Cathy’s Myelofibrosis Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Cathy was diagnosed with myelofibrosis after a routine blood test.
After her husband retired, she encouraged him to do a blood test with her to get a sense of their health status. Her husband’s blood test results turned out normal while hers showed a low platelet count and teardrop-shaped red blood cells.
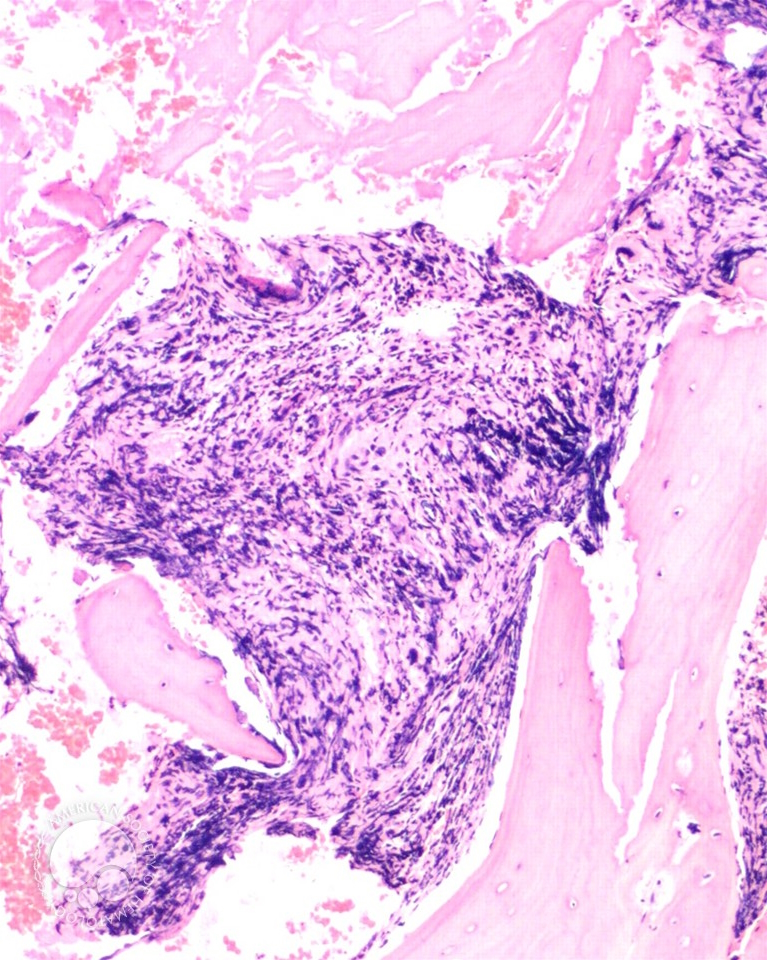
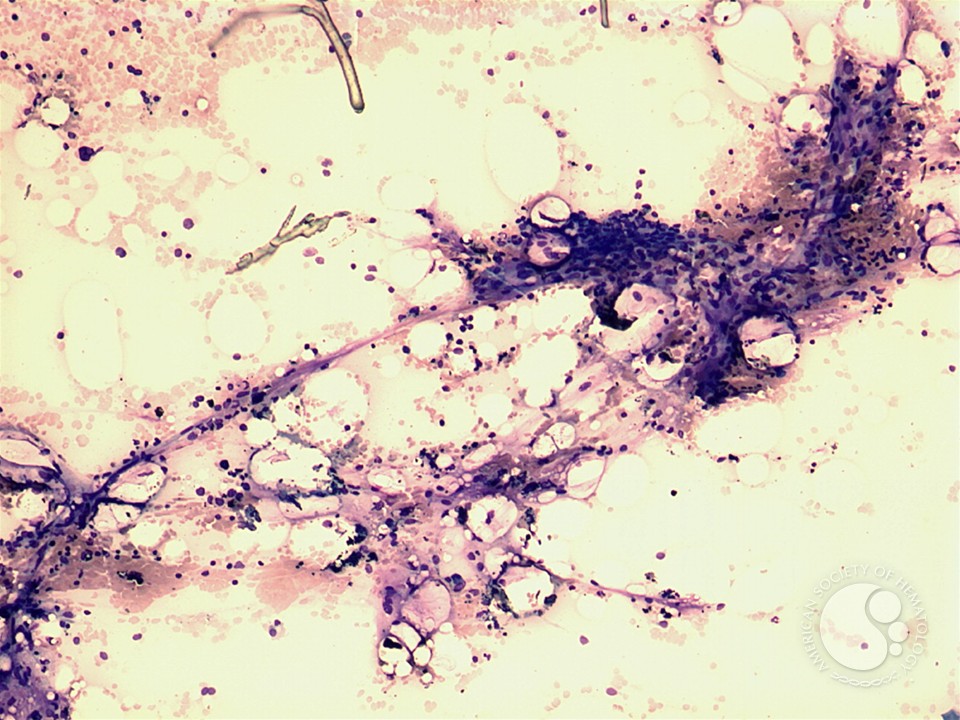
She later got a spleen ultrasound, which revealed a slightly enlarged spleen measuring 18 cm, and a bone marrow biopsy, which revealed myelofibrosis. Her myelofibrosis story includes a stem cell transplant, clinical trials, support groups and GvHD.
In addition to Cathy’s narrative, The Patient Story offers a diverse collection of MPN stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Cathy T.
- Diagnosis:
- Myelofibrosis
- Initial Symptoms:
- None; caught at a routine blood test
- Treatment:
- Stem cell transplant
- Introduction
- Pre-diagnosis
- Diagnosis
- Treatment
- Follow-up protocol
- Community support
- Words of advice
- Clyde’s Caregiver Story
- What do you remember from the first time you saw Cathy?
- What do you like doing together?
- Reaction to Cathy’s blood test results
- Understanding myelofibrosis
- Impact of a life-threatening disease
- Caregiver’s role in the fight against cancer
- What was the biggest surprise, lesson, or difficulty for you?
- Not taking care of one’s self
- Early signs of caregiver burnout
- Differing perspectives between patient & caregiver
- Advantages of patient education
- Words of advice
- Importance of diverse community support
Introduction
I’m originally from Shanghai. I came to the US in 1990.
I’m married with a 19-year-old son and a 32-year-old stepdaughter who lives in L.A.
I worked in insurance for the last 19 years. My husband and I both did, but he did for a lot longer. I was a product manager and worked on the IT side, making sure my business had a robust and stable system.
I like running outdoors, working out, and doing weights.


Pre-diagnosis
Routine blood work
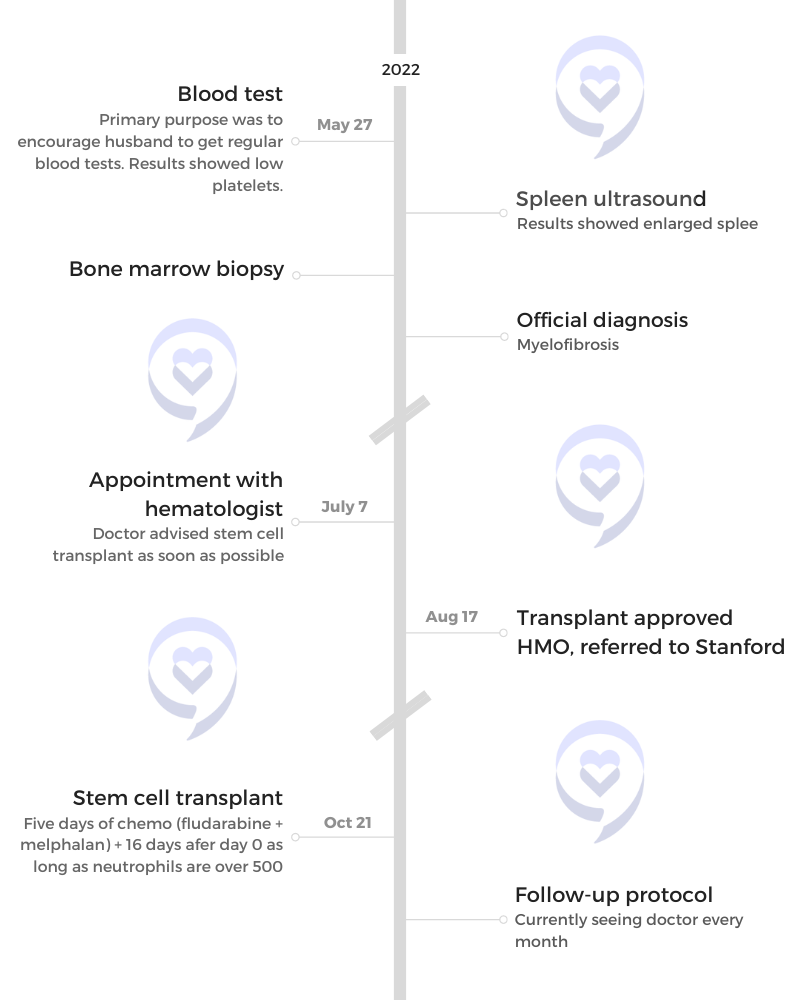
When my husband retired, I said, “Let’s go get a blood test,” because he doesn’t like to know about those numbers. His numbers came back all normal and mine was pretty much all normal except for the platelet, which was in the 50s. I didn’t understand it. I know it’s lower than the lower limit.
A couple of days later, my primary care physician from Kaiser emailed me, and said, “I want you to get a spleen ultrasound.” I wondered why. I did the ultrasound and my spleen is 18 cm. Then that’s when I started Googling and found out that 18 cm is 50% larger than normal so there must be something wrong with me.
I Googled it right away. What’s the purpose of a spleen ultrasound and what happens if it’s a certain size? I have a general idea why before I went in and when I got the result, it just confirmed my suspicion that it had something to do with a blood disorder.
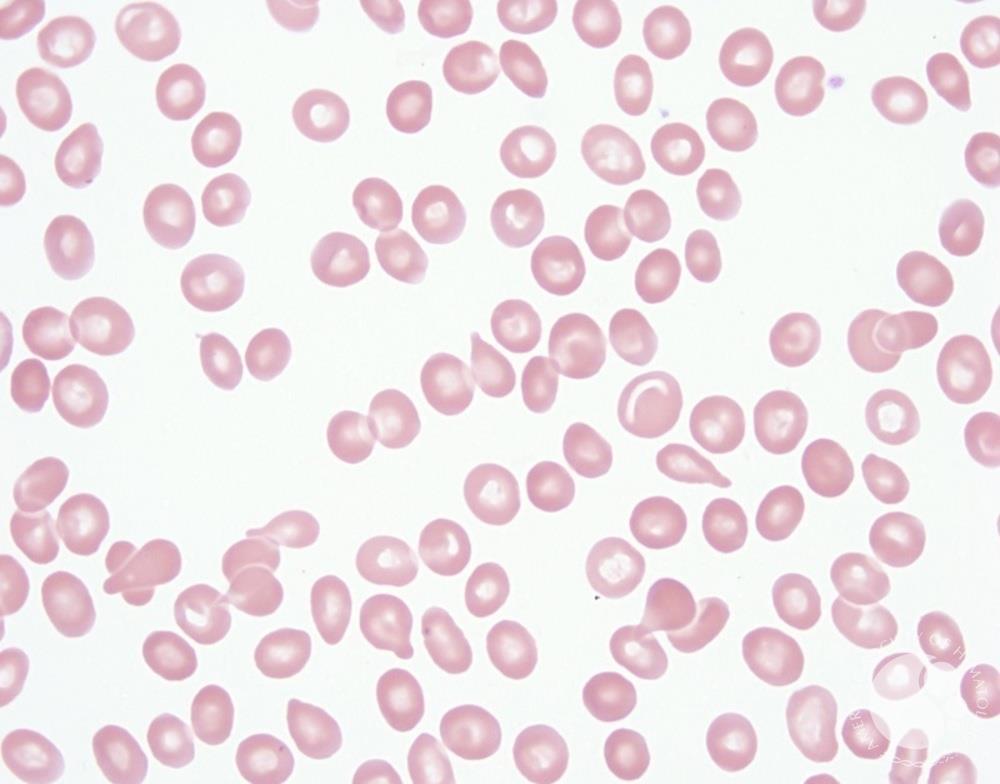
A couple of days more, my doctor said, “You have teardrop-shaped red blood cells. Now you need to get a bone marrow biopsy.” I searched YouTube videos and saw the big needle with the big handle drilling in. I asked, “Do I really need to? Is there another option?” She said, “That’s pretty much the gold standard.” I thought, Gold standard for what?
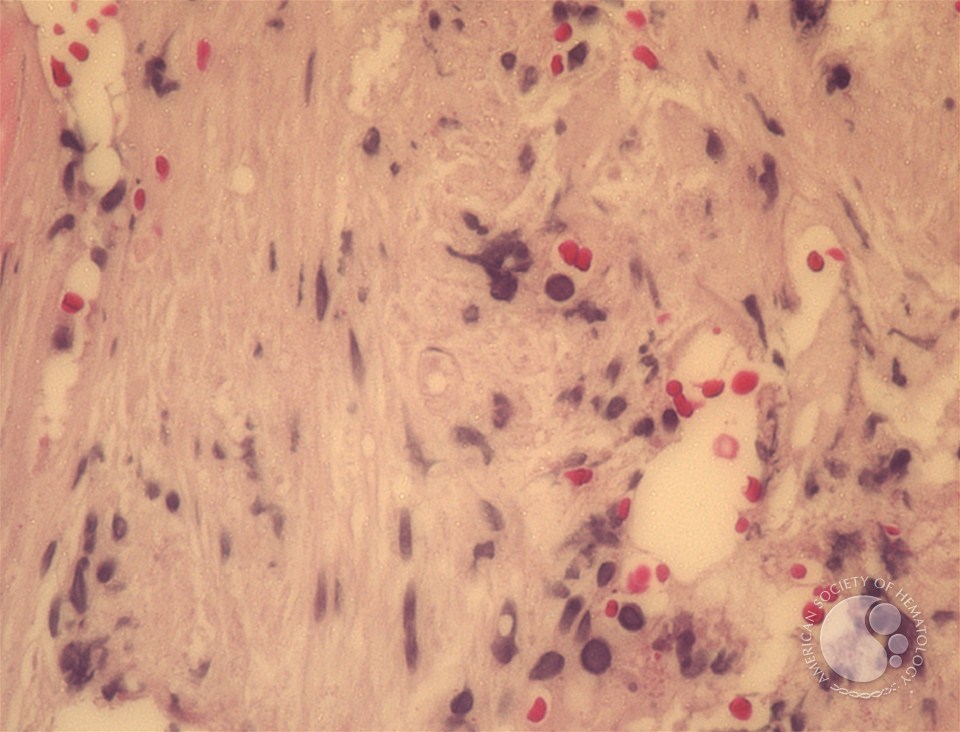
I was nervous about the procedure itself, but it wasn’t as bad as I thought. They did have a little trouble getting the marrow out. Later, I found out it was actually a symptom because I’m kind of dry.
Reaction to the diagnostic procedures
I was more anxious. I’m the type of person who likes to know all the details and I felt I wasn’t fed every detail. From the teardrop-shaped red blood cell, it pointed me in the same direction as well. I’m already thinking, I think this is it, but I’m not sure, and going back and forth.
How detailed did you get in your research?
I saw primary myelofibrosis as one potential diagnosis.
I don’t feel like I have cancer. Other than I have quite a bit of a strange bruising on me, which is normal because I’m clumsy, but those are in areas that I don’t usually hit myself with like the back of my finger. I still feel normal.
On one hand, I thought, Maybe the numbers are pointing in that direction. On the other hand, I just don’t want to believe it. Maybe something is wrong.

Were there any other symptoms?
Around late April, I had quite an episode of vertigo. Never happened to me before. I was driving home, probably 10 minutes away, when all of a sudden, I felt blood traveling from my left ear to the brain. It’s almost like I can hear it. Then my vision became blurry. I thought it was my contact lenses getting dry. I kept driving for a couple of blocks and the road just started moving. That’s when I got a little scared. I parked on the side of the street and closed my eyes. I couldn’t open my eyes. I called my husband to pick me up.
We went to the ER. They couldn’t find anything. I had a similar mini-episode about ten times for the next 2 or 3 weeks. I know when it’s coming. The noise comes then my head spins. If I keep my eyes closed, I’m okay.
I later read that it may have something to do with low platelets but I don’t hear too many people mention that. I didn’t make the connection until later on.
I still run and do weights. I work during Eastern time so I get off at 4 o’clock. I get really sleepy. I don’t usually take a nap in the afternoon but I would nap on the sofa for an hour and have him wake me up so I don’t sleep through dinner. That’s in the last month or two before the diagnosis.
Being referred to a hematologist
I’m the type of person who worries about a lot of small symptoms. I would email my PCP and she’d tell me if this is something to worry about. But this time, she acted very fast.
Three days after my blood test, I went back and looked at the history of our emails. She asked me to do the spleen ultrasound. A couple of days later, teardrop-shaped red blood cells. She said, “Read this.” In the paragraph, it already said leaning towards MPN and I had no idea what MPN is. Probably a week later, she said, “I’m going to refer you to a hematologist,” and that’s when my hematologist and I spoke.
Appointment with the hematologist
I think he had a hunch. My husband was listening to the call as well and I can tell he was trying to be very conservative. He asked me about my symptoms and was trying to gather information. Then he asked, “Do you have a sibling?” That was another clue for me.
He said, “I need a few blood tests.” He didn’t get into detail. I asked, “Am I going to get a chromosome test?” He said yes because I knew about the list of tests. I just want to make sure I’m getting all my tests.

Knowing more about your disease
As soon as I met my doctor, he said, “Don’t Google.” I’ll say the opposite but with a grain of salt. How would I be able to ask these questions or know what’s missing without knowing what tests pertain to my disease?
You have to look at reputable sites. I go to the Mayo Clinic and the American Society of Hematology. They’re hard to understand. I look at the article as if they’re a foreign language. I Google pretty much every word to understand.
I figured that it’s a disease so someone has to be able to understand it, no matter how complex. It boils down to something is wrong with you that’s causing this and therefore there’s a potential solution.
Diagnosis
How long did it take to get a diagnosis?
A month. It was the longest month.
During work, I was busy enough not to think about it. As soon as work was over, my brain just gravitated toward, “Could it be cancer? Could it be something else? What’s going to happen?”
I already looked at the life expectancy, but I didn’t know how severe I was. I did not find out about the scoring system so I don’t know how to score myself yet. What’s going to happen?
My son is 19. If I’m not here, financially, he will be okay. I planned this from when he was very young. But what if he needs guidance?
Who’s going to take care of my husband when he needs medical care? He is a lot older than me. How about my parents?
Eventually, my brain got really tired. I didn’t want to think about it anymore.


Getting the official diagnosis
I got the call with the diagnosis on July 8th. I remember when we had the call. Now, I think back, Would it have been better if it was in person or through video?
As soon as we got on the call, I could sense he was nervous. He wanted to be careful how to break the news to me. I told him, “I’ve already done my homework. I think this is what I have and if that’s the case, go ahead and tell me. I’d much rather know about it and get it over with.”
He explained the scoring system, my platelets, spleen size, and fibrosis. Mutation-wise, I’m okay.
As soon as we got off the call, I was Googling MIPSS70. Now it makes sense, but at the time, I didn’t know about it. All I know is I’m probably MF-3 but what that meant, I didn’t know.
Joining online support groups
Some are much more experienced. Some can read my bone marrow biopsy and tell me whether it’s good or bad because I couldn’t understand some of the terminologies. But a lot of time, people give you support and prayers, which are helpful, too.
Myelofibrosis scoring system
There are actually multiple scoring systems. China uses a slightly different scoring system, which doesn’t take into consideration the genetic mutation and the karyotype, which puts a person that potentially could be high risk into medium risk, which changes their life expectancy.
That was actually something I was trying to show in my Chinese group. The website is in English. People can actually click on the link and translate to Chinese. However, the algorithm stops working; it won’t do the addition for them, but it’s good to spread the word out there. You also want to look at those two as well, not just your blood count or your fibrosis level.
JAK2 gene mutation
JAK2 was my mutation type. I don’t remember what that karyotype was, but it was a deletion of one of the 44. That’s the part I don’t remember. But in the scoring system, it will tell you these are the bad ones so I fit into one of those.
Reaction to the cancer diagnosis
I wasn’t sure where the scoring system came from. I thought I’d done enough research. At first, I didn’t believe in the scoring system. But then when I started looking into it, I realized that they make sense and they’re very objective.
It’s either you have a platelet below a certain number or not, or you have this mutation or not. It’s black and white. Before this, I couldn’t tell. It’s just that I wasn’t prepared to have this number thrown at me.
Talking about the diagnosis with the family
My husband doesn’t talk much when it comes to this. I know he was trying to be very calm for me. He always said, “Maybe there’s a treatment out there. Maybe there’s hope.” He’s always trying to give me hope.
He likes to keep things to himself and I like to get it out of him so that’s our conversation. I would talk about my concerns and he doesn’t talk much.
My son, being a teenager, doesn’t talk much, but he occasionally would ask me or even his stepsister, “What’s going to happen to my mom? How many years can she live? Is it going to get bad very soon?”
You can tell he’s thinking about it, but he’s probably not comfortable coming up to me to talk. I wanted him to know right away because I think he’s old enough. I don’t want to hide this away from him.


Feeling healthy but knowing something was wrong
It was very hard. I was hoping to get a second opinion outside of Kaiser, but because it’s HMO, it’s different.
I was able to get a second opinion from a different hematologist within the Kaiser network. He took his time, looked through my numbers, and concurred with the diagnosis. I also reached out to four hospitals outside of Kaiser, some major cancer centers.
In our Facebook group, we always talked about MPN specialists. In my experience, it’s actually not that easy to get ahold of one.
My Kaiser hematologist isn’t an MPN specialist but his diagnosis was accurate. He said, “We handle one myelofibrosis patient each month,” but I didn’t know how to interpret that. Looking back, it’s probably a pretty significant number because Stanford handles about 25 myelofibrosis transplants a year.
Out of the four major hospitals, one of them got back to me. I can talk to a hematologist but not an MPN specialist and it will total about $5,000 out of pocket.
Understanding fibrosis
When your level is high, even after you’ve gone through a transplant, the fibrosis level is not going to decrease right away. It might take months before your fibrosis levels go down, which means your blood count may not go up as fast as other diseases so just be prepared.
One thing that I hear most commonly is, “Is there a drug out there that could shrink my spleen without lowering my blood count too much?” A lot of the time, by the time your spleen is enlarged, your blood count is already borderline. You’re getting close to being transfusion-dependent.
They’re all related to each other. When your fibrosis is high, your bone marrow is not making as much blood, therefore, your spleen is working extra hard to make up for it.
Some patients have spleens that are much bigger than mine and they couldn’t find a solution to reduce it. I feel bad for those patients because their spleen needs to be shrunken enough to get a transplant. I’m lucky enough that mine was just slightly enlarged. Some are 24 cm. Mine was 18.
Treatment
Discussing treatment options
He said that I might want to consider a transplant in the near future. I said, “Oh, that’s why you asked me about siblings last time.” He said, “You may not need it right away, but it’s better to consider when you’re still relatively healthy.”
He spoke very slowly just to make sure I could digest everything. I think he said I had at least 1 to 2 years. Maybe it’s five years because I didn’t feel that bad.
I didn’t digest it at that moment. I’m kind of a dinosaur when it comes to this kind of thing, but eventually, it kicks in.
I’m not too worried about dying myself, for some reason. I’m just worried about leaving people behind. What can I do now for these people? I don’t know why. It just never dawned on me. It’s not scary for me to die, but it’s scary to leave people behind.
Stem cell transplant
I pushed for the transplant. When I went in for my first appointment with the Stanford transplant doctor, after the discussion, I said, “I’m ready. Just give me a date.”
When I got the date, October 1st, I did a lot of preparation beforehand and even imagined what my room would look like.
I love the nurses there. I had about at least 15. I met 15 nurses because you have a morning shift and a night shift. I learned so much from just talking to the nurses. Why do we do this? Why is this way? Why does the chemo nurse have to wear another gown and there’s always another nurse there just to make sure I’m getting the right chemo?
They kind of became my family during those 23 days because my husband doesn’t talk much. He would spend a whole day sitting in the room with me, keeping me company, but we didn’t talk much. But when the nurse comes in, we talk, even in the middle of the night. I thought I would not have much sleep. I wake up every few hours, but I just went right back to sleep.
I started fludarabine on October 1st. I had four days of fludarabine followed by melphalan; that’s the day we need to chew ice. Forty-five minutes before, I was getting cups of ice chips from the nurse, chewing non-stop all the way through then 30 minutes after. No mouth sores at all throughout the process.
On day zero, I started to feel tired. On days one and two, barely ate, but I had fruits. The next few days, my husband pushed me to get up, walk around, and take a shower. We were supposed to walk around half an hour a day. There’s this pink mask that we wear when we go to the hallway, which makes it harder to breathe. But if I exercise in the room, then I don’t need to wear it.
I danced with my IV pole. I like dancing, but he is not into dancing so I danced with my IV pole because then I can grab the pole with me wherever I want to go. It was really fun because we played music. That was one of my exercises. I even brought in my 8-lb weight at some point so I did some weights, too, because I know I’m going to lose muscle.

Side effects of stem cell transplant
Overall, the experience was a lot smoother than I imagined.
I thought I would have a reaction to the chemo right away, but it wasn’t until 5 or 10 days after that my body started to feel them.
One way to describe the initial feeling of chemo was kind of like towards the end of pregnancy when your body is getting heavier and heavier. It’s harder to do basic stuff. Going to the bathroom takes a lot of energy. Taking a shower requires two people.
Then comes the nausea and diarrhea, but they can be controlled. What I found out later was ondansetron works for me. It doesn’t work for all patients. One of the nurses said I could have it every eight hours so I never feel the nausea and I’m ahead of the game. As soon as that happened, I was able to eat a lot more than before.
Possibility of graft-versus-host disease (GvHD)
I think age makes a difference. My brother being a full match made a total difference. Once I got my diagnosis, the first thing I did was call him. He was in China. I said, “I need you to go get an HLA typing done. I don’t want to wait for the doctor to send you the kit,” so he did and the results came back very fast.
Looking at the typing, it’s so easy to understand. They look like 12 sets of timestamps. You compare one against the other. If you match, you match. I didn’t think he would be a match because we have different blood types. He was 12 out of 12. Full match.
After that, he said, “Let me know when you can get your transplant scheduled. I need to buy the airplane ticket.” At the time, China was still on lockdown due to COVID. He lives in Shenzhen across from Hong Kong; that city was locked down so we were worried he could not leave. Fortunately, right before his departure, it opened up.
It was better than winning the lottery. You can’t buy a perfect donor match, especially one who’s related. It would be nice to win the lottery, too. But when you’re in that situation, this is definitely better because the lottery can’t save a life.

Recovering from stem cell transplant
For the first three months, I was supposed to be hiding away upstairs. I didn’t completely follow that because I felt okay. I was weak. When I went upstairs, I felt my legs were heavy. I thought maybe I could use going up and down the stairs as an exercise to gain strength.
I was hungry all the time so at midnight, I would be eating mini saltine crackers. My husband said I sounded like a little mouse in the bedroom. At four o’clock, I’ll be hungry and crave traditional Chinese food. I would be cooking rice soup and steamed pao at 4 o’clock. He doesn’t know how to cook those.
For four or five meals a day for about a month or two, I ate whatever I wanted to eat and did not gain weight. That was probably the only time in my adult life I would not gain weight eating like that.
For the first three months, I went back to Stanford ITA once every three days to check my blood. I needed a transfusion a couple of times. After that, I was fine and they just checked if I needed any adjustment on my medication.
They want to make sure because, during those first three months, you could have acute GvHD. Your blood count can fluctuate quite a bit.
Advances in research & treatment options
I actually met a lot of patients who aren’t the best candidates for a transplant. There are definitely medications to bring up their platelet or their red blood cell count. I actually talked to a lot of families of patients like that.
There’s not a whole lot that can be done. A lot of times, the patients themselves are not optimistic about what could happen to them. It’s really hard for their families to get them to a different state unless the patients are ready to deal with it.
Follow-up protocol
I still go in for follow-ups once a month. Probably at least for another year.
Community support
Importance of finding support in a community
I met a 71-year-old patient. She arrived at Stanford two weeks after me and had some complications. She ended up having to go back there and was actually hospitalized. One day, I met her in ITA and it’s like a reunion. It felt good to see someone who’s been through it with you.
That’s the reason why I started to blog online with hashtags specific to myelofibrosis. A lot of patients chime in. They know what I went through.
Sometimes they ask for my opinion or my suggestions. I didn’t post on a site where all my friends were because I didn’t want them to feel uncomfortable not knowing how to talk to me about this. I know some did get uncomfortable when they eventually found out. I don’t want to impose on them by doing that.


Supporting patients with different backgrounds
China has a very different dynamic. Patient-doctor relationships are a little different. A lot of times, patients are afraid to ask the doctor questions so they actually help each other.
The patient actually knows more about the disease than a lot of the patients here. Give them a bone marrow biopsy report and one person can look at the different numbers and decipher it for you.
The treatment options are slightly different. The philosophies are different there, too. China seems to believe in MAC approach versus the reduced intensity (RIC) approach. They want to clear all your marrows, make sure there are no bad cells in there, and then bring in the stem cell. But here, studies show that the reduced intensity produced just as good as a result.
As a result, when patients go through MAC, there is a lot of damage to their organs. They are in the hospital for two weeks of chemo and they have much stricter diet restrictions. I felt that slowed down the recovery.
There was actually one patient I met who was going through a myelofibrosis stem cell transplant. It’s very hard to find a full match for Asians. He couldn’t find any good match. I got lucky because my brother is a full match.
His two sisters flew in from China; they’re not good candidates. I think he ended up using his daughter, which is very rare. It’s very rare to use kids but the daughter pulled through. He’s going through a haploidentical transplant, which is a little harder. I think it’s a lot harder than mine because there’s more chemo involved to reduce GvHD. He had days of fever.
I message him sometimes. I message other patients as well or they message me. There are a couple that are about to go into transplant at Stanford. I want to share my experience and I want them to benefit from mine as much as they can.
Words of advice
Knowledge is power. There’s a lot of information that’s not valid. You just have to figure out which one pertains to you. Use information from Facebook groups because some of these patients did go through the transplant so they can validate one way or the other.
A lot of times they say you don’t need to know about it and just let the doctor take care of you, but you also need to be able to make calls. Is this treatment for me?
For example, when I was given the initial chemo protocol, it was part of a clinical trial with T-cell depletion, which doesn’t make sense for a full donor match so I questioned that and then it was changed to a different protocol. I’m not saying not to trust the doctors, but I think there’s a reason they put you in one versus the other. Do your homework. Make your own call.
Clyde’s Caregiver Story
What do you remember from the first time you saw Cathy?
We were both employed by the same company. I sized her up as being a very quiet, introverted, typical Asian lady, which she was. It turned out that once you get to know her, she’s a very assertive, intelligent person with a mind of her own. We started dating about two years after she started working there. It was only then that I found out she was very assertive.
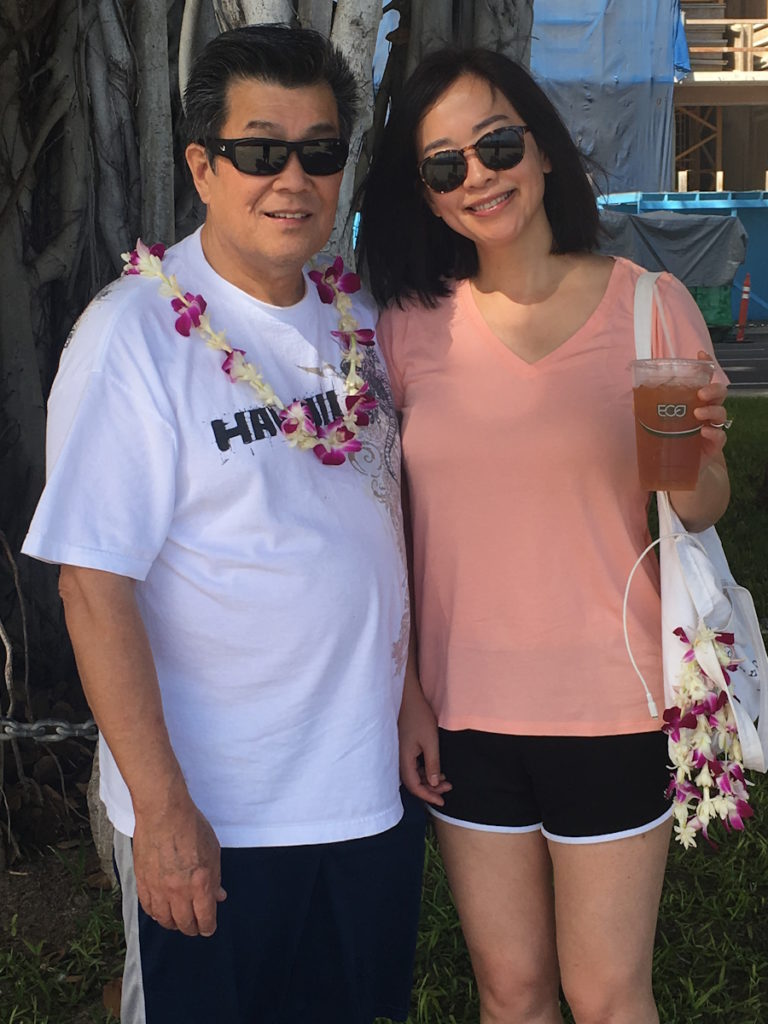
What do you like doing together?
There’s a 17-year age difference between us. There’s a cultural difference so there’s not a whole lot that we have together in common.
She likes to dance; I like to sit by the wayside. She likes to eat Chinese food; I like to eat Mexican food. Our life has been a series of compromises more than anything else.
We like to do a little bit of cooking together. We like to help out with non-profit organizations. We went to Mexico once to build a house with our school church group, but age prohibited me from doing it again. Cathy and her son Tom made a second trip down there in 2022 to help build a house.
It’s a very satisfying experience and I would encourage other people to go and do it. It allows them to see how people who are not so fortunate live. They don’t have running water, they don’t have electricity, they don’t have flush toilets, or anything else.
Reaction to Cathy’s blood test results
My personality is not to be the knee-jerk, oh-my-gosh type of reaction. We’ve got something here that’s not very normal. Let’s just see where this goes first. I had a little bit of time to process.
For the next day or two, I was thinking, It could be absolutely nothing or it could be something a little bit more serious. As time rolled on and we did more and more tests, it became very obvious that this wasn’t something that was just going to be simple. It was something that was serious.
Later on, I realized that it was something that was extremely life-threatening. It hit me a little bit slower than it hit Cathy.
I think Cathy is the type of person to look at it and say, “Okay, I know exactly where this is going.” Maybe she’s a little bit too over the top; that’s her personality and for this situation, it worked out best for her.
Understanding myelofibrosis
Cathy is the type of person to do a lot of the research. As she was doing the research, she would tell me what was going on and then I would slowly process it, but there really wasn’t anything else that I could do.
I’d talk to her every once in a while, figure out where she’s going with this, learning what she learned because she’s a very good learner at this. I’m a very slow learner so I’d have to ask her question after question after question before it would sink in.

Impact of a life-threatening disease
I couldn’t fathom it. I couldn’t fathom losing my wife. She’s a lot younger than I am and it was just racing through my head that this isn’t fair. I should be the one that should go first. I was just so afraid that I’d lose her. That was the hardest thing for me to process.
Once I got over that, I realized that we weren’t throwing in the towel. Not now, not when we still have options. She’s a strong lady. She was going to deal with it.
Because we’re a team, we’re going to see this thing through together. I’m going to be there every step of the way. I’m going to give her encouragement and we’re going to fight this together.
I had a pretty good feeling that we were going to beat this. I say we because it is her and me. As a caregiver, maybe you’re not doing the actual fighting, but you’re doing all of the support.
Caregiver’s role in the fight against cancer
If any of you have ever been in the military, you’ll know that there are actual people fighting, but 90% of the forces are in a support position. Without those people, the soldier isn’t able to fight.
As the patient, Cathy’s responsibility is to get better. As the caregiver, your responsibility is to do everything else. She doesn’t have to do anything else except get better.
We’re responsible for making her feel comfortable, whether that’s rearranging her bedding, helping her with the clothes, or getting her food. Everything else is up to me, the caregiver.


What was the biggest surprise, lesson, or difficulty for you?
The hardest thing for me was to show strength. I knew I had the strength, but emotions got in the way. The emotions and the fear of losing somebody that you actually love.
I needed to be strong. I needed not to show my worry and my concerns that things might not go the way that they need to go.
I wanted to show her a positive attitude. I wanted to put on a good face for her and show her that I’m positive that things are going to get better and that eventually, we’ll get back to as near normal a life as we possibly can.
Not taking care of one’s self
I felt that I wasn’t taking care of myself. You hear this all the time. You have to take care of yourself before you can take care of somebody else and I forgot that. I was running around to the point where I was running myself ragged.
Cathy saw that and she said, “You need to stop coming in so early in the morning. Instead of coming in at 8:00 or 8:30, come in around 10:00 or 11:00, and give yourself a little bit of time.” I did and it got better.
You do have to take care of yourself. If the caregiver falls ill, then the caregiver can’t take care of the patient.
Early signs of caregiver burnout
Everybody’s different. Maybe you start to get body aches or something like that or maybe you’re not thinking straight.
For me, it was getting very irritable. I was getting tired and getting body aches.
Look out for triggers. Are there changes in their personality? Are they doing things differently? Are they forgetting things? Are they getting clumsy? Anything like that is probably a sign that you’re getting stressed out.
Differing perspectives between patient & caregiver
Cathy is a very intelligent person and she studied this quite extensively. She’s the patient. She has an idea of what she wants. Because it is her health, I usually will defer to what she has to say.
If I had a very strong opinion in the opposite way is the only time that I would speak up. But at the same time, I’d say what I had to say and then it would be her final decision.


Advantages of patient education
They say knowledge is power. But at the same time, you have to be careful when you start looking up information on the Internet. Take it maybe with a grain of salt.
If this website pops up and says you should be doing X, Y, and Z, you have to look at the website and ask yourself, “Is this a reputable website?” If you go to another website like Stanford Hospital or the Mayo Clinic, you put a little bit more weight into what they say.
I also think that once you get on these Facebook groups, they’re good and they’re bad. They’re good because they give you support. They tell you what other people have gone through.
At the same time, you have to realize that the majority of these people are on there because they have a special issue with something. When they say, “Oh my god, this is hurting me, this is doing this to me. I had this as a symptom,” maybe the majority of people don’t have those symptoms. Be aware that they can happen to you, but take it with a grain of salt.
Words of advice
Brightening up the room really helps the patient. We had these static window stickers of plants, leaves, and all these little things that would brighten up the room. When we got to the hospital room, someone had painted a little rainbow and sunshine on the windows and the stickers were still there. We just went there recently and they’re all still up there so other patients have been using them and it’s brightening up the room. It lifts your spirit more than anything else.
Bring a rolling suitcase; that’s more for the caregiver because the caregiver is going to be taking things back and forth with them all the time. They’re going to be bringing in clean clothes, taking out dirty clothes, and maybe bringing in a little bit of food or other supplies that they maybe had forgotten the first time around. It’s just a lot easier bringing in a rolling suitcase.


In a hospital, you don’t need to worry about medication. The nurses are constantly monitoring that. But when you get home, again, it’s the caregiver’s responsibility to do virtually everything, and that includes monitoring the medicine.
A patient frequently has brain fog. They don’t know what they did. They don’t know what they should be doing. It’s up to the caregiver.
Get a two-week supply of pill bottles, each marked from Sunday all the way through Saturday. Load them all up with the morning, afternoon, and evening pills. Put them all in separate containers. That way, it’s one less thing for the caregiver to worry about.
By the time you go through the first week, you still have a one-week supply and you should be refilling the empty containers. If you can’t refill the empty containers, you know immediately that you need to order medication. Ordering medication immediately rather than waiting until they run out helped us quite a bit.
Importance of diverse community support
It’s important both to Cathy and to the other patients. To Cathy, I think it’s a mental stimulation for her. Work is one thing, but work is just work.
Helping other people is something that I think she really feels gratified in doing. At the same time, with these other people, frequently, they’re at a loss. They don’t know who to turn to. A lot of these people are overseas in China and sometimes they don’t get as good information as we do over here in the United States.


Inspired by Cathy's story?
Share your story, too!
More MPN Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant