The Right Dose: Finding the Balance in Cancer Treatment
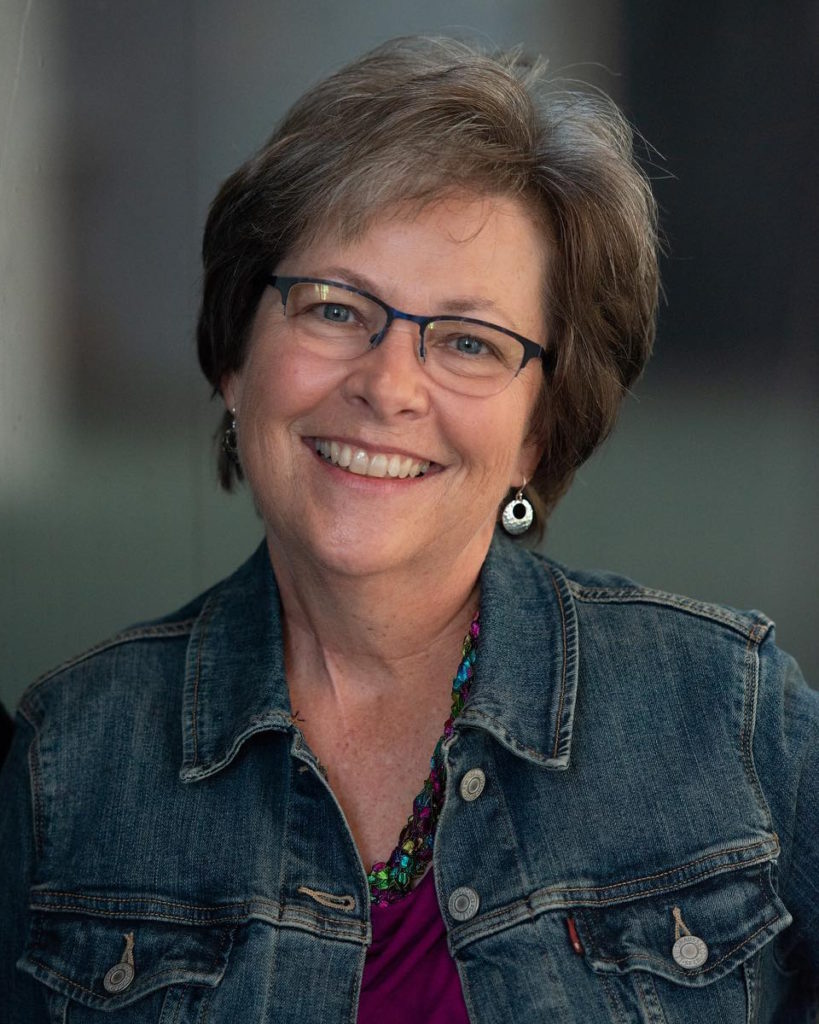
Janice Cowden is an advisor for The Right Dose. She was first diagnosed with breast cancer in 2011. Nearly five years later, she developed metastatic breast cancer, which meant the cancer had spread to other parts of her body.
Chelsey Pickthorn is also a metastatic breast cancer patient and, together, they discuss advocating for the “right dose.”

Many patients are put on treatments to help lengthen survival but it comes at the cost of severe, debilitating side effects
In this conversation, they voice how to find the right dose, how to bring it up with your doctor, and the importance of advocating for yourself.
Brought to you in partnership with Project Life.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I was completely shattered… Being diagnosed at 33, I thought that my whole world had come crumbling down.
Chelsey
Getting the cancer diagnosis
Janice: You actually remember every single moment when you get diagnosed. I can put myself right back in the office, hear the words, and feel the moment.
He said, “I have really bad news. You have stage 4 breast cancer. We have to get a biopsy to see if it’s still triple-negative.” But he just looked at me [and] said, “This isn’t good.” My husband and I both left in tears.
Chelsey: My mom, my grandmother, [and] my great-grandmother on my paternal side all had breast cancer. For me, it was the question of when and how long I have until this [will] happen.
I was suggested to get mammograms at 30 and I neglected to do that. At 32, I found a lump on the left side. I went in and I realized my nipple was inverted. I had a biopsy. They put a clip and everything was fine.

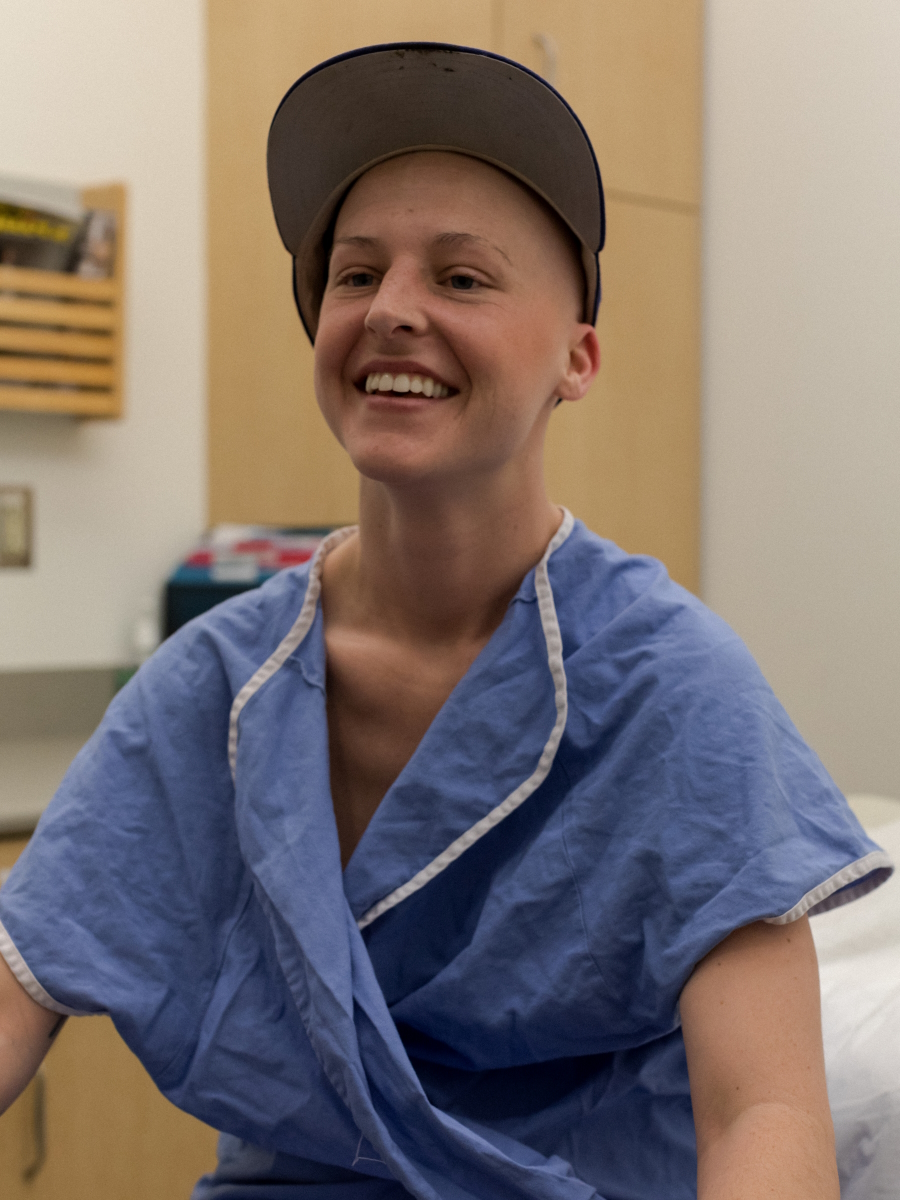

Fast forward one year later, I ended up finding a lump on the right side. Unfortunately, it was triple-negative.
I was completely shattered. I had a business. I had a lot of responsibilities. Being diagnosed at 33, I thought that my whole world had come crumbling down.
Having so many people in my family [diagnosed with breast cancer], I had what I thought was such a wealth of knowledge, but I had never heard of triple-negative.

Breast cancer treatment
Chelsey: I heard the term red devil before and when I heard that, that was when I was like, “Oh, this is really real. This is not just a joke or a simple little thing that might go away quickly.”
I did Adriamycin-Cytoxan and I made a lot of lifestyle changes. Being a hairdresser and standing behind the chair, I had to adjust my work schedule. Touching my legs after a day of work felt like I would shudder at just the tiniest touch, fall to the ground, and be ready for bed.
Janice: I had chemotherapy both times because, at the time, there weren’t any targeted therapies for triple-negative.
When you know you’re metastatic — you’re stage 4, it’s terminal, it’s incurable — I think at that point, you’re willing to endure just about anything because it’s your life.
Janice
Side effects from chemotherapy
Janice: I had a really rough time with my stage 1 treatment, which was Taxotere-Cytoxan. I had horrible mouth sores. I was very, very sick. I ended up having to get two dose reductions during that chemotherapy.
When I had Adriamycin, I didn’t end up requiring any dose reductions, but it made me pretty sick. It’s a really, really harsh chemotherapy. Adriamycin’s known as the red devil and it lives up to its name. It was really tough.
When you know you’re metastatic — you’re stage 4, it’s terminal, it’s incurable — I think at that point, you’re willing to endure just about anything because it’s your life.

Being 33, I wanted to be normal. I really wanted to put on a happy face, pretend I could get through this, and that everything was going to be okay.
Chelsey

Chelsey: The Adriamycin-Cytoxan was nasty. It was just not nice at all.
One side effect [was] peeing red. I’m like, “Okay, this is going through me really quickly.” And you just think, “What else is it hitting that fast?”
I didn’t have so much diarrhea. I had constipation from the steroids and from all the medication and that was the number one thing for me.
After you’re constipated for seven [or] 10 days, you get angry. You just really want it out of you so that was a really big struggle for me.
Being 33, I wanted to be normal. I really wanted to put on a happy face, pretend I could get through this, and that everything was going to be okay. Not being able to really open up and have the support that I needed definitely [affected] my relationships. I had support, but no one really knew exactly what it was like going through it. Feeling very lonely and disconnected from my community [and], at the same time, having them be there. That was really a struggle for me as well.
Janice: When I had the side effects from the Taxotere, I started with mouth sores.
My mouth was so tender. The mouth sores were on my gums, on the insides of my mouth, on the roof of my mouth, on my tongue, [and] in my throat. Anything hurt, even water. It hurt to drink it if it was cold, it hurt to drink it if it was too warm.
Even though I was on a soft food diet, everything burns. It stings and it’s painful. When they start going down your throat, then it’s not only painful when you’re trying to chew food, but it’s painful to swallow. And so you just decide to stop eating and even drinking.
I developed systemic thrush as a result. I went back and forth between all kinds of GI symptoms — diarrhea, constipation — and it would just go back and forth. I lost about 18 pounds in three months because I couldn’t eat.
When you’re dealing with GI side effects, you don’t know what to expect. One day, you may have horrendous diarrhea. Then you may not go at all for another four or five days. And so then you’re really confused. I treat the diarrhea and then I have constipation, then I have to treat the constipation, which then flips back to diarrhea. Your days just center around, Okay, which do I do? Do I treat diarrhea today? Do I take the chance that I don’t treat [it]? Because then I don’t want to get constipated.

When you’re dealing with GI side effects, you don’t know what to expect… I didn’t want to leave the house.
Janice

I didn’t want to leave the house because I didn’t know what to expect. Sometimes those bouts of diarrhea would come on suddenly and you certainly didn’t want to be caught out somewhere, you know? I didn’t feel like going out anyway.
My nose [and] my eyes ran constantly. I was miserable.
Finding out about dose reductions
Janice: I didn’t know about dose reductions. When I went to my oncologist for the third round, I think it was, he saw how sick I was and how awful my mouth and everything else was. I was just in terrible shape. He said, “We’re going to reduce your dose.”
It helped a little bit. But by the time I reached my fourth round, which was three weeks later, I still wasn’t well enough for him to feel comfortable giving me even that dose. So he reduced it [further].
Quality of life and longevity [are] the most important things I’m looking at. Being 38, I want to live as long as possible.
Chelsey
Chelsey: The prognosis of triple-negative and knowing the recurrence rate in five years was very heavy on my mind. Having had two grandmothers who passed away from metastatic disease, I was riddled with a great deal of fear.
At my one year, I noticed a small bump on my upper shoulder and I mentioned it to my doctor. Three months later, it wasn’t gone. It was still there and it was bigger.
I went on vacation and thought, All right, I’m going to enjoy myself on this vacation. But I booked a doctor’s appointment and sure enough, they immediately biopsy it that day.
The next day, I was getting a scan and had the tech basically say to me, “Well, you’re metastatic.” I remember laying there in the scanning machine and just lost it.
If this is what that is, which it sounds like it is, I was like, “Wow, what a terrible way to find out.” I said to my doctor, “I can’t believe the tech would even mutter those words to me.”
Sure enough, it was metastatic and I had another spot on my lung. My oncologist said, “We’ll just put you back on ACT.”

The knowledge that I do have from my mother and my family is many times, chemo is what kills people. I said, “Hell no. I’m not going back on Adriamycin-Cytoxan. There’s absolutely no way because how long am I going to have to live? I’m 34 years old.”
I started trying to put out feelers and figure out what my options were. I had to switch insurances, which was just a huge stress. And, of course, working to have my insurance to be able to then have care was just a terrible situation.

I had foundation medicine done and it opened me up. I have a somatic BRCA mutation so that opened me up to be on a trial for olaparib.
Initially, the side effects were extremely low. I had a couple [of] bouts of diarrhea, but I really tried to control a lot of that stuff with my diet. I basically had been on it for about two and a half years until infections. [In] 2021, I had shingles, impetigo, COVID three times, [and] E. coli twice. The actual personal side effects seemed low, but the infections and the susceptibility that I had to everything [was] just over the moon.
[After being on the olaparib for 1.5 years, she was seeing results]. Once I hit that mark, I said, “Why wouldn’t we titrate or pull things back? Because I’m well and I’m on a trial so it’s very regimented, it’s scheduled.” My doctors were like, “Oh,” at first.
Each appointment I kept going back, “Okay, I’m ready. Are we going to do this?” Finally, I think it had been a year, they went to the trial and requested a dose reduction.
Quality of life and longevity [are] the most important things I’m looking at. Being 38, I want to live as long as possible. I’m not really interested in having leukemia and all of these other comorbidities that develop from medication. So that’s the driving force for me asking for a dose reduction because I was in a place of success, I should say. Why would I continue to keep poisoning myself while it’s done its job at this point?
You have to self-advocate. You have to be okay with going to your oncologist and saying, ‘We need to talk about this,’ because it should be a decision between you and your oncologist.
Janice
Janice: I think a lot of people don’t even realize that they can ask for a dose reduction or they don’t know to go to their oncologist and say, “How can we better manage these side effects I’m having? How can we improve my quality of life? Because I don’t want to give up treatment, but at the same time, I’m not having a quality of life with the side effects that I’m having from the treatment.”
You have to self-advocate. You have to be okay with going to your oncologist and saying, “We need to talk about this,” because it should be a decision between you and your oncologist.
A lot of times, as good as they are at treating our cancer, our physicians don’t necessarily look at the whole person and how our lives are outside of treatment. What is the impact? Are we able to get out of bed during the day? Are we so fatigued? What are those side effects that are causing us to have such a poor quality of life?





The first is just to encourage patients to advocate for themselves. If they are having side effects that are really destroying their quality of life, they need to have that conversation.
Many patients that I’ve talked to [are] afraid to report side effects from their treatment because they’re afraid that their oncologist is going to pull them off treatment that’s working. They don’t want to complain. They don’t want to be seen as a whiner. But these are things that your doctor needs to know.
Clinical trials are quite different than when you’re just getting standard of care from your oncologist because those conversations occur between you and your oncology team whereas, in a clinical trial, you have a few more people that are involved.
But even when you’re in a clinical trial, you absolutely should be able to talk to the trial investigator or the person seeing you, whether it’s a nurse practitioner or just one of the nurses working with you in the trial. You can still report it to your oncologist as well.
These are things they need to know because side effects are reported in clinical trials. For patients who may receive that drug, if it’s FDA-approved down the line, we need to know those side effects. Were they mild? Were they moderate? How much did they impact your quality of life? That’s when we need to determine: is that dose the right dose really for that patient? Because if you reduce the dose and the quality of life improves and the side effects lessen, then we need to look at that a little more closely.


At the end of the day, what we’re looking at is personalized medicine: getting the right dose, the right drug, for the right patient. We don’t experience the same side effects from a drug.
Unfortunately, the new targeted therapies and endocrine therapies come in one dose. What we really need to start looking at is: Are they effective? Are they as effective at lower doses? Does that mean that patients could have a better quality of life and still have [the] quantity of life?
The toxicities would be less because we’re on this for life so you want to preserve as much of your organ function and your general health as you can. When you’re suffering from extreme toxicities and side effects from drugs, sometimes those either cause patients to discontinue treatment or the toxicities become so severe that their organ function is impaired. And that alone will lead to also a lesser length of life as well.
We’ve looked at this whole paradigm of maximum tolerated dose. Decades later, why are we still doing that? Why are we still pushing for the highest dose possible when we could possibly look at the optimal dose?
What is the optimal dose? If that means it’s lower, it’s still effective, and we’re creating fewer toxicities and patients can stay on the drug longer, patients will take the drugs because they’re not dealing with severe side effects, then it’s a win-win. At the end of the day, it’s a win-win for oncologists and for patients.
At the end of the day, what we’re looking at is personalized medicine: getting the right dose, the right drug, for the right patient.
Janice
Metastatic Breast Cancer Patient Stories
Deb O., Breast Cancer (De Novo Triple Positive and ER+ HER-)
Symptoms: First instance: appearance of lump that later on increased in size, orange peel-like skin around inverted nipple, persistent ache under right arm; second instance: appearance of lump
Treatments: First instance: chemotherapy, targeted therapy, hormone therapy; second instance: surgery (mastectomy), chemotherapy, radiation therapy, CDK 4/6 inhibitor
Tammy U., Metastatic Breast Cancer, Stage 4
Symptoms: Severe back pain, right hip pain, left leg pain
Treatments: Surgeries (mastectomy, hip arthroplasty), chemotherapy, radiation therapy, hormone therapy, targeted therapies (CDK4/6 inhibitor, antibody-drug conjugate)
Nicole B., Triple-Negative Metastatic Breast Cancer, Stage 4 (Metastatic)
Symptoms: Appearance of lumps in breast and liver, electric shock-like sensations in breast, fatigue
Treatments: Chemotherapy, surgeries (installation of chemotherapy port, mastectomy with flat aesthetic closure), targeted therapy (antibody-drug conjugate), hyperbaric oxygen therapy, lymphatic drainage
Dalitso N., IDC, Stage 4, HER+
Symptoms: Appearance of large tumor in left breast, severe back and body pain
Treatments: Surgery (hysterectomy), vertebroplasty, radiation therapy, hormone therapy, clinical trial
Marissa T., ILC, Stage 4, BRCA2+
Symptoms: Appearance of lump in right breast, significant fatigue, hot flashes at night, leg restlessness leading to sudden, unexpected leg muscle cramps
Treatments: Chemotherapy, hormone therapy, PARP inhibitor, integrative medicine
Janice C., Triple-Negative Metastatic Breast Cancer, Stage 4
Symptoms: Appearance of lump in left breast near sternum, fatigue, bone and joint pain
Treatments: Surgery (lumpectomy), radiation therapy (brachytherapy), chemotherapy
Dana S., IDC, Stage 4 (Metastatic)
Symptom: Appearance of large lump in left armpit
Treatments: Targeted therapy, hormone blockers, bone infusions
Maria S., Breast Cancer, Stage 4
Symptoms: Intermittent but severe pain including a burning sensation on the side of the breast, appearance of a cyst and a lump, abnormally warm and pink-colored breast, nipple inversion, strangely liquid menstrual periods, unusual underarm odor, darkening and dimpling of the nipple, severe fatigue, night sweats
Treatments: Chemotherapy, surgeries (mastectomy, lymphadenectomy), radiation therapy, targeted therapy
- 1
- 2








One reply on “The Right Dose”
I’m thankful for this story’s
They gave me hope and trust I will survive 💖