulled over into a parking lot and said, “Did I hear you correctly? You’re referring me to an oncologist?” She said yes. I asked why. She said, “Your platelet counts were extremely high. They were in the millions.” I asked her what that meant. She said, “We’re not quite sure. That’s why he’s referring you to an oncologist.” The journey began from there.
I took the medication for about a year and a half, and started feeling much better, to the point where my numbers started leveling out.
Meeting My First Oncologist
When I got home, I went online, like most people do. I searched, “high platelets, what does that mean?” It gave me different things. The first thing most oncologists want to do is a bone marrow biopsy to figure out what’s going on in the marrow. She said, “I think this is what it is.”
One of the things that was a little alarming for me at that time was when she said, “You’re fairly young and most of the time, we don’t see this present in people of your age.” In that moment, I didn’t feel like there was more that she was willing to do.
One of the things she asked was, “Do you and your husband still want to potentially have another child?” I said yes because at that time, I was in my mid-30s. I didn’t feel like she wanted to explore any other options because I was a unique case.

Getting a Second Opinion
I ended up at Emory Hospital in Atlanta. At the time, the oncologist there felt as if I would do better on another medication that was fairly new to the oncology world. It had recently come out of a clinical trial, but it was showing very positive results. He said, “I think you would fare better on this,” so that’s what I did.
I took the medication for about a year and a half, and started feeling much better, to the point where my numbers started leveling out. The platelet counts had gone down to the normal range. That was one of the things that he was hoping for.
The clinical trial findings had shown that some individuals were able to get off the medication and their bodies were able to sustain themselves, and that’s where I thought I had ultimately landed until the next journey began.
No one could give me an answer. I was feeling frustrated because I didn’t understand how this could happen.
My Reaction to the Essential Thrombocythemia Diagnosis
When I was young, my mother had leukemia. She was with me at the doctor’s appointment that day, and our initial thought process was whether it was hereditary and potentially came from her. They said it typically wasn’t how it works. I found out that there was a JAK2 mutation in my blood that was causing the essential thrombocythemia (ET) to happen.
I had a lot of questions. I was very inquisitive. How does this happen? How do you get the mutation? It was a little frustrating because I couldn’t get any direct answers. Ultimately, they landed on I was born with this mutation.
If I were born with this mutation, why did it express itself at this point in my life? What made it express itself? If it’s been in my DNA this entire time, why did it express itself at this time? No one could give me an answer. I was feeling frustrated because I didn’t understand how this could happen.


Educating Myself on Treatment Options
In your mind, you just want to survive and get better. I didn’t lean too heavily into what the complications could be. I know that if I read too much into all of those things, it could create a roadblock for me because my mind would shift to these other things, so I didn’t want to go down that road.
Our insurance wouldn’t pay for the medication. Thankfully, we found an organization that provided financial assistance. The medication was over $1,000 a month, but even so, my husband and I were prepared to do whatever we needed to do to afford it so that it could improve my quality of life.
Our insurance wouldn’t pay for the medication… my husband and I were prepared to do whatever we needed to do to afford it so that it could improve my quality of life.
Possibility of Disease Progression
There wasn’t any tracking, but I was made aware that there could potentially be a progression of the disease. Once I was a year out and feeling well, everything seemed okay. Honestly, it never even crossed my mind that something worse could come down the pipe. I went back to living life and jumping into entrepreneurship and my family. I wasn’t looking back.
When I Started Feeling Symptoms Again
Once again, fatigue was the biggest presenting symptom. I also experienced stomach pain. Looking back, that was my enlarged spleen that was causing the pain in my stomach, but I thought they were two isolated things. Neither one of them meant that I had cancer. I thought they were independent of each other, so I kept going on and diagnosing myself of what I thought was going on until it became too much to bear.


Feeling Worsening Symptoms
I developed dizziness. About two weeks before the actual diagnosis, I started getting dizzy. Two main events made me think that something was going on. My husband and I were at a track and field day with our daughter. We had to walk quite a distance from the parking lot to the bleachers, and I was struggling with my breathing and dizziness.
We were towards the end of the year, so I wanted to buy my daughter’s teacher a thank-you gift. I was in line at the store and felt like I was going to pass out. I told the cashier I was going to leave my stuff and go to the car for a minute. I took dimenhydrinate because I thought I was going to have vertigo. I was sitting in the car for about 10 minutes and thought I’d try again.
I went back into the store and I seemed to be okay. I get back in line then I start to feel it again. I jokingly said, “I’m in a big hurry. I’m not trying to rush you, but can we speed it up?” She was extremely nice; she was talking and taking her time, but I felt like I was about to pass out.
I got back in the car, called my husband, and told him I might have to go to a walk-in clinic or somewhere the following day because I was still getting dizzy.
‘All your blood levels are dangerously low. I don’t even know how you’re functioning.’
Later on, I had a sharp pain in my stomach again, so I thought something was up. The next morning, I get up to find out what time the clinic opens because I want to be the first person in.
That morning, I wasn’t dealing with any dizziness. It was the pain in the stomach that was presenting more that day. I thought I might have bacteria in my stomach. I go to the clinic and explain the symptoms to the doctor. She said, “We’ll test you for H. pylori and make sure you don’t have that, but let’s run some blood work to rule out anything,” which was the best thing that she could have ever done for me.
She called me the next day and said, “Your labs came back and all your blood levels are dangerously low. I don’t even know how you’re functioning. You need to go to the emergency room right now. They’re probably going to give you a blood transfusion. I’m emailing you your lab work so you can show it when you get there. They will figure out what’s going on because I’m not quite sure, but something’s going on.”


Going to the Emergency Room
My husband brought me to the ER and my mom drove up from Georgia to be with me. Thankfully, they were very attentive when I showed them the lab work that the doctor emailed me and they immediately took me back. They initially went down the track of gastroenterology. They said, “We’re going to draw some more blood to see for ourselves.”
After the lab work, the doctor came back in and blatantly said, “No, this is cancer.” My mom, my husband, and I were looking at each other. One of the oncologists whom I previously saw was on call at the ER that day. When the doctor on call was saying that this was cancer, she said his name and when I told her I knew him, she came to get him. He comes in, remembers me, and takes over my care completely.
Finding Out I Have Myelofibrosis
He transferred me to another hospital that he felt would be able to serve me better. He ordered the bone marrow biopsy. He came back and said, “It’s myelofibrosis.” He immediately put me on the national donor list. He informed me that he feels like I need to have a bone marrow transplant to live.
I was in complete bone marrow failure at that point. My body was not making any blood cells at all and that’s why my blood levels were so dangerously low. Every day, old cells die off and your body generates new cells, but mine were dying off and nothing was being generated. Until they found me a donor, I was going to have regular blood transfusions to keep my body going.
They noticed how calm I was. There’s no other way to describe it except for the peace of God.
My Reaction to a New Cancer Diagnosis
Surprisingly, I was very calm. I ended up staying in the hospital for five days after going to the ER. I called family and close friends, and when they came to visit, they noticed how calm I was. There’s no other way to describe it except for the peace of God. I had a peace that I only know came from Him because I knew that it was serious, but it didn’t rattle me. It didn’t make me feel hopeless. I felt that I’ve been through ET, so I can make it through this one.
One night, when I was in the hospital by myself, I was lying in bed and talking to God. I was saying, “Okay, we’re going through this,” and I feel Him say to me, “You’re not going to die. It’s bigger than you.” I didn’t quite understand what it meant in that moment, but it gave me something to hold on to. Even at times when I felt like I was going to die, I said, “Nope. He said I’m not going to die, so I’m not. It’s going to be okay.”


My Thoughts on Needing a Bone Marrow Transplant
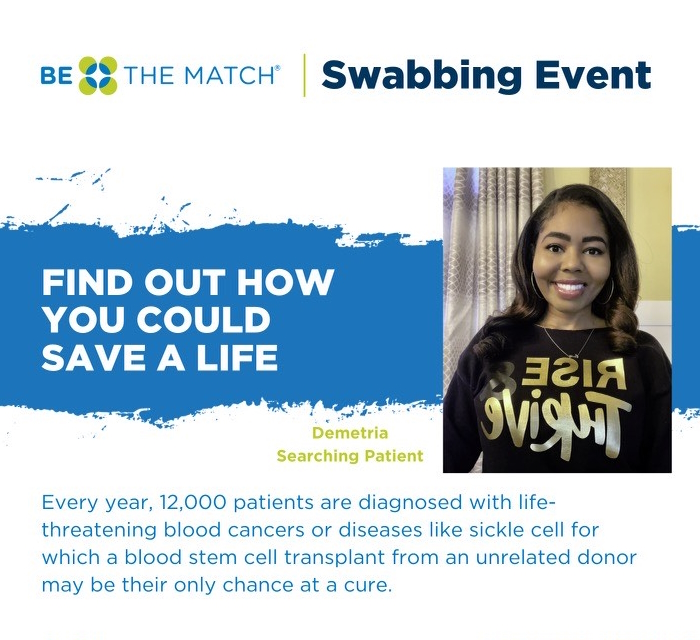
When they said they were putting me on the national donor list, I thought it was great until I had a visit with the transplant surgeon. He said, “We are very hopeful that you can get a donor, but African Americans make up the lowest percentage on the national registry. Because of that, your chance of finding a donor is a longer stretch. It could potentially be two to three years because we don’t have enough pool of people to pull from.”
That stopped me in my tracks because you have this hope that you can get a donor, but you find out the chances are very slim based on the statistics. I asked him, “What can I do to help? How do we get more African Americans or Blacks to sign up to get on the registry?” He said, “Be The Match. You would probably have to contact them,” and that’s exactly what we did.
We contacted them to figure out how to hold donation drives to increase the number of individuals on the registry. That became part of my focus. Honestly, I think that helped to keep me from thinking about the other things because my focus shifted. How can we increase the number of African Americans on the registry so that if another person has this diagnosis, they don’t have to face the fact that there are only 29% of people to pull from?
To hear that they found me a donor was unbelievable.
Finding a Match
By God’s grace, two and a half months later, I received a phone call. My husband and I were sitting on the couch. You know how sometimes you don’t answer unknown numbers because you think it’s spam? By this time, I’m answering every phone call regardless of whether I know the number or not, because I don’t know who it could be.
An unknown number called and I answered it. She confirmed that it was me on the phone and said, “I think we have potentially found a donor for you.” My mouth flew open. I put her on speakerphone so my husband could hear her.
It was a surreal moment. In my head, I had two to three years. To hear that they found me a donor was unbelievable.

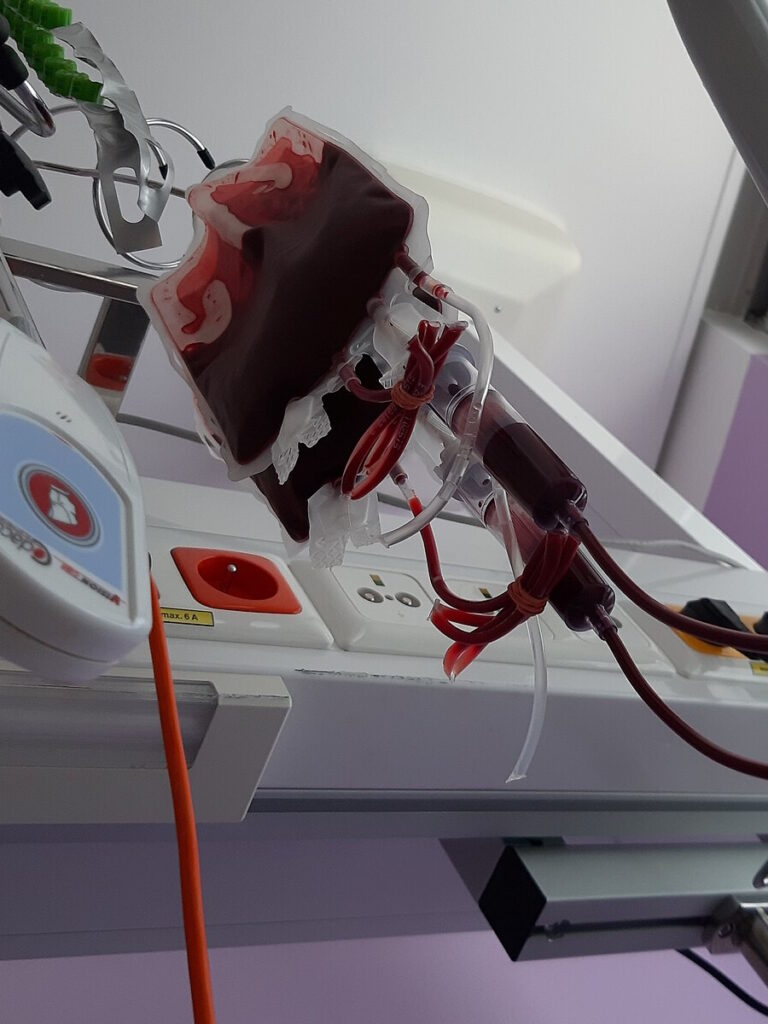
Undergoing Regular Blood Transfusions
A year prior, my oncologist had moved to where I lived, so he knew all of the transplant surgeons and was in direct contact with them. They were walking him through my protocol. They immediately wanted to shrink my spleen, so they put me on a medication to help shrink the spleen and ease some of the symptoms from myelofibrosis. That was a big help in addition to going every 7 to 10 days for transfusions.
The transfusions improved my quality of life. Typically, the day after a transfusion, I would wake up and feel better. Their goal was to keep my hemoglobin level above seven, which is still low, but I felt wonderful coming from a four.
When I would go see the oncologist, they would check my blood levels and send me to have a transfusion. I pretty much knew that I was going to get a transfusion every week. I made friends with all the staff. It wasn’t as sad as people may think because even though my life revolved around being in a doctor’s office or a hospital every week, I still got to interact with people. This was my new normal.
We were praying that my donor wouldn’t think it’s too much and back out.
Preparing Myself for the Bone Marrow Transplant
My husband and I prayed for my donor because they say potential until you get close enough to where everything is solidified. Potential means that they’ve located the donor and reached out to them, and they agreed, but there are several more steps that the donor has to go through.
I didn’t know that all of the pre-testing that I went through, my donor also went through, so I thought that the donor was a selfless human being to go through all of that for a stranger. We were praying that my donor wouldn’t think it’s too much and back out.
Once we got close enough to the point where it’s final and I’m having the transplant, my hair was extremely long. Our daughter was 10 years old at the time, so she didn’t fully understand everything because we wanted to shield her from some of the details. I told her, “Mommy’s going to lose her hair.” She was saddened by that because she loved to play with my hair.
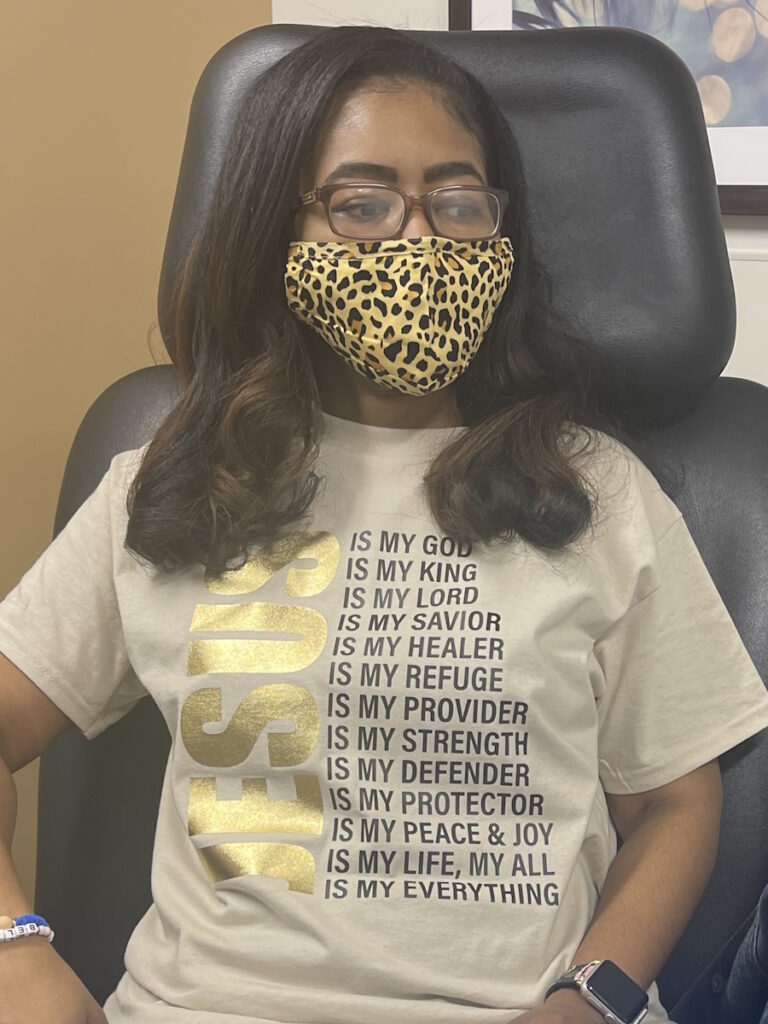

I thought, “How do I bring her into a part of this?” I allowed her to cut my hair before going to have the transplant. We recorded it and shared it on social media. It had a huge number of views and shares. I began to understand what God meant when He said it was bigger than me. I met so many incredible people through social media.
I brought her into it so that she could feel like she was a part of it. I knew that I was going to lose my hair. It softened the blow a little bit to see a shorter amount leave your head than long strands. Mentally, that’s how I prepared myself for losing all my hair. Outside of that, I decided I have to be present every day and show up every day ready for the journey.
My experience taught me to reprioritize my life… If you don’t take care of yourself, then nothing else can thrive.
My Life After Transplant
My experience taught me to reprioritize my life. I was a busy bee. I was everywhere doing everything. All good stuff, but sometimes, something like this stops you in your tracks. It completely slowed me down. I had time to reflect on what things are most important.
When you’re lying in bed, you’re not thinking about customers; you’re thinking about your family and your loved ones. They’re most important to me. It redefined how I show up and what matters to me the most. How am I going to live my life from this point forward? It changed everything.
It’s so funny because when I see people out, they say, “You look so good!” I always say, “Thank you, but I feel so good.” Feeling good is better than looking good. They always laugh because I appreciate that I look good, but I appreciate most that I feel good.
I didn’t even know that this is how I was supposed to feel because it became a normal feeling, the way I previously felt. I thought that what it was like as a busy person, not understanding fully that it wasn’t having a good quality of life, even though externally you had a lot of good things. I succumbed to the fact that that’s how you feel when you’re busy. I’m amazed because I didn’t even know that this is how I was supposed to feel.

Educating People About Myeloproliferative Neoplasms (MPNs)
I’m hoping to create a nonprofit where I can continue some of the efforts that we were doing. I paused the transplant to regain my health and get things in order.
Now I feel like I’m at a place where I can embark on something a little bit bigger. I do think it’s important, especially around entrepreneurship and business owners. A lot of us wear so many hats that tons of us do exactly what I did. We keep going. We keep showing up for our businesses and our customers, but we don’t necessarily show up for ourselves.
I want to work on how that looks, where I can encourage business owners and entrepreneurs. I understand the hustle. I understand that a lot of times, that’s what it takes to get your business off the ground. But you are the most valuable person in that thing. If you don’t take care of yourself, then nothing else can thrive.
Take a step back and look at what you’re doing for yourself.
My Advice About Paying Attention to Your Body
It’s not selfish to take care of yourself. The first law of nature is self-preservation, which we violate all the time. We put other things and other people ahead of ourselves. If we aren’t well, then we can’t be well to anybody else.
When you shift that perspective about life and how you show up, then you will prioritize your health. You will prioritize being good to yourself. We’re all guilty of that to some degree, but I hope that in sharing my story, it would inspire people to look beyond what it is that you’re doing for others, take a step back, and look at what you’re doing for yourself.
A lot of times, when I wanted to go to doctor appointments and do certain things, I would say, “Oh, but my clients are going to be so disappointed if I have to cancel them.” If I’m not here, that’s going to be more devastating than me having to cancel on her. Look at life a little differently. Are you taking care of yourself? Take care of yourself first.


My Advice About the Mental and Emotional Side of a Cancer Diagnosis
You have to remain hopeful. Hope is what you can hold on to when everything else feels like it’s slipping through your fingers. Hope anchors you to the possibility of living on the other side of this thing. When you lose hope, then you have nothing. Hope is the foundation.
People say, “How do you have hope when it looks so daunting?” I had to shift to gratefulness. Gratefulness was another key piece that helped me to remain hopeful.
Nobody’s grateful for a diagnosis, but I was grateful that there was a solution at hand. I was grateful that there were people who were willing to do whatever they needed to do to help me on my journey. When you begin to be grateful amid the storm, that’s where hope can start to shine its head a little bit.
It could have been a lot worse. I don’t know how worse it could get, but it could have been. Hopefulness is what anchors you to the possibility of more.
Stress can be a silent killer as well. Stress probably undergirds most diseases and diagnoses. Make sure that as you navigate through life, you check on yourself. Am I carrying too much? Am I worrying too much?
With the current state of things, people are worried about whether they can afford food or housing. At the end of the day, your life is the most important thing. Even when things are tight and it feels like you don’t have enough, the worry and the stress will do more than not having enough.
Remain hopeful. Hope is what you can hold on to when everything else feels like it’s slipping through your fingers.

Inspired by Demetria's story?
Share your story, too!
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant